Abstract
Background
Laparoscopic liver resection (LLR) has become an essential method for treating malignant liver tumors. Although the perioperative and oncologic outcomes of LLR in patients with hepatocellular carcinoma have been reported, there are few reports of LLR for intrahepatic cholangiocarcinoma (IHCC).
Methods
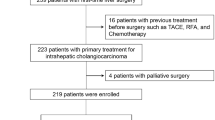
Patients who underwent liver resection for T1 or T2 IHCC between March 2010 and March 2015 in Gyeongsang National University Hospital were enrolled. They were divided into open (n = 23) and laparoscopic (n = 14) approaches, and the perioperative and oncologic outcomes were compared.
Results
The Pringle maneuver was less frequently used (p = 0.015) and estimated blood loss was lesser (p = 0.006) in the laparoscopic group. There were no significant differences in complication rate (p = 1.000), hospital stay (p = 0.371), tumor size (p = 0.159), lymph node metastasis (p = 0.127), and the number of retrieved lymph nodes (p = 0.553). The patients were followed up for a median of 21 months. The 3-year overall survival (OS) and recurrence-free survival (RFS) rates were 74.7 and 55.2 %, respectively. No differences were observed in the 3-year OS (75.7 vs 84.6 %, p = 0.672) and RFS (56.7 vs 76.9 %, p = 0.456) rates between the open and laparoscopic groups, even after the groups were divided into patients that received liver resection with or without lymph node dissection.
Conclusion
LLR for IHCC is a treatment modality that should be considered as an option alongside open liver resection in selected patients.


Similar content being viewed by others
References
Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, Pawlik TM, Gores GJ (2014) Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol 60(6):1268–1289. doi:10.1016/j.jhep.2014.01.021
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker C-G, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey J-N, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS (2009) The international position on laparoscopic liver surgery. Ann Surg 250(5):825–830. doi:10.1097/SLA.0b013e3181b3b2d8
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schon MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261(4):619–629. doi:10.1097/SLA.0000000000001180
Abu Hilal M, Badran A, Di Fabio F, Pearce NW (2011) Pure laparoscopic en bloc left hemihepatectomy and caudate lobe resection in patients with intrahepatic cholangiocarcinoma. J Laparoendosc Adv Surg Tech A 21(9):845–849. doi:10.1089/lap.2011.0247
Uy BJ, Han HS, Yoon YS, Cho JY (2015) Laparoscopic liver resection for intrahepatic cholangiocarcinoma. J Laparoendosc Adv Surg Tech A 25(4):272–277. doi:10.1089/lap.2014.0233
Tsai TJ, Chouillard EK, Gumbs AA (2012) Laparoscopic right hepatectomy with intrahepatic transection of the right bile duct. Ann Surg Oncol 19(2):467–468. doi:10.1245/s10434-011-1927-5
Gumbs AA, Jarufe N, Gayet B (2013) Minimally invasive approaches to extrapancreatic cholangiocarcinoma. Surg Endosc 27(2):406–414. doi:10.1007/s00464-012-2489-8
Morine Y, Shimada M (2015) The value of systematic lymph node dissection for intrahepatic cholangiocarcinoma from the viewpoint of liver lymphatics. J Gastroenterol. doi:10.1007/s00535-015-1071-2
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. doi:10.1097/SLA.0b013e3181b13ca2
Dodson RM, Weiss MJ, Cosgrove D, Herman JM, Kamel I, Anders R, Geschwind JF, Pawlik TM (2013) Intrahepatic cholangiocarcinoma: management options and emerging therapies. J Am Coll Surg 217(4):736–750. doi:10.1016/j.jamcollsurg.2013.05.021
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection—2,804 patients. Ann Surg 250(5):831–841. doi:10.1097/SLA.0b013e3181b0c4df
Chan FK, Cheng KC, Yeung YP (2014) Laparoscopic liver resection: lessons learnt after 100 cases. Hong Kong Med J 20(5):386–392. doi:10.12809/hkmj134066
Takahashi M, Wakabayashi G, Nitta H, Takeda D, Hasegawa Y, Takahara T, Ito N (2013) Pure laparoscopic right hepatectomy by anterior approach with hanging maneuver for large intrahepatic cholangiocarcinoma. Surg Endosc 27(12):4732–4733. doi:10.1007/s00464-013-3202-2
Choi SB, Kim KS, Choi JY, Park SW, Choi JS, Lee WJ, Chung JB (2009) The prognosis and survival outcome of intrahepatic cholangiocarcinoma following surgical resection: association of lymph node metastasis and lymph node dissection with survival. Ann Surg Oncol 16(11):3048–3056. doi:10.1245/s10434-009-0631-1
de Jong MC, Nathan H, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H, Pulitano C, Barroso E, Clary BM, Aldrighetti L, Ferrone CR, Zhu AX, Bauer TW, Walters DM, Gamblin TC, Nguyen KT, Turley R, Popescu I, Hubert C, Meyer S, Schulick RD, Choti MA, Gigot JF, Mentha G, Pawlik TM (2011) Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol 29(23):3140–3145. doi:10.1200/JCO.2011.35.6519
Kawarada Y, Yamagiwa K, Das BC (2002) Analysis of the relationships between clinicopathologic factors and survival time in intrahepatic cholangiocarcinoma. Am J Surg 183(6):679–685
Li DY, Zhang HB, Yang N, Quan Y, Yang GS (2013) Routine lymph node dissection may be not suitable for all intrahepatic cholangiocarcinoma patients: results of a monocentric series. World J Gastroenterol 19(47):9084–9091. doi:10.3748/wjg.v19.i47.9084
Kim DH, Choi DW, Choi SH, Heo JS, Kow AW (2015) Is there a role for systematic hepatic pedicle lymphadenectomy in intrahepatic cholangiocarcinoma? A review of 17 years of experience in a tertiary institution. Surgery 157(4):666–675. doi:10.1016/j.surg.2014.11.006
Acknowledgments
We gratefully acknowledge financial support from National R&D Program for Cancer Control, Ministry for Health, Welfare and Family affairs, Republic of Korea, grant number 0820050. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Woohyung Lee, Ji-Ho Park, Ju-Yeon Kim, Seung-Jin Kwag, Taejin Park, Sang-Ho Jeong, Young-Tae Ju, Eun-Jung Jung, Young-Joon Lee, Soon-Chan Hong, Sang-Kyung Choi, and Chi-Young Jeong have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Lee, W., Park, JH., Kim, JY. et al. Comparison of perioperative and oncologic outcomes between open and laparoscopic liver resection for intrahepatic cholangiocarcinoma. Surg Endosc 30, 4835–4840 (2016). https://doi.org/10.1007/s00464-016-4817-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4817-x