Abstract
Background
Palliative surgical oncology patients represent a unique group with complex needs who often require multidisciplinary input for the provision of timely and holistic care. The authors assembled a multi-disciplinary palliative intervention team and evaluated its association with the quality of discussions on goals of care (GOC) among advanced cancer patients undergoing palliative interventions.
Methods
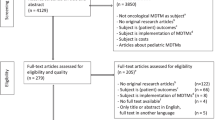
This prospective cohort study analyzed advanced cancer patients undergoing palliative interventions at a single urban academic center from October 2019 to March 2022. In January 2021, a multi-disciplinary palliative surgical intervention (MD-PALS) team was assembled. All palliative surgical oncology patients were discussed at multi-disciplinary meetings and managed by members of the MD-PALS team. An interrupted time series (ITS) model was built to evaluate the association of MD-PALS implementation and the quality of GOC discussions as measured by a consensus-derived four-point GOC discussion quality score.
Results
The study recruited 126 palliative surgical oncology patients: 44 in the pre-MD-PALS group and 82 in the post-MD-PALS group. The two groups did not differ significantly in baseline demographics, treatment, or postoperative and survival outcomes. Compared with the pre-MD-PALS group, the post-MD-PALS group had a significantly higher mean GOC discussion quality score (1.34 vs 2.61; p < 0.001). Based on the ITS model, the average quarterly GOC discussion quality score increased significantly among patients after implementation of the MD-PALS team (change = 1.93; 95 % confidence interval, 0.96–2.90; P = 0.003).
Conclusion
The implementation of an MD-PALS team was associated with improvements in the quality of GOC discussions among palliative surgical oncology patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Advanced cancer is prevalent in an ageing population and accounts for up to 30 % of deaths in many countries.1 In the recent decade, palliative interventions have been increasingly used during end-of-life (EOL) situations for surgical oncology patients to reduce symptoms and improve quality of life (QoL).2,3 However, less than 10 % of surgical patients receive specialist palliative care consultations or have goals-of-care (GOC) discussions within the last year of life.4 Furthermore, advanced cancer patients often are faced with complex oncologic issues due to the interplay of systemic, locoregional treatment options and disease biology, complicating decision-making processes near EOL.
Although an inter-disciplinary approach with conventional tumor boards involving surgical, medical, and radiation oncologists represents the standard of care in the management of routine surgical oncology patients, it may be suboptimal in the setting of palliative surgical oncology.5,6 Palliative patients often are plagued with unique EOL issues such as symptom control, emotional distress, social support, and spirituality issues.7,8
To address this uniquely vulnerable population, we established a multi-disciplinary palliative surgical intervention (MD-PALS) team comprising specialist palliative care physicians, surgical oncologists, medical and radiation oncologists, gastroenterologists, nutritionists, interventional radiologists, rehabilitation physicians, psychiatrists, psychologists, and medical social workers. We hypothesized that the diversity and experience of MD-PALS members can facilitate and improve care delivery for palliative surgical oncology patients with complex EOL needs. In this study, we aimed to evaluate the relationship between the implementation of MD-PALS and the quality of GOC discussions among advanced cancer patients and their families during surgical admissions.
Methods
Study Design and Population
We performed a single-center prospective cohort study of advanced cancer patients who received palliative interventions (i.e., surgery, endoscopic or interventional radiologic procedures) at the Division of Surgery and Surgical Oncology of the Singapore General Hospital between October 2019 and March 2022. This study was approved by the SingHealth Centralized Institutional Review Board, and informed consent obtained before enrolment of patients.
Intervention: MD-PALS Team
The MD-PALS team, assembled in January 2021, included members from surgical oncology, medical and radiation oncology, palliative care physicians, gastroenterologists, interventional radiologists, advanced practice and specialty nurses, nutritionists, psychologists, and medical social workers. Fortnightly meetings were held by the MD-PALS team to discuss all patients receiving palliative interventions from January 2021 onward. Before assembly of the MD-PALS team, specialist consultations from the respective members of the group were requested on an ad hoc basis by the primary team caring for the patient.
Advanced cancer patients who received palliative interventions between October 2019 and December 2020 were in the pre-MD-PALS group, whereas those admitted between January 2021 and March 2022 were in the post-MD-PALS group.
Outcome Measure: Quality of Discussions on GOC
The primary outcome of the study was the quality of GOC discussions, which was measured using a four-point composite score as follows: 1 (intent and expected benefits and morbidities associated with palliative surgery or other interventions), 2 (conveyance of overall prognosis), 3 (consideration of patients’ priorities and goals of treatment), 4 (determination of code status). A score of 0 or 1 was assigned if the aforementioned components were respectively absent or present from clinical documentation, with a maximum possible GOC discussion quality score of 4 points. These components were reviewed and considered essential in GOC discussions during a consensus meeting held among the MD-PALS team members. Communication documentation review was performed by two physicians (J.J.Y.S. and J.S.M.W.) independently, and conflicts were resolved by a third senior author (C.S.M.C.).
We also reviewed the number of consultations by specialist palliative care physicians and other members of the MD-PALS team during each patient’s index surgical admission for palliative intervention.
Other Study Covariates
Data on patient demographics, tumor characteristics, palliative interventions, postoperative or postprocedural complications, length of index admission, systemic chemotherapy or radiotherapy, and hospital readmission were collected via manual chart review of electronic medical records at the index surgical admission for palliative intervention.9
Statistical Analysis
Continuous characteristics were compared using the two-sample t test, whereas categorical characteristics were compared using Fisher’s exact test. Overall survival (OS) was measured from the date of palliative intervention to the date of death. Alive patients were censored as of 11 August 2022, when data were cut off for analysis, and no patients were lost to follow-up evaluation.
The Kaplan-Meier method was used to estimate OS distribution, and the log-rank test was used to compare OS between the two patient groups. Because the longer follow-up duration among the pre-MD-MPALS patients could distort the OS comparison, a sensitivity analysis was performed in which the OS duration of all patients who survived beyond 12 months was censored at 12 months.
Mean GOC discussion quality scores between the pre- and post-MD-PALS groups were compared using the two-sample t test, with additional adjustments made for age, Eastern Cooperative Oncology Group (ECOG) performance status, and whether the patient underwent palliative surgery using analysis of covariance. A segmented linear regression model was fitted to evaluate the change in the level and trend of the average quarterly GOC discussion quality score after MD-PALS implementation. Diagnostic checks of the fitted model were performed to ensure that all model assumptions were met.
To evaluate the robustness of the results from this interrupted time series (ITS) analysis, a sensitivity analysis based on segmented beta regression of the mean proportion of quality components of GOC discussions achieved by the patients was performed.
Exploratory subgroup analyses were performed to examine the differences in GOC discussion quality scores between the pre- and post-MD-PALS groups by type of palliative interventions using logistic regression. Firth’s penalized likelihood estimation method was used for covariates with a complete separation issue. Goodness of fit was assessed based on the Hosmer-Lemeshow test.
All statistical tests were two-sided with a 5 % significance level. Analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) and Stata 16.1 (StataCorp, College Station, TX, USA).
Results
The study enrolled 44 (34.9 %) patients in the pre-MD-PALS group and 82 (65.1 %) patients in the post-MD-PALS group. The median follow-up period was 27.1 months in the pre-MD-PALS group and 10.6 months in the post-MD-PALS groups. The two groups did not differ significantly in terms of clinical and demographic characteristics (Table 1). The most common indication for consideration of palliative interventions was intestinal obstruction. After intervention, the pre- and post-MD-PALS groups did not differ significantly in hospital readmissions (50.0 % vs 47.6 %; P = 0.853), and the median overall survival (OS) durations were respectively 9.2 and 5.8 months (P = 0.410).
The mean GOC discussion quality score was significantly higher in the post-MD-PALS group than in the pre-MD-PALS group (1.34 vs 2.64; P < 0.001; Table 2). After adjustment for age, ECOG performance status, and whether the patients received palliative surgery, the mean GOC discussion scores remained significantly higher in the pre-MD-PALS group than in the post-MD-PALS group (1.34 vs 2.61; P ≤ 0.001). The proportion of patients who received quality discussions on goals of surgery, prognosis, priorities and preferences of treatment options, and code status increased significantly after MD-PALS implementation (all P < 0.05; Table 3). Subgroup analysis of GOC discussion quality scores by palliative intervention types did not show differences for the patients who underwent surgical, endoscopic, or radiologic interventions (Table S2).
The interrupted time series (ITS) analysis showed a significant increase in the average quarterly GOC discussions quality score by 1.93 points (95 % conficence interval [CI], 0.96–2.90; P = 0.003) after MD-PALS implementation (Fig. 1). The trend of the average quarterly GOC discussions quality score however remained the same as that during the pre-MD-PALS era. The conclusions on the changes in the level and trend of the average GOC discussions quality score after MD-PALS implementation based on the sensitivity ITS analysis were similar to those of the original ITS analysis. Details of this sensitivity ITS analysis are presented in Fig. S1 and Table S1.
A higher proportion of the post-MD-PALS patients than the pre-MD-PALS patients had specialist palliative care consultations (41.5 % vs 31.8 %; P = 0.339) and inputs from the various members of the multi-disciplinary teams (84.1 % vs 81.8 %; P = 0.804) during their index admission for palliative interventions, although these differences did not reach statistical significance (Table 4).
Discussion
Overall, findings from our study suggest that the implementation of a multi-disciplinary palliative intervention team (MD-PALS) and the involvement of the various specialist providers in the care of palliative surgical oncology patients improved one aspect of palliative care delivery: the quality of GOC discussions conducted. This may be attributable to increased collaboration and a ready exchange of clinical information as a result of the MD-PALS platform. The primary surgical oncologist, informed by MD-PALS members, can now better identify key EOL issues surrounding the palliative surgical patient and is well-placed to conduct quality GOC discussion during a surgical admission.
In previous efforts to improve the quality of GOC discussions, investigators have evaluated the use of didactic lectures, one-on-one training, or even role-playing with standardized patients.10,11,12,13,14,15 Although these are important in equipping clinicians with the skills necessary to conduct GOC discussions, their effectiveness may be limited by varying levels of proficiency among the members of a multidisciplinary team and differences in opinions regarding the most goal-concordant management plan. In our anecdotal experience, it is not uncommon for patients to have encounters with various members of the multidisciplinary team, with a resulting lack of clarity in terms of their GOC and management plan. Therefore, the MD-PALS team was formed at our institution to build a “Community of Practice” aimed at improving palliative care processes, enhancing interdisciplinary collaboration, and streamlining communication with patients and their families.16
Increased involvement of specialist palliative care physicians in the care of palliative surgical oncology patients during the post-MDPALS era (31.8 % vs 41.5 %) also likely contributed to the improvements in the quality of GOC discussions. A randomized controlled trial by Vanbutsele et al.17 demonstrated that early and systematic integration of palliative care improves the quality of life and is more beneficial for patients with advanced cancer than palliative care consultations offered on demand. The authors concluded that the results may be attributable to the different focus of treatment offered by the palliative team compared with the oncology team. In our experience, the specialist palliative care team at our institution contributed significantly in terms of integrating the recommendations of MD-PALS and facilitating the GOC discussions with the patients and families.
The current study was limited by the relatively small sample and the unequal cohort sizes of the pre- and post-MD-PALS groups. We hypothesized that the smaller pre-MD-PALS cohort was likely due to changes in workflows and elective hospital admissions during the COVID-19 pandemic.18,19,20,21 Because the pre-MDPALS era coincided with the outbreak of COVID-19 in Singapore, the lower proportion of patients and families receiving GOC discussions also may be explained by isolation and visiting policies. In addition, there is no existing international consensus on what constitutes quality GOC discussions, and our MD-PALS consensus definition of the four essential GOC components informed by literature and our local clinical experience may limit the generalizability of this study.22,23,24
In conclusion, the implementation of an MD-PALS team improved the quality of GOC discussions among palliative surgical oncology patients. These findings provide an opportunity and direction for future studies on improving the quality of palliative care of advanced cancer patients.
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Chen VW, Portuondo JI, Cooper Z, Massarweh NN. Use of palliative interventions at end of life for advanced gastrointestinal cancer. Ann Surg Oncol. 2022;29:7281–92. https://doi.org/10.1245/s10434-022-12342-1.
Wong JSM, Ng IAT, Juan WKD, et al. Trajectories of patient-reported outcomes after palliative gastrointestinal surgery in advanced cancer: is good quality of life sustainable? Ann Surg Open. 2022;3:e206. https://doi.org/10.1097/AS9.0000000000000206.
Roeland EJ, Triplett DP, Matsuno RK, et al. Patterns of palliative care consultation among elderly patients with cancer. J Natl Compr Canc Netw. 2016;14:439–45. https://doi.org/10.6004/jnccn.2016.0050.
Lamb B, Green JSA, Vincent C, Sevdalis N. Decision-making in surgical oncology. Surg Oncol. 2011;20:163–8. https://doi.org/10.1016/j.suronc.2010.07.007.
Hanna NN, Bellavance E, Keay T. Palliative surgical oncology. Surg Clin North Am. 2011;91:343–53. https://doi.org/10.1016/j.suc.2010.12.004.
Buss MK, Rock LK, McCarthy EP. Understanding palliative care and hospice. Mayo Clinic Proc. 2017;92:280–6. https://doi.org/10.1016/j.mayocp.2016.11.007.
Kemp C. Cultural issues in palliative care. Semin Oncol Nursing. 2005;21:44–52. https://doi.org/10.1053/j.soncn.2004.10.007.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Lilly CM, De Meo DL, Sonna LA, et al. An intensive communication intervention for the critically ill. Am J Med. 2000;109:469–75. https://doi.org/10.1016/S0002-9343(00)00524-6.
Alexander SC, Keitz SA, Sloane R, Tulsky JA. A controlled trial of a short course to improve residents’ communication with patients at the end of life. Acad Med. 2006;81:1008–12. https://doi.org/10.1097/01.ACM.0000242580.83851.ad.
Back AL. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167:453. https://doi.org/10.1001/archinte.167.5.453.
Wilkinson S, Perry R, Blanchard K, Linsell L. Effectiveness of a three-day communication skills course in changing nurses’ communication skills with cancer/palliative care patients: a randomised controlled trial. Palliat Med. 2008;22:365–75. https://doi.org/10.1177/0269216308090770.
Curtis JR, Back AL, Ford DW, et al. Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA. 2013;310:2271. https://doi.org/10.1001/jama.2013.282081.
Brighton LJ, Koffman J, Hawkins A, et al. A systematic review of end-of-life care communication skills training for generalist palliative care providers: research quality and reporting guidance. J Pain Symptom Manage. 2017;54:417–25. https://doi.org/10.1016/j.jpainsymman.2017.04.008.
Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge University Press, Cambridge, England, 1991.
Vanbutsele G, Pardon K, Van Belle S, et al. Effect of early and systematic integration of palliative care in patients with advanced cancer: a randomised controlled trial. Lancet Oncol. 2018;19:394–404. https://doi.org/10.1016/S1470-2045(18)30060-3.
Cahalane AM, Cui J, Sheridan RM, et al. Changes in interventional radiology practice in a tertiary academic center in the United States during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Radiol. 2020;17:873–7. https://doi.org/10.1016/j.jacr.2020.05.005.
Al-Dorzi HM, Aldawood AS, Almatrood A, et al. Managing critical care during COVID-19 pandemic: the experience of an ICU of a tertiary care hospital. J Infect Public Health. 2021;14:1635–41. https://doi.org/10.1016/j.jiph.2021.09.018.
Whelehan DF, Connelly TM, Ridgway PF. COVID-19 and surgery: a thematic analysis of unintended consequences on performance, practice, and surgical training. Surgeon. 2021;19:e20–7. https://doi.org/10.1016/j.surge.2020.07.006.
Brethauer SA, Poulose BK, Needleman BJ, et al. Redesigning a department of surgery during the COVID-19 pandemic. J Gastrointest Surg. 2020;24:1852–9. https://doi.org/10.1007/s11605-020-04608-4.
Lee KC, Walling AM, Senglaub SS, et al. Improving serious illness care for surgical patients: quality indicators for surgical palliative care. Ann Surg. 2022;275:196–202. https://doi.org/10.1097/SLA.0000000000003894.
Lilley EJ, Lindvall C, Lillemoe KD, Tulsky JA, Wiener DC, Cooper Z. Measuring processes of care in palliative surgery: a novel approach using natural language processing. Ann Surg. 2018;267:823–5. https://doi.org/10.1097/SLA.0000000000002579.
Lindvall C, Deng CY, Moseley E, et al. Natural language processing to identify advance care planning documentation in a multisite pragmatic clinical trial. J Pain Symptom Manage. 2022;63:e29–36. https://doi.org/10.1016/j.jpainsymman.2021.06.025.
Acknowledgment
This study was supported by the NCCS Cancer Fund (research) and SingHealth Duke-NUS Academic Medicine Centre, facilitated by the Joint Office of Academic Medicine (JOAM). Wong Si Min Jolene is supported by the National Research Council Clinician Scientist-Individual Research Grant (CIRG21jun-0038). We acknowledge Ms. Sahara Bte Abu Baka, Dr. Qingyuan Zhuang, Dr. Shirlyn Hui Shan Neo, Dr. Jamie Xuelian Zhou, Dr. Wah Ying Ong, Dr. Grace Meijuan Yang, Dr. Shirlynn Ho, Dr. Mark Chang Chuen Cheah, Dr. Too Chow Wei, Dr. Apoorva Gogna, Dr. Leong Sum, Dr. Sivanathan Chandramohan, Dr. Christopher Khor Jen Lock, Dr. Damien Tan Meng Yew, Dr. Clement Wu Chun Ho, Dr. Daniel Quah Song Chiek, Dr. Ramalingam Mothi Babu, Dr. Jack Junjie Chan, Dr. Matthew Chau Hsien Ng, Dr. Lee Suat Ying, and Dr. Shuting Han for their contributions as team members of MD-PALS and for their various contributions to this report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Soon, J.J.Y., Juan, D.W.K., Ong, W.S. et al. Implementation of a Multi-Disciplinary Team and Quality of Goals of Care Discussions in Palliative Surgical Oncology Patients. Ann Surg Oncol 30, 8054–8060 (2023). https://doi.org/10.1245/s10434-023-14190-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14190-z