Abstract
Background
The influence of morphological status on the long-term outcome of patients undergoing liver resection for intrahepatic cholangiocarcinoma (ICC) is poorly defined. We sought to study the impact of morphological status on overall survival (OS) of patients undergoing curative-intent resection for ICC.
Methods
A total of 1083 patients who underwent liver resection for ICC between 1990 and 2015 were identified. Data on clinicopathological characteristics, operative details, and morphological status were recorded and analyzed. A propensity score-matched analysis was performed to reduce confounding biases.
Results
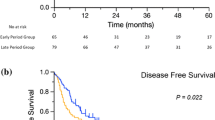
Among 1083 patients, 941(86.9%) had a mass-forming (MF) or intraductal-growth (IG) type, while 142 (13.1%) had a periductal-infiltrating (PI) or MF with PI components (MF + PI) ICC. Patients with an MF/IG ICC had a 5-year OS of 41.8% (95% confidence interval [CI] 37.7–45.9) compared with 25.5% (95% CI 17.3–34.4) for patients with a PI/MF + PI (p < 0.001). Morphological type was found to be an independent predictor of OS as patients with a PI/MF + PI ICC had a higher hazard of death (hazard ratio [HR] 1.42, 95% CI 1.11–1.82; p = 0.006) compared with patients who had an MF/IG ICC. Compared with T1a–T1b–T2 MF/IG tumors, T1a–T1b–T2 PI/MF + PI and T3–T4 PI/MF + PI tumors were associated with an increased risk of death (HR 1.47 vs. 3.59). Conversely, patients with T3–T4 MF/IG tumors had a similar risk of death compared with T1a–T1b–T2 MF/IG patients (p = 0.95).
Conclusion
Among patients undergoing curative-intent resection of ICC, morphological status was a predictor of long-term outcome. Patients with PI or MF + PI ICC had an approximately 45% increased risk of death long-term compared with patients who had an MF or IG ICC.


Similar content being viewed by others
References
Liver Cancer Study Group of Japan. Intrahepatic cholangiocarcinoma macroscopic typing. In: Okamoto E (ed). Classification of primary liver cancer. Tokyo, Japan, Kanehara; 1997. pp 6–7.
Dodson RM, Weiss MJ, Cosgrove D, et al. Intrahepatic cholangiocarcinoma: management options and emerging therapies. Journal of the American College of Surgeons. 2013;217(4):736–50.
Amini N, Ejaz A, Spolverato G, Kim Y, Herman JM, Pawlik TM. Temporal trends in liver-directed therapy of patients with intrahepatic cholangiocarcinoma in the United States: a population-based analysis. Journal of Surgical Oncology. 2014;110(2):163–70.
de Jong MC, Nathan H, Sotiropoulos GC, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. Journal of Clinical Oncology. 2011;29(23):3140–45.
Hyder O, Hatzaras I, Sotiropoulos GC, et al. Recurrence after operative management of intrahepatic cholangiocarcinoma. Surgery. 2013;153(6):811–18.
Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surgery. 2014;149(6):565–74.
Nathan H, Aloia TA, Vauthey JN, et al. A proposed staging system for intrahepatic cholangiocarcinoma. Annals of Surgical Oncology. 2009;16(1):14–22.
Nathan H, Pawlik TM. Staging of intrahepatic cholangiocarcinoma. Current Opinion in Gastroenterology. 2010;26(3):269–73.
Spolverato G, Ejaz A, Kim Y, et al. Tumor size predicts vascular invasion and histologic grade among patients undergoing resection of intrahepatic cholangiocarcinoma. Journal of Gastrointestinal Surgery. 2014;18(7):1284–91.
Spolverato G, Kim Y, Ejaz A, et al. Conditional probability of long-term survival after liver resection for intrahepatic cholangiocarcinoma: a multi-institutional analysis of 535 patients. JAMA Surgery. 2015;150(6):538–45.
Spolverato G, Vitale A, Cucchetti A, et al. Can hepatic resection provide a long-term cure for patients with intrahepatic cholangiocarcinoma? Cancer. 2015;121(22):3998–4006.
de Jong MC, Pulitano C, Ribero D, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Annals of Surgery. 2009;250(3):44–48.
Spolverato G, Yakoob MY, Kim Y, et al. The impact of surgical margin status on long-term outcome after resection for intrahepatic cholangiocarcinoma. Annals of Surgical Oncology. 2015;22(12):4020–28.
Spolverato G, Kim Y, Alexandrescu S, et al. Is hepatic resection for large or multifocal intrahepatic cholangiocarcinoma justified? Results from a multi-institutional collaboration. Annals of Surgical Oncology. 2015;22(7):2218–25.
DeOliveira ML, Cunningham SC, Cameron JL, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Annals of Surgery. 2007;245(5):755–62.
Endo I, Gonen M, Yopp AC, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Annals of Surgery. 2008;248(1):84–96.
Nakagohri T, Kinoshita T, Konishi M, Takahashi S, Gotohda N. Surgical outcome and prognostic factors in intrahepatic cholangiocarcinoma. World Journal of Surgery. 2008;32(12):2675–80.
Bagante F, Gani F, Spolverato G, et al. Intrahepatic cholangiocarcinoma: prognosis of patients who did not undergo lymphadenectomy. Journal of the American College of Surgeons. 2015;221(6):1031–40.
Hatzaras I, Schmidt C, Muscarella P, Melvin WS, Ellison EC, Bloomston M. Elevated CA 19–9 portends poor prognosis in patients undergoing resection of biliary malignancies. HPB (Oxford). 2010;12(2):134–38.
Yamasaki S. Intrahepatic cholangiocarcinoma: macroscopic type and stage classification. Journal of Hepato-Biliary-Pancreatic Surgery. 2003;10(4):288–91.
Shimada K, Sano T, Sakamoto Y, Esaki M, Kosuge T, Ojima H. Surgical outcomes of the mass-forming plus periductal infiltrating types of intrahepatic cholangiocarcinoma: a comparative study with the typical mass-forming type of intrahepatic cholangiocarcinoma. World Journal of Surgery. 2007;31(10):2016–22.
Ohtsuka M, Ito H, Kimura F, et al. Results of surgical treatment for intrahepatic cholangiocarcinoma and clinicopathological factors influencing survival. The British Journal of Surgery. 2002;89(12):1525–31.
Yamamoto M, Takasaki K, Yoshikawa T, Ueno K, Nakano M. Does gross appearance indicate prognosis in intrahepatic cholangiocarcinoma? Journal of Surgical Oncology. 1998;69(3):162–67.
Amin MB EiC, American Joint Committee on Cancer. Springer, New York; 2017.
Austin PC, Grootendorst P, Anderson GM. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Statistics in Medicine. 2007;26(4):734–53.
Hyder O, Marques H, Pulitano C, et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: an Eastern and Western experience. JAMA Surgery. 2014;149(5):432–38.
Guglielmi A, Ruzzenente A, Campagnaro T, et al. Patterns and prognostic significance of lymph node dissection for surgical treatment of perihilar and intrahepatic cholangiocarcinoma. Journal of Gastrointestinal Surgery. 2013;17(11):1917–28.
Guglielmi A, Ruzzenente A, Campagnaro T, et al. Intrahepatic cholangiocarcinoma: prognostic factors after surgical resection. World Journal of Surgery. 2009;33(6):1247–54.
Spolverato G, Bagante F, Weiss, M, Alexandrescu S, Marques HP, Aldrighetti L, et al. Comparative performances of the 7th and the 8th editions of the American Joint Committee on Cancer staging systems for intrahepatic cholangiocarcinoma. Journal of Surgical Oncology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors have no personal conflicts of interest to declare.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bagante, F., Spolverato, G., Weiss, M. et al. Impact of Morphological Status on Long-Term Outcome Among Patients Undergoing Liver Surgery for Intrahepatic Cholangiocarcinoma. Ann Surg Oncol 24, 2491–2501 (2017). https://doi.org/10.1245/s10434-017-5870-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5870-y