Abstract
Background
As many as 40 % of breast cancer patients undergoing axillary lymph node dissection (ALND) and radiotherapy develop lymphedema. We report our experience performing lymphatic–venous anastomosis using the lymphatic microsurgical preventive healing approach (LYMPHA) at the time of ALND. This technique was described by Boccardo, Campisi in 2009.
Methods
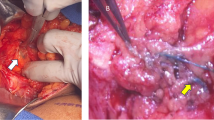
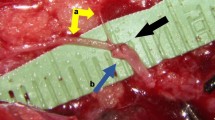
LYMPHA was offered to node-positive women with breast cancer requiring ALND. Afferent lymphatic vessels, identified by injection of blue dye in the ipsilateral arm, were sutured into a branch of the axillary vein distal to a competent valve. Follow-up was with pre- and postoperative lymphoscintigraphy, arm measurements, and (L-Dex®) bioimpedance spectroscopy.
Results
Over 26 months, 37 women underwent attempted LYMPHA, with successful completion in 27. Unsuccessful attempts were due to lack of a suitable vein (n = 3) and lymphatic (n = 5) or extensive axillary disease (n = 1). There were no LYMPHA-related complications. Mean follow-up time was 6 months (range 3–24 months). Among completed patients, 10 (37 %) had a body mass index of ≥30 kg/m2 (mean 27.9 ± 6.8 kg/m2, range 17.4–47.6 kg/m2), and 17 (63 %) received axillary radiotherapy. Excluding two patients with preoperative lymphedema and those with less than 3-month follow-up, the lymphedema rate was 3 (12.5 %) of 24 in successfully completed and 4 (50 %) of 8 in unsuccessfully treated patients.
Conclusions
Our transient lymphedema rate in this high-risk cohort of patients was 12.5 %. Early data show that LYMPHA is feasible, safe, and effective for the primary prevention of breast cancer-related lymphedema.



Similar content being viewed by others
References
Wilke L, McCall L, Posther K, et al. Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Ann Surg Oncol. 2006;13:491–500.
Giuliano A, Hunt K, Ballman K, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis. JAMA. 2011;305:569–75.
Fleissig A, Fallowfiel L, Langridge C, et al. Postoperative arm morbidity and quality of life: results of the ALMANAC randomized trial comparing sentinel node biopsy with standard axillary treatment in the management of patients with early breast cancer. Breast Cancer Res Treat. 2006;95:279–93.
Veronesi U, Paganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003;349:546–53.
Mansel R, Fallowfield L, Kissin M, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC trial. J Natl Cancer Inst. 2006;98:599–609.
McLaughlin S, Wright M, Morris K, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: patient perceptions and precautionary behaviors. J Clin Oncol. 2008;26:5220–6.
Boughey J, Suman V, Mittendorf E, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer. JAMA. 2013;310:1455–61.
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet. 2013;14:500–15.
Hayes S, Johansson K, Stout N, et al. Upper-body morbidity after breast cancer. Cancer. 2012;118:2237–49.
Hayes S, Disipio T, Rye S, et al. Prevalence and prognostic significance of secondary lymphedema following breast cancer. Lymphat Res Biol. 2011;9:135–41.
Chang D, Feigenberg S, Indelicato D, et al. Long-term outcomes in breast cancer patients with ten or more positive axillary nodes treated with combined-modality therapy: the importance of radiation field selection. Int J Radiat Biol Phys. 2007;67:1043–51.
Warren L, Miller C, Horick N, et al. The impact of radiation therapy on the risk of lymphedema after treatment for breast cancer: a prospective cohort study. Int J Radiat Oncol Biol Phys. 2014;88:565–71.
Ridner S, Dietrich M, Stewart B, Armer J. Body mass index and breast cancer treatment-related lymphedema. Support Care Cancer.2011;19:853–7.
Helyer L, Varnic M, Le L, Leong W, McCready D. Obesity is a risk factor for developing postoperative lymphedema in breast cancer patients. Breast J. 2010;16:48–54.
Vignes S, Porcher R, Arrault M, Dupuy A. Long-term management of breast cancer–related lymphedema after intensive decongestive physiotherapy. Breast Cancer Res Treat. 2007;101:285–90.
Pasket E, Dean J, Oliveri J, Harrop J. Cancer-related lymphedema risk factors, diagnosis, treatment, and impact. J Clin Oncol. 2012;30:3726–33.
Yah-Chen T, Ying Xu J, Cormier S, et al. Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol. 2009;27:2007–14.
Pronin V, Adamian A, Zolotarevsky V, Rozanov Y, Savchenko T, Akimov A. Lymphovenous anastamosis for the prevention of a post-mastectomy edema of the arm. Sov Med. 1989;4:32–35.
Pronin V, Adamian A, Zolotarevsky V, Rozanov J, Savchenko T, Akimov A. Lymphovenous anastamosis formation at an early stage after radical mastectomy. Sov Med. 1989;8:77–9.
Casabona F, Bogliolo S, Menada M, Sala P, Villa G, Ferrero S. Feasibility of axillary reverse mapping during sentinel lymph node biopsy in breast cancer patients. Ann Surg Oncol. 2009;16:2459–63.
Stanton A, Modi S, Britton T, et al. Lymphatic drainage in the muscle and subcutis of the arm after breast cancer treatment. Breast Cancer Res Treat. 2009;117:549–57.
Thompson M, Korourian S, Henry-Tillman R, et al. Axillary reverse mapping (ARM): a new concept to identify and enhance lymphatic preservation. Ann Surg Oncol. 2007;14:1890–5.
Ochoa D, Korourian S, Boneti C, Adkins L, Badgwell B, Klimberg S. Axillary reverse mapping: five-year experience. Surgery. 2014;156:1261–8.
Boccardo F, Casabona F, De Cian F, et al. Lymphedema microsurgical preventive healing approach: a new technique for primary prevention of arm lymphedema after mastectomy. Ann Surg Oncol. 2009;16:703–8.
Boccardo F, Casabona F, Friedman D, et al. Surgical prevention of arm lymphedema after breast cancer treatment. Ann Surg Oncol. 2011;18:2500–5.
Boccardo F, Casabona F, DeCian F, et al. Lymphatic microsurgical preventing healing approach (LYMPHA) for primary surgical prevention of breast cancer–related lymphedema: over 4 year follow up. Microsurgery. 2014;34:421–4.
Kleinhans E, Baumeister R, Hahn D, Siuda S, Bull U, Moser E. Evaluation of transport kinetics in lymphoscintigraphy: follow-up study in patients with transplanted lymphatic vessels. Eur J Nucl Med. 1985;10:349–52.
Blaney J, McCollum G, Lorimer J, Bradley J, Kennedy R, Rankin J. Prospective surveillance of breast cancer-related lymphedema in the first-year post-surgery: feasibility and comparison of screening measures. Support Care Cancer. 2015;23(6):1549–59.
Lee M, Beith J, Ward L, Kilbreath S. Lymphedema following taxane-based chemotherapy in women with early breast cancer. Lymphat Res Biol. 2014;12:282–8.
Kilbreath S, Lee M, Refshauge K, et al. Transient swelling versus lymphoedema following surgery for breast cancer. Support Care Cancer. 2013;21:2207–15.
Norman S, Localio R, Potashnik S, et al. Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol. 2009;27:390–7.
Norman S, Miller L, Erikson H, Norman M, McCorkle R. Development and validation of a telephone questionnaire to characterize lymphedema in women treated for breast cancer. Phys Ther. 2001;81:1192–205.
Acknowledgments
Supported in part by a Columbia University Department of Surgery Start-up Award. We wish to thank Francesco Boccardo, Coradino Campisi, and the staff of the IRCCS Università Ospedale San Martino–IST Istituto Nazionale per la Ricerca sul Cancro, Department of Surgery, Operative Unit of Lymphatic Surgery, and Section of Lymphology, Lymphatic Surgery, and Microsurgery, Genoa, Italy, for their mentorship and collaboration, which has been instrumental in helping to advance the LYMPHA method at Columbia University Medical Center.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feldman, S., Bansil, H., Ascherman, J. et al. Single Institution Experience with Lymphatic Microsurgical Preventive Healing Approach (LYMPHA) for the Primary Prevention of Lymphedema. Ann Surg Oncol 22, 3296–3301 (2015). https://doi.org/10.1245/s10434-015-4721-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4721-y