Abstract
Purpose of Review
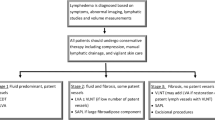
Lymphedema is a chronic limb swelling caused by lymphatic dysfunction and is currently incurable. Breast cancer–related lymphedema (BCRL) affects up to 5 million Americans and occurs in one-third of breast cancer survivors following axillary lymph node dissection. Compression remains the mainstay of therapy. Surgical management of BCRL includes excisional procedures to remove excess tissue and physiologic procedures to attempt to improve fluid retention in the limb. The purpose of this review is to highlight surgical management strategies for preventing and treating breast cancer–related lymphedema.
Recent Findings
Immediate lymphatic reconstruction (ILR) is a microsurgical technique that anastomoses disrupted axillary lymphatic vessels to nearby veins at the time of axillary lymph node dissection (ALND) and has been reported to reduce lymphedema rates from 30 to 4–12%.
Summary
Postsurgical lymphedema remains incurable. Surgical management of lymphedema includes excisional procedures and physiologic procedures using microsurgical technique. Immediate lymphatic reconstruction has emerged as a prophylactic strategy to prevent lymphedema in breast cancer patients.


Similar content being viewed by others
References
Azhar SH, Lim HY, Tan BK, Angeli V. The unresolved pathophysiology of lymphedema. Front Physiol. 2020;11:137. https://doi.org/10.3389/fphys.2020.00137.
Schulze H, Nacke M, Gutenbrunner C, Hadamitzky C. Worldwide assessment of healthcare personnel dealing with lymphoedema. Health Econ Rev. 2018;8(1):10. https://doi.org/10.1186/s13561-018-0194-6.
Beaulac SM, McNair LA, Scott TE, LaMorte WW, Kavanah MT. Lymphedema and quality of life in survivors of early-stage breast cancer. Arch Surg. 2002;137(11):1253–7. https://doi.org/10.1001/archsurg.137.11.1253.
Bundred N, Foden P, Todd C, Morris J, Watterson D, Purushotham A, et al. Increases in arm volume predict lymphoedema and quality of life deficits after axillary surgery: a prospective cohort study. Br J Cancer. 2020;123(1):17–25. https://doi.org/10.1038/s41416-020-0844-4.
Chang SB, Askew RL, Xing Y, Weaver S, Gershenwald JE, Lee JE, et al. Prospective assessment of postoperative complications and associated costs following inguinal lymph node dissection (ILND) in melanoma patients. Ann Surg Oncol. 2010;17(10):2764–72. https://doi.org/10.1245/s10434-010-1026-z.
Norman SA, Localio AR, Kallan MJ, Weber AL, Torpey HA, Potashnik SL, et al. Risk factors for lymphedema after breast cancer treatment. Cancer Epidemiol Biomarkers Prev. 2010;19(11):2734–46. https://doi.org/10.1158/1055-9965.EPI-09-1245.
Shaitelman SF, Cromwell KD, Rasmussen JC, Stout NL, Armer JM, Lasinski BB, Cormier JN. Recent progress in the treatment and prevention of cancer-related lymphedema. CA Cancer J Clin. 2015;65(1):55–81. https://doi.org/10.3322/caac.21253.
Schook CC, Mulliken JB, Fishman SJ, Grant FD, Zurakowski D, Greene AK. Primary lymphedema: clinical features and management in 138 pediatric patients. Plast Reconstr Surg. 2011;127(6):2419–31. https://doi.org/10.1097/PRS.0b013e318213a218.
Smeltzer DM, Stickler GB, Schirger A. Primary lymphedema in children and adolescents: a follow-up study and review. Pediatrics. 1985;76(2):206–18.
Johnson AR, Kimball S, Epstein S, Recht A, Lin SJ, Lee BT, et al. Lymphedema incidence after axillary lymph node dissection: quantifying the impact of radiation and the lymphatic microsurgical preventive healing approach. Ann Plast Surg. 2019;82(4S Suppl 3):S234–s41. https://doi.org/10.1097/sap.0000000000001864.
van der Putte SC, van Limborgh J. The embryonic development of the main lymphatics in man. Acta Morphol Neerl Scand. 1980;18(4):323–35.
Yang Y, Oliver G. Development of the mammalian lymphatic vasculature. J Clin Invest. 2014;124(3):888–97. https://doi.org/10.1172/JCI71609.
International Society of L. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology. Lymphology. 2013;46(1):1–11.
Key TJ, Verkasalo PK, Banks E. Epidemiology of breast cancer. Lancet Oncol. 2001;2(3):133–40. https://doi.org/10.1016/S1470-2045(00)00254-0.
Tao Z, Shi A, Lu C, Song T, Zhang Z, Zhao J. Breast cancer: epidemiology and etiology. Cell Biochem Biophys. 2015;72(2):333–8. https://doi.org/10.1007/s12013-014-0459-6.
American Cancer Society: Cancer Research News Cancer Updates. https://www.cancer.org/research/acs-research-news.html?tag=content-type:cancer-updates (2024). Accessed 22 January 2024.
Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N Y Acad Sci. 2008;1131:147–54. https://doi.org/10.1196/annals.1413.014.
Hayes SC, Johansson K, Stout NL, Prosnitz R, Armer JM, Gabram S, Schmitz KH. Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. 2012;118(8 Suppl):2237–49. https://doi.org/10.1002/cncr.27467.
Fisher CS, Margenthaler JA, Hunt KK, Schwartz T. The Landmark Series: Axillary Management in Breast Cancer. Ann Surg Oncol. 2020;27(3):724–9. https://doi.org/10.1245/s10434-019-08154-5.
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318(10):918–26. https://doi.org/10.1001/jama.2017.11470.
Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15(12):1303–10. https://doi.org/10.1016/S1470-2045(14)70460-7.
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11(10):927–33. https://doi.org/10.1016/S1470-2045(10)70207-2.
Veronesi U, Viale G, Paganelli G, Zurrida S, Luini A, Galimberti V, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg. 2010;251(4):595–600. https://doi.org/10.1097/SLA.0b013e3181c0e92a.
Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, Dhingra K, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17(2):460–9. https://doi.org/10.1200/JCO.1999.17.2.460.
Ueno NT, Buzdar AU, Singletary SE, Ames FC, McNeese MD, Holmes FA, et al. Combined-modality treatment of inflammatory breast carcinoma: twenty years of experience at M. D. Anderson Cancer Center. Cancer Chemother Pharmacol. 1997;40(4):321–9. https://doi.org/10.1007/s002800050664.
Boccardo F, Casabona F, De Cian F, Friedman D, Murelli F, Puglisi M, et al. Lymphatic microsurgical preventing healing approach (LYMPHA) for primary surgical prevention of breast cancer-related lymphedema: over 4 years follow-up. Microsurgery. 2014;34(6):421–4. https://doi.org/10.1002/micr.22254.
Cohen SR, Payne DK, Tunkel RS. Lymphedema: strategies for management. Cancer. 2001;92(4 Suppl):980–7. https://doi.org/10.1002/1097-0142(20010815)92:4+<980::aid-cncr1410>3.0.co;2-e.
Petrek JA, Senie RT, Peters M, Rosen PP. Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer. 2001;92(6):1368–77. https://doi.org/10.1002/1097-0142(20010915)92:6<1368::aid-cncr1459>3.0.co;2-9.
Rodriguez JR, Hsieh F, Huang CT, Tsai TJ, Chen C, Cheng MH. Clinical features, microbiological epidemiology and recommendations for management of cellulitis in extremity lymphedema. J Surg Oncol. 2020;121(1):25–36. https://doi.org/10.1002/jso.25525.
Brorson H, Ohlin K, Olsson G, Karlsson MK. Breast cancer-related chronic arm lymphedema is associated with excess adipose and muscle tissue. Lymphat Res Biol. 2009;7(1):3–10. https://doi.org/10.1089/lrb.2008.1022.
Goss JA, Greene AK. Sensitivity and specificity of the Stemmer sign for lymphedema: a clinical lymphoscintigraphic study. Plast Reconstr Surg Glob Open. 2019;7(6):e2295. https://doi.org/10.1097/GOX.0000000000002295.
Ridner SH, Dietrich MS, Stewart BR, Armer JM. Body mass index and breast cancer treatment-related lymphedema. Support Care Cancer. 2011;19(6):853–7. https://doi.org/10.1007/s00520-011-1089-9.
Greene AK, Zurakowski D, Goss JA. Body mass index and lymphedema morbidity: comparison of obese versus normal-weight patients. Plast Reconstr Surg. 2020;146(2):402–7. https://doi.org/10.1097/PRS.0000000000007021.
Hassanein AH, Maclellan RA, Grant FD, Greene AK. Diagnostic accuracy of lymphoscintigraphy for lymphedema and analysis of false-negative tests. Plast Reconstr Surg Glob Open. 2017;5(7):e1396. https://doi.org/10.1097/GOX.0000000000001396.
Maclellan RA, Zurakowski D, Voss S, Greene AK. Correlation between lymphedema disease severity and lymphoscintigraphic findings: a clinical-radiologic study. J Am Coll Surg. 2017;225(3):366–70. https://doi.org/10.1016/j.jamcollsurg.2017.06.005.
Gloviczki P, Calcagno D, Schirger A, Pairolero PC, Cherry KJ, Hallett JW, Wahner HW. Noninvasive evaluation of the swollen extremity: experiences with 190 lymphoscintigraphic examinations. J Vasc Surg. 1989;9(5):683–9; discussion 90. https://doi.org/10.1067/mva.1989.vs0090683.
Szuba A, Shin WS, Strauss HW, Rockson S. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med. 2003;44(1):43–57.
Executive Committee of the International Society of L. The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology. 2020;53(1):3–19.
Sander AP, Hajer NM, Hemenway K, Miller AC. Upper-extremity volume measurements in women with lymphedema: a comparison of measurements obtained via water displacement with geometrically determined volume. Phys Ther. 2002;82(12):1201–12.
Sitzia J. Volume measurement in lymphoedema treatment: examination of formulae. Eur J Cancer Care (Engl). 1995;4(1):11–6. https://doi.org/10.1111/j.1365-2354.1995.tb00047.x.
Warren AG, Janz BA, Slavin SA, Borud LJ. The use of bioimpedance analysis to evaluate lymphedema. Ann Plast Surg. 2007;58(5):541–3. https://doi.org/10.1097/01.sap.0000244977.84130.cf.
Ridner SH, Montgomery LD, Hepworth JT, Stewart BR, Armer JM. Comparison of upper limb volume measurement techniques and arm symptoms between healthy volunteers and individuals with known lymphedema. Lymphology. 2007;40(1):35–46.
Keeley V. The early detection of breast cancer treatment-related lymphedema of the arm. Lymphat Res Biol. 2021;19(1):51–5. https://doi.org/10.1089/lrb.2020.0097.
Landau MJ, Kim JS, Gould DJ, Patel KM. Vectra 3D imaging for quantitative volumetric analysis of the upper limb: a feasibility study for tracking outcomes of lymphedema treatment. Plast Reconstr Surg. 2018;141(1):80e–4e. https://doi.org/10.1097/PRS.0000000000003912.
Maclellan RA, Greene AK. Lymphedema. Semin Pediatr Surg. 2014;23(4):191–7. https://doi.org/10.1053/j.sempedsurg.2014.07.004.
Johansson K, Lie E, Ekdahl C, Lindfeldt J. A randomized study comparing manual lymph drainage with sequential pneumatic compression for treatment of postoperative arm lymphedema. Lymphology. 1998;31(2):56–64.
Carl HM, Walia G, Bello R, Clarke-Pearson E, Hassanein AH, Cho B, et al. Systematic Review of the Surgical Treatment of Extremity Lymphedema. J Reconstr Microsurg. 2017;33(6):412–25. https://doi.org/10.1055/s-0037-1599100.
Chang DW, Masia J, Garza R 3rd, Skoracki R, Neligan PC. Lymphedema: surgical and medical therapy. Plast Reconstr Surg. 2016;138(3 Suppl):209S–18S. https://doi.org/10.1097/PRS.0000000000002683.
Greene AK, Sudduth CL, Taghinia A. Lymphedema (seminars in pediatric surgery). Semin Pediatr Surg. 2020;29(5):150972. https://doi.org/10.1016/j.sempedsurg.2020.150972.
Hoffner M, Ohlin K, Svensson B, Manjer J, Hansson E, Troeng T, Brorson H. liposuction gives complete reduction of arm lymphedema following breast cancer treatment-a 5-year prospective study in 105 patients without recurrence. Plast Reconstr Surg Glob Open. 2018;6(8):e1912. https://doi.org/10.1097/GOX.0000000000001912.
Schaverien MV, Munnoch DA, Brorson H. Liposuction treatment of lymphedema. Semin Plast Surg. 2018;32(1):42–7. https://doi.org/10.1055/s-0038-1635116.
Bamba R, Chu A, Gallegos J, Herrera FA, Hassanein AH. Outcomes analysis of microsurgical physiologic lymphatic procedures for the upper extremity from the United States National Surgical Quality Improvement Program. Microsurgery. 2022;42(4):305–11. https://doi.org/10.1002/micr.30844.
Cheng MH, Chen SC, Henry SL, Tan BK, Chia-Yu Lin M, Huang JJ. Vascularized groin lymph node flap transfer for postmastectomy upper limb lymphedema: flap anatomy, recipient sites, and outcomes. Plast Reconstr Surg. 2013;131(6):1286–98. https://doi.org/10.1097/PRS.0b013e31828bd3b3.
Maldonado AA, Chen R, Chang DW. The use of supraclavicular free flap with vascularized lymph node transfer for treatment of lymphedema: a prospective study of 100 consecutive cases. J Surg Oncol. 2017;115(1):68–71. https://doi.org/10.1002/jso.24351.
Kenworthy EO, Nelson JA, Verma R, Mbabuike J, Mehrara BJ, Dayan JH. Double vascularized omentum lymphatic transplant (VOLT) for the treatment of lymphedema. J Surg Oncol. 2018;117(7):1413–9. https://doi.org/10.1002/jso.25033.
Hassanein AH, Danforth R, DeBrock W, Mailey B, Lester M, Socas J. Deep inferior epigastric artery vascularized lymph node transfer: a simple and safe option for lymphedema. J Plast Reconstr Aesthet Surg. 2020;73(10):1897–916. https://doi.org/10.1016/j.bjps.2020.03.017.
Coriddi M, Wee C, Meyerson J, Eiferman D, Skoracki R. Vascularized jejunal mesenteric lymph node transfer: a novel surgical treatment for extremity lymphedema. J Am Coll Surg. 2017;225(5):650–7. https://doi.org/10.1016/j.jamcollsurg.2017.08.001.
Gould DJ, Mehrara BJ, Neligan P, Cheng MH, Patel KM. Lymph node transplantation for the treatment of lymphedema. J Surg Oncol. 2018;118(5):736–42. https://doi.org/10.1002/jso.25180.
Johnston ME, Socas J, Hunter JL, Ceppa EP. Laparoscopic gastroepiploic lymphovascular pedicle harvesting for the treatment of extremity lymphedema: a novel technique. Surg Laparosc Endosc Percutan Tech. 2017;27(3):e40–e3. https://doi.org/10.1097/SLE.0000000000000412.
Crowley JS, Liu FC, Rizk NM, Nguyen D. Concurrent management of lymphedema and breast reconstruction with single-stage omental vascularized lymph node transfer and autologous breast reconstruction: A case series. Microsurgery. 2023. https://doi.org/10.1002/micr.31017.
Nguyen AT, Chang EI, Suami H, Chang DW. An algorithmic approach to simultaneous vascularized lymph node transfer with microvascular breast reconstruction. Ann Surg Oncol. 2015;22(9):2919–24. https://doi.org/10.1245/s10434-015-4408-4.
Dayan JH, Dayan E, Smith ML. Reverse lymphatic mapping: a new technique for maximizing safety in vascularized lymph node transfer. Plast Reconstr Surg. 2015;135(1):277–85. https://doi.org/10.1097/PRS.0000000000000822.
Klimberg VS. A new concept toward the prevention of lymphedema: axillary reverse mapping. J Surg Oncol. 2008;97(7):563–4. https://doi.org/10.1002/jso.20905.
Boneti C, Korourian S, Bland K, Cox K, Adkins LL, Henry-Tillman RS, Klimberg VS. Axillary reverse mapping: mapping and preserving arm lymphatics may be important in preventing lymphedema during sentinel lymph node biopsy. J Am Coll Surg. 2008;206(5):1038–42; discussion 42-4. https://doi.org/10.1016/j.jamcollsurg.2007.12.022.
Noguchi M, Noguchi M, Nakano Y, Ohno Y, Kosaka T. Axillary reverse mapping using a fluorescence imaging system in breast cancer. J Surg Oncol. 2012;105(3):229–34. https://doi.org/10.1002/jso.22094.
Ochoa O, Metzner M, Theoharis C, Chrysopoulo M, Pisano S, Nastala C, et al. Deep inferior epigastric lymph node basin: analysis of novel donor site for vascularized lymph node transfer among 10 consecutive patients. Microsurgery. 2019;39(3):215–20. https://doi.org/10.1002/micr.30372.
Brown S, Mehrara BJ, Coriddi M, McGrath L, Cavalli M, Dayan JH. A Prospective study on the safety and efficacy of vascularized lymph node transplant. Ann Surg. 2022;276(4):635–53. https://doi.org/10.1097/SLA.0000000000005591.
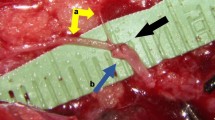
Hassanein AH, Sacks JM, Cooney DS. Optimizing perioperative lymphatic-venous anastomosis localization using transcutaneous vein illumination, isosulfan blue, and indocyanine green lymphangiography. Microsurgery. 2017;37(8):956–7. https://doi.org/10.1002/micr.30222.
Chang DW, Suami H, Skoracki R. A prospective analysis of 100 consecutive lymphovenous bypass cases for treatment of extremity lymphedema. Plast Reconstr Surg. 2013;132(5):1305–14. https://doi.org/10.1097/PRS.0b013e3182a4d626.
Koshima I, Inagawa K, Urushibara K, Moriguchi T. Supermicrosurgical lymphaticovenular anastomosis for the treatment of lymphedema in the upper extremities. J Reconstr Microsurg. 2000;16(6):437–42. https://doi.org/10.1055/s-2006-947150.
Tourani SS, Taylor GI, Ashton MW. Long-term patency of lymphovenous anastomoses: a systematic review. Plast Reconstr Surg. 2016;138(2):492–8. https://doi.org/10.1097/PRS.0000000000002395.
Schwarz GS, Grobmyer SR, Djohan RS, Cakmakoglu C, Bernard SL, Radford D, et al. Axillary reverse mapping and lymphaticovenous bypass: Lymphedema prevention through enhanced lymphatic visualization and restoration of flow. J Surg Oncol. 2019;120(2):160–7. https://doi.org/10.1002/jso.25513.
Johnson AR, Singhal D. Immediate lymphatic reconstruction. J Surg Oncol. 2018;118(5):750–7. https://doi.org/10.1002/jso.25177.
Cook JA, Sasor SE, Loewenstein SN, DeBrock W, Lester M, Socas J, et al. Immediate lymphatic reconstruction after axillary lymphadenectomy: a single-institution early experience. Ann Surg Oncol. 2021;28(3):1381–7. https://doi.org/10.1245/s10434-020-09104-2.
Cakmakoglu C, Kwiecien GJ, Schwarz GS, Gastman B. Lymphaticovenous bypass for immediate lymphatic reconstruction in locoregional advanced melanoma patients. J Reconstr Microsurg. 2020;36(4):247–52. https://doi.org/10.1055/s-0039-3401829.
Thompson M, Korourian S, Henry-Tillman R, Adkins L, Mumford S, Westbrook KC, Klimberg VS. Axillary reverse mapping (ARM): a new concept to identify and enhance lymphatic preservation. Ann Surg Oncol. 2007;14(6):1890–5. https://doi.org/10.1245/s10434-007-9412-x.
Giuliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994;220(3):391–8; discussion 8-401. https://doi.org/10.1097/00000658-199409000-00015.
Sakurai T, Endo M, Shimizu K, Yoshimizu N, Nakajima K, Nosaka K, et al. Axillary reverse mapping using fluorescence imaging is useful for identifying the risk group of postoperative lymphedema in breast cancer patients undergoing sentinel node biopsies. J Surg Oncol. 2014;109(6):612–5. https://doi.org/10.1002/jso.23528.
Valente SA, Al-Hilli Z, Radford DM, Yanda C, Tu C, Grobmyer SR. Near infrared fluorescent lymph node mapping with indocyanine green in breast cancer patients: a prospective trial. J Am Coll Surg. 2019;228(4):672–8. https://doi.org/10.1016/j.jamcollsurg.2018.12.001.
Cook JA, Sinha M, Lester M, Fisher CS, Sen CK, Hassanein AH. Immediate lymphatic reconstruction to prevent breast cancer-related lymphedema: a systematic review. Adv Wound Care (New Rochelle). 2022;11(7):382–91. https://doi.org/10.1089/wound.2021.0056.
Chang DW. Lymphaticovenular bypass for lymphedema management in breast cancer patients: a prospective study. Plast Reconstr Surg. 2010;126(3):752–8. https://doi.org/10.1097/PRS.0b013e3181e5f6a9.
Coriddi M, Mehrara B, Skoracki R, Singhal D, Dayan JH. Immediate lymphatic reconstruction: technical points and literature review. Plast Reconstr Surg Glob Open. 2021;9(2):e3431. https://doi.org/10.1097/GOX.0000000000003431.
Friedman R, Bustos VP, Postian T, Pardo J, Hamaguchi R, Lee BT, et al. Utilizing a lower extremity vein graft for immediate lymphatic reconstruction. J Plast Reconstr Aesthet Surg. 2022;75(8):2831–70. https://doi.org/10.1016/j.bjps.2022.06.076.
Scaglioni MF, Fontein DBY, Arvanitakis M, Giovanoli P. Systematic review of lymphovenous anastomosis (LVA) for the treatment of lymphedema. Microsurgery. 2017;37(8):947–53. https://doi.org/10.1002/micr.30246.
Ko E, Han W, Cho J, Lee JW, Kang SY, Jung SY, et al. Fibrin glue reduces the duration of lymphatic drainage after lumpectomy and level II or III axillary lymph node dissection for breast cancer: a prospective randomized trial. J Korean Med Sci. 2009;24(1):92–6. https://doi.org/10.3346/jkms.2009.24.1.92.
Boccardo F, Casabona F, De Cian F, Friedman D, Villa G, Bogliolo S, et al. Lymphedema microsurgical preventive healing approach: a new technique for primary prevention of arm lymphedema after mastectomy. Ann Surg Oncol. 2009;16(3):703–8. https://doi.org/10.1245/s10434-008-0270-y.
Casabona F, Bogliolo S, Valenzano Menada M, Sala P, Villa G, Ferrero S. Feasibility of axillary reverse mapping during sentinel lymph node biopsy in breast cancer patients. Ann Surg Oncol. 2009;16(9):2459–63. https://doi.org/10.1245/s10434-009-0554-x.
Feldman S, Bansil H, Ascherman J, Grant R, Borden B, Henderson P, et al. Single institution experience with lymphatic microsurgical preventive healing approach (LYMPHA) for the primary prevention of lymphedema. Ann Surg Oncol. 2015;22(10):3296–301. https://doi.org/10.1245/s10434-015-4721-y.
Hahamoff M, Gupta N, Munoz D, Lee BT, Clevenger P, Shaw C, et al. A lymphedema surveillance program for breast cancer patients reveals the promise of surgical prevention. J Surg Res. 2019;244:604–11. https://doi.org/10.1016/j.jss.2017.10.008.
Coriddi M, Dayan J, Bloomfield E, McGrath L, Diwan R, Monge J, et al. Efficacy of immediate lymphatic reconstruction to decrease incidence of breast cancer-related lymphedema: preliminary results of randomized controlled trial. Ann Surg. 2023;278(4):630–7. https://doi.org/10.1097/SLA.0000000000005952.
Cook JA, Hassanein AH. ASO Author Reflections: immediate lymphatic reconstruction: a proactive approach to breast cancer-related lymphedema. Ann Surg Oncol. 2021;28(3):1388–9. https://doi.org/10.1245/s10434-020-09110-4.
Funding
This work was supported by the US National Institutes of Health (NIH) grants NIH K08HL167164 and R21AR082600 and the Department of Defense W81XWH2110135 to AHH.
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahmed, S., Imeokparia, F.O. & Hassanein, A.H. Surgical Management of Lymphedema: Prophylactic and Therapeutic Operations. Curr Breast Cancer Rep (2024). https://doi.org/10.1007/s12609-024-00543-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s12609-024-00543-4