Abstract
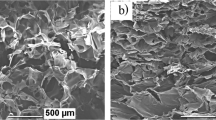
Klebsiella pneumoniae is regarded as one of the most profound bacteria isolated from the debilitating injuries caused by burn wounds. In addition, the multidrug resistance (MDR) and biofilm formation make treating burn patients with clinically available antibiotics difficult. Bacteriophage therapy has been proven an effective alternative against biofilm-mediated wound infections caused by MDR bacterial strains. In the current study, the bacteriophage (BPKPФ1) against MDR Klebsiella pneumoniae was isolated and loaded into the chitosan microparticles (CHMPs), which was later incorporated into the Sepineo P 600 to convert into a gel (BPKPФ1-CHMP-gel). BPKPФ1 was characterized for lytic profile, morphological class, and burst size, which revealed that the BPKPФ1 belongs to the family Siphoviridae. Moreover, BPKPФ1 exhibited a narrow host range with 128 PFU/host cell of burst size. The BPKPФ1-loaded CHMPs showed an average particle size of 1.96 ± 0.51 μm, zeta potential 32.16 ± 0.41 mV, and entrapment efficiency in the range of 82.44 ± 1.31%. Further, the in vitro antibacterial and antibiofilm effectiveness of BPKPФ1-CHMPs-gel were examined. The in vivo potential of the BPKPФ1-CHMPs-gel was assessed using a rat model with MDR Klebsiella pneumoniae infected burn wound, which exhibited improved wound contraction (89.22 ± 0.48%) in 28 days with reduced inflammation, in comparison with different controls. Data in hand suggest the potential of bacteriophage therapy to be developed as personalized therapy in case of difficult-to-treat bacterial infections.
Graphical abstract








Similar content being viewed by others
Abbreviations
- MDR:
-
Multidrug resistance
- AMR:
-
Antimicrobial resistance
- BP:
-
Bacteriophage
- K. pneumoniae :
-
Klebsiella pneumoniae
- BPKPФ1:
-
Bacteriophage against K. pneumoniae
- CHMPs:
-
Chitosan microparticles
- BPKPФ1-CHMPs:
-
Bacteriophage chitosan microparticles
- DLAO:
-
Double-layer agar overlay
- TEM:
-
Transmission electron microscopy
- SEM:
-
Scanning electron microscopy
- SSD:
-
Silver sulfadiazine
- USG/PA:
-
Ultrasound/photoacoustic
References
Center for disease control and prevention. Antibiotic resistance threats in the United States, 2019: US Department of Health and Human Services, Centres for Disease Control; 2019.
NIH. Forgery International Center. The paradox of antimicrobial resistance in India. Global Health Matters May/June 2022. 2022;21(3).
Taneja N, Sharma M. Antimicrobial resistance in the environment: the Indian scenario. The Ind J Med Res. 2019;149(2):119–28.
Greenhalgh DG. Management of burns. N Engl J Med. 2019;380(24):2349–59.
Markiewicz-Gospodarek A, Kozioł M, Tobiasz M, Baj J, Radzikowska-Büchner E, Przekora A. Burn wound healing: clinical complications, medical care, treatment, and dressing types: the current state of knowledge for clinical practice. Int J Environ Res. 2022;19(3):1338.
Masson-Meyers DS, Andrade TAM, Caetano GF, Guimaraes FR, Leite MN, Leite SN, et al. Experimental models and methods for cutaneous wound healing assessment. Int J Experiment Pathol. 2020;101(1-2):21–37.
Shariati A, Moradabadi A, Ghaznavi-Rad E, Dadmanesh M, Komijani M, Nojoomi F. Investigation into antibacterial and wound healing properties of platelets lysate against Acinetobacter baumannii and Klebsiella pneumoniae burn wound infections. Annals Clin Microbiol Antimicrob. 2021;20(1):40.
Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev. 2005;18(4):657–86.
Navon-Venezia S, Kondratyeva K, Carattoli A. Klebsiella pneumoniae: a major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol Rev. 2017;41(3):252–75.
Anand T, Virmani N, Kumar S, Mohanty AK, Pavulraj S, Bera BC, et al. Phage therapy for treatment of virulent Klebsiella pneumoniae infection in a mouse model. J Global Antimicrob Resist. 2020;21:34–41.
Chang RYK, Morales S, Okamoto Y, Chan H-K. Topical application of bacteriophages for treatment of wound infections. Transl Res. 2020;220:153–66.
Vandenheuvel D, Meeus J, Lavigne R, Van den Mooter G. Instability of bacteriophages in spray-dried trehalose powders is caused by crystallization of the matrix. Int J Pharm. 2014;472(1-2):202–5.
Inst. CaLSI. Methods for determining bactericidal activity of antimicrobial agents; approved guideline M26-A. Clin Lab Stand. 1999;19:7.
Kim J, Jo A, Chukeatirote E, Ahn J. Assessment of antibiotic resistance in Klebsiella pneumoniae exposed to sequential in vitro antibiotic treatments. Annals Clin Microbiol Antimicrob. 2016;15(1):60.
Singh A, Singh AN, Rathor N, Chaudhry R, Singh SK, Nath G. Evaluation of bacteriophage cocktail on septicemia caused by colistin-resistant Klebsiella pneumoniae in mice model. Front Pharmacol. 2022;13:778676.
Hyman P. Phages for phage therapy: isolation, characterization, and host range breadth. Pharmaceuticals (Basel). 2019;12(1):35. https://doi.org/10.3390/ph12010035.
Luong T, Salabarria AC, Edwards RA, Roach DR. Standardized bacteriophage purification for personalized phage therapy. Nat Protocols. 2020;15(9):2867–90.
Kropinski AM, Mazzocco A, Waddell TE, Lingohr E, Johnson RP. Enumeration of bacteriophages by double agar overlay plaque assay. Methods Mol Biol (Clifton, NJ). 2009;501:69–76.
El-Atrees DM, El-Kased RF, Abbas AM, Yassien MA. Characterization and anti-biofilm activity of bacteriophages against urinary tract Enterococcus faecalis isolates. Sci Rep. 2022;12(1):13048.
Jurczak-Kurek A, Gąsior T, Nejman-Faleńczyk B, Bloch S, Dydecka A, Topka G, et al. Biodiversity of bacteriophages: morphological and biological properties of a large group of phages isolated from urban sewage. Sci Rep. 2016;6(1):34338.
Khan Mirzaei M, Nilsson AS. Isolation of phages for phage therapy: a comparison of spot tests and efficiency of plating analyses for determination of host range and efficacy. Plos One. 2015;10(3):e0118557.
Dewanggana MN, Evangeline C, Ketty MD, Waturangi DE, Yogiara MS. Isolation, characterization, molecular analysis and application of bacteriophage DW-EC to control Enterotoxigenic Escherichia coli on various foods. Sci Rep. 2022;12(1):495.
Akhwale JK, Rohde M, Rohde C, Bunk B, Spröer C, Boga HI, et al. Isolation, characterization and analysis of bacteriophages from the haloalkaline lake Elmenteita, Kenya. Plos One. 2019;14(4):e0215734.
Allué-Guardia A, Jofre J, Muniesa M. Stability and infectivity of cytolethal distending toxin type V gene-carrying bacteriophages in a water mesocosm and under different inactivation conditions. Appl Environ Microbiol. 2012;78(16):5818–23.
Ellis EL, Delbruck M. The growth of bacteriophage. J The J Gen Physiol. 1939;22(3):365–84.
Chang Y, Shin H, Lee JH, Park CJ, Paik SY, Ryu S. Isolation and genome characterization of the virulent Staphylococcus aureus bacteriophage SA97. Viruses. 2015;7(10):5225–42.
Pan Y, Ren X, Wang S, Li X, Luo X, Yin Z. Annexin V-conjugated mixed micelles as a potential drug delivery system for targeted thrombolysis. Biomacromolecules. 2017;18(3):865–76.
Sareen R, Kapil M, Gupta GN. Incubation and its effect on Leishman stain. J Lab Phys. 2018;10(3):357–61.
Dehari D, Mehata AK, Priya V, Parbat D, Kumar D, Srivastava AK, et al. Luliconazole nail lacquer for the treatment of onychomycosis: formulation, characterization and in vitro and ex vivo evaluation. AAPS Pharm Sci Tech. 2022;23(6):175.
Rahimzadeh G, Saeedi M, Moosazadeh M, Hashemi SMH, Babaei A, Rezai MS, et al. Encapsulation of bacteriophage cocktail into chitosan for the treatment of bacterial diarrhea. Sci Rep. 2021;11(1):15603.
Ilomuanya MO, Enwuru NV, Adenokun E, Fatunmbi A, Adeluola A, Igwilo CI. Chitosan-based microparticle encapsulated Acinetobacter baumannii phage cocktail in hydrogel matrix for the management of multidrug resistant chronic wound infection. Turk J Pharm Sci. 2022;19(2):187–95.
Baghel S, Nair VS, Pirani A, Sravani AB, Bhemisetty B, Ananthamurthy K, et al. Luliconazole-loaded nanostructured lipid carriers for topical treatment of superficial Tinea infections. Dermatol Ther. 2020;33(6):e13959.
Li X, Kong X, Shi S, Zheng X, Guo G, Wei Y, et al. Preparation of alginate coated chitosan microparticles for vaccine delivery. BMC Biotechnol. 2008;8(1):89.
Anjum MM, Patel KK, Dehari D, Pandey N, Tilak R, Agrawal AK, et al. Anacardic acid encapsulated solid lipid nanoparticles for Staphylococcus aureus biofilm therapy: chitosan and DNase coating improves antimicrobial activity. Drug Deliv Translat Res. 2021;11(1):305–17.
Proniuk S, Blanchard J. Anhydrous Carbopol® polymer gels for the topical delivery of oxygen/water sensitive compounds. Pharm Dev Technol. 2002;7(2):249–55.
Dantas MGB, Reis SAGB, Damasceno CMD, Rolim LA, Rolim-Neto PJ, Carvalho FO, et al. Development and evaluation of stability of a gel formulation containing the monoterpene borneol. The Sci World J. 2016;2016:7394685.
Patel KK, Surekha DB, Tripathi M, Anjum MM, Muthu MS, Tilak R, et al. Antibiofilm potential of silver sulfadiazine-loaded nanoparticle formulations: a study on the effect of DNase-I on microbial biofilm and wound healing activity. Mol Pharm. 2019;16(9):3916–25.
Rodríguez-Melcón C, Alonso-Calleja C, García-Fernández C, Carballo J, Capita R. Minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) for twelve antimicrobials (biocides and antibiotics) in eight strains of Listeria monocytogenes. Biol. 2021;11(1)
Plota M, Sazakli E, Giormezis N, Gkartziou F, Kolonitsiou F, Leotsinidis M, et al. In vitro anti-biofilm activity of bacteriophage K (ATCC 19685-B1) and daptomycin against staphylococci. Microorganisms. 2021;9(9)
Liu Y, She P, Xu L, Chen L, Li Y, Liu S, et al. Antimicrobial, antibiofilm, and anti-persister activities of penfluridol against Staphylococcus aureus. Front Microbiol. 2021;12:727692.
Kim T, Zhang Q, Li J, Zhang L, Jokerst JV. A gold/silver hybrid nanoparticle for treatment and photoacoustic imaging of bacterial infection. ACS Nano. 2018;12(6):5615–25.
Suda T, Hanawa T, Tanaka M, Tanji Y, Miyanaga K, Hasegawa-Ishii S, et al. Modification of the immune response by bacteriophages alters methicillin-resistant Staphylococcus aureus infection. Sci Rep. 2022;12(1):15656.
Li CW, Wang Q, Li J, Hu M, Shi SJ, Li ZW, et al. Silver nanoparticles/chitosan oligosaccharide/poly(vinyl alcohol) nanofiber promotes wound healing by activating TGFβ1/Smad signaling pathway. Int J Nanomed. 2016;11:373–86.
Puapermpoonsiri U, Spencer J, van der Walle CF. A freeze-dried formulation of bacteriophage encapsulated in biodegradable microspheres. Eur J Pharm Biopharm Official J Arbeitsgemeinschaft fur Pharmazeutische Verfahrenstechnik eV. 2009;72(1):26–33.
Perween N, Prakash SK, Siddiqui O. Multi drug resistant Klebsiella isolates in burn patients: a comparative study. J Clin Diagn Res JCDR. 2015;9(9):Dc14-6.
Ye M, Sun M, Huang D, Zhang Z, Zhang H, Zhang S, et al. A review of bacteriophage therapy for pathogenic bacteria inactivation in the soil environment. Environ Int. 2019;129:488–96.
Lan P, Jiang Y, Zhou J, Yu Y. A global perspective on the convergence of hypervirulence and carbapenem resistance in Klebsiella pneumoniae. J Glob Antimicrob Resist. 2021;25:26–34.
Farhadi M, Ahanjan M, Goli HR, Haghshenas MR, Gholami M. High frequency of multidrug-resistant (MDR) Klebsiella pneumoniae harboring several β-lactamase and integron genes collected from several hospitals in the north of Iran. Annals Clin Microbiol Antimicrob. 2021;20(1):70.
de Jonge PA, Nobrega FL, Brouns SJJ, Dutilh BE. Molecular and evolutionary determinants of bacteriophage host range. Trends Microbiol. 2019;27(1):51–63.
Kazimierczak J, Wójcik EA, Witaszewska J, Guziński A, Górecka E, Stańczyk M, et al. Complete genome sequences of Aeromonas and Pseudomonas phages as a supportive tool for development of antibacterial treatment in aquaculture. Virol J. 2019;16(1):4.
Jończyk E, Kłak M, Międzybrodzki R, Górski A. The influence of external factors on bacteriophages—review. Folia Microbiol. 2011;56(3):191–200.
Khawaja KA, Abbas Z, Rehman SU. Isolation and characterization of lytic phages TSE1-3 against Enterobacter cloacae. J Open Life Sci. 2016;11(1):287–92.
Ahmadi H, Radford D, Kropinski AM, Lim LT, Balamurugan S. Thermal-stability and reconstitution ability of listeria phages P100 and A511. Front Microbiol. 2017;5(8):2375. https://doi.org/10.3389/fmicb.2017.02375.
Mohammadian F, Rahmani HK, Bidarian B, Khoramian B. Isolation and evaluation of the efficacy of bacteriophages against multidrug-resistant (MDR), methicillin-resistant (MRSA) and biofilm-producing strains of Staphylococcus aureus recovered from bovine mastitis. BMC Vet Res. 2022;18(1):406.
Patzelt A, Richter H, Knorr F, Schäfer U, Lehr CM, Dähne L, et al. Selective follicular targeting by modification of the particle sizes. J Controlled Release : Official J Control Release Soc. 2011;150(1):45–8.
Loh B, Gondil VS, Manohar P, Khan FM, Yang H, Leptihn S. Encapsulation and delivery of therapeutic phages. Appl Environ Microbiol. 2021;87(5)
Abdelsattar AS, Abdelrahman F, Dawoud A, Connerton IF, El-Shibiny A. Encapsulation of E. coli phage ZCEC5 in chitosan–alginate beads as a delivery system in phage therapy. AMB Express. 2019;9(1):87.
Ma Y, Pacan JC, Wang Q, Xu Y, Huang X, Korenevsky A, et al. Microencapsulation of bacteriophage felix O1 into chitosan-alginate microspheres for oral delivery. Appl Environ Microbiol. 2008;74(15):4799–805.
Choińska-Pulit A, Mituła P, Śliwka P, Łaba W, Skaradzińska A. Bacteriophage encapsulation: trends and potential applications. Trends Food Sci Technol. 2015;45(2):212–21.
Kim, S., Jo, A. and Ahn, J. Application of chitosan–alginate microspheres for the sustained release of bacteriophage in simulated gastrointestinal conditions. Int J Food Sci Technol. 2015;50:913–8. https://doi.org/10.1111/ijfs.12736.
Rotman SG, Sumrall E, Ziadlou R, Grijpma DW, Richards RG, Eglin D, et al. Local bacteriophage delivery for treatment and prevention of bacterial infections. Front Microbiol. 2020;11:538060.
Zyman A, Górski A, Międzybrodzki R. Phage therapy of wound-associated infections. Folia Microbiol (Praha). 2022;67(2):193–201.
Pinto AM, Cerqueira MA, Bañobre-Lópes M, Pastrana LM, Sillankorva S. Bacteriophages for chronic wound treatment: from traditional to novel delivery systems. Viruses. 2020;12(2):235. https://doi.org/10.3390/v12020235.
Sulakvelidze A, Alavidze Z, Morris JG Jr. Bacteriophage therapy. Antimicrob Agents Chemother. 2001;45(3):649–59.
Mantri Y, Tsujimoto J, Donovan B, Fernandes CC, Garimella PS, Penny WF, et al. Photoacoustic monitoring of angiogenesis predicts response to therapy in healing wounds. Wound repair and regeneration : official publication of the Wound Healing Society [and] the European Tissue Repair. Soc. 2022;30(2):258–67.
Acknowledgements
Author D. Dehari would like to thank the Indian Institute of Technology (BHU) Varanasi for providing financial assistance in the form of a research support grant to conduct the study. SEM and Confocal microscopy were performed at IIT (BHU) Varanasi, for which the authors express their appreciation to the Central Instrument Facility Centre. The authors are also grateful to the Virus Research & Development Laboratory in the Department of Microbiology at the Institute of Medical Science at Banaras Hindu University in Varanasi for providing lab space for the study of Bateriophages as part of scheme 5066 and the use of an Optima XPN-100 Ultracentrifuge (supported by the Department of Science and Technology’s PURSE program). Department of Geology (BHU) is also acknowledged for the facility of scanning electron microscope used to examine biological samples. Also acknowledged is SATHI (Banaras Hindu University) for providing the Photoacoustic imaging platform.
Author information
Authors and Affiliations
Contributions
Deepa Dehari: conceptualization, methodology, formal analysis and data curation, and writing; Aiswarya Chaudhuri, Dulla Naveen Kumar, and Meraj Anjum: formulation, data collection, participated in animal experiments; Rajesh Kumar and Akshay Kumar: bacterial strain collection, bacteriophage isolation, and data curation; Dinesh Kumar: validation, review, and editing, Gopal Nath: provided microbiology lab facility, conceptualization, supervised, writing—review and editing; and Ashish Kumar Agrawal: conceived and supervised the project, reviewing, editing, and approved the final manuscript. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
IAEC approved all animal experiments with approval no-IIT(BHU)/IAEC/2022/007 from the Department of Pharmaceutical Eng. & Tech., Indian Institute of Technology (BHU), Varanasi, U.P., India.
Conflict of Interest
The authors declare no competing interest
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 462 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dehari, D., Chaudhuri, A., Kumar, D.N. et al. A Bacteriophage-Loaded Microparticle Laden Topical Gel for the Treatment of Multidrug-Resistant Biofilm-Mediated Burn Wound Infection. AAPS PharmSciTech 24, 165 (2023). https://doi.org/10.1208/s12249-023-02620-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02620-w