Abstract
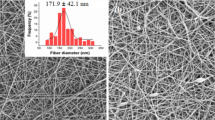
Nanofibers have many promising biomedical applications. They can be used for designing transdermal and dermal drug delivery systems. This project aimed to prepare and characterize polyvinylpyrrolidone-based nanofibers as a dermal and transdermal drug delivery system using pioglitazone. Pioglitazone is an oral antidiabetic drug. In addition, it can act as an inflammatory process modulator, making it a good candidate for managing different skin inflammatory conditions such as atopic dermatitis, skin ulcers, and diabetic foot wound healing. Several nanofiber formulations were prepared using the electrospinning method at different drug loadings, polyvinylpyrrolidone concentrations, and flow rates. A cast film with the exact composition of selected nanofiber formulations was prepared as a control. Nanofibers were characterized using a scanning electron microscope to calculate the diameter. Fourier-transform infrared spectroscopy, differential scanning calorimetry, thermogravimetric analysis, and powder X-ray diffraction were performed for physical and biochemical characterizations. In vitro release, drug loading efficiency, and swelling studies were performed. Ex vivo permeation studies were performed using Franz diffusion cells with or without applying a solid microneedle roller. Round uniform nanofibers with a smooth surface were obtained. The diameter of nanofibers was affected by the drug loading and polymer concentration. Fourier-transform infrared spectra showed a potential physical interaction between the drug and the polymer. According to X-ray diffraction, pioglitazone existed in an amorphous form in prepared nanofibers, with partial crystallinity in the casted film. Nanofibers showed a higher swelling rate compared to the casted film. The drug dissolution rate for nanofibers was 2.3-folds higher than the casted films. The polymer concentration affected the drug dissolution rate for nanofibers; however, drug loading and flow rate did not affect the drug dissolution rate for nanofibers. The application of solid microneedles slightly enhances the total amount of drug permeation. However, it did not affect the flux of the drug through the separated epidermis layer for pioglitazone. The drug permeation flux in nanofibers was approximately five times higher than the flux of the casted film. It was observed that pioglitazone is highly retained in skin layers.

Graphical abstract











Similar content being viewed by others
References
Ramalingam M, Ramakrishna S. In: Ramalingam M, Ramakrishna SBT-NC for BA, editors. 1 - Introduction to nanofiber composites: Woodhead Publishing; 2017. p. 3–29. Available from: http://www.sciencedirect.com/science/article/pii/B9780081001738000016.
Ko FK. Nanofiber technology: bridging the gap between nano and macro world. Nanoeng Nanofibrous Mater. 2004;169:1–18.
Morie A, Garg T, Goyal AK, Rath G. Nanofibers as novel drug carrier–an overview. Artif Cells Nanomed Biotechnol. 2016;44(1):135–43.
Kamble P, Sadarani B, Majumdar A, Bhullar S. Nanofiber based drug delivery systems for skin: A promising therapeutic approach. J Drug Deliv Sci Technol. 2017;41:124–33.
Tseng Y-Y, Liu S-J. Nanofibers used for the delivery of analgesics. Nanomedicine. 2015;10(11):1785–800.
Naghibzadeh M. Nanofibers for skin regeneration. Trends Biomater Artif Organs. 2012;26(2): 86–102.
Goyal R, Macri LK, Kaplan HM, Kohn J. Nanoparticles and nanofibers for topical drug delivery. J Control Release. 2016;240:77–92.
Allen L, Ansel HC. Ansel’s pharmaceutical dosage forms and drug delivery systems. 10th ed. Baltimore: Lippincott Williams & Wilkins; 2013. p. 342–257.
Rai VK, Mishra N, Yadav KS, Yadav NP. Nanoemulsion as pharmaceutical carrier for dermal and transdermal drug delivery: formulation development, stability issues, basic considerations and applications. J Control release. 2018;270:203–25.
Javadzadeh Y, Bahari LA. Therapeutic nanostructures for dermal and transdermal drug delivery. In: Nano-and microscale drug delivery systems. Elsevier; 2017. p. 131–46.
Honeywell-Nguyen PL, Bouwstra JA. Vesicles as a tool for transdermal and dermal delivery. Drug Discov today Technol. 2005;2(1):67–74.
Chacko IA, Ghate VM, Dsouza L, Lewis SA. Lipid vesicles: A versatile drug delivery platform for dermal and transdermal applications. Colloids Surfaces B Biointerfaces. 2020;195:111262.
Alexander A, Dwivedi S, Giri TK, Saraf S, Saraf S, Tripathi DK. Approaches for breaking the barriers of drug permeation through transdermal drug delivery. J Control Release. 2012;164(1):26–40.
Naik A, Kalia YN, Guy RH. Transdermal drug delivery: overcoming the skin's barrier function. Pharm Sci Technolo Today. 2000;3(9):318–26.
Alkilani A, McCrudden MT, Donnelly R. Transdermal drug delivery: innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics. 2015;7(4):438–70.
Barry BW. Novel mechanisms and devices to enable successful transdermal drug delivery. Eur J Pharm Sci. 2001;14(2):101–14.
Hamed R, Farhan A, Abu-Huwaij R, Mahmoud NN, Kamal A. Lidocaine microemulsion-laden organogels as lipid-based systems for topical delivery. J Pharm Innov. 2020;15(4):521–34.
Waghule T, Singhvi G, Dubey SK, Pandey MM, Gupta G, Singh M, Dua K. Microneedles: A smart approach and increasing potential for transdermal drug delivery system. Biomed Pharmacother. 2019;109:1249–58.
Sweetman SC. Martindale: The complete drug reference. Drug Monographs: Pharmaceutical Press; 2011.
Espinoza LC, Vera-García R, Silva-Abreu M, Domènech Ò, Badia J, Rodríguez-Lagunas MJ, Clares B, Calpena AC. Topical Pioglitazone nanoformulation for the treatment of atopic dermatitis: design, characterization and efficacy in hairless mouse model. Pharmaceutics. 2020;12(3):255.
Espinoza LC, Silva-Abreu M, Calpena AC, Rodríguez-Lagunas MJ, Fábrega M-J, Garduño-Ramírez ML, Clares B. Nanoemulsion strategy of pioglitazone for the treatment of skin inflammatory diseases. Nanomed Nanotechnol Biol Med. 2019;19:115–25.
Rojewska A, Karewicz A, Karnas K, Wolski K, Zając M, Kamiński K, Szczubiałka K, Zapotoczny S, Nowakowska M. Pioglitazone-loaded nanostructured hybrid material for skin ulcer treatment. Materials (Basel). 2020;13(9):2050.
Natarajan J, Sanapalli BKR, Bano M, Singh SK, Gulati M, Karri VVSR. Nanostructured lipid carriers of pioglitazone loaded collagen/chitosan composite scaffold for diabetic wound healing. Adv Wound Care. 2019;8(10):499–513.
Prasad PS, Imam SS, Aqil M, Sultana Y, Ali A. QbD-based carbopol transgel formulation: characterization, pharmacokinetic assessment and therapeutic efficacy in diabetes. Drug Deliv. 2016;23(3):1047–56.
Alam S, Aslam M, Khan A, Imam SS, Aqil M, Sultana Y, Ali A. Nanostructured lipid carriers of pioglitazone for transdermal application: from experimental design to bioactivity detail. Drug Deliv. 2016;23(2):601–9.
Nair AB, Gupta S, Al-Dhubiab BE, Jacob S, Shinu P, Shah J, et al. Effective therapeutic delivery and bioavailability enhancement of pioglitazone using drug in adhesive transdermal patch. Pharmaceutics. 2019;11(7):359.
Cam ME, Yildiz S, Alenezi H, Cesur S, Ozcan GS, Erdemir G, Edirisinghe U, Akakin D, Kuruca DS, Kabasakal L, Gunduz O, Edirisinghe M. Evaluation of burst release and sustained release of pioglitazone-loaded fibrous mats on diabetic wound healing: an in vitro and in vivo comparison study. J R Soc Interface. 2020;17(162):20190712.
Mahmoud NN, Qabooq H, Alsotari S, Tarawneh OA, Aboalhaija NH, Shraim S, Alkilany AM, Khalil EA, Abu-Dahab R. Quercetin-gold nanorods incorporated into nanofibers: development, optimization and cytotoxicity. RSC Adv. 2021;11:19956–66.
Madhukar A, Naresh K, Kumar CN, Sandhya N, Prasanna P. Rapid and sensitive RP-HPLC analytical method development and validation of pioglitazone hydrochloride. Der Pharm Chem. 2011;3:128–32.
Suresh R, Sree VJ, Manavalan R, Vallippan K. Aspect of validation in HPLC method development for pharmaceutical analysis-comparison of validation requirements by FDA, USP And ICH. Inter. J Pharm Sci. 2010;1(12):123–32.
Obaidat R, Al-Shar'i N, Tashtoush B, Athamneh T. Enhancement of levodopa stability when complexed with β-cyclodextrin in transdermal patches. Pharm Dev Technol. 2018;23(10):986–97.
Abu-Huwaij R, Obaidat RM, Sweidan K, Al-Hiari Y. Formulation and in vitro evaluation of xanthan gum or carbopol 934-based mucoadhesive patches, loaded with nicotine. Aaps Pharmscitech. 2011;12(1):21–7.
van Diest PJ, Savulescu J. No consent should be needed for using leftover body material for scientific purposesForAgainst. BMJ. 2002;325(7365):648–51.
Henning A, Neumann D, Kostka K-H, Lehr C-M, Schaefer UF. Influence of human skin specimens consisting of different skin layers on the result of in vitro permeation experiments. Skin Pharmacol Physiol. 2008;21(2):81–8.
Jian L, Cao Y, Zou Y. Dermal-epidermal separation by heat. In: Epidermal cells. Springer; 2019. p. 23–5.
Hegab H, Tariq M, Syed NA, Rizvi G, Pop-Iliev R. Towards Analysis and Optimization of Electrospun PVP (Polyvinylpyrrolidone) Nanofibers. Adv Polym Technol. 2020;2020:1–9.
Pokharkar V, Kutwal M, Mandpe L. Pioglitazone solid dispersion system prepared by spray drying method: in vitro and in vivo evaluation. PDA J Pharm Sci Technol. 2013;67(1):23–34.
Bhosale UM, Galgatte UC, Chaudhari PD. Development of pioglitazone hydrochloride lipospheres by melt dispersion technique: Optimization and evaluation. J Appl Pharm Sci. 2016;6(01):107–17.
Swain RP, Subudhi BB. Effect of semicrystalline copolymers in solid dispersions of pioglitazone hydrochloride: in vitro-in vivo correlation. Drug Dev Ind Pharm. 2019;45(5):775–86.
Sun W, Araci Z, Inayathullah M, Manickam S, Zhang X, Bruce MA, Marinkovich MP, Lane AT, Milla C, Rajadas J, Butte MJ. Polyvinylpyrrolidone microneedles enable delivery of intact proteins for diagnostic and therapeutic applications. Acta Biomater. 2013;9(8):7767–74.
Alshora DH, Alsaif S, Ibrahim MA, Ezzeldin E, Almeanazel OT, Abou El Ela AES, et al. Co-stabilization of pioglitazone HCL nanoparticles prepared by planetary ball milling: in-vitro and in-vivo evaluation. Pharm Dev Technol. 2020;1–10;25:845–54.
Tao M, Wang J, Wang Y. Solubilities of pioglitazone hydrochloride in different solvents. J Chem Eng Data. 2011;56(5):2710–3.
Patil SV, Pawar AP, Sahoo SK. Improved compressibility, flowability, dissolution and bioavailability of pioglitazone hydrochloride by emulsion solvent diffusion with additives. Die Pharm Int J Pharm Sci. 2012;67(3):215–23.
Ngawhirunpat T, Opanasopit P, Rojanarata T, Akkaramongkolporn P, Ruktanonchai U, Supaphol P. Development of meloxicam-loaded electrospun polyvinyl alcohol mats as a transdermal therapeutic agent. Pharm Dev Technol. 2009;14(1):73–82.
Zahedi P, Rezaeian I, Jafari SH, Karami Z. Preparation and release properties of electrospun poly (vinyl alcohol)/poly (ɛ-caprolactone) hybrid nanofibers: optimization of process parameters via D-optimal design method. Macromol Res. 2013;21(6):649–59.
Gencturk A, Kahraman E, Güngör S, Özhan G, Özsoy Y, Sarac AS. Polyurethane/hydroxypropyl cellulose electrospun nanofiber mats as potential transdermal drug delivery system: characterization studies and in vitro assays. Artif Cells Nanomed Biotechnol. 2017;45(3):655–64.
Taepaiboon P, Rungsardthong U, Supaphol P. Vitamin-loaded electrospun cellulose acetate nanofiber mats as transdermal and dermal therapeutic agents of vitamin A acid and vitamin E. Eur J Pharm Biopharm. 2007;67(2):387–97.
Kamble RN, Gaikwad S, Maske A, Patil SS. Fabrication of electrospun nanofibres of BCS II drug for enhanced dissolution and permeation across skin. J Adv Res. 2016;7(3):483–9.
Bruschi ML, editor. Mathematical models of drug release: Woodhead Publishing; 2015;63:63–86. Available from: https://www.sciencedirect.com/science/article/pii/B9780081000922000059
Tuğcu-Demiröz F, Saar S, Tort S, Acartürk F. Electrospun metronidazole-loaded nanofibers for vaginal drug delivery. Drug Dev Ind Pharm. 2020;46(6):1015–25.
Li Z, Wang C. Effects of working parameters on electrospinning. In: One-dimensional nanostructures. Springer; 2013. p. 15–28.
Bhardwaj N, Kundu SC. Electrospinning: a fascinating fiber fabrication technique. Biotechnol Adv. 2010;28(3):325–47.
Rasekh M, Karavasili C, Soong YL, Bouropoulos N, Morris M, Armitage D, Li X, Fatouros DG, Ahmad Z. Electrospun PVP–indomethacin constituents for transdermal dressings and drug delivery devices. Int J Pharm. 2014;473(1–2):95–104.
Shen X, Yu D, Zhu L, Branford-White C, White K, Chatterton NP. Electrospun diclofenac sodium loaded Eudragit® L 100-55 nanofibers for colon-targeted drug delivery. Int J Pharm. 2011;408(1–2):200–7.
Silva-Abreu M, Calpena AC, Espina M, Silva AM, Gimeno A, Egea MA, García ML. Optimization, biopharmaceutical profile and therapeutic efficacy of pioglitazone-loaded PLGA-PEG nanospheres as a novel strategy for ocular inflammatory disorders. Pharm Res. 2018;35(1):11.
Obaidat RM, AlTaani B, Ailabouni A. Effect of different polymeric dispersions on in-vitro dissolution rate and stability of celecoxib class II drug. J Polym Res. 2017;24(4):58.
Tao M, Wang Z, Gong J, Hao H, Wang J. Determination of the solubility, dissolution enthalpy, and entropy of pioglitazone hydrochloride (form II) in different pure solvents. Ind Eng Chem Res. 2013;52(8):3036–41.
Poornima B, Prasad K, Bharathi K. Solid-State Screening and Evaluation of Pioglitazone Hydrochloride. Curr Pharm Anal. 2018;14(1):8–16.
Bonthagarala B, Dasari V, Kotra V, Swain S, Beg S. Quality-by-Design based development and characterization of pioglitazone loaded liquisolid compact tablets with improved biopharmaceutical attributes. J Drug Deliv Sci Technol. 2019;51:345–55.
Paradkar A, Ambike AA, Jadhav BK, Mahadik KR. Characterization of curcumin–PVP solid dispersion obtained by spray drying. Int J Pharm. 2004;271(1–2):281–6.
Allahverdiyev AM, Kon KV, Abamor ES, Bagirova M, Rafailovich M. Coping with antibiotic resistance: combining nanoparticles with antibiotics and other antimicrobial agents. Expert Rev Anti Infect Ther. 2011;9(11):1035–52. https://doi.org/10.1586/eri.11.121. PMID: 22029522.
Celebioglu A, Uyar T. Electrospun formulation of acyclovir/cyclodextrin nanofibers for fast-dissolving antiviral drug delivery. Mater Sci Eng C. 2021;118:111514.
Al-Majed A, Bakheit AHH, Aziz HAA, Alharbi H, Al-Jenoobi FI. Pioglitazone. Profiles Drug Subst Excipients Relat Methodol. 2016;41:379–438.
Yu D-G, Gao L-D, White K, Branford-White C, Lu W-Y, Zhu L-M. Multicomponent amorphous nanofibers electrospun from hot aqueous solutions of a poorly soluble drug. Pharm Res. 2010;27(11):2466–77.
Dai X-Y, Nie W, Wang Y-C, Shen Y, Li Y, Gan S-J. Electrospun emodin polyvinylpyrrolidone blended nanofibrous membrane: a novel medicated biomaterial for drug delivery and accelerated wound healing. J Mater Sci Mater Med. 2012;23(11):2709–16.
Wu X, Branford-White CJ, Zhu L, Chatterton NP, Yu D. Ester prodrug-loaded electrospun cellulose acetate fiber mats as transdermal drug delivery systems. J Mater Sci Mater Med. 2010;21(8):2403–11.
Goonoo N, Bhaw-Luximon A, Jhurry D. Drug loading and release from electrospun biodegradable nanofibers. J Biomed Nanotechnol. 2014;10(9):2173–99.
Krstić M, Radojević M, Stojanović D, Radojević V, Uskoković P, Ibrić S. Formulation and characterization of nanofibers and films with carvedilol prepared by electrospinning and solution casting method. Eur J Pharm Sci. 2017;101:160–6.
Akhgari A, Ghalambor Dezfuli A, Rezaei M, Kiarsi M, Abbaspour M. The design and evaluation of a fast-dissolving drug delivery system for loratadine using the electrospinning method. Jundishapur J Nat Pharm Prod. 2016;11(2):e33613. https://doi.org/10.17795/jjnpp-33613.
Nguyen J, Ita KB, Morra MJ, Popova IE. The influence of solid microneedles on the transdermal delivery of selected antiepileptic drugs. Pharmaceutics. 2016;8(4):33.
Hoang MT, Ita KB, Bair DA. Solid microneedles for transdermal delivery of amantadine hydrochloride and pramipexole dihydrochloride. Pharmaceutics. 2015;7(4):379–96.
Shi Y, Wei Z, Zhao H, Liu T, Dong A, Zhang J. Electrospinning of ibuprofen-loaded composite nanofibers for improving the performances of transdermal patches. J Nanosci Nanotechnol. 2013;13(6):3855–63.
Bhat LR, Godge RK, Vora AT, Damle MC. Validated Rp-HPLC method for simultaneous determination of Telmisartan and Hydrochlorothiazide in pharmaceutical formulation. J Liq Chromatogr Relat Technol. 2007;30(20):3059–67.
Alquadeib BT. Development and validation of a new HPLC analytical method for the determination of diclofenac in tablets. Saudi Pharm J. 2019;27(1):66–70.
Acknowledgements
For Deanship of Research at Jordan University of Science and Technology for funding this project with Fund number (385/2020)
Author information
Authors and Affiliations
Contributions
Rana Obaidat: Design of the work; supervision, analysis, or interpretation of data for the work; and Final approval of the version to be published.
Ayat Abu Shameh: Performed the research in the lab, data acquisition, data analysis, and writing it as part of her master’s degree thesis.
Mohannad Aljarrah: contributed to design, characterization of the nanofiber preparation, characterization, and writing
Rania Hamed: contributed to the design of surface tension, rheology measurements, and writing.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Round uniform nanofibers with a smooth surface were prepared.
• The diameter of nanofibers was affected by the drug loading and PVP concentration.
• FTIR spectra showed a potential physical interaction between the drug and the polymer.
• PGZ existed in an amorphous form in the prepared nanofibers, and with partial crystallinity in the casted film.
• Nanofibers showed a higher swelling rate compared to the casted film.
• The drug dissolution rate for Nanofibers was 2.3-folds higher than the casted films. The drug dissolution rate for Nanofibers was affected by the PVP concentration; however, drug loading and flow rate did not affect the drug dissolution rate for Nanofibers.
• The application of solid microneedles slightly enhances the total amount of drug permeation. However, it did not affect the flux of the drug through the separated epidermis layer for PGZ. The drug permeation flux was approximately five times higher than the flux of the casted film.
• It was observed that PGZ is highly retained in skin layers.
Appendices
Appendix
Testing various penetration enhancers to enhance permeation of PGZ through the skin
High-Performance Liquid Chromatography (HPLC)
Development of HPLC Method
A modified high-performance liquid chromatography (HPLC) method for PGZ analysis was developed and validated based on Akkala et al. (29). A C18 HPLC column with a particle size of 5 μm (150 mm x 4.6 mm) was used. The mobile phase was composed of methanol and 10mM potassium dihydrogen phosphate at a volume ratio of 70:30, respectively, with a pH of 6.8. The mobile phase was filtered through 0.45 μm membrane filters and was degassed before use.
The separation was carried out at room temperature (25 °C), at a flow rate of 1 mL/min, injection volume of 25 μL, and detection wave length of 267 nm.
A stock solution of PGZ with a concentration of 200 μg/ml was prepared by dissolving 10mg in 100 mL of methanol. Different standard solutions with concentrations ranging from 0.1 to 200 μg/ml were prepared by diluting specific volumes of stock solution using mobile phase.
Validation of HPLC Method
The developed HPLC method for PGZ was validated according to the ICH guidelines. Validation included:
-
A)
Linearity
Linearity of the developed HPLC method was assessed by injecting freshly prepared standard solutions of PGZ (0.1–200 μg/ml in the mobile phase) into the HPLC system. The experiment was repeated six times, and calibration graphs were constructed by plotting the mean HPLC area under the curve versus the concentration of PGZ in each standard.
-
B)
Accuracy and Precision
The developed HPLC method’s accuracy and precision were examined by replicating injections (n = 6) of three standard solutions of PGZ at a concentration of 0.5, 40, and 150 μg/ml. The samples were injected daily for three different days. The % accuracy was calculated from the measured PGZ concentration concerning its actual concentration. The relative standard deviations (%RSD) were calculated for each standard solution intra- and inter-daily.
-
C)
Specificity
The specificity of the developed HPLC method was assessed to examine whether there is any potential interference between the peaks of excipients present in the formulation the peak of the drug. This was done by injecting a placebo solution containing all the possible sample ingredients except the drug and comparing the HPLC chromatograph of this placebo solution with PGZ solution.
-
D)
Detection and Quantification Limits
The detection limit (DL) and quantification limit (QL) of the HPLC method were calculated from the slope of the calibration curve (S), which was obtained as described in section 2.3.1.2, and the standard deviation of the response (σ) of 6 blank samples, according to the following equations (73):
High-Performance Liquid Chromatography Results
Development of HPLC Method
A modified HPLC method for PGZ was developed based on the method of Akkala et al (29). The typical HPLC chromatograph of PGZ is presented in Figure 13. PGZ was eluted at a retention time of 5 minutes that was considered to be very suitable. Almost similar retention time of PGZ was observed in the method previously developed by Akkala et al.
Validation of HPLC Method
-
A)
Linearity
The linearity of the calibration curve over a range of 0.1–200 μg/mL was assessed by plotting the mean HPLC area under the curve versus the concentration of PGZ (Figure 14). The correlation coefficient (R2) of the observed curve was found to be 0.9995, which indicates the linearity of the HPLC method.
-
B)
Specificity
The specificity of the developed HPLC method was assessed by injecting a placebo solution containing all the possible sample ingredients except the drug (namely: PVP, ethanol, DMF, DMSO and Transcutol® P) and comparing the HPLC chromatograph of this placebo solution with that of PGZ solution. As shown in the HPLC chromatograph of this placebo solution (Figure 15), no interference peaks were observed or close to the drug's retention time.
-
C)
Accuracy and Precision
The developed HPLC method’s accuracy and precision were examined by replicating injections (n = 6) of three standard solutions of PGZ at a concentration of 0.5, 40, and 150 μg/ml. The intra- and inter-day accuracy and precision results for the HPLC method are presented in Table III.
The intra-day %recoveries were ranged from 95.8 to 100.8%, and the inter-day %recoveries were ranged from 95.02 to 100.51%. All %recovery values were within the acceptance criteria (90–110%), which indicates that the method is accurate (74). The intra-day %RSD ranged from 0.11 to 0.75%, and the inter-day %RSD ranged from 0.82 to 1.28%. All %RSD values were within the acceptance criteria (≤ 2%), indicating that the method is precise (73).
-
D)
Detection and Quantification Limits
The detection limit (DL) and quantification limit (QL) of the HPLC method were calculated from the slope of the calibration curve obtained in Figure 14 and the standard deviation of the response for six blank samples as described in equations 8 and 9, respectively. The detection limit was 0.022 μg/mL, and the quantification limit was 0.067 μg/mL.
Rights and permissions
About this article
Cite this article
Obaidat, R., Shameh, A.A., Aljarrah, M. et al. Preparation and Evaluation of Polyvinylpyrrolidone Electrospun Nanofiber Patches of Pioglitazone for the Treatment of Atopic Dermatitis. AAPS PharmSciTech 23, 51 (2022). https://doi.org/10.1208/s12249-021-02204-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02204-6