Abstract
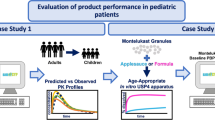
This study investigated the impact of gastro-intestinal fluid volume and bile salt (BS) concentration on the dissolution of carbamazepine (CBZ) immediate release (IR) 100 mg tablets and to integrate these in vitro biorelevant dissolution profiles into physiologically based pharmacokinetic modelling (PBPK) in pediatric and adult populations to determine the biopredictive dissolution profile. Dissolution profiles of CBZ IR tablets (100 mg) were generated in 50–900 mL biorelevant adult fasted state simulated gastric and intestinal fluid (Ad-FaSSGF and Ad-FaSSIF), also in three alternative compositions of biorelevant pediatric FaSSGF and FaSSIF medias at 200 mL. This study found that CBZ dissolution was poorly sensitive to changes in the composition of the biorelevant media, where dissimilar dissolution (F2 = 46.2) was only observed when the BS concentration was changed from 3000 to 89 μM (Ad-FaSSIF vs Ped-FaSSIF 50% 14 BS). PBPK modeling demonstrated the most predictive dissolution volume and media composition to forecast the PK was 500 mL of Ad-FaSSGF/Ad-FaSSIF media for adults and 200 mL Ped-FaSSGF/FaSSIF media for pediatrics. A virtual bioequivalence simulation was conducted by using Ad-FaSSGF and/or Ad-FaSSIF 500 mL or Ped-FaSSGF and/or Ped-FaSSIF 200 mL dissolution data for CBZ 100 mg (reference and generic test) IR product. The CBZ PBPK models showed bioequivalence of the product. This study demonstrates that the integration of biorelevant dissolution data can predict the PK profile of a poorly soluble drug in both populations. Further work using more pediatric drug products is needed to verify biorelevant dissolution data to predict the in vivo performance in pediatrics.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dissolution is commonly used as an in vitro testing method for orally administered drug products, such as tablets. Typically, biopredictive dissolution methods can use biorelevant media that is designed to simulate the composition of gastrointestinal (GI) fluids, such as fasted state simulated gastric fluid (FaSSGF) and fasted state simulated intestinal fluid (FaSSIF) which are both derived from the characterization of healthy adults GI media composition (1, 2). However, the solubility of drug substances (and hence dissolution profiles of oral drug products) in pediatric GI fluid may be different from those in adults due to inherent differences in GI fluid volume (3) and composition, for example in terms of bile salt (BS) concentrations (4).
Biorelevant pediatric Ped-FaSSGF media has been proposed previously, based on literature-reported BS concentration (5, 6), where values were lower in neonates (20 µM) and infants (60 µM) in comparison to adults (80 µM). Moreover, due to the lack of accurate data on pediatric BS concentrations, simulated Ped-FaSSIF media with BS concentrations corresponding to 50 and 150% (1.5 and 4.5 mM) of adult content (3 mM) were proposed as an alternative media for exploratory studies (5). Recent studies that characterized pediatric gastric and intestinal fluids measured a lower BS concentration in pediatric fasted state intestinal fluids compared to adults (0.18 mM vs 3 mM) (4, 7,8,9) providing new data on which pediatric simulated media can be developed.
The volume of dissolution media is a critical factor in designing the in vitro dissolution method for poorly soluble drug substances. Generally, the recommended dissolution volume in USP I/II apparatus is 500 mL, which more closely resembles the GI volume in adults (10). The volume of fluids in pediatric populations has been reported in two recent studies where the fasted gastric volume was reported to be a maximum of 8 mL in a population from 0 to 16 years (n = 32) (3) although an alternative study suggested a median volume of 5.0 mL in infants and 26.6 mL in adolescents (11). The corresponding fasted state intestinal fluids were reported to reach a maximum of 51 mL in a population from 0 to 16 years (n = 32) (3) or have a median volume of 23.9 mL in infants and 62.9 mL in adolescents (11). When considering the dissolution volume to use, an important consideration is the fluid volume administered with a tablet which is typically 240 mL in adults whereas previous data on relative bioavailability studies suggest a volume of 120 mL in children (12, 13).
Physiologically based pharmacokinetics (PBPK) modeling uses mathematical models and simulations to combine animal or human physiological data with drug characteristics to mechanistically describe the PK behaviors of a drug (14). PBPK has been particularly useful in pediatric drug development as it can factor ontogeny into relevant predictions (15,16,17), making quantitative predictions in pregnancy and in the fetus (18, 19), and in examining pediatric predictions in drug absorption in varying age groups (20). PBPK models can also incorporate in vitro dissolution data to predict the in vivo performance of oral formulations and to verify the clinical relevance of in vitro dissolution data (21,22,23). The identification of a biopredictive dissolution method for pediatric populations and subsequent integration of the generated dissolution data into PBPK modeling would aid in de-risking pediatric clinical programs, specifically with reference to relative bioavailability studies or bioequivalence (BE) studies for generic drug products. Furthermore, virtual bioequivalence (VBE) trials using PBPK modeling could provide a powerful tool to predict and compare the in vivo performance of test drug products and reference listed drug (RLD) products by integrating the dissolution data generated by using the biorelevant medias and the inclusion of inter-subject variabilities.
Carbamazepine (CBZ) is an anti-convulsant drug used in adults/pediatric populations to control seizures and as a mood-stabilizing drug in patients suffering from bipolar disorder (trigeminal neuralgia), attention-deficit hyperactivity disorder (ADHD) and schizophrenia (24, 25). The solubility of CBZ in water was measured to range from 0.14 to 0.27 mg/L at 25°C (26) According to the Biopharmaceutics Classification System (BCS), CBZ is a BCS class II (poorly soluble; highly permeable) compound where dissolution is the rate limiting factor for its absorption (27). Due to its high pKa (11.8 or 14), no ionization of CBZ is expected within the physiological pH range (28). A previous study (5) showed that CBZ solubility in neonatal or infant FaSSGF, where the BS concentration was, respectively, 25% (20 µM) or 75% (60 µM) of adult values (80 µM), was significantly reduced at the lower BS concentrations. However, the impact on solubility of CBZ upon varying the BS concentration in FaSSIF media from 50 to 150% (1.5–4.5 mM) was not significant (29). The impact of gastric fluid volume (135 mL in neonates, 120 mL in infants) on the dissolution of the reference product, Tegretol© (carbamazepine) 200 mg tablets, was reported using the USP4 Flow-through-apparatus and media volumes selected to match those in neonates and infants. In all cases, dissolution was incomplete due to volume-limited dissolution (29). No data is available on dissolution of CBZ pediatric suspensions which may be the more commonly used dosage form for such young patients.
To better understand the impact of biorelevant dissolution conditions on the release of CBZ from a tablet formulation and to integrate these dissolution profiles into PBPK software to evaluate the impact on the predicted PK profile in pediatric and adult populations, this work seeks to explore the following objectives:
-
To compare in vitro dissolution profiles of CBZ IR tablets using industry recommended USP media as well as biorelevant simulated adult and pediatric medias.
-
To explore the impact of dissolution media volume on the dissolution profiles of CBZ tablet.
-
To compare the dissolution profiles of the RLD and generic CBZ 100 mg IR tablets using USP media, adult biorelevant, and our new proposed pediatric biorelevant media for PBPK-based virtual BE testing.
-
PBPK model development and validation for CBZ to identify the absorption factors that could result in bioinequivalence between pediatric and adult populations or between branded or generic CBZ product by integrating the biorelevant dissolution data into a CBZ PBPK model.
Materials and Methods
Chemicals
Bile Salts
Cholic acid (CA); glycocholic acid (GC); glycochenodeoxycholic acid (GCDC); glycodeoxycholic acid (GDC); glycoursodeoxycholic acid (GUDC); taurocholic acid (TC); taurochenodeoxycholic acid (TCDC); taurodeoxycholic acid (TDC); tauroursodeoxycholic acid (TUDC); taurolithocholic acid (TLC); deoxycholic acid (DC), lithocholic acid (LC), and ursodeoxycholic acid (UDC) were purchased from either Sigma Aldrich (Gillingham, UK) or Acros Organics (Fisher Scientific, Loughborough, UK).
CBZ powder, sodium-lauryl-sulfate (SLS), lecithin, pepsin, acetonitrile HPLC grade, sodium hydroxide (NaOH), and hydrochloric acid (HCL) were purchased from Sigma Aldrich (Gillingham, UK). Biorelevant powder (Ad-FaSSGF/Ad-FaSSIF) was purchased from Biorelevant (https://biorelevant.com/; London, UK).
Tegretol© 100 mg tablets (Novartis Pharmaceuticals UK Limited, Batch No-B00964; Exp-07/2023) were used as RLD and Carbamazepine Medreich 100 mg tablets (Medreich PLC, Feltham, UK) as a generic product. Tegretol© was purchased from Queen Elizabeth Hospital Pharmacy (Birmingham, UK) and generic product from New Castle Healthcare NHS pharmacy.
Preparation of Dissolution Media
USP Media
SLS (1% w/v) was added to Milli-Q Type-1 (18.2 MΩ cm–1) water and stirred at 40°C for 2 h. The pH was adjusted to enable comparison with biorelevant dissolution media. The pH of the USP media was adjusted (but not buffered) to either 1.2 (to mimic gastric pH) by adding 0.1 N HCl or to 6.5 (to mimic intestinal pH) by adding 0.1 M NaOH before use. All pH-adjusted USP dissolution media were prepared on the day of the experiment and used within 4 h of preparation (30, 31).
Adult Biorelevant Media
Ad-FaSSGF.V2 (pH 1.2) and Ad-FaSSIF.V2 (pH 6.5) (9, 32) were prepared according to the protocol provided by the supplier, Biorelevant (London, UK). The pH of the media Ad-FaSSGF.V2 was adjusted (but not buffered) to either 1.2 by adding 0.1 N HCl or to 6.5 by adding 0.1 M NaOH before use. Media was used within 48 h of preparation. FaSSIF V2 media is the most widely used simulated intestinal fluid despite more recent versions and reviews of further characterization of adult intestinal fluids (8, 32, 33).
In the literature, FaSSGF-V2 has a pH value of 1.6, but we modified it to pH 1.2 for this study as described above. The traditional medium to simulate gastric conditions in the fasted state was USP simulated gastric fluid (SGF) which has a pH of 1.2. Note that due to the pH independent solubility of CBZ, this slight difference in pH would not have a significant impact on this study (34). In addition to this, a range of ~ 1 to 3 has been reported for gastric pH in fasted healthy humans after they have ingested a glass of water (35).
In this study, Ad-FaSSGF contained taurocholate to represent the bile salt concentration (0.08 mM), phospholipids (0.02 mM), sodium (34 mM), and chloride (59 mM). The Ad-FaSSIF media contained taurocholate (3 mM), phospholipids (0.75 mM), sodium (148 mM), chloride (106 mM), and phosphate (29 mM).
Pediatric Biorelevant Media
Ped-FaSSGF/FaSSIF (14BS) Media
Ped-FaSSGF containing 14 bile salts (14BS) and Ped-FaSSIF (14BS) were prepared based on the median concentrations (mM) (0.016 mM for Ped-FaSSGF and 0.178 mM for Ped-FaSSIF) of bile acids present in the gastric or intestinal fluid samples aspirated from children reported previously (4). All the ingredients listed in Supplementary Table S1 were added to Milli-Q Type-1 (18.2 MΩ cm–1) water and stirred for 2 h until completely dissolved; the pH of each media was then adjusted to either 1.2 by adding 0.1 N HCL or to 6.5 by adding NaOH before use. Ped-FaSSGF and Ped-FaSSIF were stored at 8°C and used within 48 h of preparation.
Ped-FaSSGF/FaSSIF (50% 14BS) Media
This media was prepared to contain 50% of the concentration of each BS reported previously (4) by diluting the Ped-FaSSGF/FaSSIF media containing the 14 BS with Milli-Q Type-1 water. As a result of dilution, the concentration of other components such as sodium chloride, lecithin, and pepsin was also reduced to 50% of the originally reported concentration. Finally, the pH of the prepared 50% 14BS media was adjusted to either pH 1.2 or 6.5 by adding 0.1 N HCL or NaOH, respectively. This 50% version was included to provide a “worst-case” scenario as there was large variability in the measured bile salt concentrations from the GI fluids of pediatric participants (4).
Ped-FaSSGF/FaSSIF (Na TCA) Media
Ad-FaSSGF and Ad-FaSSIF contained only a single bile salt, Na TCA (3 mM in Ad-FaSSIF; 0.08 mM in Ad-FaSSGF); therefore, Ped-FaSSGF/FaSSIF media containing only Na TCA were also prepared. Na TCA concentrations mimicked the total bile acid concentration found in the 14 BS pediatric media.
High Performance Liquid Chromatography (HPLC) Method Development
HPLC methodology was based on previous methods (36, 37) where the accuracy and specificity were previously reported. In brief, HPLC analysis of CBZ was carried out using an Agilent (1260 infinity 2) HPLC equipped with binary pump, DAD detector UV at 285 nm, and C18 column (Ascentis: 25 cm, 5 µm, 4.6 mm). The mobile phase was water and acetonitrile at a ratio of 6:4 (v/v) which ran in isocratic mode at a flow rate of 1.0 mL/min. The injection volume was 5 µL, and the run time was 10 min (min), followed by 1-min post run to avoid any co-elution or carry-over of the analyte.
Calibration Standards
CBZ Calibration standards (0.002–1 mg/mL) were prepared in all the different adult/pediatric FaSSGF/FaSSIF media to exclude any interference or matrix effect (CBZ HPLC peak and calibration standards provided in Supplementary Figures S1A to S1K).
In Vitro Dissolution Study
Dissolution studies were conducted in accordance with USP dissolution (General chapter 711) guidelines (38) using USP apparatus 2 (Copley Scientific, Nottingham, UK). The temperature of dissolution medium in vessels was maintained at 37.0°C ± 0.5°C. Six replicates/units were used for each experiment. The size of the dissolution vessel was changed for smaller volumes (200 mL, 100 mL, and 50 mL) to match the hydrodynamics of the standard vessels. To scale down the volumes, low-volume conversion kits (Copley, UK) comprising vessels of either 100- or 200-mL capacity with appropriate mini-paddles, vessel cover, and centering ring assemblies were used. One mL of dissolution medium was withdrawn without replacement at each pre-specified time point (15, 30, 60, 90, 120, and 150 min) and filtered using Agilent’s 13-mm syringe filters (polypropylene 0.45 µm pore size) before analysis using the validated HPLC method. A summary of the dissolution conditions is presented in Supplementary Table S2. The dissolution studies were all conducted using a 100 mg CBZ tablet. This tablet strength is not available in the USA but is available in the UK (25). This strength was selected to use the lowest dose to be applicable to pediatric populations and also to minimize the solubility effects when evaluating the dissolution conditions (30); the lower strength enabled the maximum discrimination between the dissolution conditions and also accounts for the high permeability of CBZ to best enable integration into the PBPK modeling software.
Dissolution Data Analysis
Similarity between two dissolution profiles was determined by the difference factor (F1) and similarity factor (F2) (39) calculated as follows:
where Rt = Dissolution (% label claim) for reference (R) formulation at time t
- T t :
-
Dissolution (% label claim) for test (T) formulation at time t.
- n :
-
number of time points
Generally, three or more dissolution sampling timepoints with one measurement after 85% dissolution are required to calculate F1 and F2. The compared dissolution profiles are considered similar when F1 ≤ 15 and F2 ≥ than 50.
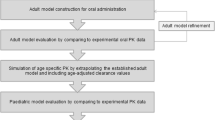
CBZ PBPK Model
A PBPK model for CBZ was developed using SimCyp® Simulator (Version 21, Release 1; Certara UK Limited, Sheffield, UK) that incorporated drug-dependent and system-related input parameters obtained from SimCyp’s internal compound library (Supplementary Table S4). The in vitro dissolution datasets generated in the “In Vitro Dissolution Study” section were incorporated into SimCyp® Simulator Advanced Dissolution, Absorption and Metabolism (ADAM) model; full details of the dissolution data that was integrated are provided in Supplementary Table S3.
The dissolution profiles using various BS concentrations and dissolution volumes were integrated into SimCYP according to the methods previously described by Guimaraes (2002) (40). In brief, a single-stage fasted intestinal profile (FaSSIF dissolution conditions as an intestinal profile) was integrated as the “intestinal profile.” Using this approach, the software considers the same dissolution profile for the stomach and intestinal compartments (FaSSIF dissolution conditions). A second scenario was also included where both the single-stage fasted gastric and intestinal profiles (input of the CBZ single-stage dissolution profile in fasted state simulated gastric fluids (FaSSGF) entered as “stomach profile” and single-stage dissolution profile in fasted state simulated intestinal fluids entered as “intestinal profile” thus incorporating both FaSSGF + FaSSIF dissolution conditions.
Model prediction was validated using published clinical PK studies with CBZ (Tegretol© IR 100 or 200 mg) conducted in an adult population (41,42,43,44). Note that, here, the term validation is used as defined by Kuemmel 2019, “Process of determining the degree to which a model or simulation is an accurate representation of the real world.” In other terms, “validation relates to model (model form, model inputs), comparator (test samples, test conditions), and assessment (equivalency of input parameters, output comparisons)” (45).
SimCyp Pediatric Version 21 (Release 1) was used as the pediatric PBPK (ped-PBPK) modeling platform. CBZ specific properties (including its metabolic clearance) used in the adult PBPK model (Supplementary Table S4) were transferred into the pediatric model (Supplementary Table S5). The metabolic clearance of CBZ is mediated by CYP3A4, CYP 3A5, and CYP2C8; hence, the ontogeny of CBZ-metabolizing enzymes in pediatric populations was expressed according to the following sigmoidal function (Eq. 3) which is a default equation used in SimCyp (46, 47).
where Fmax is the maximum adult relative expression, Fbirth is the relative expression of enzyme at birth, Age50 is the age at which the fractional expression (/activity) is in the middle of the birth and adult values, and n is the exponent related to the sigmoidicity of the developmental curve or analogous to the Hill coefficient.
In order to incorporate the age-dependent expression pattern of CYP3A4, CYP3A5, and CYP2C8 in the pediatric PBPK model, the time to reach 50% maturation (Age50) for each enzyme was used. The Age50 of hepatic and intestinal CYP3A4 maturation was 0.64 and 2.36 years, respectively (47,48,49). For CYP3A5, since no age-dependent change in hepatic expression was noted (50), no ontogeny for hepatic CYP3A5 was assumed in this study but for intestinal ontogeny, similar Age50 value (i.e., 2.36) of CYP3A4 was considered. For CYP2C8 ontogeny, Age50 of hepatic maturation was 0.366 years (51). A zero value was used for intestinal CYP2C8 ontogeny due to lack of abundance data (52).
Generally, young children have lower volume of distribution (Vss) for lipophilic drugs due to reduced body fat compared to adults. Due to lack of a volume of distribution (Vd) values in children, a Vd of 0.3 L/kg in young children (compared to 0.78–1.9 L/kg in adults) was estimated by our visual trial and error simulations in order to fit the pediatric PBPK model to the observed data (53). Moreover, the volume of fluid intake with CBZ tablet was changed to 120 mL for pediatric populations compared to 240 mL for adult populations in line with reported clinical protocols (13).
The CBZ model was validated in adults by calculating the prediction error percentage (PE%) fold error (FE), average fold error (AFE), and absolute average fold error (AAFE) for Cmax and AUC. The adult model was subsequently updated and applied to children (6–15 years) and further verified and validated using clinical PK data conducted in children on 20 mg/kg dose (n = 12) by Hartley (1991) (54) and 9.3 mg/kg dose (n = 6) by Bano (1986) (55) (Table III).
This PBPK model was also used to predict the plasma concentration profile of CBZ in pediatric populations younger than 6 years to better understand the potential differences in CBZ exposure between children younger and older than 6 years old when CBZ was administered as an IR suspension (prepared from crushed Tegretol© tablets) (56). CBZ doses of 17 and 19 mg/kg suspension were tested in 20.9 days new-born (n = 7; 3.2 kg; 25 mL water) and 5.1-year-old children (1.25–8 years; n = 5; 120 mL water), respectively (56). Based on the fraction absorbed (66%) from the IR suspension (42), the 66% was assumed to be dissolved for an IR suspension to run the simulations in younger (< 6 years) pediatric population. This assumption would be a limitation of model simulations, and any future dissolution work would help to further improve the model prediction.
Due to higher clearance values in younger children (57), a clearance value of 3.18 L/h (42) was used to run the model; the volume of distribution (Vss) was fitted (by visual observation of the superimposed predicted and observed datasets) (2.6 L/kg for 20.9 days new-born and or 2.850 L/kg for 5.1 years child) to capture the observed clinical datasets published in Rey (1979) study (56).
Virtual Bioequivalence (VBE) Studies
Preliminary exposure simulations were performed using the dissolution data generated in Ad-FaSSGF and Ad-FaSSIF 500 mL media for Tegretol© 100 mg IR tablets and the predicted PK profile was validated using literature data (Kohlman study (42); 200 mg IR tablet). Although the dissolution data was generated using 100 mg tablet, previous literature has reported that the dissolution of these IR tablets is similar to the 200 mg product used in the clinical study (54). So, the assumption of similar dissolution profiles for both 100 mg and 200 mg tablets was used for the simulation purposes.
VBE simulations were performed in a fully replicated, two treatment, multiple trials (N = 10) in a cross-over design with a sample size of n = 12,16, 24, 36, and 48 in healthy adults (18–45 years) (58). The number trials (N = 10) were fixed as per the SimCyp VBE protocol (23, 58). A single dose of CBZ IR tablets 100 mg was administered with 240 mL of fluids. For VBE simulation, the dissolution profiles for Tegretol© 100 mg and generic product 100 mg (Medreich) generated in Ad-FaSSGF and FaSSIF 500 mL were incorporated into the adult PBPK model. The default coefficients of variation (%CV) for accounting the inter-subject variability of the physiological parameters provided in the SimCyp database for the North European Caucasian healthy adult volunteers population were applied for each parameter.
For pediatrics, VBE simulations were performed with a sample size of 12, 16, 24, 36, and 48 healthy subjects (6.5–15 years, to match existing published clinical data sets) and a single dose of CBZ IR tablets 100 mg administered with 120 mL of fluids. Furthermore, the pediatric simulation outputs were validated using literature data (Hartley (1991); 20 mg/kg/day given as 100 or 200 mg tablets twice daily and Bano (1986); 9.3 mg/kg per day).
The input dissolution profile from the full suite of in vitro dissolution tests (Ad-FaSSGF and FaSSIF at 500/200/100/50 mL; Ped-FaSSGF and FaSSIF-14 BS at 200 mL or Ped-FaSSGF and FaSSIF-50% 14 BS at 200 mL or Ped-FaSSGF and FaSSIF-Na TCA at 200 mL) was integrated into the PBPK model to identify which profile gave the best match to the existing clinical data set from Hartley study (54).
Evaluation of Predictability of the PBPK Model
Prediction error for AUC and Cmax were evaluated by the following formula (14, 59, 60):
In this study, we considered a PE value of < 20% confirming the good predictability of the model. In addition, Fold error (FE) for AUC and Cmax were evaluated by the following equation (40, 59,60,61):
Furthermore, the mean predicted plasma concentration–time profiles were also assessed by the average fold error (AFE) and validated by the absolute average fold error (AAFE) (Eqs. 6 and 7 respectively) (40, 61).
where n denotes the number of observed PK sampling points, Predictedi is the predicted concentration at time point i, Observedi is the observed concentration at time point i.
The FE indicates the predictive accuracy of each data point as shown in equation (62). The AFE indicates whether the predicted profile underestimates (AFE < 1) or overestimates (AFE > 1) the observed values, as shown in Eq. 6, whereas the AAFE quantifies the absolute error from the observed values, as shown in Eq. 7. An AAFE value close to unity represents the precision of the simulations (62). When comparing the simulated data to clinical data, the populations were matched in terms of age range and sample size for each study.
Results
In Vitro Dissolution Data
The dissolution profiles of CBZ 100 mg tablets obtained using the pH-adjusted USP media (30) were compared with those obtained using biorelevant adult FaSSGF and FaSSIF media with a dissolution volume of 900 mL (Supplementary Figure S2).
When the dissolution profile from USP dissolution media 1% SLS (pH 1.2 and 6.5) was compared to Adult FaSSGF/FaSSIF profiles, a decrease in % of release for Tegretol© 100 mg tablets was observed. The major difference in these media is the surfactant type and concentration used; a 1% SLS media is a high surfactant concentration and perhaps it is unsurprising that such raid dissolution is observed compared to the biorelevant media. The results indicated that the pH of the media did not affect the overall dissolution.
The impact of media volume on dissolution was evaluated using both Ad-FaSSGF and Ad- FaSSIF media and the results are shown in Fig. 1a and b, respectively.
As expected for a poorly soluble drug like CBZ, reducing the volume of dissolution media resulted in decreased % drug release from the tablet formulation. However, the decrease in % release was not significant according to the F1/F2 statistic when the volume was reduced from 900 to 500 mL and from 100 to 50 mL. For both Ad-FaSSGF and Ad-FaSSIF media, the F1/F2 values are shown in Table I.
The impact of media composition on the dissolution of Tegretol© 100 mg tablets was further assessed in a 200 mL volume of both simulated pediatric gastric and intestinal media to mimic the pediatric GI fluid volume (Fig. 2a and b).
When 200 mL of media was used, based on F1 and F2 comparison, dissimilarity was observed between Ad-FaSSIF and Ped-FaSSIF 50% 14BS (Table II). This is likely resulting from the large differences in the BS concentration (3000 vs 89 µM).
In Vitro Dissolution Comparison Between Generic and RLD Product
Adult FaSSGF/FaSSIF (500 mL)
Dissolution of the RLD and generic product was compared in simulated adult GI media using a volume of 500 mL. The volume of 500 mL is consistent with in vivo studies where it is known that by ingesting 250 mL of water with the dosage form, plus the residual water in the adult GI tract that a maximum total volume of about 300–500 mL will be available in the proximal small intestine (1, 63, 64). Based on the F1/F2 criteria, the dissolution profiles of the two products were similar in Ad-FaSSIF (F1 = 6.5, F2 = 64.2), but not in Ad-FaSSGF (F1 = 21.7, F2 = 43.1) (Fig. 3). A similar conclusion was reached when the test was repeated in 200 mL simulated pediatric media (Fig. 4).
Pediatric FaSSGF/FaSSIF (200 mL)
Comparison of % of release between reference CBZ (Tegretol©) and generic (Medreich) 100 mg tablets in Ped-FaSSIF media containing 14 BS showed dissolution similarity between the two products (Fig. 4). At pH 1.2, comparison of both the reference and generic profiles showed differences (F1 = 34.8 and F2 = 43.0). It appears that CBZ generic has higher % release at gastric pH as compared to the reference drug.
Validation of Adult and Pediatric PBPK Model
Simulations conducted using the adult PBPK model captured the observed plasma time-concentration profiles for CBZ given as a single oral dose of 100 mg (41), 200 mg (41, 42), and 400 mg (as 2 × 200 mg) (42,43,44) in the fasted state. The model was simulated by incorporating the dissolution data generated by using Ad-FaSSGF and FaSSIF 500 mL media (Table III, Supplementary Figures S4A to S4F). All PE, FE, AFE, and AAFE values indicate successful predictions (AUC0-t PE: − 10.3 to 5.33%; Cmax PE: − 10.6 to 12.8%; AUC0-t FE: 0.90 to 1.05; Cmax FE: 0.89 to 1.13; AFE: 0.97 to 1.35; AAFE: 1.15 to 1.39) (Table III).
When dissolution profiles generated in 200 mL biorelevant media Ped-FaSSGF and FaSSIF (containing 14 BS) were incorporated into Ped-PBPK model to simulate in vivo dissolution conditions, the model predicted the observed PK parameters very well. All FE, AFE, and AAFE values indicate successful predictions (AUC0-t PE: 4.04 to 21.8%; Cmax PE: 2.97 to 6.48%; AUC0-t FE: 1.04 to 1.22; Cmax FE: 1.03 to 1.06; AFE/AAFE: 1.17 to 1.46 (Table III; Supplementary Figures S5 and S6).
For newborn (20.9 days) and young children (< 6 years), the model predicted plasma concentrations in good agreement with the observed PK datasets (Rey 1979). For newborn, the results showed AUC0-t PE: 9.52%; Cmax PE: 0.39%; AUC0-t FE: 1.10; Cmax FE: 1.0; AFE: 1.24 and AAFE: 1.33. For young children (5.1 years), the results showed AUC0-t PE: 10.1%; Cmax PE: − 3.68%; AUC0-t FE: 1.10; Cmax FE: 0.96; AFE: 1.14 and AAFE: 1.15 respectively (Table III).
Effect of Variations in Bile Salt Concentrations on the Predicted CBZ Plasma Exposure in a Pediatric Population
A comparison of the predicted PK profile based on the in vitro dissolution profiles from the full range of pediatric media (Ped-FaSSGF and FaSSIF 14 BS, Ped-FaSSGF and FaSSIF 50% 14 BS, Ped-FaSSGF and FaSSIF Na TCA, and Ad-FaSSGF and FaSSIF) at 200 mL was conducted. Simulations were also performed to mimic the adult biorelevant media at 200 mL where only Na TCA was used to prepare the medium. Table IV shows the PE, FE, AFE, and AAFE for each input dissolution profile to determine the most biopredictive dissolution conditions.
When the dissolution profiles generated in 200 mL biorelevant media Ped-FaSSGF and FaSSIF (containing 14 BS or 50% 14 BS) or Ped-FaSSGF and FaSSIF (containing Na TCA) were incorporated into Ped-PBPK model to simulate actual in vivo dissolution conditions, the model predicted the observed PK parameters reasonably well (AUC0-t PE: − 7.07 to 4.04%; Cmax PE: − 8.61 to 2.97%; AUC0-t FE: 0.93 to 1.04; Cmax FE: 0.91 to 1.03; AFE: 0.97 to 1.08; AAFE: 1.07 to 1.11) (Table IV; Supplementary Figure S8). Input dissolution profiles generated almost similar systemic exposure, so all the three dissolution profiles, in this instance, are biopredictive.
Effect of Various Dissolution Volumes on the CBZ Plasma Exposure
When USP 1% SLS (pH 1.2 and 6.5, 900 mL) dissolution profiles were incorporated into the adult PBPK model, the model over predicted the observed PK parameters of CBZ captured from various adult PK studies (41,42,43,44) (for majority of the PK studies, PE for AUC0-t and Cmax was > 20%; AUC0-t FE: 1.12 to 1.32; Cmax FE: 1.12 to 1.43; AFE and AAFE ranged between 1.37 and 1.93). However, the predictions were slightly improved for Ad-FaSSGF and FaSSIF 900 mL dissolution profiles; the PE value for AUC0-t and Cmax ranged between − 1.0 to 16.8% and − 1.06 to 24.8% respectively. The AFE (1.37–1.51) and AAFE (1.20–1.51) values indicated a slight overestimation of the mean PK parameters.
Simulations with Ad-FaSSGF and Ad-FaSSIF 500 mL dissolution datasets as input were in good agreement with observed data but with a small overestimation of the mean PK parameters (AUC0-t PE: < 6%; Cmax PE: ≤ 13%; AUC0-t FE: 0.90–1.05; Cmax FE: 0.89–1.13; AFE: 0.97–1.35, and AAFE: 1.15–1.39). Thus, the most predictive dissolution volume and media composition to forecast the PK was 500 mL of Ad-FaSSGF and Ad-FaSSIF media for adults.
Incorporation of Ad-FaSSGF and Ad-FaSSIF dissolution datasets at 200, 100, and 50 mL significantly underpredicted the observed plasma-concentration profiles (For 200 mL, AUC0-t PE: − 48.3 to − 54.1% and Cmax PE: − 40.8 to − 52.8%; for 100 mL, AUC0-t PE: − 72.0 to − 76.3% and Cmax PE: − 70.3 to − 76.3%; for 50 mL, AUC0-t PE: − 90.4 to − 91.9% and Cmax PE: − 89.5 to − 91.8%). All PE, FE, AFE, and AAFE values are provided in Supplementary Table S6 and figures for the impact of various dissolution volumes on CBZ exposures in observed PK studies are provided in Supplementary Figures S9-S12.
When 500 mL (Ad-FaSSGF and FaSSIF) dissolution profiles were incorporated into the pediatric PBPK model, the model over predicted the PK parameters of CBZ (AUC0-t PE: 126%; Cmax PE: 128%; AUC0-t FE: 2.26; Cmax FE: 2.28; AFE/AAFE: 2.26) compared to the clinically observed PK parameters (54) (Table IV; Fig. 5). A trend for 200 mL Ad-FaSSGF and FaSSIF dissolution datasets was close to pediatric 200 mL datasets (AUC0-t PE: 17.2%; Cmax PE: 18.8%; AUC0-t FE: 1.17; Cmax FE: 1.19; AFE/AAFE: 1.22). On the contrary, Ad-FaSSGF and FaSSIF 100 mL/50 mL under predicted the observed PK parameters (100 mL: AUC0-t PE: − 41.2; Cmax PE: − 40.6; AUC0-t /Cmax FE: 0.59; AFE: 0.60; AAFE: 1.66; 50 mL: AUC0-t PE: − 78.8; Cmax PE: − 79.2; AUC0-t /Cmax FE: 0.21; AFE: 0.22; AAFE: 4.45).
Plasma exposure of CBZ (IR 100 mg tablets) in pediatrics as a result of incorporating various dissolution datasets by changing the Ad-FaSSGF and FaSSIF dissolution media volumes from 500 to 50 mL and comparison to Ped-FaSSGF and FaSSIF 200 mL dissolution datasets. Observed clinical data from Hartley (1991) study
In Vitro Tests and Virtual Bioequivalence (VBE) Simulation in Adults and Pediatrics for CBZ (Tegretol.© 100 mg Tablets -Novartis vs CBZ Generic 100 mg Tablets -Medreich)
Virtual simulations performed in healthy adults using the Ad-FaSSGF and FaSSIF 500 mL dissolution datasets for both the RLD and generic product confirmed their BE as the Geometric mean ratios (GMR) for the AUC and Cmax lay between 0.8 and 1.25 (Table V; Supplementary figures S13A). For pediatric populations, when simulations were performed using Ped-FaSSIF (14 BS) 200 mL dissolution datasets or both the Ped-FaSSGF and Ped-FaSSIF 200 mL datasets for both the RLD and generic product, the AUC and Cmax values for both the reference and test product were found to lie between 0.8 and 1.25 (Table V; Supplementary figures S14A).
Discussion
The first objective of this research work was to explore biopredictive dissolution methodology by comparing the dissolution of CBZ (100 mg) IR tablets in the industry recommended compendial method (1% SLS, USP-2 paddle apparatus at 75 rpm in 900 mL) with the biorelevant dissolution medias. Our results suggested complete dissolution of 100 mg CBZ in 1% SLS at pH 1.2 and 6.5, respectively. This is in agreement with a previous study (30) which showed complete release from CBZ 100 mg IR tablet in 1% SLS media within 60 min. The solubility of CBZ is increased tenfold by the addition of 1% SLS to water and by 1.7 times in the presence of 17.3 mM Na TCA as a bile salt (65).
According to a previous study, the differences in solubility enhancement are likely to be due to surfactant’s concentration in the media relative to their critical micelle concentration (CMC) (66). The CMC values for CBZ in the presence of SLS in water at 25°C is 0.0079 mM (67) and in the presence of BS is 2–12 mM (68) indicating that SLS provides greater solubilising capacity compared to the BS. This is true with our datasets where % release was found to be faster and more complete in the presence of SLS as compared to achieving 91% release in Ad-FaSSGF 900 mL media, and 94% in Ad-FaSSIF media. Dissolution in Ad-FaSSIF media in comparison to Ad-FaSSGF media is slightly higher and is attributed to the higher concentration of bile salts present in the FaSSIF media which lowers the surface tension and enhanced increased tablet wetting (69, 70). CBZ’s dissolution is pH independent due to its neutral charge. This is further supported by the literature-based solubility values for CBZ in biorelevant medias (Supplementary Materials Table S7). Two studies (42, 71) reported solubility values for CBZ in FaSSGF and FaSSIF media (142/208.7 mg/L in FaSSGF; 146 or 233.6 mg/L in FaSSIF).
Decreasing the dissolution volume (from 900 to 50 mL) to mimic variations in GI fluid volume of pediatric patients to reflect values identified in a study of children aged 0–16 years (4) showed a decrease in the rate and extent of dissolution of CBZ% released from 91 to 5% in Ad-FaSSGF and 94 to 8% in Ad-FaSSIF media. Hence, CBZ dissolution was shown to be sensitive to changes in volume; this is important when extrapolating from adult to pediatric populations. However, it should be noted that the dose will also be changed when moving from adult to pediatric populations; for CBZ, the oral dose in adults is usually not more than 1000 to 1600 mg per day, and in children (6–12 years), the dose is not more than 1000 mg per day. Moreover, caution is required when the dose is bridged from adults to children especially for narrow therapeutic index (NTI) drugs such as CBZ. Due to the poor solubility of CBZ and low volume of GI fluids, there is a risk of precipitation of CBZ along with the excipients leading to sub-therapeutic levels for CBZ. During in vitro dissolution experiments, visual observations indicated turbidity or precipitation of poorly soluble CBZ or excipients especially in lower volume dissolution medias (50 to 200 mL), and this is in agreement with the previously published work where the study observed CBZ precipitated due to formation of dihydrate crystals with a needle-shaped morphology (65, 72). We recommend further studies to explore the precipitation rate of CBZ in the presence or absence of multiple BS species.
Comparison of all the three pediatric medias (14 BS, 50% 14 BS or Na TCA) showed similar dissolution profiles (F1 < 15, F2 > 50%). This is also true when Ad-FaSSGF and FaSSIF 200 mL medias compared to the pediatric medias. However, dissimilarity was observed only between Ad-FaSSIF and Ped-FaSSIF 50% 14BS which might be due to the large difference in bile salt concentrations (3000 vs 89 µM). Hence, pediatric biorelevant medias can be formulated by using only single bile salt such as TCA which makes manufacture simple. Kohlman (42) reported the solubility of CBZ as 208.8 ± 3.9 mg/L and 206.3 ± 10.9/234.9 ± 4.3 mg/L in neonate-FaSSGF (0.02 mM Na TCA) and P-FaSSIF-50%/ P-FaSSIF-150% respectively. This literature data is in agreement with the data in this study where CBZ solubility, like dissolution, is relatively insensitive to bile salt concentration within these ranges (73). Previous literature has reported that there is not a well-defined CMC for FaSSIFv2 but a total concentration of TCA and lecithin between 2 and 3 mM is required; thus, the range of media used will encompass this range with the pediatric media having concentrations below the anticipated CMC (8). However, caution is required while extrapolating the dissolution profile from Ad-FaSSIF media to Ped-FaSSIF media containing significantly lower concentrations of BS.
Comparison of RLD and generic 100 mg tablets in Ad-FaSSIF 500 mL and Ped-FaSSIF 200 mL showed similar profiles (Supplementary Fig. 13A and Supplementary Fig. 14A) but it is worth noting that differences in profiles for the test and innovator were only seen in Ad-FaSSGF (F1 = 17.8, F2 = 43.1) and Ped-FaSSGF (F1 = 25.9, F2 = 43) medias in a high-stressed situation of low volume and lower BS concentrations. However, this discrepancy is unlikely to cause any significant changes in plasma exposure as there are limitations in USP 2 apparatus which include the non-continuous dissolution/absorption system mimicking GI physiology and this may or may not be clinically relevant as most absorption occurs in the small intestine (74, 75).
Incorporation of USP 1% SLS 900 mL (pH 1.2 and 6.5) and Ad-FaSSGF and Ad-FaSSIF 900 mL in the validated Ad-PBPK model showed slight overestimation of the observed PK parameters but were well within the observed clinical PK variabilities. Ad-FaSSGF and Ad-FaSSIF at 500 mL, the predicted plasma concentration profiles matched well with the observed PK parameters. Ad-FaSSGF and Ad-FaSSIF dissolution volumes from 200 to 50 mL poorly predict the observed healthy adult PK parameters. Hence, any media at either 900 or 500 mL could be used for testing adult generic products.
Further incorporation of adult dissolution datasets (Ad-FaSSGF and Ad-FaSSIF dissolution volume from 500 to 50 mL) in the validated Ped-PBPK model showed that the adult media tended to over predict exposure compared to the data from the pediatric media due to higher BS concentrations, and data also suggested that the dissolution data from 200 mL Ped-FaSSGF and FaSSIF 14 BS media was closest to the pediatric clinical data (Hartley 1991) although a slightly lower volume may have provided a more accurate prediction (Fig. 5). Thus, dissolution data from 200 mL pediatric media mapped well to the observed clinical data although it should be noted that the literature data that was used to demonstrate prediction required the participants to take 120 mL liquid with their CBZ tablet. In practice, the volume used in pediatric populations may be lower and as such a reduced volume should be used to assess risk on overall exposure.
Incorporation of an alternative pediatric medias (Ped-FaSSGF and FaSSIF 14 BS, 50% 14 BS or Na TCA) into the ped-PBPK model showed that all the three dissolution profiles mapped well to the observed pediatric clinical data (Supplementary Figure S8), and interestingly, all the three profiles were well within the observed clinical PK variabilities. This implies that any pediatric media can be used for testing the in vivo performance of the CBZ product for pediatric patients, but we recommend expanding the biorelevant dissolution series of case studies for a wider proportion of pediatric drug/drug products which are sensitive towards pH changes across the GI tract. It should be noted that there can be many dissolution conditions where the resulting profiles happen to generate similar disposition, but later fail in predictions for one reason or another. Therefore, further work on a wider range of dissolution testing conditions may provide more reassurance on the critical parameters.
For the CBZ tablet case, even though the dissolution of the Tegretol©/generic product was not similar (according to the F1/F2 values) to the branded drug profile in the FaSSGF media for either adults or pediatrics which might be due to low BS levels and poor mixing of the dissolution apparatus may have exacerbated small changes that would be negligible in the GI physiology. However, when incorporated into PBPK model for virtual testing both products were found to be bioequivalent. This is anticipated as any undissolved drug in gastric fluid will transit to the intestinal fluid which it could further undergo dissolution and absorption (75). The VBE simulation results showed narrow 90% confidence intervals for PK parameters which might change if VBE trials accounted for observed intraindividual or with-in subject variability (WSV) as these factors are mainly attributed to drug-related GI absorption due to variations in residual gastric volume, low aqueous solubility, low oral bioavailability, high acid lability, and extensive first-pass metabolism (58, 76, 77). Implementation of WSV in our VBE trials is lacking as the WSV for most of the GI parameters and their % co-variations are not available (58). However, future studies are warranted to integrate WSV data into VBE trials to minimize the risk of false positive or false negative results in BE studies.
The simulation methods presented in this study will be useful in the prediction of actual in vivo dissolution conditions of poorly soluble drugs by using biorelevant media in in vitro testing. Incorporation of bio-relevant dissolution data for both the adult and pediatric population helped to explore and account for both population variabilities in terms of differences in GI fluid volumes as well as the differences in BS concentrations in the GI fluid medias.
In this research work, we prepared the Ped-FaSSGF and Ped-FaSSIF media by characterizing the gastric and intestinal fluids from our previous research work (4). There are few caveats in using the proposed pediatric media as the fluid composition (bile salts) were based on characterization of GI fluid collected from pediatric patients undergoing diagnosis for GI-related diseases. Furthermore, no information on prandial state in those pediatric patients was available. However, the study results used in this study could provide an initial indication of general trends of BS concentrations in pediatrics and their impact on the dissolution of poorly soluble drugs. The pH of the FaSSGF media for both adult and pediatric media used in this study is slightly lower (pH 1.2) than the literature reported pH value of 1.6 (32). However, a recent review indicated that the mean gastric pH values in healthy newborns (1.5–5.3) with high interindividual variability but pH for pre-school (2.0–2.2) and school-going children (1.7) is similar to healthy adults (1.4–3.3). However, this slight change in pH and its impact on solubility of the neutral drugs are negligible. There are recent reviews (78, 79) providing the details to pediatric GI physiology that could be used to improvise the composition and physicochemical characteristics of pediatric medias, but larger dataset would be needed to further characterize the healthy pediatric GI fluid.
This study used a single generic product to compare the CBZ dissolution profile to an innovator with similar dissolution profiles for a proof-of-concept study. We were unable to source the same batch of the two products (generic and Tegretol©) used in the pediatric clinical study (Hartley 1991). It would be ideal to compare the same batches in the in vitro study to those used in the in vivo study. Here, the clinical data was used to verify the pediatric PBPK model as the clinical equivalence of the product would have had to be demonstrated to achieve the licensed status. Studies including a wider range of generic products to test dissolution in the proposed or improvised pediatric medias and predict the pediatric relative bioavailability or BE dataset for these generic products would be warranted.
The work presented in this study is limited to a single model drug, CBZ. Further work using more pediatric drug products is needed to better understand and verify biorelevant dissolution data to be used to predict the in vivo performance in pediatric populations. Ideally, the clinical BE study should provide the % CV for the inter-subject variability of the physiological parameters. Due to lack of these datasets, the Adult PBPK model for BE testing used the SimCyp default % CV used in the North European Caucasian healthy adult volunteers population. Generally, the model should use inter- and intra-subject variabilities and match what were obtained from clinical studies.
Conclusion
The use of biorelevant GI volumes and fluid composition in dissolution testing provided superior predictions of PK profiles of CBZ in pediatric populations compared to the use of adult biorelevant conditions. The most predictive dissolution data for integration into the pediatric PBPK model was 200 mL pediatric media (Ped-FaSSGF and Ped FaSSIF) irrespective of bile salt concentration or components used to represent the bile salts. The dissolution profiles in pediatric media are close to that of Ad-FaSSGF and Ad-FaSSIF 200 mL dissolution datasets, and the use of the existing Ad-FaSSGF and Ad-FaSSIF media may be preferred (at lower volumes) as these are recognized media across scientific and regulatory communities and are also readily available products. The use of lower dissolution volumes must be considered in the testing and risk assessment of pediatric medicines. However, the work needs to be extended to incorporate additional case studies in order to determine the most suitable dissolution conditions for a wider range of drug products.
VBE simulations were performed for two CBZ products (RLD and generic) by incorporating the adult and pediatric biorelevant dissolution datasets generated separately for both the products in a cross-over multiple trials design and were validated against observed plasma profiles. In both the populations, plasma exposure for both the product was found to be bioequivalent.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Klein S. The use of biorelevant dissolution media to forecast the in vivo performance of a drug. AAPS J. 2010;12(3):397–406. https://doi.org/10.1208/s12248-010-9203-3.
Mann J, Dressman J, Rosenblatt K, Ashworth L, Muenster U, Frank K, et al. Validation of dissolution testing with biorelevant media: an OrBiTo study. Mol Pharm. 2017;14(12):4192–201. https://doi.org/10.1021/acs.molpharmaceut.7b00198.
Papadatou-Soulou E, Mason J, Parsons C, Oates A, Thyagarajan M, Batchelor HK. Magnetic resonance imaging quantification of gastrointestinal liquid volumes and distribution in the gastrointestinal tract of children. Mol Pharm. 2019;16(9):3896–903. https://doi.org/10.1021/acs.molpharmaceut.9b00510.
Pawar G, Papadatou-Soulou E, Mason J, Muhammed R, Watson A, Cotter C, et al. Characterisation of fasted state gastric and intestinal fluids collected from children. Eur J Pharm Biopharm. 2021;158:156–65. https://doi.org/10.1016/j.ejpb.2020.11.010.
Maharaj AR, Edginton AN, Fotaki N. Assessment of age-related changes in pediatric gastrointestinal solubility. Pharm Res. 2016;33(1):52–71. https://doi.org/10.1007/s11095-015-1762-7.
Van der Vossen AC, Hanff LM, Vulto AG, Fotaki N. Potential prediction of formulation performance in paediatric patients using biopharmaceutical tools and simulation of clinically relevant administration scenarios of nifedipine and lorazepam. Br J Clin Pharmacol. 2019;85(8):1728–39. https://doi.org/10.1111/bcp.13956.
Van Den Abeele J, Rayyan M, Hoffman I, Van de Vijver E, Zhu W, Augustijns P. Gastric fluid composition in a paediatric population: age-dependent changes relevant for gastrointestinal drug disposition. Eur J Pharm Sci. 2018;123:301–11. https://doi.org/10.1016/j.ejps.2018.07.022.
Fuchs A, Leigh M, Kloefer B, Dressman JB. Advances in the design of fasted state simulating intestinal fluids: FaSSIF-V3. Eur J Pharm Biopharm. 2015;94:229–40. https://doi.org/10.1016/j.ejpb.2015.05.015.
Jantratid E, Janssen N, Reppas C, Dressman JB. Dissolution media simulating conditions in the proximal human gastrointestinal tract: an update. Pharm Res. 2008;25(7):1663. https://doi.org/10.1007/s11095-008-9569-4.
Friedel HD, Brown CK, Barker AR, Buhse LF, Keitel S, Kraemer J, et al. FIP Guidelines for dissolution testing of solid oral products. J Pharm Sci. 2018;107(12):2995–3002. https://doi.org/10.1016/j.xphs.2018.08.007.
Van der Veken M, Aertsen M, Brouwers J, Stillhart C, Parrott N, Augustijns P. Gastrointestinal fluid volumes in pediatrics: a retrospective MRI study. Pharmaceutics. 2022;14(9). https://doi.org/10.3390/pharmaceutics14091935.
Best BM, Capparelli EV, Diep H, Rossi SS, Farrell MJ, Williams E, et al. Pharmacokinetics of lopinavir/ritonavir crushed versus whole tablets in children. J Acquir Immune Defic Syndr. 2011;58(4):385–91. https://doi.org/10.1097/QAI.0b013e318232b057.
Larsen RH, Hjalgrim LL, Grell K, Kristensen K, Pedersen LG, Brünner ED, et al. Pharmacokinetics of tablet and liquid formulations of oral 6-mercaptopurine in children with acute lymphoblastic leukemia. Cancer Chemother Pharmacol. 2020;86(1):25–32. https://doi.org/10.1007/s00280-020-04097-x.
US Food and Drug Administration. The use of physiologically based pharmacokinetic analyses—biopharmaceutics applications for oral drug product development, manufacturing changes, and controls. Guidance for Industry. U.S. Department of Health and Human Services Food and Drug Administration. Center for Drug Evaluation and Research (CDER). 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/use-physiologically-based-pharmacokinetic-analyses-biopharmaceutics-applications-oral-drug-product. Accessed 12 Apr 2023.
Duan P, Wu F, Moore JN, Fisher J, Crentsil V, Gonzalez D, et al. Assessing CYP2C19 ontogeny in neonates and infants using physiologically based pharmacokinetic models: impact of enzyme maturation versus inhibition. CPT Pharmacometrics Syst Pharmacol. 2019;8(3):158–66. https://doi.org/10.1002/psp4.12350.
Cheung KWK, van Groen BD, Burckart GJ, Zhang L, de Wildt SN, Huang S-M. Incorporating ontogeny in physiologically based pharmacokinetic modeling to improve pediatric drug development: what we know about developmental changes in membrane transporters. J Clin Pharmacol. 2019;59(S1):S56–69. https://doi.org/10.1002/jcph.1489.
Yang X, Wu H, Mehta D, Sullivan MC, Wang J, Burckart GJ, et al. Ontogeny equations with probability distributions for anthropomorphic measurements in preterm and term neonates and infants for use in a PBPK model. Comput Toxicol. 2019;11:101–17. https://doi.org/10.1016/j.comtox.2019.03.007.
Liu XI, Momper JD, Rakhmanina N, van den Anker JN, Green DJ, Burckart GJ, et al. Physiologically based pharmacokinetic models to predict maternal pharmacokinetics and fetal exposure to emtricitabine and acyclovir. J Clin Pharmacol. 2020;60(2):240–55. https://doi.org/10.1002/jcph.1515.
Liu XI, Momper JD, Rakhmanina NY, Green DJ, Burckart GJ, Cressey TR, et al. Physiologically based pharmacokinetic modeling framework to predict neonatal pharmacokinetics of transplacentally acquired emtricitabine, dolutegravir, and raltegravir. Clin Pharmacokinet. 2021;60(6):795–809. https://doi.org/10.1007/s40262-020-00977-w.
Liu XI, van den Anker JN, Burckart GJ, Dallmann A. Evaluation of physiologically based pharmacokinetic models to predict the absorption of BCS class I drugs in different pediatric age groups. J Clin Pharmacol. 2021;61(Suppl 1):S94-s107. https://doi.org/10.1002/jcph.1845.
Heimbach T, Kesisoglou F, Novakovic J, Tistaert C, Mueller-Zsigmondy M, Kollipara S, et al. Establishing the bioequivalence safe space for immediate-release oral dosage forms using physiologically based biopharmaceutics modeling (PBBM): case studies. J Pharm Sci. 2021. https://doi.org/10.1016/j.xphs.2021.09.017.
Ibarra M, Valiante C, Sopeña P, Schiavo A, Lorier M, Vázquez M, et al. Integration of in vitro biorelevant dissolution and in silico PBPK model of carvedilol to predict bioequivalence of oral drug products. Eur J Pharm Sci. 2018;118:176–82. https://doi.org/10.1016/j.ejps.2018.03.032.
Loisios-Konstantinidis I, Cristofoletti R, Fotaki N, Turner DB, Dressman J. Establishing virtual bioequivalence and clinically relevant specifications using in vitro biorelevant dissolution testing and physiologically-based population pharmacokinetic modeling case. example: Naproxen. Eur J Pharm Sci. 2020;143:105170. https://doi.org/10.1016/j.ejps.2019.105170.
Tolou-Ghamari Z, Zare M, Habibabadi JM, Najafi MR. A quick review of carbamazepine pharmacokinetics in epilepsy from 1953 to 2012. J Res Med Sci. 2013;18(Suppl 1):S81–5.
National Institute for Health and Care Excellence (NICE): British National Formulary (BNF). Carbamazepine. https://bnf.nice.org.uk/drugs/carbamazepine/. Accessed 12 Apr 2023.
Shayanfar A, Velaga S, Jouyban A. Solubility of carbamazepine, nicotinamide and carbamazepine–nicotinamide cocrystal in ethanol–water mixtures. Fluid Phase Equilib. 2014;363:97–105. https://doi.org/10.1016/j.fluid.2013.11.024.
US Food and Drug Administration. M9 Biopharmaceutics classification system-based biowaivers. guidance for industry. U.S. Department of Health and Human Services Food and Drug Administration. Center for Drug Evaluation and Research (CDER). 2021. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m9-biopharmaceutics-classification-system-based-biowaivers. Accessed 12 Apr 2023.
García MA, Cristofoletti R, Abrahamsson B, Groot DW, Parr A, Polli JE, et al. Biowaiver monograph for immediate-release solid oral dosage forms: carbamazepine. J Pharm Sci. 2021;110(5):1935–47. https://doi.org/10.1016/j.xphs.2021.02.019.
Mencarelli G, Jones J, Brown J, Timmins P, Fotaki N. Age related biorelevant dissolution testing for paediatric formulations. Int J Pharm. 2018;536(2):492–3. https://doi.org/10.1016/j.ijpharm.2017.08.015.
El-Massik MA, Abdallah OY, Galal S, Daabis NA. Towards a universal dissolution medium for carbamazepine. Drug Dev Ind Pharm. 2006;32(7):893–905. https://doi.org/10.1080/03639040600762677.
Yarasca Á, Jáuregui A, Bendezú Acevedo MDR, Palomino-Jhong J, García Ceccarelli J, Alvarado C, et al. In vitro biopharmaceutical equivalence of carbamazepine sodium tablets available in Lima, Peru. Dissolution Technol. 2021;28. https://doi.org/10.14227/DT280221PGC2.
Vertzoni M, Dressman J, Butler J, Hempenstall J, Reppas C. Simulation of fasting gastric conditions and its importance for the in vivo dissolution of lipophilic compounds. Eur J Pharm Biopharm. 2005;60(3):413–7. https://doi.org/10.1016/j.ejpb.2005.03.002.
Vertzoni M, Augustijns P, Grimm M, Koziolek M, Lemmens G, Parrott N, et al. Impact of regional differences along the gastrointestinal tract of healthy adults on oral drug absorption: An UNGAP review. Eur J Pharm Sci. 2019;134:153–75. https://doi.org/10.1016/j.ejps.2019.04.013.
Rahman Z, Agarabi C, Zidan AS, Khan SR, Khan MA. Physico-mechanical and stability evaluation of carbamazepine cocrystal with nicotinamide. AAPS PharmSciTech. 2011;12(2):693–704. https://doi.org/10.1208/s12249-011-9603-4.
Hens B, Tsume Y, Bermejo M, Paixao P, Koenigsknecht MJ, Baker JR, et al. Low buffer capacity and alternating motility along the human gastrointestinal tract: implications for in vivo dissolution and absorption of ionizable drugs. Mol Pharm. 2017;14(12):4281–94. https://doi.org/10.1021/acs.molpharmaceut.7b00426.
Mowafy HA, Alanazi FK, El Maghraby GM. Development and validation of an HPLC-UV method for the quantification of carbamazepine in rabbit plasma. Saudi Pharm J. 2012;20(1):29–34. https://doi.org/10.1016/j.jsps.2011.04.003.
Medina JR, Salazar DK, Hurtado M, Cortés AR, Domínguez-Ramírez AM. Comparative in vitro dissolution study of carbamazepine immediate-release products using the USP paddles method and the flow-through cell system. Saudi Pharmaceutical Journal. 2014;22(2):141–7. https://doi.org/10.1016/j.jsps.2013.02.001.
General Chapter. Stage 6 Harmonization 〈711〉 Dissolution. United States Pharmacopeia. 2011. https://www.usp.org/sites/default/files/usp/document/harmonization/gen-method/stage_6_monograph_25_feb_2011.pdf. Accessed 12 Apr 2023.
US Food and Drug Administration. Guidance for industry: dissolution testing of immediate release solid oral dosage forms. U.S. Department of Health and Human Services Food and Drug Administration. Center for Drug Evaluation and Research (CDER). 1997. https://www.fda.gov/media/70936/download. Accessed 12 Apr 2023.
Guimarães M, Vertzoni M, Fotaki N. Performance evaluation of Montelukast pediatric formulations: part II - a PBPK modelling approach. Aaps j. 2022;24(1):27. https://doi.org/10.1208/s12248-021-00662-1.
Géradin AP, Abadie FV, Campestrini JA, Theobald W. Pharmacokinetics of carbamazepine in normal humans after single and repeated oral doses. J Pharmacokinet Biopharm. 1976;4(6):521–35. https://doi.org/10.1007/bf01064556.
Kohlmann P, Stillhart C, Kuentz M, Parrott N. Investigating oral absorption of carbamazepine in pediatric populations. AAPS J. 2017;19(6):1864–77. https://doi.org/10.1208/s12248-017-0149-6.
Kovacević I, Parojcić J, Homsek I, Tubić-Grozdanis M, Langguth P. Justification of biowaiver for carbamazepine, a low soluble high permeable compound, in solid dosage forms based on IVIVC and gastrointestinal simulation. Mol Pharm. 2009;6(1):40–7. https://doi.org/10.1021/mp800128y.
Olling M, Mensinga TT, Barends DM, Groen C, Lake OA, Meulenbelt J. Bioavailability of carbamazepine from four different products and the occurrence of side effects. Biopharm Drug Dispos. 1999;20(1):19–28. https://doi.org/10.1002/(sici)1099-081x(199901)20:1%3c19::aid-bdd152%3e3.0.co;2-q.
Kuemmel C, Yang Y, Zhang X, Florian J, Zhu H, Tegenge M, et al. Consideration of a credibility assessment framework in model-informed drug development: potential application to physiologically-based pharmacokinetic modeling and simulation. CPT Pharmacometrics Syst Pharmacol. 2020;9(1):21–8. https://doi.org/10.1002/psp4.12479.
Adiwidjaja J, Boddy AV, McLachlan AJ. Implementation of a physiologically based pharmacokinetic modeling approach to guide optimal dosing regimens for imatinib and potential drug interactions in paediatrics. Front Pharmacol. 2020;10. https://doi.org/10.3389/fphar.2019.01672.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45(9):931–56. https://doi.org/10.2165/00003088-200645090-00005.
Emoto C, Fukuda T, Johnson TN, Adams DM, Vinks AA. Development of a pediatric physiologically based pharmacokinetic model for sirolimus: applying principles of growth and maturation in neonates and infants. CPT Pharmacometrics Syst Pharmacol. 2015;4(2):e17-e. https://doi.org/10.1002/psp4.17.
Hines RN. Ontogeny of human hepatic cytochromes P450. J Biochem Mol Toxicol. 2007;21(4):169–75. https://doi.org/10.1002/jbt.20179.
Upreti VV, Wahlstrom JL. Meta-analysis of hepatic cytochrome P450 ontogeny to underwrite the prediction of pediatric pharmacokinetics using physiologically based pharmacokinetic modeling. J Clin Pharmacol. 2016;56(3):266–83. https://doi.org/10.1002/jcph.585.
Song G, Sun X, Hines RN, McCarver DG, Lake BG, Osimitz TG, et al. Determination of human hepatic CYP2C8 and CYP1A2 age-dependent expression to support human health risk assessment for early ages. Drug Metab Dispos. 2017;45(5):468–75. https://doi.org/10.1124/dmd.116.074583.
Verscheijden LFM, Koenderink JB, Johnson TN, de Wildt SN, Russel FGM. Physiologically-based pharmacokinetic models for children: starting to reach maturation? Pharmacol Ther. 2020;211:107541. https://doi.org/10.1016/j.pharmthera.2020.107541.
Jamei M, Marciniak S, Edwards D, Wragg K, Feng K, Barnett A, et al. The Simcyp population based simulator: architecture, implementation, and quality assurance. In Silico Pharmacol. 2013;1(1):9. https://doi.org/10.1186/2193-9616-1-9.
Hartley R, Aleksandrowicz J, Bowmer CJ, Cawood A, Forsythe WI. Dissolution and relative bioavailability of two carbamazepine preparations for children with epilepsy. J Pharm Pharmacol. 1991;43(2):117–9. https://doi.org/10.1111/j.2042-7158.1991.tb06644.x.
Bano G, Raina RK, Sharma DB. Pharmacokinetics of carbamazepine in protein energy malnutrition. Pharmacology. 1986;32(4):232–6. https://doi.org/10.1159/000138174.
Rey E, d’Athis P, de Lauture D, Dulac O, Aicardi J, Olive G. Pharmacokinetics of carbamazepine in the neonate and in the child. Int J Clin Pharmacol Biopharm. 1979;17(2):90–6.
Calvier EAM, Krekels EHJ, Johnson TN, Rostami-Hodjegan A, Tibboel D, Knibbe CAJ. Scaling drug clearance from adults to the young children for drugs undergoing hepatic metabolism: a simulation study to search for the simplest scaling method. AAPS J. 2019;21(3):38. https://doi.org/10.1208/s12248-019-0295-0.
Bego M, Patel N, Cristofoletti R, Rostami-Hodjegan A. Proof of concept in assignment of within-subject variability during virtual bioequivalence studies: propagation of intra-subject variation in gastrointestinal physiology using physiologically based pharmacokinetic modeling. AAPS J. 2022;24(1):21. https://doi.org/10.1208/s12248-021-00672-z.
Rastogi V, Yadav P, Lal N, Rastogi P, Singh BK, Verma N, et al. Mathematical prediction of pharmacokinetic parameters-an in-vitro approach for investigating pharmaceutical products for IVIVC. Futur J Pharm Sci. 2018;4(2):175–84. https://doi.org/10.1016/j.fjps.2018.03.001.
Zhang X, Ye X, Hu K, Li W, Li W, Xiao Q, et al. A physiologically based pharmacokinetic model for studying the biowaiver risk of biopharmaceutics classification system class I drugs with rapid elimination: dexketoprofen trometamol case study. Front Pharmacol. 2022;13. https://doi.org/10.3389/fphar.2022.808456.
Statelova M, Holm R, Fotaki N, Reppas C, Vertzoni M. Successful extrapolation of paracetamol exposure from adults to infants after oral administration of a pediatric aqueous suspension is highly dependent on the study dosing conditions. Aaps j. 2020;22(6):126. https://doi.org/10.1208/s12248-020-00504-6.
Obach RS, James GB, Theodore EL, Silber BM, Barry CJ, Fiona M, et al. The prediction of human pharmacokinetic parameters from preclinical and in vitro metabolism data. J Pharmacol Exp Ther. 1997;283(1):46.
US Food and Drug Administration. Guidance for industry: bioavailability and bioequivalence studies submitted in NDAs or INDs-General Considerations U.S. Department of Health and Human Services Food and Drug Administration. Center for Drug Evaluation and Research (CDER). 2014. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioavailability-and-bioequivalence-studies-submitted-ndas-or-inds-general-considerations. Accessed 12 Apr 2023.
US Food and Drug Administration. Dissolution testing and acceptance criteria for immediate-release solid oral dosage form drug products containing high solubility drug substances. Guidance for Industry U.S. Department of Health and Human Services Food and Drug Administration. Center for Drug Evaluation and Research (CDER). 2018. https://www.fda.gov/files/drugs/published/Dissolution-Testing-and-Acceptance-Criteria-for-Immediate-Release-Solid-Oral-Dosage-Form-Drug-Products-Containing-High-Solubility-Drug-Substances-Guidance-for-Industry.pdf. Accessed 12 Apr 2023.
Rodríguez-Hornedo N, Murphy D. Surfactant-facilitated crystallization of dihydrate carbamazepine during dissolution of anhydrous polymorph. J Pharm Sci. 2004;93(2):449–60. https://doi.org/10.1002/jps.10496.
Li M, Qiao N, Wang K. Influence of sodium lauryl sulfate and tween 80 on carbamazepine-nicotinamide cocrystal solubility and dissolution behaviour. Pharmaceutics. 2013;5(4):508–24. https://doi.org/10.3390/pharmaceutics5040508.
Srabovic M PM, Pehlic E. Micellar solubilization of carbamazepine. JSRR [Internet] 2014;24:3106–16. https://www.journaljsrr.com/index.php/JSRR/article/view/21049. Accessed 12 Apr 2023
Coello A, Meijide F, Núñez ER, Tato JV. Aggregation behavior of bile salts in aqueous solution†‡. J Pharm Sci. 1996;85(1):9–15. https://doi.org/10.1021/js950326j.
Lehto P, Aaltonen J, Tenho M, Rantanen J, Hirvonen J, Tanninen VP, et al. Solvent-mediated solid phase transformations of carbamazepine: effects of simulated intestinal fluid and fasted state simulated intestinal fluid. J Pharm Sci. 2009;98(3):985–96. https://doi.org/10.1002/jps.21490.
Zarmpi P, Flanagan T, Meehan E, Mann J, Østergaard J, Fotaki N. Biopharmaceutical implications of excipient variability on drug dissolution from immediate release products. Eur J Pharm Biopharm. 2020;154:195–209. https://doi.org/10.1016/j.ejpb.2020.07.014.
Pas T, Struyf A, Vergauwen B, Van den Mooter G. Ability of gelatin and BSA to stabilize the supersaturated state of poorly soluble drugs. Eur J Pharm Biopharm. 2018;131:211–23. https://doi.org/10.1016/j.ejpb.2018.08.003.
Murphy D, Rodríguez-Cintrón F, Langevin B, Kelly RC, Rodríguez-Hornedo N. Solution-mediated phase transformation of anhydrous to dihydrate carbamazepine and the effect of lattice disorder. Int J Pharm. 2002;246(1–2):121–34. https://doi.org/10.1016/s0378-5173(02)00358-7.
Dunn C, Perrier J, Khadra I, Wilson CG, Halbert GW. Topography of simulated intestinal equilibrium solubility. Mol Pharm. 2019;16(5):1890–905. https://doi.org/10.1021/acs.molpharmaceut.8b01238.
Forner K, Hidalgo I, Lin J, Ackermann M, Langguth P. Dissolution/permeation: the importance of the experimental setup for the prediction of formulation effects on fenofibrate in vivo performance. Die Pharmazie - Int J Pharm Sci. 2017;72(10):581–6. https://doi.org/10.1691/ph.2017.7066.
Stillhart C, Vučićević K, Augustijns P, Basit AW, Batchelor H, Flanagan TR, et al. Impact of gastrointestinal physiology on drug absorption in special populations––an UNGAP review. Eur J Pharm Sci. 2020;147:105280. https://doi.org/10.1016/j.ejps.2020.105280.
Davit BM, Conner DP, Fabian-Fritsch B, Haidar SH, Jiang X, Patel DT, et al. Highly variable drugs: observations from bioequivalence data submitted to the FDA for new generic drug applications. Aaps j. 2008;10(1):148–56. https://doi.org/10.1208/s12248-008-9015-x.
Grimm M, Koziolek M, Kühn J-P, Weitschies W. Interindividual and intraindividual variability of fasted state gastric fluid volume and gastric emptying of water. Eur J Pharm Biopharm. 2018;127:309–17. https://doi.org/10.1016/j.ejpb.2018.03.002.
Wollmer E, Ungell AL, Nicolas JM, Klein S. Review of paediatric gastrointestinal physiology relevant to the absorption of orally administered medicines. Adv Drug Deliv Rev. 2022;181:114084. https://doi.org/10.1016/j.addr.2021.114084.
Guimarães M, Statelova M, Holm R, Reppas C, Symilllides M, Vertzoni M, et al. Biopharmaceutical considerations in paediatrics with a view to the evaluation of orally administered drug products - a PEARRL review. J Pharm Pharmacol. 2019;71(4):603–42. https://doi.org/10.1111/jphp.12955.
Acknowledgements
GP, MCJ, and HKB are grateful to U.S. FDA members for valuable contribution in providing useful comments and advice on this manuscript.
Funding
This research work is carried out by the University of Birmingham under the project “Research Proposal to better understand risk mitigation in the evaluation of relative bioavailability of pediatric generic products” funded by U.S. FDA through FDA BAA-17–00123 (Pediatric Generic Contract). Dr. Abdullah Al Shoyaib was supported by an appointment to the Research Participation Program at CDER, administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy and the FDA.
Author information
Authors and Affiliations
Contributions
GP, FW, GJB, KF, YMM, AAS, and HKB contributed to the conception and design of the work. GP carried out the dissolution experiments, HPLC method development, sample analyses, and data acquisition. GP, HKB, and MCJ contributed to the dissolution data interpretations, analyses, and visualizations. PBPK model development, validations, and simulations were performed by GP and HKB. GP and HKB wrote the manuscript with the help of all authors who provided critical feedback and helped in shaping the manuscript. LZ, LF, FW, and HKB helped in funding acquisition, supervision, resources, and project administration. All authors contributed to drafting/revising of the content and final approval of the version to be published. We agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Disclaimer
The opinions expressed in this article are those of the authors and should not be interpreted as the position of the U.S. FDA and the cases being presented do not imply FDA’s endorsement of the products.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pawar, G., Wu, F., Zhao, L. et al. Integration of Biorelevant Pediatric Dissolution Methodology into PBPK Modeling to Predict In Vivo Performance and Bioequivalence of Generic Drugs in Pediatric Populations: a Carbamazepine Case Study. AAPS J 25, 67 (2023). https://doi.org/10.1208/s12248-023-00826-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-023-00826-1