Abstract
The International Prostate Symptom Score (IPSS), the quality of life (QoL) score, and the benign prostatic hyperplasia impact index (BII) are three different scales commonly used to assess the severity of lower urinary tract symptoms associated with benign prostatic hyperplasia (BPH-LUTS). Based on a phase II clinical trial including 403 patients with moderate to severe BPH-LUTS, the objectives of this study were to (i) develop traditional pharmacometric and bounded integer (BI) models for the IPSS, QoL score, and BII endpoints, respectively; (ii) compare the power and type I error in detecting drug effects of BI modeling with traditional methods through simulation; and (iii) obtain quantitative translation between scores on the three abovementioned scales using a BI modeling framework. All developed models described the data adequately. Pharmacometric modeling using a continuous variable (CV) approach was overall found to be the most robust in terms of type I error and power to detect a drug effect. In most cases, BI modeling showed similar performance to the CV approach, yet severely inflated type I error was generally observed when inter-individual variability (IIV) was incorporated in the BI variance function (g()). BI modeling without IIV in g() showed greater type I error control compared to the ordered categorical approach. Lastly, a multiple-scale BI model was developed and estimated the relationship between scores on the three BPH-LUTS scales with overall low uncertainty. The current study yields greater understanding of the operating characteristics of the novel BI modeling approach and highlights areas potentially requiring further improvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benign prostate hyperplasia (BPH) is a common condition in the aging male and is estimated to affect 50% of males by age 60 years and 90% by age 85 years (1,2). The increase in prostatic weight frequently leads to a spectrum of clinical manifestations known as lower urinary tract symptoms (LUTS). The severity of BPH-LUTS is most commonly measured by the International Prostate Symptom Score (IPSS) (also known as the American Urological Association score) (3), which consists of seven questions describing the severity of symptoms. These comprise the feeling of incomplete bladder emptying, frequency of urination, intermittency during urination, the urgency to urinate, weakness of the urinary stream, straining during urination, and nocturia. Each IPSS question can be scored from 0 to 5, resulting in a summary IPSS that may range from 0 to 35. The IPSS is commonly used as a primary efficacy endpoint in BPH-LUTS clinical trials and is considered the gold standard diagnostic tool in the clinic (4,5). In addition to the IPSS, two additional endpoints for assessing BPH-LUTS are regularly implemented in clinical trials: the quality of life (QoL) score (6) and the BPH impact index (BII) (7). The QoL question evaluates a patient’s perception of his ability to tolerate his current level of BPH-LUTS for the rest of his life. It is rated between 0 and 6, with 0 corresponding to feeling “delighted” regarding this outlook and 6 corresponding to feeling “terrible.” Research has previously pointed towards the utility of the QoL score to diagnose BPH-LUTS severity and its significant correlation to the IPSS (6). The BII questionnaire consists of four questions that respectively aim to assess the impact of BPH-LUTS on a patient’s level of physical discomfort, degree of worrying, general inconvenience caused by urinary problems, and impediment of desired activity. A summary BII score between 0 and 13 is possible. Significant correlation with the IPSS and QoL score has been established (8), as well as clinical significance thresholds of changes in the IPSS and the BII (9). However, the direct connection between observed scores on each of the three abovementioned BPH-LUTS scales has to our knowledge not been investigated. Given the use of different rating scales in the clinic and in clinical trials within BPH-LUTS, such knowledge may allow for informed translation between scales. This may be important in the context of clinical research as well as for bridging between clinical trials.
Traditionally, model-based analysis of rating scales with more than 10 categories treats the data as a continuous variable (CV) (10), which violates the inherent discrete nature of the data. On the other hand, using an ordered categorical (OC) approach may require too many parameters and does not allow for prediction of categories that are not observed in the data. Recently, bounded integer (BI) modeling was presented as a method for describing data originating from scales (11). The BI approach often showed lower Akaike information criterion values compared to the CV and OC approaches in the analysis of several different scales (11), indicating that it may be a promising method for longitudinal analysis of clinical trials employing scale endpoints. However, the power to detect a drug effect and corresponding type I error of the BI modeling approach has not yet been examined. This knowledge may contribute to solidifying the utility of BI modeling in comparison to traditionally used methods. The objectives of the current work were hence to (i) develop BI models for the IPSS, QoL score, and BII BPH-LUTS scales based on data from a phase II double-blind parallel-group clinical trial; (ii) compare the power and type I error in detecting a drug effect of the developed BI models with traditional continuous variable and/or ordered categorical modeling models, respectively; and (iii) develop a BI model regarding trial data from the three BPH-LUTS scales simultaneously to establish the connection between scores on the different scales.
Methods
Data
Ferring Pharmaceuticals A/S trial CS36 (NCT00947882) was a phase II double-blind, parallel-group, dose-finding study evaluating the efficacy and safety of a single subcutaneous injection of the GnRH antagonist degarelix over 6 months. Four hundred and three patients with moderate to severe BPH-LUTS were randomized to placebo, 10-, 20-, or 30-mg degarelix 40 mg/mL solution. For trial inclusion, all patients were required to have an IPSS ≥ 13 and a QoL ≥ 3 at screening 2 weeks before dosing at the baseline visit. Each patient had seven scheduled visits post-baseline (14, 30, 61, 91, 121, 152, and 182 days post-dose). The IPSS and QoL score was measured at all eight trial visits, while the BII was measured at baseline, 91 days post-dose, and 182 days post-dose. CS36 was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. Further details regarding the CS36 trial have been presented previously elsewhere (12,13).
Modeling methodology
Model development
Continuous variable modeling
A continuous variable (CV) longitudinal IPSS model previously presented elsewhere (12) was used as basis for comparison with the BI approach in the current study. The CV IPSS model was developed on the current CS36 data and was modified to contain no covariates or IIV distribution transformations. The longitudinal trajectory of the IPSS was described according to
with Baseline representing the baseline IPSS, Pmax the maximal placebo effect, Tprog the half-life to reach Pmax, Drift describing relapse or continued remission over time, and Drug the offset drug effect of degarelix. IIV was included for Baseline and Tprog assuming a lognormal distribution while IIV for Pmax and Drift, respectively, were assumed normally distributed. A combined residual error model was used.
For the modeling of BII data, time-varying placebo effect models such as the linear, bi-linear, power, exponential, Weibull, and inverse Bateman structural placebo models were tested, as well as a time-independent placebo effect model (intercept), and combinations thereof (slope-intercept). Offset, linear, and onset drug effect models were examined to describe degarelix treatment effect on the BII scale.
Ordered categorical modeling
A rule of thumb is to use an ordered categorical (OC) approach when there are less than ten categories (10). As the QoL score consists of seven categories, an OC proportional odds (PO) model (14) was used to model these data. The BII total score contains fourteen discrete response values, all of which apart from the extreme values can be arrived at through many different combinations of responses. However, it may be viewed by some modelers as an ordered categorical variable. An OC PO model was therefore also applied to the total BII score in the current work.
In the OC PO model, the logit of the probability of an observation Y being equal or greater than a score j in the ith individual at time t is given by
where fj is a function of the baseline probability of each score (αm) and the effect of predictors (in the current work, the time-dependent placebo, and drug effect, respectively):
and ηi is the inter-individual variability (IIV), with mean zero and variance ω2. Similar placebo and drug effect models to those mentioned for CV BII model development were investigated in OC model development for the QoL and BII scales, respectively. Lastly, the probability of observing a particular score is given by
Bounded integer modeling
The methodology has been described in detail elsewhere (11). Briefly, given a scale of n categories, the probits (Z1/n to Z(n-1)/n) are first calculated to specify n-1 cut-offs, which border n equally-sized areas under a standard normal distribution N(0,1). For the IPSS, 35 cut-offs were used, six cut-offs were used for the QoL, and 13 cut-offs were used for the BII. Subsequently, in conjunction with the probits, the probability of each category is determined through a function describing a normal distribution of fixed (θ) and random effects (ηi), time, and covariates f(θ, ηi,f, t, Xi,f), along with a variance function g(σ, ηi,g, t, Xi,g), i.e., N(f(θ, ηi,f, t, Xi,f) and g(σ, ηi,g, t, Xi,g)). The probability for the kth category, Pi,j(k), is defined as
with Φ being the cumulative distribution of the normal distribution function, i.e., the area under the latent function curve within the cut-off interval. For the first category (k = 1):
representing the cumulative distribution function in the interval [-∞, Z1/n], and for the last category (k = n):
representing the cumulative distribution in the interval [Z(n-1)/n, ∞].
Similar placebo and drug effect models to those described within CV BII model development were tested on the latent probit scale. Moreover, the addition of a Drift parameter similar to what was incorporated in the CV IPSS model was also examined. BI models with and without inter-individual variability (IIV) in the BI variance function, g(), were developed for each scale to precisely assess potential sources of variation in performance. Including an IIV term in the BI variance function allows the scoring consistency to vary between subjects and has previously been shown to reduce the Akaike information criterion substantially (11). In all of the developed BI models that included IIV in g(), a lognormal distribution was specified for this IIV term as described in Wellhagen et al. (11).
Joint bounded integer modeling of multiple scales
Due to its utilization of a latent scale, a multivariate approach can be implemented under the BI framework, which regards multiple scale measures describing the same disease simultaneously (15). In the current analysis, a joint BI model describing changes in IPSS, QoL, and BII over time in individual patients was developed. The IPSS cut-offs (Z1/36 to Z35/36) were specified as the reference (i.e., identical to the probits in the BI model considering only the IPSS scale), while the cut-offs for the QoL and the BII scores, respectively, were estimated on this same latent scale. The relationship between scores from each scale could thereby be established. Given that the IPSS was used as the reference scale in the joint BI model, the longitudinal model was developed according to the trajectory of the IPSS. The same longitudinal model described the longitudinal trajectory of probabilities for the QoL score and the BII. Differences in scale measurement frequency over the trial period is likely to influence the consistency in patients’ scores, and therefore, incorporation of a separate g() variance function was investigated for the BII scale in the joint BI model: BII measurements were only available at three visits in the CS36 trial period compared to eight measurements over the trial period for the IPSS and the QoL score.
Model selection and evaluation
For nested models, the difference in objective function value (OFV) corresponding to a significance level of 0.05 was considered statistically significant assuming a χ2 distribution. For non-nested models, the difference in Akaike information criterion (AIC) was used. AIC was computed as the objective function value (OFV) plus two times the number of model parameters. Model stability based on the convergence of minimization and covariance steps, parameter precision assessed through NONMEM’s relative standard error estimate, and graphical diagnostics was also considered during model selection. Visual predictive checks (VPCs) were used to assess the adequacy of the model characterization of the observed longitudinal data on each scale.
Power and type I error calculation
The analysis of power and type I error considered multiple simulation scenarios from different types of models using BPH-LUTS scales that differ in the number of possible scores as case studies. The latter allowed for comparison of the BI model with different types of reference models (CV and/or OC). Simulating data from only type of model would bias the analysis and therefore the current work sought to gain an overall understanding of the operating characteristics of the BI approach by testing its performance under different conditions. A stochastic simulation and estimation (SSE) procedure with 500 trial replicates at different sample sizes was used to assess the power to detect a drug effect of the developed models. In the SSE, a drop in OFV of 3.841 (p = 0.05 assuming a χ2 distribution) was used as the threshold to establish statistical significance of the drug effect between the reduced (without a drug effect parameter) and full models (with a drug effect parameter). All simulated trials had the same allocation ratio of patients in the placebo and treatment arms as in the CS36 clinical trial. No dropout was simulated for simplicity purposes. For the comparison of power of the BI IPSS model and the CV IPSS model, a pharmacometric item response theory (IRT) model (12) that was previously developed on the same CS36 data set as in the current study was used as the simulation model. Simulated total IPSS responses were hence obtained from the sum of simulated item-level IPSS responses. For power estimation of models regarding the QoL score and the BII, respectively, the simulation model was a previously developed integrated IRT model (13), which was also developed on the same data used in the current work. In the investigation of power to detect of a drug effect of the developed models within each BPH-LUTS scale, pharmacometric IRT models, which describe the respective observed longitudinal trajectories of the IPSS, QoL score, and BII in the CS36 trial adequately (12,13), were chosen as the simulation model in the main investigational scenario to minimize simulation model bias and generate integer scores as would be observed in, e.g., an actual clinical trial within BPH-LUTS. Additionally, SSE procedures were also performed using each of the different developed models that inherently respect the integer nature of the data (i.e., OC and BI models) as the simulation model. The type I error of the models in detecting a drug effect was investigated in an identical fashion to power, except for the simulation models containing no drug effect.
Software
Modeling was carried out using the Laplace estimation method in NONMEM version 7.4.3 and Perl-Speaks-NONMEM (PsN) (16) version 4.9.0. Laplacian estimation with interaction was used for the continuous variable models. R version 3.6.0 and the xpose4 package (16) were used for the post-processing of results and graphics.
Results
The baseline CS36 trial characteristics and the mean time course of each BPH-LUTS scale have been presented elsewhere (12,13). In summary, each of the four trial arms showed a marked mean decrease from baseline for all three BPH-LUTS scales. Furthermore, by visual inspection of the mean data from the three degarelix treatment arms, no dose-response relationship was evident on any of the symptom scales. In total, 3117 IPSS, 3119 QoL scores, and 1116 BII responses from 403 patients were available for analysis.
Model development
International Prostate Symptom Score
Reference model
The parameter estimates along with their relative standard errors in the CV IPSS model (IPSS-A) are shown in Table I. Implementing dose-response or exposure-response models (linear and Emax) did not decrease the OFV significantly. A VPC of the CV IPSS model indicated adequate description of the data and is shown in the Supplemental Material.
Bounded integer models
A BI model without inter-individual variability (IIV) in the variance function, g(), was first developed (model IPSS-B). In this model, the longitudinal trajectory of the IPSS was described by the same structural model as in the CV approach (model IPSS-A). In Table I, the Baseline parameter refers to the z-score from a normal distribution, and consequently the placebo and drug effect represent changes on this latent scale. Normally distributed IIV was included for the Baseline, Pmax, and Drift parameters, while lognormal IIV was specified for Tprog. Incorporation of an offset drug effect resulted in an OFV drop of 22.2. In the second BI model (IPSS-C), IIV was included for the g() function assuming a lognormal distribution, and this yielded a drop in OFV of 393.6 compared to IPSS-B. However, in the presence of the g() IIV parameter, the Drift parameter was no longer significant and was removed in a fourth model (IPSS-D). Incorporation of an offset drug effect resulted in an OFV reduction of 38.2 and 51.9 in IPSS-C and IPSS-D, respectively. Parameter estimates for the three BI IPSS models are shown in Table I. Similar to the CV IPSS model (IPSS-A), no dose-response or exposure-response relationship was found to be significant. VPCs for each of the three BI IPSS models showed adequate description of the data and are presented in the Supplemental Material, along with the NONMEM code used for estimation and simulation.
Quality of life score
Reference model
An OC proportional odds model was developed (QoL-A) where the longitudinal change in logit probability of observing a QoL score, Y, was described by
where X = 1,..,6, Bx is the baseline logit probability, Pmax is the maximal placebo effect, Tprog is the half-life to reach Pmax, and ηi is the IIV in logit baseline probability. Inclusion of a drug effect parameter did not result in significant OFV reduction. Parameter estimates for the proportional odds model for the QoL score are shown in Table II. A VPC for the OC QoL model (QoL-A) is shown in the Supplemental Material, indicating good fit to the data.
Bounded integer models
First, a BI model without IIV in g() was developed (QoL-B). A longitudinal model similar to the BI IPSS model without IIV in g() (IPSS-B) described the data. Next, in the second BI QoL model (QoL-C), IIV was included in the g() function, yielding an OFV drop of 590.5 points. No significant drug effect was identified in either BI QoL model. Overall low parameter uncertainty (Table II) and adequate fit to the data as evidenced by VPCs (Supplemental Material) was observed.
Benign prostatic hyperplasia impact index
Reference models
One CV (model BII-A) and one OC model (BII-B) were developed to describe the BII data. In the BII CV model (BII-A), the longitudinal model was specified by
where Baseline is the baseline BII, PlaceboInt is the intercept placebo effect model, and Drug is the offset degarelix effect. IIV was included for Baseline as well as PlaceboInt assuming a normal distribution. An additive model best described the residual error. Incorporation of an offset drug effect decreased the OFV by 4.6. Incorporating of dose-response or exposure-response models did not yield a significant decrease in OFV. A VPC for the CV BII model (BII-A) is presented in the Supplemental Material, indicating adequate fit of the model to the observed data.
In the OC model (BII-B), the same type of longitudinal model as in the BII CV model (BII-A) described the time course of the logit probability for each score. An additive IIV term was added to the baseline logit probability. Incorporation of an offset drug effect yielded an OFV reduction of 7.1 points. A categorical VPC shows the adequate fit of the model to the data (Supplemental Material), and parameter estimates for both the CV (BII-A) and OC (BII-B) model are shown in Table III.
Bounded integer model
Including IIV for the g() parameter did not result in a statistically significant improvement in OFV, and therefore only a single BI model was developed for the BII scale. In the BII BI model (BII-C), incorporation of an offset drug effect decreased the OFV by 5.1. The parameter estimates for the BI model are shown in Table III. No dose-response or exposure-response model provided a significant decrease in OFV. A VPC for the BI BII model is shown in the Supplemental Material, indicating adequate fit of the model.
Akaike information criterion
Table IV shows the AIC for all the developed models. Within the IPSS and QoL scales, BI models displayed a lower AIC compared to the reference models when a random effect was included in the BI variance function, g(). Furthermore, the BI model for the BII (that did not include a g() random effect) (BII-C) also showed a lower AIC compared to the CV BII model (BII-A), and so did OC QoL model (QoL-A) compared to the BI QoL model without a g() random effect (QoL-B). However, the CV IPSS model (IPSS-A) performed better in terms of fit compared to the BI model without a g() random effect (IPSS-B), and the same was seen with the OC BII model (BII-B) compared to the BI BII model (BII-C).
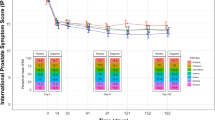
Power and type I error in detecting a drug effect
The power to detect a drug effect and associated type I error of the four IPSS models under four different simulation scenarios is shown in Fig. 1. The type I error of detecting a drug effect of the BI model with IIV in g()and omitting the Drift parameter (model IPSS-D) was very high across all investigated simulation scenarios except for when data was simulated from model IPSS-D itself. On the other hand, the BI IPSS model that retained both the Drift parameter and the g() random effect (model IPSS-C) generally showed a type I error rate at the nominal level in all scenarios, similar to the CV IPSS model (IPSS-A). The BI IPSS model without a g() random effect (model IPSS-B) showed an adequate type I error control except when the data was simulated from BI models incorporating IIV in the g() function (i.e., simulation from models IPSS-C and IPSS-D, respectively, in Fig. 1). Overall, the CV model (model IPSS-A) showed the best type I error control and power across the different scenarios. Figure 2 shows the power and type I error of the developed QoL models. As reported in the model development section, these models did not include a drug effect parameter due to lack of statistical significance of the latter in the CS36 trial. A hypothetical offset drug effect parameter was therefore specified in the OC simulation model (QoL-A) as well as in the respective BI simulation models (QoL-B and QoL-C), similar to the offset drug effect included in the IRT simulation model (13). The magnitude of the drug effect was specified as -0.5 in OC simulation model QoL-A and -0.1 in the BI simulation model QoL-B and QoL-C, respectively. Consequently, an offset drug effect was also included and estimated in the full OC PO QoL score and the BI QoL score models in the SSE procedure in order to estimate type I error and power. BI model QoL-B showed the best type I error control among the three models across all four simulation scenarios, as the 95% CI for the type I error estimate consistently included 5%. Meanwhile, the OC model QoL-A and the BI model with a random effect in g() QoL-C had highly inflated type I error in detecting a drug effect, except when data was simulated from the OC model QoL-A.
Power and type I error in detecting a drug effect for the four developed pharmacometric models describing the International Prostate Symptom Score (IPSS) under four different simulation models and varying trial sample sizes. Five hundred trial replicates were generated under each sample size for both power and type I error estimation. Model IPSS-A used a continuous variable (CV) approach with a combined residual error model. The bounded integer (BI) model IPSS-B did not contain inter-individual variability (IIV) in the BI variance function (g()), BI model IPSS-C contained both IIV in g() as well as a Drift parameter, while IPSS-D contained IIV in g() but did not estimate a Drift parameter.
– Power and type I error in detecting a drug effect for the three developed pharmacometric models describing the Quality of Life (QoL) score under four different simulation models and varying trial sample sizes. 500 trial replicates were generated under each sample size for both power and type I error estimation. Model QoL-A used an ordered categorical (OC) approach. The bounded integer (BI) model QoL-B did not contain inter-individual variability in the BI variance function (g()) while BI model QoL-C did
Figure 3 shows the power and type I error of models for the BII scale under three different simulation scenarios. The type I error and power of the CV BII model (BII-A) and BI model BII-C that did not contain IIV in g() was comparable in all simulated scenarios, while the OC BII model (BII-B) showed inflated type I error except when data was simulated from this model (Fig. 3, top right panel).
Power and type I error in detecting a drug effect for the three developed pharmacometric models describing the BPH impact index (BII) score under three different simulation models and varying trial sample sizes. Five hundred trial replicates were generated under each sample size for both power and type I error estimation. Model BII-A used a continuous variable (CV) approach with an additive residual error model. Model BII-B used an ordered categorical (OC) approach. Bounded Integer (BI) model BII-C did not contain inter-individual variability in the BI variance function (g())
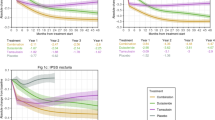
Joint bounded integer modeling
A joint BI model describing responses to the IPSS, QoL score, and BII over time in 403 patients was successfully developed. A longitudinal model similar to the BI IPSS model with a random effect in g() and without a drift parameter (IPSS-D) described the data. Incorporation of a separate BI variance function for the BII scale decreased the objective function by 583.5 points. An offset drug effect was estimated yielding an OFV drop of 50.5 points. The relationship between scores on each scale was estimated with overall low uncertainty as shown in Fig. 4. The estimated cut-offs allowing translation between the IPSS and the QoL score all had low uncertainty associated with them (< 8% RSE). Higher uncertainty (< 14% RSE) was observed for the cut-offs relating the IPSS to the BII compared to the IPSS-QoL cut-offs, and this was especially pronounced for BII scores greater than 10 (RSE ranging from 17.9 to 32.5%). The longitudinal parameter estimates of the joint BI model are shown in the Supplemental Material. All three scales were adequately described in the joint BI model as assessed through VPCs. These are shown in the Supplemental Material along with the NONMEM code used to generate the joint BI model.
Schematic representation of the relationship between scores of the International Prostate Symptom Score (IPSS), quality of life (QoL), and the benign prostatic hyperplasia impact index (BII) scales in the joint bounded integer model. The probits of the IPSS were used as reference cut-offs. The bold red and green vertical lines indicate the estimated cut-offs for the QoL and BII scores, respectively, along with their relative standard errors. Back translation of latent z-score values to observe score values allowed for mapping of scores
Discussion
This study presents the application of BI modeling within a BPH-LUTS clinical trial setting, where multiple disease-specific scale endpoints traditionally assess the efficacy of new treatments. Building further upon previous investigations focusing on AIC comparison of BI models with CV and OC models, respectively (11), the current study assesses the power and type I error in detecting a drug effect of the BI modeling approach compared to these traditional methods. Lastly, by way of development of a joint BI model, the relationship between scores of the IPSS, QoL, and BII scales was established, which to our knowledge has not been shown beforehand.
Akaike information criterion
The first objective of the current paper was to develop BI models for each of the three BPH-LUTS scales used in trial CS36. Models with and without IIV in g() were developed, and this led to the development of three different BI models for the IPSS (IPSS-B, IPSS-C, and IPSS-D), two for the QoL score (QoL-B and QoL-C), and one for the BII scale (BII-C). Similar to previous BI models of different scales (11), the BI models with IIV in g() (models IPSS-C, IPSS-D, and QoL-C) showed the best data description in terms of AIC among all models within each scale. It can however be argued that since including IIV in the BI variance function translates to incorporating IIV in the residual variance of a CV model (11), this would be a fairer comparison. Hence, the CV IPSS model (model IPSS-A) was exploratorily further developed to include IIV in the residual variance (which we in the “Discussion” section refer to as model IPSS-A-2). An additive error model and a log-normally distributed IIV similar to the implementation by Karlsson et al. (17) were used, as the combined error model resulted in convergence issues. Furthermore, similar to model IPSS-D, the Drift parameter was no longer statistically significant and was removed from the model. Model IPSS-A-2 showed a substantially lower AIC compared to the BI IPSS model with a g() random effect (decrease of 789.2 points). However, its simulation properties were poor, as substantial data was simulated well below and above the possible minimally and maximally possible IPSS of zero and 35, respectively (Supplemental Material). Hence, compared to the CV approach which implements an additional random effect in the residual error, BI modeling with IIV in g() may have the advantage of describing the data well while preserving high predictive ability.
Unlike the previous analysis of the Likert pain data (11), the BI model of the QoL score without an IIV random effect in g() (model QoL-B) showed substantially better fit in terms of AIC compared to the OC model (model QoL-A). However, the fit of the BI BII model without IIV in g() (model BII-C) was not superior to the OC BII model (BII-B). The current data had eight measurements for the QoL score and three BII measurements per patient over the 6-month trial period. The number of longitudinal measurements may hence potentially influence the descriptive performance of BI modeling compared to the OC method; as the number of visits increases, more complex longitudinal trajectories may be captured by the BI model. The latter allows for inclusion of more IIV components compared to the standard OC model with a single random effect. Further discussion on comparison of BI and OC modeling has been reported elsewhere (11).
In previous work, BI models were reported to result in certain parameters becoming “superfluous” compared to their corresponding CV models (11). In the current work, however, the same structural model was ultimately developed for the BI model without IIV in g() (model IPSS-B) and the CV IPSS model (IPSS-A). However, following introduction of IIV in g() during BI IPSS modeling (models IPSS-C and IPSS-D), the Drift parameter was no longer statistically significant. The introduction of an IIV random effect in g() may therefore be a source of explanation for parameters losing statistical significance, as its flexibility may affect parameter identifiability.
Type I error and power
The second objective of the current analysis was to investigate the type I error and power of BI models, and this was achieved through a series of different simulations within each scale. Results overall indicated that incorporating IIV in the g() function of BI models may result in very high type I error as evidenced within different simulation scenarios for the IPSS and for the QoL scale. In the IPSS simulations, the increase in type I error may be attributed to model misspecification: When simulating from models that incorporate the Drift parameter (the IPSS IRT model, model IPSS-B, and model IPSS-C in Fig. 1), the BI model without this parameter (IPSS-D) consistently showed severely inflated type I error. When simulating from model IPSS-D, this same model performed well in terms of type I error and showed higher power to detect a drug effect compared to other models (IPSS-A, IPSS-B, IPSS-C); however, it is to be noted that the latter models still controlled type I error adequately (except for model IPSS-B, which had slightly inflated type I error). In the case of QoL score simulations, the BI model with a g() random effect (model QoL-C) had high η-shrinkage (> 80%) in the Tprog IIV term. This likely rendered this IIV term largely uninformative due to model parameter identifiability issues, thereby resulting in model misspecification. Furthermore, for models IPSS-D and QoL-C (with IIV in g()), the type I error was seen to increase with increasing sample size, namely, in the IRT simulation scenarios in Figs. 1 and 2, respectively. This may indicate that the more patients are included in the trial (and hence the larger the IIV in the longitudinal trajectories of patients), the larger room for error in detecting a drug effect with this type of BI model. It is however to be noted that the type I error of an exploratory CV model with IIV in the residual variance (model IPSS-A-2 presented earlier in the “Discussion” section) was similar to model IPSS-D across the four different simulation scenarios (data not shown). The severely inflated type I error as observed with model IPSS-D may therefore not be exclusive to the BI approach, but may instead be associated with incorporating IIV in the residual error component of models. Including IIV in the residual variance has shown adequate type I error control in terms of covariate inclusion in PK models (18). However, to our knowledge, it has not previously been investigated within the context of detecting drug effects in longitudinal drug-disease modeling using a nonlinear mixed effects modeling framework. Further research on these types of models may be of interest.
Misspecification of random effects is known to increase type I error for hypothesis testing on the fixed effect of interest within the context of linear mixed models (19,20). Authors have furthermore pointed towards data-driven random effects specification having higher potential for type I error inflation compared to the design-driven approach (20,21,22). This may also apply to the current findings; e.g., in the IRT simulation scenarios, the CV (IPSS-A) and BI models (IPSS-B, IPSS-C, and QoL-B) included similar random effects as the simulation models (12,13). The developed BI models were therefore more in line with the design of the simulated trial data and consequently in general showed better type I error rates. Oppositely, the IPSS BI model that included IIV in g() and omitted the Drift IIV parameter (model IPSS-D) could be said to adhere to a data-driven random effect specification approach. The IRT models used for simulation (12,13) were previously developed on the same CS36 data set as the current models, explaining the similarity between random effects.
To preserve both good data description as well as adequate type I error control in detecting a drug effect, it could be advised that if IIV is to be included in the BI g() function, this should be performed as the last model development step. Careful consideration of the influence of this parameter on the original structural model parameters (i.e., without IIV in g()) should be given, e.g., η-shrinkage. Furthermore, parameters that were significant prior to inclusion of IIV in g() may have to remain in the model regardless of their significance after its inclusion (e.g., similar to the Drift parameter in model IPSS-C). However, although this proposed approach may afford better type I error control, it may also limit the power to detect a drug effect: This was observed with model IPSS-C when simulating data from models IPSS-C and IPSS-D, respectively, in Fig. 1. This loss of power was also seen with models IPSS-A, IPSS-B, and IPSS-C when simulating from model IPSS-D with no Drift parameter.
Even though the IPSS CV model (IPSS-A) inherently violates the integer nature of the scale data, it was overall more robust in terms of type I error control and preservation of power compared to the different BI models across the different IPSS simulation scenarios. Notably and surprisingly, when simulating from BI model IPSS-C, the CV model (IPSS-A) had substantially higher power compared to BI model IPSS-B although they both shared a similar longitudinal model structure. Furthermore, model IPSS-A had higher power to detect a drug effect than the BI simulation model IPSS-C. A potential explanation may be that probabilistic models such as BI (and OC) do not incorporate residual error in the same manner as the CV approach. The residual error component in CV models may be an important factor in terms of signal-to-noise, as it describes residual error through a random effect (or two in the case of a combined error model) and thereby differs from the standard BI fixed effect g() function (e.g., as in model IPSS-B). Model IPSS-A implemented a combined residual error model, and in sensitivity analyses, similar power and type I error was observed with a CV model implementing an additive residual error model (data not shown). CV modeling of bounded scores using a combined error model has previously been reported to result in ill behavior (23). However, this was not the case in the current work, as model IPSS-A converged successfully, yielded a lower AIC than implementing an additive residual error model, and did not suffer in terms of type I error and power performance in detecting a drug effect. Lastly, the loss of power in IPSS-C may potentially be explained by the very high correlation between random effect parameters Drift and Asy in model IPSS-C, hindering clear distinction between these parameters during estimation, and thereby limiting the power to detect a drug effect.
The BI QoL model with no random effect in g() (model QoL-B) showed the best type I error control with no loss of power across the different QoL score simulation scenarios (Fig. 2), highlighting that this type of BI approach may be well-suited for detecting drug effects in trials using smaller scales for which using a CV approach is not viable. The poor type I error control observed with the OC models of the QoL score (QoL-A) and the BII (BII-B), respectively, may be explained by the limited number of IIV parameters that may be incorporated into OC models. A standard OC PO model with a single random effect on the baseline logit probability was used in the current work. BI models may allow for a greater number of IIV parameters to be incorporated and hence potentially would allow for more flexibility for describing heterogeneous and stochastic data while accurately detecting drug effects.
Meaningful comparison of the power to detect a drug effect between models can only be made when their type I error rate is comparable. Therefore, no comparison of power was made when the type I error of models differed substantially. Adjustment for type I error was performed for power comparison in an exploratory fashion (data not shown), yet accurate determination of type I error adjusted power may require many more trial replicates (e.g., ~ 10,000) (24).
This work is the first to investigate the power and type I error of the BI approach. The overall findings indicate that the methodology performs well in comparison to traditional methods when no IIV is included in the g() function. However, further research to optimize its performance in detecting drug effects may be required, particularly when including IIV in the g() variance function. Individual model averaging (25,26), which has recently shown high ability to control the type I error of detecting a drug effect in the presence of model misspecification, may be of interest to investigate in this context. Moreover, in the original presentation of the BI methodology (11) as well as in the current study, probits as driven by the standard normal distribution determined the score cut-offs, and a normal distribution described the mean-variance (f()-g()) function. The impact on type I error and power when using other distribution functions in BI models as well as further developments to the BI g() function may be of interest to inspect. Moreover, as other methods for analyzing bounded score data have been presented, such as beta-regression (27), censoring (28), and the coarsened grid (29), the current results emphasize that further research examining the power and type I error of these methods is also of interest. Lastly, the current simulation scenarios assumed a parallel-group placebo-controlled trial design spanning a 6-month period, similar to the CS36 trial. Offset drug effects were also exclusively investigated in the simulation scenarios. Future research may potentially seek to investigate the performance of models while varying trial design characteristics (such as study duration) and other types of drug effects.
Joint bounded integer model
A joint BPH-LUTS scale BI model was developed, incorporating responses to the IPSS, QoL score, and BII in individual patients over the 6-month trial period. This allowed for quantification of the connection between scores on each scale and thus achieved the third objective of the current paper. Knowledge of the relationship between scores on different BPH-LUTS scales may be useful, e.g., for comparison of patient population characteristics in different BPH-LUTS clinical trials, where trial inclusion is commonly contingent on patients’ response to one or more BPH-LUTS scales and may differ substantially between trials. In clinical diagnosis of BPH-LUTS, three categories of BPH-LUTS severity have been specified based on the IPSS: mild (0 to 7), moderate (8,9,10,11,12,13,14,15,16,17,18, to 19), and severe (20 to 35) (3). In the current model, it was estimated that mild BPH-LUTS translates to a QoL score ≤ 1 or a BII ≤ 2, moderate BPH-LUTS translates to a QoL score of 2 or 3 or a BII of at least 3 and maximally 6, and lastly, severe BPH-LUTS translates to a QoL score ≥ 4 or a BII ≥ 7. Furthermore, it was estimated that an IPSS ≥ 13 corresponds to a QoL score ≥ 3, which is consistent with the inclusion criteria used in the currently analyzed trial, as well as many other BPH-LUTS clinical trials. Within the scope of BPH-LUTS clinical trials designed in similar fashion to the CS36 trial, the joint BI model may also be used for predictive purposes. For example, it may be served in obtaining knowledge regarding the longitudinal trajectory of the QoL and BII in patients should only IPSS data be available from patients. Given that similar longitudinal parameter estimates were obtained in the IPSS BI approach (model IPSS-D) and in the joint BI model, prediction of QoL and BII data may be achieved through initial development of an IPSS BI model followed by input of the longitudinal parameter estimates into a joint BI model to be used for simulation. The currently reported cut-off estimates for the QoL score and the BII (as well as the latter scale’s separate variance g() function) could then be used to simulate these scores. It is to be noted that using a joint BI modeling approach may serve as the primary modeling strategy (instead of developing separate BI models for each scale) and has been utilized in previous work (15,30). Use of a joint BI approach is also supported in the current work given the adequate description of data from each scale as assessed through VPCs. Ultimately, the choice between individual and joint BI modeling likely depends on the goal of the pharmacometric analysis, and further research may seek to emphasize the benefits of each of the two approaches depending on the latter.
The relationship between the IPSS and QoL scores in the joint BI model was estimated with low uncertainty, while larger imprecision was observed for the estimated BII cut-offs. This may be explained by the fewer observed BII measurements per patient compared to the QoL in the current data (three versus eight measurements per patient over the 6-month trial period). The high uncertainty was especially evident for cut-offs for BII scores above 10, which may be explained by fewer of these scores being observed in the current data set. Another way to connect scores on different scales is by the use of IRT modeling, where patients’ underlying disability serves as the link between scales. Good alignment with the results of such analysis (13) was seen with the current BI approach. Lastly, covariate relationships may be of interest to investigate to further improve the joint BI model. Due to long run times with the current model, this was not performed in this study.
Conclusion
This paper presents the development of BI models for three different commonly used scales within BPH-LUTS based on data from a Phase II clinical trial. Through simulations, this study sheds light on the type I error and power to detect a drug effect of BI modeling in comparison to traditional methods for analyzing bounded score data from different BPH-LUTS scales. Overall, the CV approach was more robust compared to the BI approach although it violates the integer nature of the data. BI modeling without IIV in the variance function performed similarly to the CV approach in most cases; however, further research may seek to optimize its performance. Further research on type I error control of BI models with IIV in the BI variance function may be of high interest. In general, the OC approach showed higher type I error in detecting a drug effect compared to the BI approach, and the latter may therefore be an attractive approach for detecting drug effects in longitudinal analysis of trials using scales with few categories as endpoints. Lastly, a joint BI model was allowed for estimation of the relationship between scores of the IPSS, QoL, and BII scales, which may be useful knowledge in clinical diagnosis and translation between clinical trial inclusion criteria and results.
References
Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132(3):474–9.
Medina JJ, Parra RO, Moore RG. Benign prostatic hyperplasia (the aging prostate). Med Clin North Am. 1999;83(5):1213–29.
Barry MJ, Fowler FJ, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549–57 discussion 1564.
US Food and Drug Administration. Guidance for the non-clinical and clinical investigation of devices used for the treatment of benign prostatic hyperplasia (BPH) (2010). <https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-non-clinical-and-clinical-investigation-devices-used-treatment-benign-prostatic-hyperplasia> Accessed March 20, 2020.
Griffith JW. Self-report measurement of lower urinary tract symptoms: a commentary on the literature since 2011. Curr Urol Rep. 2012;13(6):420–6.
O’leary MP. Validity of the “bother score” in the evaluation and treatment of symptomatic benign prostatic hyperplasia. Rev Urol. 2005;7(1):1–10.
Barry MJ, Williford WO, Chang Y, Machi M, Jones KM, Walker-Corkery E, et al. Benign prostatic hyperplasia specific health status measures in clinical research: how much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? J Urol. 1995;154(5):1770–4.
O’Leary MP, Wei JT, Roehrborn CG, Miner M. BPH Registry and patient survey steering committee. Correlation of the International Prostate Symptom Score bother question with the benign prostatic hyperplasia impact index in a clinical practice setting. BJU Int. 2008;101(12):1531–5.
Barry MJ, Fowler FJ, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK. Measuring disease-specific health status in men with benign prostatic hyperplasia. Measurement Committee of The American Urological Association. Med Care. 1995;33(4 Suppl):AS145–55.
Hu C. On the comparison of methods in analyzing bounded outcome score data. AAPS J. 2019;21(6):102.
Wellhagen GJ, Kjellsson MC, Karlsson MO. A bounded integer model for rating and composite scale data. AAPS J. 2019;21(4):74.
Lyauk YK, Jonker DM, Lund TM, Hooker AC, Karlsson MO. Item response theory modeling of the International Prostate Symptom Score in patients with lower urinary tract symptoms associated with benign prostatic hyperplasia. AAPS J. 2020;22(5):115.
Lyauk YK, Lund TM, Hooker AC, Karlsson MO, Jonker DM. Integrated item response theory modeling of multiple patient-reported outcomes assessing lower urinary tract symptoms associated with benign prostatic hyperplasia. AAPS J. 2020;22(5):98.
Sheiner LB. A new approach to the analysis of analgesic drug trials, illustrated with bromfenac data. Clin Pharmacol Ther. 1994;56(3):309–22.
Germovsek E, Hansson A, Kjellsson MC, Ruixo JJP, Westin Å, Soons PA, et al. Relating nicotine plasma concentration to momentary craving across four nicotine replacement therapy Formulations. Clin Pharmacol Therapeut. 2020;107(1):238–45.
Keizer RJ, Karlsson MO, Hooker A. Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT Pharmacometrics Syst Pharmacol. 2013;2:e50.
Karlsson MO, Jonsson EN, Wiltse CG, Wade JR. Assumption testing in population pharmacokinetic models: illustrated with an analysis of Moxonidine data from congestive heart failure patients. J Pharmacokinet Pharmacodyn. 1998;26(2):207–46.
Silber HE, Kjellsson MC, Karlsson MO. The impact of misspecification of residual error or correlation structure on the type I error rate for covariate inclusion. J Pharmacokinet Pharmacodyn. 2009;36(1):81–99.
Litière S, Alonso A, Molenberghs G. Type I and Type II error under random-effects misspecification in generalized linear mixed models. Biometrics. 2007;63(4):1038–44.
Barr DJ, Levy R, Scheepers C, Tily HJ. Random effects structure for confirmatory hypothesis testing: Keep it maximal. J Mem Lang. 2013;68(3):255–78.
Clark HH. The language-as-fixed-effect fallacy: A critique of language statistics in psychological research. J Verbal Learn Verbal Behav. 1973;12(4):335–59.
Bolker BM, Brooks ME, Clark CJ, Geange SW, Poulsen JR, Stevens MHH, et al. Generalized linear mixed models: a practical guide for ecology and evolution. Trends Ecol Evol (Amst). 2009;24(3):127–35.
Hu C, Randazzo B, Sharma A, Zhou H. Improvement in latent variable indirect response modeling of multiple categorical clinical endpoints: application to modeling of guselkumab treatment effects in psoriatic patients. J Pharmacokinet Pharmacodyn. 2017;44(5):437–48.
Wählby U, Bouw MR, Jonsson EN, Karlsson MO. Assessment of type I error rates for the statistical sub-model in NONMEM. J Pharmacokinet Pharmacodyn. 2002;29(3):251–69.
Tessier A, Chasseloup E, Karlsson MO. Use of mixture models in pharmacometric model-based analysis of confirmatory trials: part I - simulation study evaluating type I error and power of proof-of-concept trials Abstr 9122. 2019 Population Approach Group Europe (PAGE).
Chasseloup E, Tessier A, Karlsson MO. Use of mixture models in pharmacometric model-based analysis of confirmatory trials: part II – control of the type I error with real placebo data Abstr 9149. 2019 Population Approach Group Europe (PAGE).
Smithson M, Verkuilen J. A better lemon squeezer? Maximum-likelihood regression with beta-distributed dependent variables. Psychol Methods. 2006;11(1):54–71.
Hutmacher MM, French JL, Krishnaswami S, Menon S. Estimating transformations for repeated measures modeling of continuous bounded outcome data. Stat Med. 2011;30(9):935–49.
Hu C, Yeilding N, Davis HM, Zhou H. Bounded outcome score modeling: application to treating psoriasis with ustekinumab. J Pharmacokinet Pharmacodyn. 2011;38(4):497–517.
Germovsek E, Hansson A, Karlsson MO, Westin Å, Soons PA, Vermeulen A, et al. A time-to-event model relating integrated craving to risk of smoking relapse across different nicotine replacement therapy formulations. Clin Pharmacol Therapeut. 2021;109(2):416–23.
Acknowledgments
The authors would like to thank Gustaf Wellhagen and Eva Germovsek for valuable input and discussions during this work.
Funding
Open access funding provided by Uppsala University. This work was funded jointly by the Danish Innovation Fund (grant number 5189-00064b), Ferring Pharmaceuticals A/S, and the Swedish Research Council Grant 2018-03317.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Y.K.L and D.M.J. are employees of Ferring Pharmaceuticals A/S. The authors report no other conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 2012 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lyauk, Y.K., Jonker, D.M., Hooker, A.C. et al. Bounded Integer Modeling of Symptom Scales Specific to Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia. AAPS J 23, 33 (2021). https://doi.org/10.1208/s12248-021-00568-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-021-00568-y