Abstract
Ciliated muconodular papillary tumor (CMPT) is a rare type of tumor with both benign and malignant characteristics. Herein, we report the surgical case of a 65-year-old man with CMPT. Chest computed tomography revealed a solitary cavitary lesion with a maximum diameter of 11-mm in S10b of the right lower lung. A thoracoscopic lung wedge resection was subsequently performed. On microscopic examination, the tumor was composed of highly columnar cells with tubular-to-papillary and cystic growth patterns. On immunostaining, it was positive for the epidermal growth factor receptor. The tumor was diagnosed as a CMPT, exhibiting no recurrence after two years of follow-up.
Similar content being viewed by others
Introduction
Ciliated muconodular papillary tumor (CMPT) is a rare lung tumor that was first reported in 2002. This tumor involves ciliated, goblet, and basal cell proliferation with mucin secretion [1]. On computed tomography (CT), CMPT commonly presents as ground-glass opaque peripheral nodules, while cavitary formation is rarely observed. This study presents a surgical case of CMPT in a 65-year-old man with a cavitary lesion in the right lower lung field identified on chest CT. The diagnostic pitfalls and considerations are further discussed.
Case
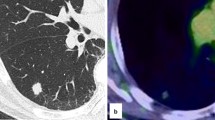
A 65-year-old man had been referred to our hospital for evaluation 4 years prior, after the detection of a cavitary lesion on chest CT during routine health screening. He had a history of hyperlipidemia and impaired glucose tolerance. Laboratory examination revealed elevated triglyceride and LDL-cholesterol levels. The serum levels of the tumor markers carcinoembryonic antigen (CEA), pro-gastrin-releasing peptide, and squamous cell carcinoma antigen were within the normal limits. CT revealed a solitary cavitary lesion with a maximum diameter of 11 mm in S10b of the right lower lung (Fig. 1). 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET) revealed no abnormal FDG accumulation in the tumor or lymph nodes. Thoracoscopic lung wedge resection was subsequently performed under one-lung anesthesia to verify the presence of a primary malignancy (Fig. 2). The resected specimen showed an 11-mm cavity, and intraoperative analysis of the frozen section revealed only inflammatory changes; therefore, additional lobectomy was not performed. On microscopic examination, the tumor was composed of tall columnar cells, exhibiting tubular-to-papillary and cystic growth patterns (Fig. 3a, b). Lymphocyte infiltration was further observed in the interstitium. On immunohistochemical staining, basal cells were positive for p40, and alveolar epithelial cells were positive for thyroid transcription factor 1 (TTF-1) (Fig. 4a, b). Tall columnar cells strongly expressed epidermal growth factor receptor (EGFR) and v-raf murine sarcoma viral oncogene homolog B1 V600E (BRAF V600E) and anaplastic lymphoma kinase (ALK) were not expressed (Fig. 4c–e). The final pathological diagnosis was CMPT. The postoperative course was uneventful, with no recurrence 2 years later.
Discussion
CMPT (which was first reported in 2002) is a rare tumor that develops in the peripheral lung. This lesion exhibits papillary growth during alveolar replacement, and ciliated and goblet cells are accompanied by mucus production [1]. CMPT was classified as an adenoma in the 5th edition of the WHO classification [2]; however, CMPT has been described as having both benign and malignant features. The presence of cilia, basal cells, and a low Ki-67 index are all indicators of a benign tumor. Conversely, findings, suggestive of a malignant tumor include a ruptured alveolar structure, central fibrosis, proliferation along the alveolar walls and skip lesions, lack of encapsulation, micropapillary patterns, and positive staining for CEA. The immunohistochemical findings of this tumor are similar to those of lung adenocarcinoma. CMPT is typically positive for CEA, TTF-1, and cytokeratin (CK) 7, but negative for CK20 [3, 4]. Although the malignant potential of CMPT remains unknown, some studies have associated it with various gene alterations. Recently, EGFR, ALK, AKT1, KRAS, BRAF, and HRAS gene mutations were all detected via gene analyses among patients with CMPT [5,6,7]. These findings are suggestive of a neoplastic change. Thus, their malignant potential requires further investigation.
CMPT is frequently detected incidentally as a small, peripheral, ground-glass opacity or nodule on CT. In a previous study examining 38 cases of CMPTs (17 men and 21 women), the mean age at identification was 68 years (range 50–84 years), and the average tumor diameter was 1.1 cm (range 0.4–4.5 cm) [8]. Most CMPT lesions developed in the peripheral lesions of the lung with approximately 79.4–81.5% occurring in the lower lobe [8, 9]. CT findings included nodular shadows in 28 patients (73.7%) and hollow shadows and ground-glass-like shadows in the remaining 10 (26.3%). In another study, the CT findings of 16 patients with CMPTs, including eight (50.0%) with solid nodules, seven (43.8%) with high-density ground-glass nodules (GGNs), and one (6.3%) with pure GGNs, were examined. CMPTs grew very slowly at 0.49 mm/year in maximal diameter. Moreover, 10 out of 16 lesions (62.5%) were found near the pleura [9]. Based on this, it may be difficult to distinguish CMPT from lung cancer, when pleural changes are present.
FDG-PET findings of 15 patients with surgically resected CMPTs showed moderate FDG uptake in one patient, with the maximum standardized uptake values (SUVmax) of 3.67. The remaining 14 patients showed mild FDG uptake, with the SUVmax ranging from 0.57 to 1.35. According to the relationship between FDG accumulation and pathological lymphocyte infiltration, cases with mild FDG accumulation exhibit minimal lymphocyte infiltration and large amounts of mucin. Meanwhile, cases with moderate FDG accumulation exhibit significant lymphatic infiltration [10].
Since CMPT often presents as a small nodule in the peripheral lesion of the lung, it is difficult to diagnose on bronchoscopy. As such, surgical resection is often performed to confirm the diagnosis. In 38 CMPT cases, partial resection was performed in 27 (71.1%), while segmentectomy was performed in one, and lobectomy was performed in 10 [8]. When sufficient excision margins are obtained in the excision range, a partial excision is considered curative [11]. In this case, the maximum tumor diameter was 11 mm, and malignant findings were not observed in the intraoperative analysis of the frozen sections. Therefore, a sufficient resection margin was secured, and the operation was successfully completed via partial resection.
The prognosis for CMPT is good, and no recurrence or metastasis was reported during the mean follow-up period of 33.8 months [8]. Since the pathological findings of CMPT exhibit both benign and malignant characteristics, careful follow-up is necessary. In conclusion, this study reports a rare case of CMPT, which was managed by thoracoscopic lung wedge resection, with no recurrence detected in 2 years of follow-up.
Availability of data and materials
Not applicable.
Abbreviations
- CMPT:
-
Ciliated muconodular papillary tumor
- CT:
-
Computed tomography
- CEA:
-
Carcinoembryonic antigen
- FDG:
-
18 F-fluorodeoxyglucose
- PET:
-
Positron emission tomography
- EGFR:
-
Epidermal growth factor receptor
- ALK:
-
Anaplastic lymphoma kinase
- CK:
-
Cytokeratin
- AKT1:
-
Serine/threonine kinase 1
- KRAS:
-
v-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog
- BRAF:
-
v-raf murine sarcoma viral oncogene homolog B1
- SUVmax:
-
Maximum standardized uptake values
References
Ishikawa Y. Ciliated muconodular papillary tumor of the peripheral lung: benign or malignant? Pathol Clin Med. 2002;20:964–5.
WHO classification of tumours, 5th ed. Vol.5 Thoracic tumours. IARC; 2021.
Harada T, Akiyama Y, Ogasawara H, Kishi F, Hattori A, Okamoto K, et al. Ciliated muconodular papillary tumor of the peripheral lung: a newly defined rare tumor. Respir Med CME. 2008;1:176–8.
Sato S, Koike T, Homma K, Yokoyama A. Ciliated muconodular papillary tumour of the lung: a newly defined low-grade malignant tumour. Interact Cardiovasc Thorac Surg. 2010;11:685–7.
Kamata T, Yoshida A, Kosuge T, Watanabe S, Asamura H, Tsuta K. Ciliated muconodular papillary tumors of the lung: a clinicopathologic analysis of 10 cases. Am J Surg Pathol. 2015;39:753–60.
Chang JC, Montecalvo J, Borsu L, Lu S, Larsen BT, Wallace WD, et al. Bronchiolar adenoma expansion of the concept of ciliated muconodular papillary tumors with proposal for revised terminology based on morphologic immunophenotypic, and genomic analysis of 25 cases. Am J Surg Pathol. 2018;42:1010–26.
Liu L, Aesif SW, Kipp BR, Voss JS, Daniel S, Aubry MC, et al. Ciliated muconodular papillary tumors of the lung can occur in western patients and show mutations in BRAF and AKT1. Am J Surg Pathol. 2016;40:1631–6.
Osugi J, Hasegawa T, Nozawa Y, Fujiu K, Yue C. A surgical case of ciliated muconodular papillary tumor in the left lower lobe of the lung. Jpn J Chest Surg. 2021;35:44–50.
Onishi Y, Kusumoto M, Motoi N, Watanabe H, Watanabe SI. Ciliated Muconodular papillary tumor of the lung: thin-section CT findings of 16 cases. AJR Am J Roentgenol. 2020;214:61–5.
Onishi Y, Ito K, Motoi N, Motoi N, Morita T, Watanabe SI, et al. Ciliated muconodular papillary tumor of the lung: 18F-PET/CT findings of 15 cases. Ann Nucl Med. 2020;34:448–52.
Yuki D, Kawano O, Fukai I, Uchiyama T, Baba Y, Murata T. A surgical case of a ciliated muconodular tumor that required additional exploration to distinguish it from mucinous adenocarcinoma in situ. Jpn J Lung Canc. 2013;53:831–5.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Hiroaki Shidei, Hiroe Aoshima, and Masato Kanzaki conceived of this study design. Hiromi Onizuka, Yoji Nagashima, and Yukio Nakatani participated in providing the pathological findings. All authors performed this study and collated this manuscript as a group effort. Hiroaki Shidei wrote the first draft of the manuscript. Hiroe Aoshima assisted Hiroaki Shidei in preparing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient for the publication of this case report and the accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shidei, H., Aoshima, H., Ogihara, A. et al. A surgical case of ciliated muconodular papillary tumor of the lung. Gen Thorac Cardiovasc Surg Cases 2, 29 (2023). https://doi.org/10.1186/s44215-022-00024-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44215-022-00024-z