Abstract
Background
Arterial hypotension is common in patients during surgery and those admitted to the intensive care unit (ICU) postoperatively. Perioperative arterial hypotension reportedly significantly affects surgical patients’ outcomes. Blood pressure level is the most crucial factor that influences organ perfusion. Hypoperfusion and organ dysfunction are correlated based on their severity associated with hypotension. As several factors can cause intraoperative hypotension, anesthetists must promptly identify the etiology for appropriate treatment and revert the patient’s hemodynamic profile.
Objectives
This review discusses the concept of perioperative hypotension, identifies its effects in clinical situations, and provides remedies and techniques to predict and avoid its significant consequences.
Conclusions
The primary determinant of organ perfusion is blood pressure. On the other hand, profound hypotension is common in surgical patients and is connected to hypoperfusion and organ failure. Currently, hypotension is addressed once low blood pressure levels are recorded. Early detection of oncoming hypotension or its clinical prediction is of paramount importance in allowing the clinician to treat hypotension and reduce the incidence and length of hypotensive episodes promptly and aggressively.
Similar content being viewed by others
Background
When examining organ-specific outflow pressure, mean arterial pressure (MAP) is the fundamental predictor of end-organ perfusion. Healthy people’s blood pressure changes greatly during the day, although it may be kept steady within certain parameters. Patients who are undergoing surgery, who are critically ill, and who have tissue hypoperfusion and organ damage are more likely to experience profound hypotension [1, 2].
Intraoperative hypotension has been linked to a higher risk of postoperative mortality [3, 4], myocardial injury after non-cardiac surgery (MINS) [5], myocardial infarction [6], cardiogenic shock [7], acute renal failure [8], delirium [2], and stroke [9] in patients undergoing non-cardiac surgery under general anesthesia [10,11,12,13,14]. Although blood flow autoregulation protects the brain, heart, and kidneys from hypotension-induced hypoperfusion, blood pressure is almost entirely responsible for perfusion of other organ systems, particularly splanchnic organs, such as the stomach, liver, and pancreas, which have a low blood flow autoregulation capacity [15]. Intermittent or continuous blood pressure monitoring using invasive or non-invasive measurement methods is the standard of care in perioperative and critical care medicine to preserve patient safety and improve perfusion pressure. To reduce the overall degree of severe hypotension, imminent hypotension is increasingly being recognized and treated early.
In the present review, we discuss the concept of hypotension, identify its effects in most clinical situations, and provide remedies and techniques to predict and avoid its significant consequences.
The physiology of blood pressure
Systolic arterial pressure (SAP) is the maximum pressure measured in the arterial vasculature and arises from the contraction of the left ventricle. It depends on stroke volume (SV), heart rate (HR), systemic vascular resistance (SVR), the distensibility of the aorta, and the large arteries near the heart. The lowest pressure recorded in the arterial tree is called diastolic arterial pressure (DAP). DAP is influenced by SVR, compliance of the vasculature (“windkessel model” of the vasculature), the duration of diastole, and the duration of the cardiac cycle [16].
Mean arterial pressure (MAP) is the average arterial pressure throughout one cardiac cycle.
Cardiac output (CO) and SVR are the determinants of MAP. The MAP value is under the control of the renin-angiotensin-aldosterone system and the autonomic nervous system, whose complex physiology is well beyond the scope of this review. However, it is important to emphasize that anesthesiologists should be aware of the implications of changes in both peripheral resistance and circulating volume on MAP via regulation of the carotid sinus and aortic arch baroceptors and the renin-angiotensin-aldosterone cascade. In fact, most of the anesthesia drugs and techniques routinely used and many factors related to the surgical procedure occurring perioperatively, of which blood loss is a caricatural example, can alter either the vascular tone or the plasma volume.
The goal of physiological regulation of blood pressure and flow with the oxygen content of arterial blood is to facilitate adequate tissue oxygenation.
Systemic perfusion pressure (PP) regulates the blood flow of the whole organism [17]. PP is calculated as MAP–central venous pressure (CVP). When analyzing the single end-organ perfusion instead, it is less correct to refer to CVP as downstream pressure; hence, the closing pressure (CP) of the respective area or tissue should be taken into account.
The best example of such a concept is the perfusion of the brain, which, under physiological conditions, depends on the cerebral perfusion pressure (CPP), which is calculated as MAP–intracranial pressure (ICP), where ICP is assimilated CP or downstream pressure. An analog case occurs under pathological conditions in other body areas, such as in the muscle compartment or the abdomen, when compartment syndrome occurs.
In some organs, such as the brain, spinal cord, kidneys, and heart, blood flow is kept constant within MAP limits of autoregulation blood flow [18]. On the other hand, autoregulation occurs within a defined range of blood pressure. For example, for cerebral perfusion, MAP values in healthy individuals are 60–160 mmHg, within which blood flow is kept constant.
Kidneys blood flow is maximal within 70–130 mmHg of MAP values [19]; therefore, glomerular filtration is optimal in this pressure range.
Myocardial blood flow is autoregulated within certain limits of coronary perfusion pressure (CoPP), although myocardial perfusion is not maintained at a constant value; instead, it is adjusted to the current myocardial O2 demand [20].
In daily routine, blood pressure is often used as a surrogate for blood flow. Nevertheless, perioperative changes in blood pressure are unreliable substitutes for simultaneous changes in cardiac output (CO), as demonstrated in 402 anesthetized patients undergoing different surgical procedures [21]. In each case, the blood pressure parameters SAP, DAP, MAP, PP, and CO were measured before and after the administration of a fluid bolus of 500 ml colloidal solution for 10–20 min. As the CO increased by > 15%, a positive response to the volume expansion was evaluated. Although blood pressure parameters increased more in responders than in non-responders, relative changes in pressure values showed low sensitivity and specificity. Thus, the relative pressure changes failed to predict changes in CO in more than half of the patients. Similar results were found in patients with septic shock [19].
Defining arterial hypotension
Whereas blood pressure management is a pillar of anesthetic care perioperatively, the definition of hypotension remains challenging. Although there are numerous references that support the need for perioperative blood pressure regulation [22,23,24,25], at present, there are no universally accepted perioperative blood pressure thresholds to define hypotension [26].
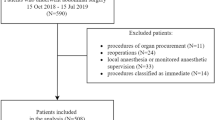
Weinber and colleagues published a comprehensive study of intraoperative hypotension criteria in adults who underwent non-cardiac surgery [27]. Hypotension was mostly defined by changes in SAP, MAP, or a combination of the two. The investigators tried to determine whether studies reported an absolute threshold value for hypotension, hypotension as a change from a pressure baseline value, a baseline blood pressure for reporting relative threshold values, and a methodology for determining the severity of hypotension.
The majority of studies reported a MAP < 60 mmHg and/or a SAP < 90 mmHg as absolute numerical thresholds for hypotension. A total of 126 studies used a relative threshold to represent hypotension, most of which showed a percentage decrease (10 to 60%) from baseline for either MAP or SAP (Fig. 1). Other hypotension definitions refer to a blood pressure requiring therapeutic interventions, such as volume expansion or vasoactive medications.
Causes of perioperative hypotension
The causes of perioperative hypotension can be related to the patient, anesthesia, or surgery.
Preoperative risk factors associated with hypotension are advanced age, low blood pressure before anesthesia induction, hypovolemia [28,29,30], higher American Society of Anesthesiologists (ASA) status, chronic treatment with antihypertensive drugs, and planned high-risk surgery [31,32,33,34](Fig. 2).
Whereas beta blockers and calcium antagonists have direct recommendations relating to the perioperative regime, because they have been associated with both injury and benefit, there is controversy about whether angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers (ACE-Is/ARBs) should be maintained in the perioperative period. Intraoperative hypotension caused by ACE-I and ARB medication that persists throughout the perioperative period [35] has been linked to severe perioperative morbidity [36] and has prompted some clinicians to discontinue treatment. The current perioperative guidelines are divided in their recommendations for continuing or stopping ACEIs/ARBs during surgery.
According to the 2014 American College of Cardiology/American Heart Association guidelines [31], continuing therapy before surgery is appropriate. Additionally, if therapy is stopped, it should be resumed as soon as clinically possible, whereas the Canadian Cardiovascular Society’s most recent guidelines [32] recommend skipping therapy 24 h before surgery (strong recommendation, low quality of evidence).
The European Society of Cardiology/European Society of Anaesthesiology approach [33], on the other hand, bases its recommendations on the indication for ACE-I/ARB treatment, including 24-h termination if the medication is indicated for hypertension and continuation if it is prescribed for heart failure or left ventricular systolic dysfunction [33].
In addition, if these latter patients are not on ACE-I/ARB medication prior to surgery, recommendations advise starting it one week before surgery [34].
Intraoperative hypotension has a complex origin, and it is most prevalent in patients undergoing surgery under general and neuraxial anesthesia [9, 37,38,39]. The main factors contributing to hypotension intraoperatively are excessive depth of anesthesia [40, 41], blood loss [42], and vasodilation.
Hypotension is also common in postoperative care in the ICU. Several causes can be listed, including myocardial ischemia [43], hypovolemia, arrhythmias [44, 45], vasoplegia, dynamic left ventricle outflow tract (LVOT) obstruction [46, 47], pneumothorax [48], tamponade [49], pulmonary embolism [50], sepsis [51], and bleeding [52].
Remedies to treat hypotension
Although patient-related causes of hypotension are not modifiable, there is room for the anesthetic team to intervene on anesthesia- and surgery-related causes to prevent or promptly reverse hypotension (Fig. 3, Table 1).
Treatment of any specific cause of hypotension should be pursued in a timely and appropriate manner. To do so, identifying and correcting the underlying pathophysiologic mechanisms, such as decreased cardiac preload, altered cardiac afterload, or reduced myocardial contractility, is pivotal for causal treatment of hypotension [12].
Predicting hypotensive episodes may lead to preventive treatment and assist in avoiding hypotension. Recently, a new technology based on AI has shown promise in predicting hypotension. Hatib et al. developed a “hypotension prediction index” (HPI) to predict real-time hypotension [53]. They used machine learning to analyze many hemodynamic variables collected from the arterial blood pressure waveform in real time. After the verified the method, the model predicted arterial hypotension 15 min ahead of time, with a sensitivity of 88% and a specificity of 87%.
Wijnberge et al. [54] presented the Hypotension Prediction (HYPE) trial, in which 68 patients undergoing elective non-cardiac surgery were randomly assigned to either an AI early warning system for intraoperative treatment (intervention group) or conventional care (control group). The goal of their study was to investigate whether the intervention decreased the depth and duration of intraoperative hypotension. As evidenced by the primary result of a decreased time-weighted average of intraoperative hypotension, the trial showed that the intervention successfully reduced patients' exposure to hypotension.
Although physicians may use arterial pulse pressure waveforms to make reasonable judgments about the risk of forthcoming episodes of hypotension, there is a good chance that an AI system might make more accurate predictions [55].
Conclusions
Blood pressure is a critical factor in determining organ perfusion. Perioperative hypotension is common and is linked to hypoperfusion and organ failure. Therefore, optimal management of arterial blood pressure is required in the perioperative setting to avoid complications.
Currently, hypotension is addressed once low blood pressure levels are recorded. Preoperative risk stratification for perioperative hypotension, intraoperative, and postoperative early detection of oncoming hypotension or its clinical prediction allow the clinician to treat hypotension and reduce the incidence and length of hypotensive episodes. Machine learning-based algorithms have recently been applied to predict hypotension. However, clinical trials are needed to confirm the ability of new technologies to effectively predict hypotension cases.
Based on current knowledge, anesthesiologists should carefully screen patients at risk for hypotension at the time of the preoperative evaluation, pay a high level of attention to the perioperative clinical management to avoid hypotensive episodes, and treat the disease aggressively in a timely fashion.
Availability of data and materials
Not applicable
Abbreviations
- ICU:
-
Intensive care unit
- MAP:
-
Mean arterial pressure
- SAP:
-
Systolic arterial pressure
- DAP:
-
Diastolic arterial pressure
- SVR:
-
Systemic vascular resistances
- CVP:
-
Central venous pressure
- CPP:
-
Cerebral perfusion pressure
- ICP:
-
Intracranial pressure
- CO:
-
Cardiac output
- PP:
-
Perfusion pressure
- ASA:
-
American Society of Anesthesiologists status
- AI:
-
Artificial intelligence
- HPI:
-
Hypotension prediction index
References
Wesselink EM, Kappen TH, Torn HM, Slooter AJC, van Klei WA (2018) Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 121(4):706–721. https://doi.org/10.1016/j.bja.2018.04.036
Maheshwari K, Ahuja S, Khanna AK, Mao G, Perez-Protto S, Farag E, Turan A, Kurz A, Sessler DI (2020) Association between perioperative hypotension and delirium in postoperative critically ill patients: a retrospective cohort analysis. Anesth Analg. 130(3):636–643. https://doi.org/10.1213/ANE.0000000000004517
Monk TG, Saini V, Weldon BC, Sigl JC (2005) Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 100(1):4–10. https://doi.org/10.1213/01.ANE.0000147519.82841.5E
Mascha EJ, Yang D, Weiss S, Sessler DI (2015) Intraoperative mean arterial pressure variability and 30-day mortality in patients having noncardiac surgery. Anesthesiology. 123(1):79–91. https://doi.org/10.1097/ALN.0000000000000686
Roshanov PS, Sessler DI, Chow CK, Garg AX, Walsh MW, Lam NN, Hildebrand AM, Biccard BM, Acedillo RR, MacNeil SD, Lee VW, Szczeklik W, Mrkobrada M, Thabane L, Devereaux PJ (2021) Predicting myocardial injury and other cardiac complications after elective noncardiac surgery with the Revised Cardiac Risk Index: The VISION Study. Can J Cardiol. 37(8):1215–1224. https://doi.org/10.1016/j.cjca.2021.03.015
Roshanov PS, Sheth T, Duceppe E, Tandon V, Bessissow A, Chan MTV, Butler C, Chow BJW, Khan JS, Devereaux PJ (2019) Relationship between perioperative hypotension and perioperative cardiovascular events in patients with coronary artery disease undergoing major noncardiac surgery. Anesthesiology. 130(5):756–766. https://doi.org/10.1097/ALN.0000000000002654
Bertini P, Guarracino F. Pathophysiology of cardiogenic shock. Curr Opin Crit Care. 2021;27(4):409-415
Goren O, Matot I (2015) Perioperative acute kidney injury. Br J Anaesth 115(Suppl 2):ii3–i14
Bijker JB, Persoon S, Peelen LM, Moons KGM, Kalkman CJ, Kappelle LJ, van Klei WA (2012) Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology. 116(3):658–664. https://doi.org/10.1097/ALN.0b013e3182472320
Sessler DI, Meyhoff CS, Zimmerman NM, Mao G, Leslie K, Vásquez SM, Balaji P, Alvarez-Garcia J, Cavalcanti AB, Parlow JL, Rahate PV, Seeberger MD, Gossetti B, Walker SA, Premchand RK, Dahl RM, Duceppe E, Rodseth R, Botto F, Devereaux PJ (2018) Period-dependent associations between hypotension during and for four days after noncardiac surgery and a composite of myocardial infarction and death: a substudy of the POISE-2 Trial. Anesthesiology. 128(2):317–327. https://doi.org/10.1097/ALN.0000000000001985
Monk TG, Bronsert MR, Henderson WG, Mangione MP, Sum-Ping STJ, Bentt DR, Nguyen JD, Richman JS, Meguid RA, Hammermeister KE (2015) Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology. 123(2):307–319. https://doi.org/10.1097/ALN.0000000000000756
Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, Kurz A (2017) Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 126(1):47–65. https://doi.org/10.1097/ALN.0000000000001432
Sun LY, Wijeysundera DN, Tait GA, Beattie WS (2015) Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology. 123(3):515–523. https://doi.org/10.1097/ALN.0000000000000765
Walsh M, Devereaux PJ, Garg AX, Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, Sessler DI (2013) Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 119(3):507–515. https://doi.org/10.1097/ALN.0b013e3182a10e26
Meng J-B, Lai Z-Z, Xu X-J, Ji C-L, Hu M-H, Zhang G (2016) Effects of early continuous venovenous hemofiltration on E-selectin, hemodynamic stability, and ventilatory function in patients with septic-shock-induced acute respiratory distress syndrome. Biomed Res Int 2016 Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85006085580&doi=10.1155%2f2016%2f7463130&partnerID=40&md5=1491d170258cec0883165009676d5a1f
Pugsley MK, Tabrizchi R (2000) The vascular system. An overview of structure and function. J Pharmacol Toxicol Methods. 44(2):333–340. https://doi.org/10.1016/S1056-8719(00)00125-8
Kouz K, Hoppe P, Briesenick L, Saugel B (2020) Intraoperative hypotension: Pathophysiology, clinical relevance, and therapeutic approaches. Indian J Anaesth. 64(2):90–96. https://doi.org/10.4103/ija.IJA_939_19
Meng L, Wang Y, Zhang L, McDonagh DL (2019) Heterogeneity and variability in pressure autoregulation of organ blood flow: lessons learned over 100+ years. Crit Care Med. 47(3):436–448. https://doi.org/10.1097/CCM.0000000000003569
Pierrakos C, Velissaris D, Scolletta S, Heenen S, De Backer D, Vincent J-L (2012) Can changes in arterial pressure be used to detect changes in cardiac index during fluid challenge in patients with septic shock? Intensive Care Med. 38(3):422–428. https://doi.org/10.1007/s00134-011-2457-0
Goodwill AG, Dick GM, Kiel AM, Tune JD (2017) Regulation of coronary blood flow. Compr Physiol. 7(2):321–382. https://doi.org/10.1002/cphy.c160016
Le Manach Y, Hofer CK, Lehot J-J, Vallet B, Goarin J-P, Tavernier B et al (2012) Can changes in arterial pressure be used to detect changes in cardiac output during volume expansion in the perioperative period? Anesthesiology. 117(6):1165–1174. https://doi.org/10.1097/ALN.0b013e318275561d
Saugel B, Sessler DI (2021) Perioperative blood pressure management. Anesthesiology. 134(2):250–261. https://doi.org/10.1097/ALN.0000000000003610
Sanders RD, Hughes F, Shaw A, Thompson A, Bader A, Hoeft A, Williams DA, Grocott MPW, Mythen MG, Miller TE, Edwards MR, Miller TE, Mythen MG, Grocott MPW, Edwards MR, Ackland GL, Brudney CS, Cecconi M, Ince C, Irwin MG, Lacey J, Pinsky MR, Sanders R, Hughes F, Bader A, Thompson A, Hoeft A, Williams D, Shaw AD, Sessler DI, Aronson S, Berry C, Gan TJ, Kellum J, Plumb J, Bloomstone J, McEvoy MD, Thacker JKM, Gupta R, Koepke E, Feldheiser A, Levett D, Michard F, Hamilton M (2019) Perioperative Quality Initiative consensus statement on preoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 122(5):552–562. https://doi.org/10.1016/j.bja.2019.01.018
Meng L, Yu W, Wang T, Zhang L, Heerdt PM, Gelb AW (2018) Blood pressure targets in perioperative care. Hypertension. 72(4):806–817. https://doi.org/10.1161/HYPERTENSIONAHA.118.11688
Welte M, Saugel B, Reuter DA (2020) Perioperative blood pressure management : what is the optimal pressure? Anaesthesist. 69(9):611–622. https://doi.org/10.1007/s00101-020-00767-w
Schenk J, van der Ven WH, Schuurmans J, Roerhorst S, Cherpanath TGV, Lagrand WK, Thoral P, Elbers PWG, Tuinman PR, Scheeren TWL, Bakker J, Geerts BF, Veelo DP, Paulus F, Vlaar APJ, Cardiovascular Dynamics Section of the ESICM (2021) Definition and incidence of hypotension in intensive care unit patients, an international survey of the European Society of Intensive Care Medicine. J Crit Care. 65:142–148. https://doi.org/10.1016/j.jcrc.2021.05.023
Weinberg L, Li SY, Louis M, Karp J, Poci N, Carp BS, Miles LF, Tully P, Hahn R, Karalapillai D, Lee DK (2022) Reported definitions of intraoperative hypotension in adults undergoing non-cardiac surgery under general anaesthesia: a review. BMC Anesthesiol. 22(1):69. https://doi.org/10.1186/s12871-022-01605-9
Coccolini F, Moore EE, Kluger Y, Biffl W, Leppaniemi A, Matsumura Y et al (2019) Kidney and uro-trauma: WSES-AAST guidelines. World J Emerg Surg. 14(1):54. https://doi.org/10.1186/s13017-019-0274-x
Fawcett WJ, Thomas M (2019) Pre-operative fasting in adults and children: clinical practice and guidelines. Anaesthesia. 74(1):83–88. https://doi.org/10.1111/anae.14500
Chang R, Holcomb JB (2017) Optimal fluid therapy for traumatic hemorrhagic shock. Crit Care Clin. 33(1):15–36. https://doi.org/10.1016/j.ccc.2016.08.007
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, Davila-Roman VG, Gerhard-Herman MD, Holly TA, Kane GC, Marine JE, Nelson MT, Spencer CC, Thompson A, Ting HH, Uretsky BF, Wijeysundera DN, American College of Cardiology, American Heart Association (2014) 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 64(22):e77–e137. https://doi.org/10.1016/j.jacc.2014.07.944
Duceppe E, Parlow J, MacDonald P, Lyons K, McMullen M, Srinathan S, Graham M, Tandon V, Styles K, Bessissow A, Sessler DI, Bryson G, Devereaux PJ (2017) Canadian Cardiovascular Society Guidelines on Perioperative Cardiac Risk Assessment and Management for Patients Who Undergo Noncardiac Surgery. Can J Cardiol. 33(1):17–32. https://doi.org/10.1016/j.cjca.2016.09.008
Kristensen SD, Knuuti J, Saraste A, Anker S, Bøtker HE, Hert SD, Ford I, Gonzalez-Juanatey JR, Gorenek B, Heyndrickx GR, Hoeft A, Huber K, Iung B, Kjeldsen KP, Longrois D, Lüscher TF, Pierard L, Pocock S, Price S, Roffi M, Sirnes PA, Sousa-Uva M, Voudris V, Funck-Brentano C, Authors/Task Force Members (2014) 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 35(35):2383–2431. https://doi.org/10.1093/eurheartj/ehu282
Hollmann C, Fernandes NL, Biccard BM (2018) A systematic review of outcomes associated with withholding or continuing angiotensin-converting enzyme inhibitors and angiotensin receptor blockers before noncardiac surgery. Anesth Analg. 127(3):678–687. https://doi.org/10.1213/ANE.0000000000002837
Bertrand M, Godet G, Meersschaert K, Brun L, Salcedo E, Coriat P (2001) Should the angiotensin II antagonists be discontinued before surgery? Anesth Analg. 92(1):26–30. https://doi.org/10.1097/00000539-200101000-00006
Roshanov PS, Rochwerg B, Patel A, Salehian O, Duceppe E, Belley-Côté EP, Guyatt GH, Sessler DI, le Manach Y, Borges FK, Tandon V, Worster A, Thompson A, Koshy M, Devereaux B, Spencer FA, Sanders RD, Sloan EN, Morley EE, Paul J, Raymer KE, Punthakee Z, Devereaux PJ (2017) Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin ii receptor blockers before noncardiac surgery: an analysis of the vascular events in noncardiac surgery patients cohort evaluation prospective cohort. Anesthesiology. 126(1):16–27. https://doi.org/10.1097/ALN.0000000000001404
Südfeld S, Brechnitz S, Wagner JY, Reese PC, Pinnschmidt HO, Reuter DA, Saugel B (2017) Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J Anaesth. 119(1):57–64. https://doi.org/10.1093/bja/aex127
Maheshwari K, Turan A, Mao G, Yang D, Niazi AK, Agarwal D, Sessler DI, Kurz A (2018) The association of hypotension during non-cardiac surgery, before and after skin incision, with postoperative acute kidney injury: a retrospective cohort analysis. Anaesthesia. 73(10):1223–1228. https://doi.org/10.1111/anae.14416
Chooi C, Cox JJ, Lumb RS, Middleton P, Chemali M, Emmett RS, Simmons SW, Cyna AM, Cochrane Pregnancy and Childbirth Group (2017) Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. 8:CD002251. https://doi.org/10.1002/14651858.CD002251.pub3
Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N (2014) Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev 2014(6):CD003843
FitzGerald H, Anderson E, Anderson LR, Tracy AJ, Thomson JS (2019) Effectiveness of deep general anesthesia compared to the standard depth of general anesthesia for acute postoperative pain and patient safety: a systematic review protocol. JBI Database System Rev Implement Rep. 17(10):2129–2135. https://doi.org/10.11124/JBISRIR-2018-004040
Pavenski K, Stanworth S, Fung M, Wood EM, Pink J, Murphy MF et al (2018) Quality of evidence-based guidelines for transfusion of red blood cells and plasma: a systematic review. Transfus Med Rev S0887-7963(18):30017–30018
Fayad A, Shillcutt SK (2018) Perioperative transesophageal echocardiography for non-cardiac surgery. Can J Anaesth. 65(4):381–398. https://doi.org/10.1007/s12630-017-1017-7
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB et al (2018) 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 72(14):e91–e220. https://doi.org/10.1016/j.jacc.2017.10.054
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC et al (2019) 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 140(2):e125–e151. https://doi.org/10.1161/CIR.0000000000000665
Abbas H, Senthil Kumaran S, Zain MA, Ahmad A, Ali Z (2019) Transient systolic anterior motion of the anterior mitral valve leaflet in a critical care patient with a structurally normal heart. Cureus. 11:e3963. https://doi.org/10.7759/cureus.3963
Reddy S, Ueda K (2014) Unexpected refractory intra-operative hypotension during non-cardiac surgery: diagnosis and management guided by trans-oesophageal echocardiography. Indian J Anaesth. 58(1):51–54. https://doi.org/10.4103/0019-5049.126796
Roberts DJ, Leigh-Smith S, Faris PD, Blackmore C, Ball CG, Robertson HL, Dixon E, James MT, Kirkpatrick AW, Kortbeek JB, Stelfox HT (2015) Clinical presentation of patients with tension pneumothorax: a systematic review. Ann Surg. 261(6):1068–1078. https://doi.org/10.1097/SLA.0000000000001073
Kearns MJ, Walley KR (2018) Tamponade: hemodynamic and echocardiographic diagnosis. Chest. 153(5):1266–1275. https://doi.org/10.1016/j.chest.2017.11.003
Konstantinides SV, Meyer G, Bueno H, Galié N, Gibbs JSR, Ageno W et al (2020) 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (ERS). European Heart Journal. 41(4):543–603. https://doi.org/10.1093/eurheartj/ehz405
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C et al (2021) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85116221831&doi=10.1007%2fs00134-021-06506-y&partnerID=40&md5=abbc038a2b6b3d57810b312d8d21e566
Hamada SR, Gauss T, Pann J, Dünser M, Leone M, Duranteau J (2015) European trauma guideline compliance assessment: the ETRAUSS study. Crit Care. 19(1):423. https://doi.org/10.1186/s13054-015-1092-5
Hatib F, Jian Z, Buddi S, Lee C, Settels J, Sibert K, Rinehart J, Cannesson M (2018) Machine-learning Algorithm to Predict Hypotension Based on High-fidelity Arterial Pressure Waveform Analysis. Anesthesiology. 129(4):663–674. https://doi.org/10.1097/ALN.0000000000002300
Wijnberge M, Geerts BF, Hol L, Lemmers N, Mulder MP, Berge P, Schenk J, Terwindt LE, Hollmann MW, Vlaar AP, Veelo DP (2020) Effect of a machine learning-derived early warning system for intraoperative hypotension vs standard care on depth and duration of intraoperative hypotension during elective noncardiac surgery: the HYPE randomized clinical trial. JAMA. 323(11):1052–1060. https://doi.org/10.1001/jama.2020.0592
Angus DC (2020) Randomized clinical trials of artificial intelligence. JAMA. 323(11):1043–1045. https://doi.org/10.1001/jama.2020.1039
Acknowledgements
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
FG designed and wrote the manuscript. PB performed the literature search and substantially contributed to writing the manuscript. All authors read and approved the final manuscript
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
FG received honorarium from Edwards in 2019. PB has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guarracino, F., Bertini, P. Perioperative hypotension: causes and remedies. J Anesth Analg Crit Care 2, 17 (2022). https://doi.org/10.1186/s44158-022-00045-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44158-022-00045-8