Abstract
Mobile health (mHealth) systems are sipping into more and more healthcare functions with self-management being the foremost modus operandi. However, there has been challenges. This study explores challenges with mHealth self-management of diabetes and hypertension, two of the most comorbid chronic diseases. Existing literature present the challenges in fragments, certain subsets of the challenges at a time. Nevertheless, feedback from patient/users in extant literature depict very variegated concerns that are also interdependent. This work pursues provision of an encyclopedic, but not redundant, view of the challenges with mHealth systems for self-management of diabetes and hypertension.
Furthermore, the work identifies machine learning (ML) and self-management approaches as potential drivers of potency of diabetes and hypertension mobile health systems. The nexus between ML and diabetes and hypertension mHealth systems was found to be under-explored. For ML contributions to management of diabetes, we found that machine learning has been applied most to diabetes prediction followed by diagnosis, with therapy in distant third. For diabetes therapy research, only physical and dietary therapy were emphasized in reviewed literature. The four most considered performance metrics were accuracy, ROC-AUC, sensitivity, and specificity. Random forest was the best performing algorithm across all metrics, for all purposes covered in the literature. For hypertension, in descending order, hypertension prediction, prediction of risk factors, and prediction of prehypertension were most considered areas of hypertension management witnessing application of machine learning. SVM averaged best ML algorithm in accuracy and sensitivity, while random forest averaged best performing in specificity and ROC-AUC.
Similar content being viewed by others
Introduction
The number of people needing healthcare and number of caregivers are growing disproportionately, with the later lagging. It is not just because of world population increase, but as observed by Anderson et al. [1], healthcare-consumers are living longer. As mobile phone technology has become indispensable, the number of users has increased substantially on a yearly basis; researchers and medical practitioners are taking advantage of the abilities of mobile phone technology for the interest of the medical sector. Though many years have passed and there has been respectable advancements in mobile system intervention in health, mobile health care is still considered a developing sector in health telematics [2, 3] yet to attain its projected heights [4].
Mobile health care is the use of mobile phones technology to facilitate health care demands, thereby making it easily available and cost effective [5]. Mobile wireless technology has the capability to innovate the manner in which people interconnect with the public health services [6]. With it, health records can be shared remotely between healthcare workers and medical specialist for discourse with the purpose of reducing time and cost for patients and health specialists and effectively administering treatment for people with long-term illness [7]. Diabetes mellitus and hypertension are two comorbid chronic diseases with rising prevalence globally, which will be considered in this work.
Overview of diabetes mHealth system
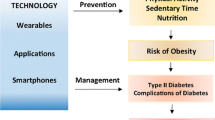
Significant improvements have been apparent in diabetes technologies (DTs), which have aided accessible, customizable, and personalized caregiving. One way of supporting patients in self-care and self-management is through the use of technology [8]. Examples of DTs include continuous subcutaneous insulin infusion (CSII), continuous glucose monitoring (CGM), or an amalgamation of both devices called automated insulin delivery (AID) [9]. Both CSII and CGM devices have proven useful in glycemic control in both ambulatory and hospitalized diabetic patients [10]. Further example of diabetes technology is a health software deployed on handheld devices, which has presented an improved approach to management of diabetes. Figure 1 presents the typical components of an mHealth system for diabetes (both human and gadgets) and how they work together. As shown in Fig. 1, such apps feature the following: blood glucose level (BGL) tracking, insulin usage tracking and dosage calibration, diet and physical activities monitoring, and measuring and keeping track of body weight, as well as access to educational information. The use of mobile health helped improve HbA1c levels in certain cross-section of patients with type 1 diabetes mellitus [11].
These data collected via manual user-input or via sensor nodes (e.g., smart blood glucose monitor) are sent to cloud-based health databases through cellular networks. From cloud computing services or medical centers, the data are collected for further analysis [12]. To foster key contextualization of these data, they are integrated with other clinical data sources like prescription registries, clinical registries, electronic health records, and laboratory-collected biomarkers [13].
Overview of hypertension mHealth system
Hypertension is when blood pressure is very high, blood pressure as the pressure applied by the flow of blood against the walls of the body’s arteries [14]. Hypertension mHealth is also a subsidiary of hypertension telehealth setup. They differ only in some of the vital signs measured in the course of management of hypertension. The technologies available for management of hypertension are similar to those for diabetes. Smartphones and Bluetooth® enabled telemonitoring are new tools that are of increasing importance in hypertension management [15]. Figure 1 presents the typical components of an mHealth system for hypertension (both human and gadgets) and how they work together. As shown in Fig. 2, data like blood pressure, heart rate, rest, and sleep measurements are taken via sensor nodes or manually keyed into the hypertension mHealth app. Wearable devices such as watches can monitor BP with the use of electrocardiography (ECG) and photoplethysmography (PPG) signals. Data from these devices are sent to central servers for centralized access to all data through the internet. In the hypertension management system framework designed in [16], the data is then compressed and reduced to extract features and patterns. Extraction of the features is based on specified symptoms and directions. Some machine learning models can then applied to the extracted features to provide clues for diagnosis and treatment.
So, mobile health intervention has found footing in management of diabetes and hypertension, with lofty projected outcomes. Intriguingly, these projected benefits of mHealth to diabetes and hypertension, and a number of smartphone users have not necessarily translated to established advantages. Some literature have discussed these impediments to a great individual detail though in fragments, i.e., a few of them per literature. There has been shortage of literature that collate all the possible challenges in a single document. Feedback from users have been many of extensive kinds [17], which means having an exhaustive discussion on just a few of these challenges does not solve the varied nature of these concerns. A further outcome is the paucity of full-flavored mHealth systems equipped to handle the varied needs of users.
Though this work reviews the challenges from the perspectives of stakeholders (app developers, healthcare givers, and health system regulators and users), they are presented mainly as they affect the users/patients. We believe the ultimate is for users to attest to improvements post-intervention of any mHealth system adopted. With this work, extracting system requirements for development of diabetes and hypertension mobile health apps should be more efficient. The long-observed comorbidity of diabetes and hypertension inspired the combined review of mHealth systems for self-management of both chronic diseases in this work. As far back as 2010, a study in Hong Kong revealed that just 42% of diabetic patients had normal blood pressure and only 56% of hypertensive patients had normal glucose tolerance [18]. High blood pressure, or hypertension, often occurs alongside diabetes and obesity [19, 20]. So, to enrich our expose of challenges to mHealth use for management of diabetes and hypertension, we review mHealth apps for diabetes and hypertension. To understand what these apps should offer, first, we describe the various approaches to cost-effective management of diabetes and hypertension. Our concern in these approaches were mainly self-management approaches, which can be supported by mobile apps. For this reason, we focus on non-pharmacological and non-surgical approaches to management of diabetes and hypertension. This is what the “Approaches to management of hypertension and diabetes” section discusses. Next, in the “Machine learning in management of diabetes: review” and “Machine learning in management of hypertension: review” sections, we present AI (specifically, machine learning) interventions to management of diabetes and hypertension. In establishing this nexus between aforementioned mHealth, approaches to the management of the two co-morbid diseases and machine learning, we explore extant literature on machine learning as applied to the management of diabetes and hypertension to reveal the focus spread of machine learning (ML) research on the identified approaches to the management of diabetes and the extent of incorporation of machine learning into mHealth systems. In the “User expectation” section, we present user expectations from diabetes and hypertension mHealth systems, while in the “Review of Existing mHealth solutions” section, features of existing mHealth systems for diabetes and hypertension are reviewed. Finally, the “General challenges” section presents general challenges faced with diabetes and hypertension mHealth systems.
Approaches to management of hypertension and diabetes
While diabetes mellitus and hypertension cannot be cured, they can be managed both physically and psychologically. Non-pharmacological interventions aid in reducing the daily dosage needed for antihypertensive medication and interrupt or slow down prehypertension deteriorating to hypertension [21]. Raveendran et al. [22] list non-pharmacological methods to include bariatric surgery, medical nutrition interventions, and change of lifestyles. Besides nutrition, lifestyle changes include exercise, avoiding stress, and lowering alcohol consumption [21]. However, surgery as non-pharmacological approach is extrinsic to self-management of diabetes and hypertension and therefore not discussed in this work. Focus is on non-surgical non-pharmacological ways of managing diabetes and hypertension: dietary intervention, physical activity, sleep, and rest. The justification for inclusion of self-management approaches in this review of MobileHealth systems in management of diabetes and hypertension is that MobileHealth systems for such ailments are mostly geared towards self-care or self-management. It makes it pertinent to present an overview of such self-management approaches as later in this paper they help us understand and classify existing works on diabetes and hypertension management.
Dietary intervention
Dieting entails taking healthy diet while desisting from taking unwholesome foods and health-damaging substances [23]. Maladjusted eating attitude and eating disorders are serious conditions in type 1 diabetes mellitus, yet under-explored [9]. Because medication can have after effect or can be disastrous due its abuse and patient’s internal body reaction to the medication, there is need to incorporate diet to the system [24]. Making a difference in a way of living such as eating wholesome meals, addition of adequate physical activities, and termination of smoking aids in obtaining an ideal blood pressure level [25]. Despite the fact that management of diet is greatly commendable as regards hypertensive patients, there is little knowledge with respect to the patients’ diet control and how the set out rules are being followed [26].
Though high blood pressure and diabetes can be managed and controlled through a healthy diet, compliance to the diet prescription is an issue. Factors that illicit non-adherence are non-availability and cost of food prescribed, low level of education, age, flexibility of diet, and recommendation incomprehensible [27,28,29]. Low level of education can affect compliance by 70%, and older adult between the age bracket of 60 and 79 years are less likely to comply to recommendation [27]. Furthermore, based on interview conducted in [29], 39% of the respondents were unable to comply to diet prescription due to the rigidity of the diet. The same study also suggests that rather than persisting on stringent diet, the diet should focus on patients predilection. Diet management works best with physical activity (PA).
Physical activities
Diabetes and hypertension are under the aegis of metabolic syndrome (MetS) [19]. Obesity and physical inactivity are the popularly known cause for diabetes and hypertension [14, 30]. Engaging in physical activity daily lowers the possibilities of having diabetes and hypertension [31, 32]. All types of movement are termed physical activity, and these include sports, walking, cycling, and wheeling [33]. For diabetic patients, physical activity aims at improving cardiorespiratory fitness, enhanced vigor, improving glycemic control, reducing insulin resistance, enhancing lipid profile, reducing blood pressure (BP) level, and maintaining ideal body weight [34, 35]. In a case of hypertension, physical activity is encouraged due to its ability to reduce blood pressure by enhancing cardiorespiratory fitness (CRF) [36]. High level of physical activity can reduce blood pressure level by the rate of reductions ranging from 5 to 17 mm Hg for systolic BP and 2 to 10 mm Hg for diastolic BP. Physical activity is also proven to be very effective in avoiding incident hypertension for adult with pre-hypertensive and normal blood pressure level [37]. Apart from the benefits of physical activity in management of diabetes and hypertension, fitness apps were found in [38] to be most preferred mHealth app, with the attendant advantage of longest periods of long-term use by patients.
Sleep and restfulness
It is not only the activity that is impactful, rest and sleep (elements of inactivity) are too. Of all the lifestyle recommendations in [39]—sleep, restfulness, activity, heart rate, and diet—sleep-related recommendations were the highest in number. Restfulness was third highest. Many reviews have surmised sleep as a contributor to glycemic control, diabetes management, and diabetes-linked complications in type 1 diabetes mellitus (T1DM) patients [40]. However, sleep has not been significantly explored as an opportunity for management of diabetes [40] and hypertension. Blood pressure (BP) dips during sleep. This explains why sleep disorders, especially obstructive sleep apnea (OSA) [41] and insomnia [42], have positive relationship with hypertension because they interrupt BP dipping. The association of restfulness from sleep with cardiovascular disease (CVD) events was pronounced in subjects with younger age and female sex [43]. Evidence is sparse on which patient phenotypes of CVD patients can benefit the most in terms of BP reduction and positive impacts of insomnia and restless leg syndrome (RLS) therapy on BP [41].
Artificial intelligence in the management of diabetes and hypertension
The technology in artificial intelligence (AI) permits the analysis of real-time empirical data and constant training to improve comprehension [44]. In health sector, AI methods are used in studying patient’s data and foretelling upcoming incidence and creating smart interface for communication with the patient improvement in his/her commitment with the treatment plan [45]. Diabetes and hypertension being chronic in nature and requiring frequent checks/tests has resulted in the production of high volume of medical data from wearable technology, for instance, that track data from patient physical activity via Bluetooth, as in Alazzam et al.’s design [46]. To collate, store, and learn data pattern [47] and predict patient health require artificial intelligence, say, machine learning [48]. This has brought on the development of blood pressure telemonitoring (BPT) for remote BP tracking. Blended with machine learning models, efficiency of BPT solutions is better tuned as viable tool to caregivers [49]. The non-pharmacological approaches in management of diabetes and hypertension discussed in the previous section have also benefited from AI. In [50], machine learning was used in increasing physical activity in diabetes mHealth system and in recommendations for sleep and restfulness in [39]. Our focus is on machine learning algorithms applied to management of diabetes and hypertension are reviewed in this section, with the specific management approach each algorithm has been used for. Deep learning was not considered because it generally requires high computational power and has the behavior of a black-box approach, which discourages application in a medical context [51].
Machine learning in management of diabetes: review
Machine learning is a trending area where computational algorithms are created to imitate human intelligence through learning [52]. Machine learning makes it easier in identifying chronic diseases, as opposed to the manual ways of diagnosing chronic disease which are frantic, time-consuming, and error-prone [53]. Furthermore, machine learning can be used to effectively prescribe diet for diabetic patients. It can also help in predicting if a person will be diabetic or hypertensive from the data provided. In [50], a text-message-based mobile app, “DIAMANTE,” built by Audacious Software is studied. This application tracks step counts by pooling from Google Fit, Apple HealthKit, or the built-in pedometer on patients’ phones. The app determines motivational messages to display to user based on step-count per day. The reinforced machine learning algorithm in the app assesses which motivational message and which time period of the day (in intervals of two and a half hours) is predicted to maximize the number of steps walked the next day. The app also assesses engagement measures; machine learning was used to measure times that the app was opened and time spent reading. Summarily, the areas of diabetes research that have had application of machine learning are prediction, diagnosis, etiopathophysiology, and therapy [54].
There have been survey works on ML applied to diabetes research. The work in [54] presents extensive survey of papers on ML and data mining methods in diabetes research. Of the various aspects of diabetes research, machine learning application to prediction and diagnosis has been the most prominent with support vector machines (SVM) being the most successful and most used ML algorithm [54]. However, information was not provided as to the distribution of the ML algorithms over the various areas of diabetes research. Also, performance of the algorithms was not presented. The review in [55] evaluated machine learning algorithms previously applied to the prediction of type 2 diabetes mellitus (T2DM) using three diabetes datasets in a unified setup and compared their performance in terms of accuracy, measure of a test’s accuracy (F-measure), and execution time, with bagging-LR being the most accurate for a balanced dataset, and random forest (RF) is the most accurate for imbalanced dataset (bagging-LR meaning logistic regression (LR) improved by bagging, an ensemble learning technique that helps to improve the performance and accuracy of machine learning algorithms). Prediction is just one of the research areas for management of diabetes. Also, whether accuracy, F-measure, and execution time or any other combination of performance metrics are the most considered/impacting remains to be seen.
Therefore, in this review, the key research contributions in this review of machine learning application to diabetes management are to:
-
Show where emphasis have been on, be it on prediction, diagnosis, etiopathophysiology, or therapy aspect of diabetes research
-
Show how much of machine learning (ML-based) treatment of diabetes has interfaced with mHealth systems
-
Show most considered and impacting ML algorithms and their performances
A total of 20 journal papers covering 2015 to 2022 were reviewed: 9 from SpringerLink, 9 from ScienceDirect, and 2 from other sources.
Review findings (ML in diabetes management)
-
1.
Application of ML to diabetes self-management approaches: Four purposes of machine learning application to diabetes research were observed: therapy, prediction (P), and diagnosis (D), the extra purpose being measurement of blood glucose level (BGL). In the area of therapy, dietary therapy (TD), physical therapy (TP), and rest therapy (TR) were considered. As extracted from Table 1 and summarized in Fig. 3, prediction of diabetes had the most application of machine learning at 52%, while ML application to diagnosis of diabetes stood at 21%.
This confirms the observation made in [54] that diabetes prediction and diagnosis has had the most focus of ML algorithms, with it tilting more to diabetes prediction [56]. Half of the times diagnosis was considered, early diagnosis, P(Early), was of interest. Observe that some literatures in Table 1 considered more than one purpose, like [46] and [57]. For instance, in [57], LR, RF, and MLP were used for diagnosis, while LR, RF, and LSTM were used for prediction. Further in our review, therapy was considered for only 14% of the literature, specifically dietary (5%) and physical therapies (9%). Rest therapy was not applied in any of the reviewed literature. Blood glucose level (BGL) monitoring/measurement was the purpose of application of ML to diabetes research in 13% of the reviewed literature, nearly equally focus of ML on all forms of non-pharmacological and non-surgical therapies highlighted in this work. These findings are explained in greater detail as follows:
-
(a)
Identification of patient physical activity: In [46], support vector machine (SVM) and decision tree machine learning models were used to identify two tasks: sitting and standing. Both models were 86% accurate for those tasks. The researchers were positive that it could become a standard mechanism for diabetes management depending on the results of a pilot study with real patients.
Investigation of status of falls and identification of key risk factors for fall in T2DM patients was done in [58] using logistic regression and random forest classifiers. Logistic regression showed that fasting C-peptide level, dorsiflexion, and knee extension strength were autonomous predictors of falls. The random forest classifier placed grip strength among the top 5 key variables for falls.
-
(b)
Identification of predisposition to diabetes: Using logistic regression (LR) and gradient boost (GB), a predictive model with respectable sensitivity and selectivity was built in [59]. Using patient demographic data (of Canadians) and results from laboratory tests, the work identified patients at risk of having diabetes mellitus. The area under the receiver operating characteristic curve (AUC-ROC) was used to evaluate the discriminatory capability of these models. The AUC-ROC for the proposed logistic regression model was 84.0%, and it was 84.7% for the proposed GB model. For sensitivity, logistic regression performed at 73.4%, and it was 71.6% for the proposed GB model. Age, high-density lipoprotein, fasting blood glucose, triglycerides, and body mass index were the prime predictors in logistic regression model. In [60], logistic regression (LR) model demonstrated that 7 factors (education, age, BMI, direct cholesterol, systolic BP, diastolic BP, and total cholesterol) out of 14 are diabetes risk factors. The overall accuracy of this ML-based system was 90.62%. The combination of LR-based feature selection and random forest (RF)-based classifier gave 94.25% accuracy for K10 partition protocol.
The study in [61] evaluated the performance of Adaptive Boost (AdaBoost) and bagging data mining ensemble techniques using J48 (c4.5) decision tree as a base learner along with standalone data mining technique J48 (c4.5). The work achieved accurate classification of patients with diabetes mellitus using diabetes risk factors with consideration for three adult groups in Canadian Primary Care Sentinel Surveillance Network (CPCSSN) database, viz., below middle-aged adults, middle-aged adults, and adults older than 55 years. The work identified AdaBoost ensemble method to outperform bagging and standalone J48 decision tree in accurate identification of diabetes patients.
-
(iii)
Diagnosis of diabetes: The GB and logistic regression models in [59] may have performed better than the random forest and decision tree models for identification of people at risk of having diabetes, but for early diagnosis of diabetes, random forest (RF) model, with accuracy (ACC) of 99.35%, holds more significant promise than GB model (93.51%) and more so AdaBoost (88.31%) and SVM (85.06%) [62]. Also, sensitivity (SEN) and specificity (SP) were metrics in which RF (99.01% and 100%) outperformed GB (97.06% and 98.08%), AdaBoost (94.51% and 87.77%), and SVM (89.72% and 91.49%), respectively. In [63], diabetes and prediabetes were predicted using artificial neural networks (ANNs), logistic regression, and decision tree models. Participants were drawn from two localities in Guangzhou, China. Recruited were 735 diabetes or prediabetes patients and 752 normal controls. With the use of questionnaire, information on family diabetes history, demographic characteristics, lifestyle risk factors, and anthropometric measurements was obtained. In the order of accuracy, sensitivity, and specificity, the models performed thus as follows: LR 76.13%, 79.59%, and 72.74%; ANN 73.23%, 82.18%, and 64.49%; and the decision tree (C5.0) 77.87%, 80.68%, and 75.13%. The best classification accuracy and specificity were achieved by decision tree (C5.0).
Four models (SVM, KNN, DT, RF) were compared for prediction of diabetes mellitus in [64] using 8 important attributes of Indian patients: triceps skin fold thickness, number of times pregnant, plasma glucose concentration, diabetes pedigree function DBP, 2-hour serum insulin, body mass index (BMI), and age. In terms of accuracy, sensitivity, and specificity, random forest algorithm, with all 100% score, outperformed SVM, K-nearest neighbor (KNN), and decision tree (J48). In the order of accuracy, sensitivity, and specificity (in %), SVM had 77.73, 51.37, and 71.09, KNN (k = 3) had 85.68, 79.47, and 89, and decision tree (J48) had 86.46, 86.56, and 86.4. A similar work was done in [65], considering same attributes and similar classifiers (LR with SVM, KNN, and decision tree (J48)), except random forest. Similar results were got as decision tree (J48) had higher accuracy than the rest, with bootstrapping (78.43%) and without bootstrapping (94.4%). KNN (k = 3) had second highest accuracy without bootstrapping (72.2%), but with bootstrapping, KNN (k = 1) had second highest accuracy (93.79%). The Pima Indian Diabetes Database (PIDD) was used. With accuracy of 81.97%, sensitivity of 91.79%, and specificity of 63.33%, Gaussian process (GP)-based classification technique performed better than linear discriminant analysis (LDA), naive Bayes (NB), and quadratic discriminant analysis (QDA) [66].
-
(iv)
Detection of inaccurate diabetes data: Decision tree machine learning algorithm was used in detection of sources of inaccurate data and delivery of quality information. The algorithm was able to classify the diabetes data as accurate or inaccurate [67].
While ML has had respectable use in physical health, chronic disease management, and remote patient monitoring, the same cannot be said about its use in chronic disease detection. In [56], a paltry 24% of the journals reviewed discussed ML models for diabetes detection. The 24% is also shared by cardiovascular and respiratory conditions. Machine learning has been applied to good results in guaranteeing data accuracy and information integrity in diabetes mHealth.
-
2.
Incorporation of ML into diabetes MobileHealth systems: The last two columns on Table 1 are for dataset source and answer to whether or not the ML models were incorporated into a diabetes mHealth system (DMS). Only 25% of the reviewed works had any form of integration into an mHealth system either in form of mHealth app [46] or an IoT devices/sensors [57, 68,69,70]. The use of IoT devices/sensors were primarily for collecting BGL data.
-
3.
Performances of ML algorithms in diabetes research: As shown in columns 4 to 10 of Table 1, the machine learning algorithms used in the reviewed works were logistic regression (LR), linear discriminant analysis (LDA), Fisher’s discriminant analysis (FDA), quadratic discriminant analysis (QDA), decision tree (DT), gradient boost (GB), random forest (RF), long short-term memory (LSTM), support vector machine (SVM), K-nearest neighbor (KNN), naïve Bayes (NB), artificial neural network (ANN), deep neural network (DNN), extreme gradient boost (XGB), AdaBoost (AB), multilayer perceptron (MLP), moving average (MA), bagging, regression tree (bagged CART), and Gaussian process-based classification (GPC). Performance metrics observed in the literature include accuracy (ACC), sensitivity (SEN), specificity (SP), precision (PR), area under curve (ROC-AUC), F-measure (F), and negative predictive value (NPV). There were others like miscalculation rate, kappa, MCC, false discovery rate (FDR), false negative rate (FNR), false positive rate (FPR), and detection rate. They were not captured in the table (Table 1) for want of space and the fact that none occurred more than twice in the reviewed literature.
The best performing ML algorithm under each performance metric is stated with the percentage level within braces, e.g., LDA predicted diabetes most accurately in [58] at 67%. Where the ML algorithm is not stated in the cell, it means all algorithms used shared that maximum value, e.g., in [71], all the ML algorithms used in the work had NPV score of 99.9%. The four (4) most considered performance metrics were accuracy (90%), ROC-AUC (55%), sensitivity (50%), and specificity (45%). This supports the use of accuracy and ROC-AUC metrics, for instance, in [72], in deciding best model for diabetes prediction. Out of the three performance metrics considered in [55], only accuracy was confirmed to be among most considered. Our review places random forest (RF) algorithm as best performing in accuracy (40% of the time), ROC-AUC (30%), sensitivity (20%), and specificity (10%). For context, this was not because of a superior frequency of deployment of RF, as number of times of use of random forest (13) was not necessarily the highest logistic regression had fourteen (14) occurrences. Contrary to SVM being most prominent ML algorithm in [54], random forest was the best performing algorithm across all metrics, for all purposes covered in the literature. Tree-based algorithms were also found in [72] to be best performing, specifically random forest algorithm. The observation of DNN’s sub-par performance in [72] could neither be confirmed nor refuted in our review. There was not enough data on this as DNN happen to be used only once in all the literature we reviewed. Though in that one time, it outperformed RF and XGB in F-measure and AOC-AUC metrics.
-
4.
Diabetes dataset: The dataset used in [71] was sourced from CONSTANCES linked with French Administrative Healthcare Database (SNDS). Other sources were National Health and Nutritional Examination Survey (NHANES), Tehran Lipid and Glucose Study (TLGS), Health Management Information System (HMIS) in Kano, Intelligent Glucose (iGLU), Pima Indians Diabetes Database (PIDD), UCI Machine Learning Database, Continuous Glucose Monitoring (CGM), Internet of Things (IoT) sensor, Canadian Primary Care Sentinel Surveillance Network (CPCSSN), and Bangladesh: Demographic and Health Survey (DHS).
Machine learning in management of hypertension: review
The key research contributions in our review of machine learning application to hypertension management are to:
-
Show the aspects of research on hypertension prediction using machine learning; and the distribution of emphases.
-
Show how much of machine learning (ML-based) treatment of hypertension has interfaced with mHealth systems
-
Show most considered and impacting ML algorithms and their performances
There have been two approaches in application of machine learning techniques in researches on high blood pressure: hypertension detection and blood pressure monitoring. The former is classification problem based on clinical data, while the latter is handled as a regression task [79]. Martinez-Rios et al. [79] reviewed works applying machine learning algorithms for classification of hypertension patients and regression algorithms used for blood pressure estimation. Also of interest was integration of machine learning into mHealth systems for management of hypertension. To identify existing works on this, we did search of various combinations of the terms referring to “machine learning,” “neural network,” “deep learning,” “detection,” “diagnosis/prognosis,” “mHealth,” “hypertension,” “high blood pressure” on PubMed and Google scholar. As eligibility criteria, only original researches written in English were included in this review. Excluded were studies involving pregnant women and patients just undergone surgical procedure. Articles on prediction of hypertension in persons below 18 were excluded. Study selection was done in two steps: in the first step, titles and abstracts were screened according to the eligibility criteria. Full-text of articles selected from step 1 were further checked for eligibility. A total of ten works were on the final shortlist.
From available studies, the two major areas of ML application to management of hypertension were identified to be detection and blood pressure estimation based on physiological variables. The former is mainly on classification models for hypertension detection, while the latter is mainly a regression problem. Literature reviewed covered both genres, estimating blood pressure values from other signals to drive use of noninvasive and continuous measurements [79]. Most common signals for generation of predictors are electrocardiography (ECG) and photoplethysmography (PPG). While home BP monitoring based on cuffs offers instantaneous readings, ambulatory blood pressure monitoring (ABPM), though more expensive, provides automatic BP reading over extended periods of time, at intervals [80].
Review of existing literature on machine learning in hypertension management
In [81], for the first time, a multi-verse optimization (MVO) algorithm is integrated with TQWT for selecting optimum tuning parameters to decompose the input BCG signals into more representative SBs. To detect hypertensive BCG signals, eleven statistical features are evaluated from each SB. Among them, a set of seven statistically significant features are selected by applying the Kruskal–Wallis test and fed to a K-nearest neighbor (K-NN) classifier with six different kernels using a 10-fold validation scheme. The highest classification accuracy of 92.21%, sensitivity of 92.96%, and specificity of 91.60% are achieved using a weighted K-NN classifier. The work in [81] presents a non-parameterized approach for the optimal decomposition of BCG data to detect HPT more accurately. The primary benefit of the proposed support system is that it can detect HPT patients with high accuracy by reducing the clinician’s workload.
In [51], wavelet scattering transform (WST) as a feature extraction technique was used to obtain features from PPG data and combined with clinical data to detect early hypertension stages by applying early and late fusion. PPG features extracted from the wavelet scattering transform in combination with a support vector machine can classify normotension (NT) with SBP < 120 mm Hg and DBP < 80 mm Hg and prehypertension (PHT) with SBP ranging from 120 to 139 mm Hg and/or DBP 80 to 89 mm Hg, with an accuracy of 71.42% and an F1-score of 76%. Interestingly, classifying normotension and prehypertension using the features extracted from PPG signals via wavelet scattering transform and physiological variables such as BMI, age, and heart rate presented no improved performance in accuracy and F1-score. In [82], five ML algorithms were applied to echocardiographic pulmonary hypertension (PH) prediction, viz., random forest of classification trees (RFc), lasso penalized logistic regression, random forest of regression trees (RFr), boosted classification trees, and SVM. Cross-validation (CV) scheme used was using a 10 times 3-fold. AUC achieved by the machine learning algorithms include random forest of regression trees at 87%, support vector machines at 83%, lasso penalized logistic regression at 78%, boosted classification trees at 80%, and random forest of classification trees at 85%. Parameters used were echocardiographic (Echo) parameters. Model training and testing in [83] used a dataset of 29,700 samples acquired via physical examination. The objective was to identify easy-to-get risk factors of hypertension, using univariate logistic regression analysis. The work utilized 10-fold cross-validation to optimize four models: CatBoost, RF, MLP, and LR. RF model performed best across metrics considered, viz., accuracy of 0.82, AUC of 0.92, specificity of 0.81, and sensitivity of 0.83. The primary risk factors identified were family history, BMI, waist circumference, and age, while in [84], age, wealth index, BMI, marital status, and working status were the primary risk factors when least absolute shrinkage operator (LASSO) was used as risk identification method. Furthermore, age, marital status, BMI, diabetes, and region were the primary risk for hypertension when support vector machine recursive feature elimination (SVMRFE) was used. Each of LASSO and SVMRFE was combined with ANN, DT, RF, and GB, with the combination SVMRFE-GB providing best accuracy at 66.98%, recall at 97.92%, F-measure at 78.99%, and AUC at 0.669 compared to others. The hypertension data in [84] was extracted from a demographic and health survey done in Bangladesh between 2017 and 2018, which included 6965 people between of ages of 35 and above. Alkaabi et al. [85] identified age, history of high cholesterol, history of diabetes, education, employment, physical activity, waist circumference, tobacco use, gender, employment, education level, physical activity, mother’s history of high blood pressure, sex, and adequate intake of fruits and vegetables as principal predictors of hypertension, in descending order. The data was drawn from Qatar biobank, having 987 records of residents 18 years and above.
In [86], gradient boost, regression partition trees (Rpart), RF, and Ensemble were the machine learning models used in prediction pulmonary artery hypertension (PAH). It was specifically aimed at identification of the diagnostic biomarkers in order to achieve early diagnosis of patients at risk of PAH. Plasma from sixty-four native patients with pulmonary artery hypertension (PAH) and 43 healthy controls were profiled for microRNA. Two (miR636 and miR-187-5p) out of the 20 microRNAs considered were picked by all feature selection methods adopted in the work, as they could predict PAH with high performance: best accuracy was achieved with XGB (83%), precision of 83% with both RF and XGB, and ROC-AUC of 84% with RF.
In [87], ML was used for detection of hypertension using population-based surveys. Dataset used was secured by integrating data from health and demographic survey in India, Bangladesh, and Nepal. The variables in the dataset were hemoglobin, blood pressure, sociodemographic and economic factors, weight, height, and random blood glucose. Six commonly used ML-based classifiers used were as follows: linear discriminant analysis (LDA), decision tree (DT), gradient boosting machine (GBM), random forest (RF), extreme gradient boosting (XGBoost), and logistic regression (LR) to predict hypertension and its risk factors. There were 818,603 participants, out of which 82,748 (10.11%) had hypertension. Age and BMI were identified as prime risk factors for hypertension. In a lower order of significance were BP, taking medicine to reduce blood pressure, education, and doctor’s understanding of high blood pressure. LDA, GBM, XGBoost, and LR demonstrated highest accuracy at 90%. Apart from decision tree (DT) which achieved precision value of 91%, other algorithms performed with 90% precision. LDA, GBM, XGBoost, and LR achieved highest recall value at 100%. In F1-score, LDA, GBM, XGBoost, and LR scored 95%. All the algorithms had log loss values below 6%.
Sakr et al. [88] used LogitBoost (LB), artificial neural network (ANN), Bayesian network classifier (BN), support vector machine (SVM), locally weighted naive Bayes (LWB), and random tree forest (RTF) in predicting the individuals at risk of developing hypertension, using data from cardiorespiratory fitness. Dataset used comprised of treadmill stress testing undergone by 23,095 patients. The data was collected between 1991 and 2009. The variables captured in the dataset include data on diagnosis, vital signs, and clinical laboratory tests. Random forest performed best across all metrics considered: sensitivity (69.96%), specificity (91.71%), precision (81.69%), ROC-AUC (93%), and F-measure (86.70%).
Review findings (ML in hypertension management)
-
1.
Aspects of hypertension prediction using ML Table 2 presents a summary of the works reviewed on machine learning prediction of hypertension. There were three main categories of researches in this area: hypertension prediction (Hyp. Pred.) [76, 82, 83, 86, 88, 89], prediction of risk factors [84, 85, 87], and prediction of prehypertension (PHT) [51]. Hypertension prediction ranked highest in statistics Most recurring risk factors associated with hypertension were observed to be BMI and age. The three works that predicted hypertension risk factors [84, 85, 87] all recommended that biochemical markers be introduced so as to improve the ML algorithms and achieve real life evaluations.
-
2.
Performances of ML algorithms in hypertension research: The machine learning algorithms used in the reviewed works as shown in columns 5 to 11 of Table 2 were logistic regression (LR), regression partition trees (Rpart), linear discriminant analysis (LDA), decision tree (DT), support vector machine (SVM), random forest (RF), random forest of classification trees (RFc), random forest of regression trees (RFr), lasso penalized logistic regression (LLR), CatBoost, K-nearest neighbor (KNN), artificial neural network (ANN), naïve Bayes (NB), deep neural network (DNN), gradient boost (GB), extreme gradient boost (XGB), AdaBoost (AB), multilayer perceptron (MLP), moving average (MA), bagging, regression tree (bagged CART), long short-term memory (LSTM), and LogitBoost (LB). Performance metrics observed in the literature include accuracy (ACC), sensitivity (SEN), specificity (SP), precision (PR), area under curve (ROC-AUC), F-measure (F), and negative predictive value (NPV). In accuracy, SVM proved most accurate in 30% of the works in which accuracy was measured, random forest in 22%, and XGB in 20%. As regards sensitivity, SVM had highest sensitivity score in 40% of the works in which sensitivity was evaluated, followed by RF with 20%. As regards specificity performance metric, RF was most effective in 80% of the works in which specificity was considered. Random forest algorithm also had the best scores in 80% of the works in which ROC-AUC was evaluated. In Table 2, where a couple of machine learning algorithms were separated by forward slash, it means all the listed algorithms shared same score in the metric under consideration, e.g., in [87], XGB, GB, LR, and LDA all had same accuracy score of 90%. Also, for [87], under sensitivity, “=ACC” means sensitivity had same score for same algorithms written under accuracy.
-
3.
Incorporation of ML into diabetes MobileHealth systems: Regarding incorporation into an mHealth system, none of the works showed any link between the machine learning setup with an mHealth system.
-
4.
Hypertension datasets: The dataset sources were health management information system (HMIS), blood pressure estimation from photoplethysmogram (PPG-BP), demographic and health survey (survey), and Qatar Biobank (QBB).
C+S stands for clinical and sociodemographic data, PH for echocardiographic pulmonary hypertension, PAH for pulmonary artery hypertension, RHC for right heart catheterization, Echo for echocardiography, and QBB for Qatar Biobank.
User expectation
Before critiquing available mHealth systems, it is important to peek into what diabetes and hypertension patients expect from a given mHealth solution at the point of adoption. Of all the stakeholders in the mHealth ecosystem, users are the most crucial. mHealth app for diabetes and hypertension should focus on helping the patients/end-users manage their health without stress. mHealth app for diabetes and hypertension is expected to have the following features: health information, dietary recommendation, tracking of blood sugar levels, tracking of blood pressure level, exercise recommendation, notifications and alerts, security of personal and health information, insulin and medication, weight and BMI, reducing risk trend chart view, logbook view, and finally integration with other devices [91,92,93,94]. Furthermore, diabetic app for self-management of diabetes should also focus on providing an avenue for the users to easily learn by providing help/support features, removing actions that are prone to errors, offering improved graphics and screen views, and motivating patients and integration of basic heuristic design concept [95]. Though usability is important, if users are at home with the utility of the app, they can overlook some usability deficiencies. Both digital and clinical distress should be considered when diabetes apps are part of the healthcare ecosystem [96].
In a study on hypertensive disorders of pregnancy (HDP), respondents recommended interoperability (i.e., integration of mHealth data in EHRs and such data made available to caregivers) [97]. On the matter of information communication, users asked for clarity especially in informing users on moment and frequency of blood pressure measurement, as well as modesty in communication of expected benefits to forestall disappointment when those results are not attained.
Review of existing mHealth solutions
In this section, a review of existing mHealth apps for management and control of diabetes and hypertension is made. The mHealth systems reviewed in this work
-
All available free
-
Were chosen based on ratings on google play and app stores and recommendations by renowned health information outlets like Healthline, MedicalNews, and Verywell Health. Healthline, for instance, has an exclusive team managing an ample medical web of over 150 medical professionals availing expert point of views, medical reviews, and clinical guidance. Healthline’s medical professionals ensure that the information they release are correct, evidence-based, state-of-the-art, person-centric, and reliable [98].
To justify choice of cost-free apps for review, in [38], cost of mHealth apps was held by users as a critical driver of abandonment of mHealth apps. Furthermore, the risk of having hypertension, diabetes, and comorbidity were found to be remarkable in the unemployed demographic [99]. Comorbidity is considered the coexistence of both diabetes and hypertension. Some challenges with adoption and continued use of mHealth solutions for diabetes and hypertension are precipitated by low income of users or/and cost of the mHealth solution, e.g., prescription non-adherence [100, 101], and adoption and sustainability [102]. It is recommended in [102] that economic analyses of diabetes mHealth solutions should capture among others the cost of the mHealth solution to the patient. As recently as 2021, the World Health Organization (WHO) recommended the inclusion of sociodemographic dimensions of the hypertensive population (e.g., income) in order to achieve equity [103].
Functionalities of existing mHealth solutions for diabetes
In this subsection, functionalities of some mHealth solutions are explained. Explained first are ones for self-management of diabetes, viz.:
-
1.
Bluestar Diabetes: BlueStar provides a number of useful functions to users like scheduled medicine reminders, tracking of blood glucose levels, and daily meal scheduling. BlueStar accommodates both type 1 or type 2 diabetic patients [104].
-
2.
Glucose tracker and Diabetic diary: This app offers features like recording, labeling, and organization of tools to help the user create a thorough account of his/her journey.
It is meant for persons with type 1 or type 2 diabetes and also gestational diabetes. To keep record of the data that mostly concerns user, the user may add customized tags like “pre-bedtime” or “post-breakfast.” In addition, user can export his/her records to his/her healthcare provider [105].
-
3.
Fooducate: Fooducate is used in management of diabetes with the use of diet and physical activity. This app has over 300,000 foods in its database. Users can simply classify the food according to its safety by scanning its barcode, which in return will display an A, B, C, or D. If a meal could not be classified in those four tiers, users are given recommendations on a more wholesome meal. It also makes it easy for users to keep record of and learn more details about the food they eat, such as added sugar and secret ingredients [106].
-
4.
Glucose Buddy: The process of recording carbohydrate intake, medications, exercise, and blood glucose readings is made easier by Glucose Buddy’s user-friendly interface. Moreover, users can gain knowledge of how their lifestyle affects their diabetes management with the help of its custom awareness [107].
-
5.
My FitnessPal: MyFitnessPal does calorie counting. It also allows users to keep tabs on their water, sugar, and carbohydrate intake, as well as their physical activity and meal time. Users can also write down their blood sugar readings and insulin shots in the app’s notes section [108].
-
6.
Bezzy T2D: This app is mostly used for chats and communications, with secure forums where people can discuss topics like daily life, diet and nutrition, relationships, recently diagnosed conditions, mental health, and more. Feeling of being a part of community is useful, especially when it comes to health [109].
-
7.
MySugr: MySugr provides estimations for the bolus dosage calculation, glucose monitoring, and carbohydrate counting. It also provides reports on the users’ blood glucose levels over the course of weeks, months, or even years. In addition, depending on the users monitoring, it will estimate their hemoglobin A1C. This app stands out due to its clear, personalized dashboard interface, flexibility, ability to connect with users’ glucose meter, and notifications that prompt user to provide further data in the future (like blood sugar levels after a physical exercise). It also helps the user collaborate with their doctor to modify their therapy and enhance the management of their diabetes using all the data and charts that are provided [110].
-
8.
Diabetes:M: Diabetes:M on its part offers notifications for test time, a system for tracking and logging nutrition intake, incorporation with fitness applications, and a blood sugar trend mapping. Additionally, the app provides an insulin bolus calculation based on the added nutritional data. Trend graphs and charts over a range of periods can be viewed, putting glucose management back in user’s control [111].
-
9.
Beat Diabetes: Beat Diabetes app is mostly for newly diagnosed patients with diabetes, as it offers lots of diabetes 101 knowledge from the foods to avoid to easy techniques to improve one’s physical activity and latest treatment choices and learn what issues to look out for [112].
-
10.
One Drop for Diabetes health: The One Drop for Diabetes Health app is a diabetes management app that makes preferably activity options for the user based on their blood glucose data. With notifications and alerts, community sharing, and regular health statistics reports, the app also uses the users’ diet, exercise, and medication information to assist them in creating a complete diabetes management plan. This way, users can monitor their progress and make necessary behavioral changes [113].
Summarized in Table 3 are the functionalities of diabetes mHealth solutions discussed.
Functionalities of existing mHealth solutions for hypertension
Having detailed features of some mHealth solutions for self-management of diabetes, next are the features of some mHealth solutions for self-management of hypertension (summary of these features are presented in Table 4):
-
1.
Cardio: A heart fitness app “Cardio” makes use of pulse-reader technology to allow users to track their heart rate with just their fingers. The users’ smartphone’s camera light measures their pulse using the camera on the back of the device. Furthermore, it assists users to increase their numbers and aerobic capability with doctor’s consent using the app’s interval training circuit [114].
-
2.
Blood Pressure Companion: This app is used to monitor vital signs, such as blood pressure and heart rate, and also alert the user in case of any problems that may require action. It also makes it easy to download precise data which can be made available to healthcare physician. Additionally, it can be used to track blood pressure, heart rate, and weight along a histogram that displays the pattern of measurements over time [115].
-
3.
Blood Pressure Monitor: With the help of this app, users monitor their vital signs and manually enter them along with other information, such as prescription intake, to produce an unlimited lifetime representation of their patterns. Furthermore, the charts provided by the app can be used to learn how various components of users’ health and treatment plan interact with one another [116].
-
4.
Pacer: Pacer is designed to provide physical activity intervention to management of diabetes and hypertension. It records the number of steps taken by measuring the distance covered; it imitates having a walking partner and fitness coach in one device. The fitness aim focuses on the supervised exercises and customized fitness programs [117].
-
5.
My Diet Coach: The software assists users in learning what motivates them, how to maintain focus and resist food cravings, and how to make tiny, healthy lifestyle adjustments. With My Diet Coach, user may set a weight reduction target and monitor his progress. User can observe his/her weight loss graphically thanks to the app’s picture-based weight tracker. My Diet Coach offers inspiring advice and phrases, e.g., when a user succeeds, it rewards [118].
-
6.
Quardio: This app gives a precise data on heart rate, blood pressure, and other indicators of cardiovascular health. A more comprehensive picture of heart’s health is achieved from numbers when users mix visual input with other health measures like their weight, body fat, and muscle composition [119].
-
7.
HealthWatch 360: HealthWatch 360 is an app created to achieve nutritional objectives, by the use of scientific principles. The user chooses a health and wellness objective to start, like lowering blood pressure. The users will then receive daily data on their nutritional status from the app’s algorithm along with a personalized nutritional plan [120].
-
8.
Instant Heart Rate: Instant Heart Rate app converts the camera on the users’ phone into a heart-rate monitor, and then shows the reading in less than 10 s. The users take the easy test while seated and gets the record of their heart rate and a graph of their pulse waveform, or they use the app’s “StandUp” exam to gauge their level of fitness and weariness. The app logs users’ beats per minute and includes a note section so they can keep track of what they were doing when the test was taken [121].
-
9.
Pulse Point response: This app connects users with cardiopulmonary resuscitation (CPR)-trained communities that are prepared to help in a cardiac (or other) emergency before the arrival of emergency vehicles. This app utilizes the users GPS to alert nearby residents who have the ability to act fast and save lives before emergency medical services come. The app provides instructions to the closest automated external defibrillator while directing emergency personnel [122].
-
10.
Hello Heart: The HIPAA (Health Insurance Portability Accountability Act)-compliant app Hello Heart delivers users daily data about their blood pressure and BMI as well as reminders to take their medications. To get started, users inquire about obtaining a code from employer or physician. Then, after signing up and entering their blood pressure data daily, they may observe variations on a weekly timeline and base their health decisions on those parameters [123].
General challenges
As advantageous as mHealth systems have proven to be in management and treatment of diabetes and hypertension, there has been some setbacks. These challenges can also be viewed as determinants to factor into design and development of diabetes and hypertension mHealth solutions. Challenges to developing and using mHealth solutions are manifold and could be introduced from the stakeholders’ perspectives [124]. Istepanian and Al-Anzi [125] admit that balance between emerging considerations or perspectives will depend on how the various stakeholders from patients, healthcare providers, clinicians, medical and mobile health market businesses, and regulators will perceive such developments. Choukou [124] merges the stakeholders into four: user (patient), care provider, developer (design/technology), and management. Considering all stakeholders provides the advantage of not leaving out any setbacks plaguing mHealth systems for the two chronic diseases considered in this work.
Therefore, holistically, the challenges can be classified under design of the mHealth app, information/content, usability, functionality, ethical issues, security and privacy, and user-perceived value [126]. A couple more limitations are presented in [127] to include poor proof of its clinical value, poor connection with the healthcare system, and lack of acceptable assessment and documentation. Carrol et al. [127] affirmed security and privacy breaches as concerns in these mHealth solutions. For emphasis, in [128], set out rules for assessing mobile self-management apps for patients with long-term illness are grouped into four criteria which include engagement, functionality, usability, and information management. Our review of relevant literature yielded a total of 13 general challenges with diabetes and hypertension mHealth systems, viz.
Security and privacy
The most dreadful and technological roadblock in mHealth is the security and privacy of the health data [129]. Patients fear for health information compromise, considering that the rate at which health records are compromised is alarming. As cyber threats keep evolving, healthcare is the biggest prey [130]. Sadly, healthcare data violations were graded as highest priced in cost of a data breach report in the year 2020 with the average total cost of 3.86 million dollars per annum [131]. That figure rose to 4.24 million dollars in 2021 [132]. These present an ever-expanding weight of security and privacy concerns in self-management mHealth systems.
Functionality
Functionality in mHealth in this context can be seen as the features of mHealth apps that will enhance the users’ engagement and overall app productivity. According to [133], functionality features include technical support, chat that connects all user of the app, notifications, and viewing of patients test result. Non-integration of technical support features greatly affects the app usability, and it also leads to loss of users as seen in [134].
The study conducted in [135] proved that functionalities such as medical monitoring, notifications, logs of blood glucose, blood pressure monitoring, diet, and physical activities which were implemented in [136,137,138] study have the ability to help users manage their diabetes, blood pressure level, and body weight. These routines varying from user to user make providing users with option of personalizing content another sought-after functionality [139]. Furthermore, Benjamin et al. [133] presented an observation from the patients using the mHealth app by [140]. It was seen that the users showed a great sign of containment, with the app rating of 90%; this is as a result of engagement with the users all-through the development process and also implementation of chat that connects the users which was very vital.
Usability
Usability is referred to the length by which a product can be used by a designated users to reach a particular aim with success, productivity, and containment in a defined frame of reference [141]. Further to this definition, we can state that a patient being able to use the mHealth app and navigate through it without difficulties will solve the adherence issue to some extent and also enhance patients’ engagement to the app. Patients achieving satisfaction of their cardinal needs by using mHealth apps makes them emotionally bonded with the mHealth apps, with resultant overall improvement of well-being [142].
The issue of usability can be solved through provision of technical support and training of users. In the study conducted by Benjamin et al. [133], six of study participants gets assistance in using the app, by providing technical support for response to questions, assisting in downloads, or educating the users by phone; it was observed that a study without a technical support or assistance have a possibility of losing more customers, and this is as a result of the fact that there is possibility that the people that partook in the study do not have a technical knowledge to use the app. In the [141] study, a questionnaire-based approach was used to measure usability.
Additionally, substantial testing of mHealth app by end-users is of essence to disclose the pre-eminent technique and layout of the app for specific groups, which in other words will increase the usability of the mHealth app [143].
As an extension of what usability entails, users should be able to easily take their biomedical measurements with any peripheral device [144]. Also significant about usability are decision support functionalities and real-time feedback [145].
Information and content
The content and information provided in mHealth apps, how the information is portrayed, and the validity of presented information have a lot to do with the patients’ recovery process [139]. Given that most patients surveyed in [146] held positive attitudes towards mHealth and had tertiary education, the authors recommended improvement of user awareness. It is expected that such level of education and keenness to learn about mHealth have already laid the groundwork for an awareness campaign. Presenting appropriate information on the app and the app’s content will make the patients to have a good knowledge of the ailment. Also, the app should pay more attention on enhancing the connection between the patients and the ailment, rather than just curing the patients [133]. With amelioration of knowledge on ailment, partakers saw their ailment in a bad direction and their symptoms as more severe [147].
Interoperability
In medicine, interoperability entails that data is transferred accurately, successfully, securely, and consistently regardless of software applications, information technology systems, and networks in various platforms [148]. Scoping review of mHealth apps for self-management of cardiovascular disease in [149] revealed lack of interoperability of mHealth applications with other systems as a major challenge. So, while mHealth presents innovative approaches to enhance primary healthcare delivery in developing countries, its impact can be extended by improving interoperability with electronic medical records (EMR), patient health records, and electronic health records (EHR) [150, 151]. Though interoperability frameworks have been in existence, their accessibility and utility for connection of mHealth solutions to electronic records are relatively unknown in the developing world [150]. The power of an EHR lies not only in the data it contains, but how it is shared—health information becomes instantly accessible to authorized providers across practices and health organizations, helping to coordinate care efficiently [152], e.g., connecting patients’ blood pressure reports to their electronic medical record for review by their physicians is one of the four major ways mHealth systems help patients manage hypertension [153]. Fragmentation of these technologies remains a considerable concern [154]. Interoperability uses standards [148], protocols, and interfaces to connect systems using fitting techniques and frameworks. Other connected issues factored in are jurisprudence, agreements, workflows, and privacy issues [154].
Interoperability is frequently described in terms of five “levels”: technical, syntactic, semantic, organizational, and legal [155, 156]. From the literature review, four themes were identified: infrastructure, interoperability standards, data security, and usability. For clarity, the themes and levels were mapped to one another in the following manner. “Infrastructure” and “security” mapped to all five levels of interoperability, “standards” mapped to all except technical interoperability, and “usability” mapped to only organizational interoperability [150]. As would be seen later, the problem of lack of interoperability births other problems like data incompleteness and non-sustainability of mHealth solutions.
As a way forward, further findings in [154] present political and leadership support as key to realization of interoperability of mHealth applications and eRecord systems. One direction for this is the more robust regulation of eRecord systems. Supporting this is the findings in [157] that the absence of national agency and policy on mHealth and use of two systems in parallel are important deterrents of mHealth solution adoption in low- and middle-income nations. For example, there is the Agency for Integration, Diffusion, and Archiving of medical information (AIDA) in Portugal [158]. It is an agent-diversified and service-based platform that makes for interoperability between healthcare information systems. From a technical point of view for instance, a cloud middleware based on the Health Level Seven International (HL7) standard was demonstrated as capable of encoding and storing, as well as interoperating and integrating EHR data between different applications in different health facilities [159, 160].
Data incompleteness
When mHealth systems do not interoperate, there is bound to be data incompleteness, thus making interoperability between different electronic health records a partial solution to data incompleteness [161]. What consists data incompleteness is where we have incomplete information in relational databases; when a fact needs to be provided in a relation, meanwhile values for some needed columns are missing [162, 163]. Furthermore, based on interviews in [161], potential partners who can benefit and address the debacle of data incompleteness in electronic health records include the following: vendors of the EHR systems, organizations that provide data solutions, owners/managers of outpatient health facilities located in the rural regions, and health care process improvement organizations. If there are regulations compelling partnership of these players, data uncertainty and incompleteness would be ameliorated.
Unsustainability
Sustainability in the context of mHealth systems is the capacity for enduring satisfaction of user needs—whether those needs remain constant or extend [164]. The ability to handle growing needs and expanding resources is scalability component of sustainability. It is in the large part a challenge from the mHealth system developer’s perspective. Sustainability also dictates that an mHealth solution should be economically workable, environmentally tolerable, and socially fair [124, 165]. Pankomera et al. [166] give a case in point of mHealth applications, especially in developing countries, that are pilot projects and not centrally managed, say, by the government—a major player in regulation. They are mostly initiated by individual non-governmental organizations that target specific health care interventions. This lack of coordination foreshadows unsustainability in that knowledge gained from one project are not applied to subsequent projects. Also, these projects are not expanded once completed. This often means that the mHealth projects are discontinued. The lack of sustainability of mHealth projects wastes a lot of resources [166].
Aamir et al. [157] recommend understanding the matter of incremental innovation as a way of ensuring that resources spent on pilot mHealth interventions are enhanced, even to complete realization of their potential. As further way forward, Choukou [124] presents a step-by-step path for achieving sustainability from mHealth idea to sustainable mHealth solution. First is design, prototyping, and testing. Second is pilot testing involving evaluation of e-prototype, determination of both feasibility indicators, and measurable outcomes. Third is strategy at facility, national, and regional levels. This is where government, non-governmental organizations (NGOs), and academia at these three levels are collaborated with for more requirements/features of a proposed mHealth solution. Finally, the mHealth characteristics are set such as are efficient, evidence-based, economically viable, socially equitable, environmentally bearable, and sustainable. These characteristics also agree with ones advocated for in [165].
Prescription non-adherence
Prescription adherence or conformity often leaves much to be desired in adults with chronic diseases [167]. Adherence is defined as the degree to which the patient’s behavior is in agreement with his or her physician’s recommendations in terms regimen, quality, and quantity [168]. To mark how consequential non-adherence has been, in [39], non-adherence percentage was most significant for the top two most recommended lifestyle factors for hypertension management—sleep and restfulness.
Long-term prescription adherence is partly but significantly precipitated by culture [169]. One of such culture is associating credibility with years of experience. Some elderly patients have reported disobliging prescriptions from perceived inexperienced caregiver; adults between 60 and 79 years were found in [27] to be less likely to observe recommendations. The lack of face-to-face interaction in mHealth solutions means this cross-section of users is left without their usual credibility indicator. Another associate of prescription non-conformity is low income [100]. Fernandez-Lazaro et al. [170] recorded prescription non-adherence in 52% of the participants in their study. Participants numbering a total of 150 were interviewed over a course of 6 months from treatment inception. Even though these statistics have more to do with medication prescriptions, the way users treat prescription of non-pharmacological therapies is no different.
Modifications in treatment, shortage of information about medications, intangible number of follow-up visits, and lack of prescription reminders on mHealth apps are very likely to encourage disregard for prescriptions [170]. A study analyzing psychological techniques found some of those techniques potent in fostering prescription adherence by the elderly with chronic diseases. A combination of interactive communication with healthcare professionals, customized feedback messages, and varied functions was found to be most effectual [171]. Furthermore, appropriate levels of adherence can be optimally achieved via customized multifarious interventions which will consider factors with patients’ enlightenment and their information needs [101]. Regarding user information needs, patient-directed feedback about BP trends is argued to be the most virulent tool in management of hypertension using mHealth systems [153]. Prescription adherence is in some cases very related to user engagement. A user engagement tool like SMS reminder improves adherence [172, 173]. Adherence dictates if the user records improvements from the mHealth intervention. Such improvements in turn foster belief and preserve user interest—a crucial ingredient of user engagement.
User engagement
User engagement has to with the standard of the user experience that focuses on desirable aspects of interaction and captivation by technology [174]. Fostering of long-term use of mHealth systems is the other ingredient of user engagement emphasized in [175]. Process appraisal of intervention trials pinpointed shortage of initial and enduring engagement of users as an affective curtailment of the benefit of mHealth interventions [176]. The WHO in [103] recommends long-term tracking of patients for better results in hypertension management. The lack of long-term user fidelity to the apps gives a reason for the report in [177, 178] that long-term effects of mHealth interventions are yet fairly convincing. Furthermore, even when user choice is instigated by cogent recommendations, the presentation of an mHealth app, in terms of functionality, is key to sustained use [179]. Diabetes, one of the ailments under review in this work, demands that patients maintain optimal blood glucose (BG) through regular tests. Devotion to this routine for a chronic disease is not easy [175], hence the need for motivation. That these are potential pieces that make up patient engagement is undisputed, but at its pivot, patient engagement is a matter of care-providers and patients’ ethos [180].
The lack of engagement in the course of treating a patient is a perennial concern for health professionals, particularly those utilizing technology as a motivational factor [181]. The bedrock of user engagement is motivation. What the different approaches to user engagement have in common is motivation. Some of the motivational factors in use include goal management, navigation, interface design, notifications, depth of knowledge, data collection methods and tools, system rules, applicative recommendations, and user system fit [182]. Considered next are the key motivational factors for prolonged use of diabetes and hypertension mHealth systems, viz.:
-
1.
Gamification: Health behavior change support systems (HBCSSs) is a promising research discipline which focuses on the use systems and services to influence health or wellbeing behavior [183,184,185]. Gamification is a fun approach to improving health behavior change, especially improving intrinsic interest in mHealth applications while reducing prescription non-adherence. The study in [181] proved gamification as a viable approach to promoting user engagement for a hypertension monitoring app. Evaluated in the study were 14 patients with hypertension, split into groups to establish if the addition of game components would inspire improved engagement in health care. The results showed gamification inspired engagement. Even better results were recorded in groups that had assistance of health professionals in that they spent longer time with the app and were inspired to maintain control of their health. Furthermore, the study in [186] explored the impact of gamification on users’ tendency to sustained use of mHealth apps. Perceived usefulness, confirmation, and satisfaction were confirmed to have stimulating effect on continuance intention. In addition, the path and workings of users’ feelings as regards self-reliance, relatedness, and competence induced by interactions with different gamification components inspire persistence in the use of mHealth apps. Findings by Tran et al. [187] indicate that for medication adherence in mHealth apps, gamification, more than financial incentives, has been more widely studied. Across the retrieved articles, gamification alone (82%) recorded more use than financial incentives (9%) alone or a mix of the two (9%). Also, in [187], point-based features were the most dominant. Literature on the individual contributions of the gaming features is lacking. Gamification may prove advantageous, but the extrinsic interests it generates are the shortcomings [188]. Some of the adverse motivational results are user health behavior becoming over-dependent on gamified HBCSSs [189], distraction from health purpose [190], discouragement due to poor scores in the gaming [191], and trivialization of health context [192]. These can distract from promotion of adherence culture in users.
-
2.
User expectation: User expectation though discussed is re-presented here as a motivational factor for user engagement. Privacy, one of the expectations users have, is a motivational factor. So much so that users in [175] recommended that mHealth systems that collect and share personal data should have succinct opt-in and opt-out feature to inspire usage. Other expectations are that the system should be provide high quality data, integrated view, timely self-management information, and feedback [175]. Adaptation of these details a user’s customized features, which if not met discourages use of an mHealth system. User expectation is a sure way of achieving engagement. If user-centered features are to be improved on, stakeholders (especially users) must be involved extensively in development of mHealth systems [193]. Meanwhile, researchers mostly do not have sufficient experience in engaging patients as collaborators as they would research subjects [194]. The panacea to this is that mHealth developers and researchers should refine their elicitation of system requirements from users. Users involved on the other hand could be trained to offer telling and actionable input to the system requirements.
-
3.
Participatory health technology: Social media is an example of participatory health technology [195]. While social interactivity feature of mHealth systems does not necessarily influence its adoption/choice decision [196], it motivates user engagement (continuance of use once chosen). People with disease history were more inclined to learning from data, as well as from others through social media fusion [175]. However, the state of social media and regulation landscape have brought on perceived susceptibility among other issues [197]. Therefore, attaining a balanced nexus between privacy and patient quest for health knowledge on the platform of participatory health demands patient empowerment, linking participatory health enabling technologies with clinical records, open data sharing agreement, and electronic consent [195].
-
4.
Goal management: User engagement from goal management point of view may involve notification functionality on the mHealth app, sending text messages out to remind patients about to take their medication or schedule appointments for their next lab test. Also, patients can be considered engaged if they use mobile devices to observe vital signs like blood glucose level, blood pressure, or body weight. Vaghefi and Tulu [182] recommend synergy of user experience and goal management approaches to achieve sustained use of mHealth solutions for chronic diseases. Self-monitoring requires functionalities where users can evaluate their own performance, which can ease attainment of their health objectives. Data tracking, checklists, and fact-finding tools were pin-pointed in [198] as three functionalities that favor goal-setting and achievement in an mHealth system. Regarding setting up of goals, many users favored having options in goal attainment evaluation tools.
Alternative approach for health behavior change (HBC)
Grady et al. [199] argue that though influencing positive health behavior by exploiting individual users and personal determinants of health has its place in public health, alternative method should be explored. They noted that the instigators of chronic diseases like diabetes and hypertension are multi-factorial and complex and thrive within institutional and societal environments and systems. Therefore, mHealth systems should as an alternative approach aim at modifying institutional systems to foster environments that nurture health behaviors. There is currently a shortage of mHealth systems adopting this approach.
Another relatively unexplored method to achieving HBC is self-compassion. Self-compassion has proven a key quality to encourage for promoting positive health behaviors [200, 201], due in part to its connection with malleable emotions. The desirable components of self-compassion are strongly positively correlated with health-promoting behaviors [202]. While self-compassion is kindness to oneself, health-promoting behavior is engagement in practices that promote well-being and health [203].
Weak recommendation system
The prevalence of diabetes and hypertension has resulted in an avalanche of mHealth apps to choose from to manage both chronic diseases. Inundated with options, users rely on recommendations of family and friends, perceived relevance, brand recognition, and user ratings, rather than evidence of effectiveness [199]. Others choose mHealth apps based on sheer number of downloads indicated, not number of current users, which in this case would be a better decision metric. Users require platforms that offer tested and evidence-based recommendation to sort out their confusion. Curated health app portals are one way. National Health Service (NHS), UK, has solved the problem. Curated health app portals (e.g., National Health Service Apps Library and the Public Health England One You App portal) appeared to engender user trustworthiness and alleviate data protection concerns [179]. This is because curated health portals publish or recommend mHealth apps that have proven results of effectiveness.
Compliance
If an mHealth application operates in a manner that consistently conforms with a rule, then it is said to be in compliance with the regulation [204]. Mobile health systems are less likely to have bugs, security issues, and poor design if it complies with software standards [205]. Moreover, for the purpose of licensing and certification, governmental and regulatory authorities demand conformity with applicable standards and rules [206], and establishments also need conformity with clearly defined rules from their suppliers to have a quality and clear production [207].
The problem and demands of many stakeholder groups are formulated as requirements that direct the building of software products [208]. Since the greater number of these demands are often derived from corporate stakeholders, such as customers or users, community stakeholders are becoming more and more important [209]. Governments and other organizations known as community stakeholders, establish laws, rules, and best practices which are considered as compliance requirements [210]. To help decrease mistakes, security issues, and bad design, mHealth applications like those for diabetes and hypertension should adhere to the health and software standards.
Fan et al. [211] present findings on major mHealth compliance violations, especially violations of General Data Protection Regulation (GDPR), a regulation to optimize privacy protection as incompleteness of privacy policy, the insecurity of data transmission, and the inconsistency of data collections. As medical equipment/devices are treated under strict regulations, so should mHealth solutions, since they are also qualified as medical devices [212].
Design and design framework
The proliferation of mHealth has not been accompanied by a corresponding growth in design guidelines for mHealth applications [213]. Design framework used in the development of mHealth systems can help resolve many of the contextual challenges with mHealth solutions afore-listed. For example, better understanding of user-preferred design features and functions of technologies is a way to achieve user engagement [214]. Another example is that designing diabetes and hypertension self-management apps without health behavior theory may lead to intangible promotion of prescription adherence [167]. Furthermore, Wei et al. [215] linked proper design of mHealth systems to good user experience and user engagement. All these prove design as the one-size-fits-all solution to most user-centered issues with diabetes and hypertension mHealth apps. Consequently, Farao et al. [213] encourage a synergy of the Information Systems Research framework and design thinking, for mHealth design in a developing, under-resourced scenario. What is more, Bhatia et al. [216] recommends addition of regulatory sandboxes as controlled and monitored real-world test setting for mHealth solutions prior to large scale deployment. This was as they observed that end-user demands and clinical shortcomings are often poorly recognized when designing solutions, contributing to a massive drop in usage, known as the “law of attrition” in electronic health.
Conclusions
Diabetes and hypertension are chronic illnesses that require management and control, and utilizing mobile technology to help patients manage their health is essential. Exponential increase in number of people with access to smartphones has made developing mobile health applications for management of diabetes and hypertension a viable and appealing approach to augmenting face-to-face caregiver-patient interactions. This work cataloged the general challenges impeding the expected advantages of mHealth intervention. They include issues with security and privacy, functionality, interoperability, usability, data incompleteness, unsustainability, user engagement, compliance, prescription non-adherence, and weak recommendation system. Though the challenges were mostly user-centered challenges, there are also ones from perspective of other stakeholders like mHealth developers and health policy makers. All these challenges could be addressed by how the design framework of an mHealth system is laid out. Since the use of diabetes and hypertension mHealth solutions is mostly about self-management, the work identified self-management of the two non-communicable diseases to be mostly of non-surgical and non-pharmacological genre. Dietary management, physical exercise, and sleep were identified to be cost-adaptive and cost-effective alternatives that fit the two classes.
The use of mHealth solutions has not evolved past advancements in treatment (diagnosis and early detection) of these two co-morbid diseases anymore than the treatment has evolved past headway in machine learning in healthcare. This necessitated the review on machine learning as applied to diabetes and hypertension, with the objective of understanding the aspects of diabetes and hypertension research approached by machine learning and which machine learning models have impacted more in terms of performance and extent to which there has been a nexus between machine learning and mHealth still with bias on diabetes and hypertension.
Availability of data and materials
Not applicable.
Abbreviations
- AB:
-
AdaBoost
- ANN:
-
Artificial neural networks
- API:
-
Application programming interface
- AID:
-
Automated insulin delivery
- AIDS:
-
Agency for Integration, Diffusion, and Archiving of medical information
- AUC:
-
Area under the ROC curve
- BGL:
-
Blood glucose level
- BPT:
-
Blood pressure telemonitoring
- BMI:
-
Body mass index
- D(Early):
-
Early detection of diabetes
- CGM:
-
Continuous glucose monitoring
- CSII:
-
Continuous subcutaneous insulin delivery
- CVD:
-
Cardiovascular disease
- CPCSSN:
-
Canadian Primary Care Sentinel Surveillance Network
- CPR:
-
Cardiopulmonary resuscitation
- C + S:
-
Clinical and sociodemographic data
- DL:
-
Deep learning
- DNN:
-
Deep neural network
- DTs:
-
Diabetes technologies
- DT:
-
Decision tree
- ECG:
-
Electrocardiography
- Echo:
-
Echocardiography
- EHR:
-
Electronic health record
- EMR:
-
Electronic medical record
- FDA:
-
Fisher’s discriminant analysis
- G:
-
Gradient boost
- GP:
-
Gaussian process
- GDPR:
-
General Data Protection Regulation
- HIPAA:
-
Health Insurance Portability Accountability Act
- HBCSSs:
-
Health behavior change support systems
- HL7:
-
Health Level Seven International
- HPM:
-
Hybrid prediction mode
- MLP:
-
Multilayer perceptron
- MA:
-
Moving average
- LDA:
-
Linear discriminant analysis
- LR:
-
Logistic regression
- LSTM:
-
Long short-term memory
- ML:
-
Machine learning
- MetS:
-
Metabolic syndrome
- NB:
-
Naive Bayes
- NGO:
-
Non-governmental organizations
- OSA:
-
Obstructive sleep apnea
- PAH:
-
Pulmonary artery hypertension
- PH:
-
Pulmonary hypertension
- PPG:
-
Photoplethysmography
- P(risk):
-
Prediction of risk factors of diabetes
- PIDD:
-
Pima Indian Diabetes Database
- RLS:
-
Restless leg syndrome
- ROC:
-
Receiver operating characteristics
- SMOTE:
-
Synthetic minority over-sampling technique
- SVM:
-
Support vector machine
- T1DM:
-
Type 1 diabetes mellitus
- WHO:
-
World Health Organization
- XGB:
-
Extreme gradient boost
References
Anderson K, Burford O, Emmerton L (2016) Mobile health apps to facilitate self-care: a qualitative study of user experiences. PloS One 11(5):0156164
Steinhubl S, Muse E, Topol E (2015) The emerging field of mobile health. science translational medicine. The emerging field of mobile health. Sci Transl Med 7(283):777–780
Silva B, Rodrigues JJ, Canelo F, Lopes I, Lloret J (2019) Towards a cooperative security system for mobile-health applications. Electronic Commerce Res 19(3):629–654
Istepanian RS, AlAnzi T (2020) Mobile health (m-health): Evidence-based progress or scientific retrogression. In: Biomedical Information Technology. Elsevier, Academic Press, p 717–733
Chen Y, Yang L, Zhang M, Yang J (2018) Central or peripheral? cognition elaboration cues’ effect on users’ continuance intention of mobile health applications in the developing markets. Int J Med Inform 116:33–45
Organization, W.H et al (2018) mHealth. use of appropriate digital technologies for public health: report by director-general. 71st World Health Assembly provisional agenda item 12. p 71
Vegesna A, Tran M, Angelaccio M, Arcona S (2017) Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemed e-Health 23(1):3–17
Brzan PP, Rotman E, Pajnkihar M, Klanjsek P (2016) Mobile applications for control and self management of diabetes: a systematic review. J Med Syst 40(9):1–10
Priesterroth L, Grammes J, Clauter M, Kubiak T (2021) Diabetes technologies in people with type 1 diabetes mellitus and disordered eating: a systematic review on continuous subcutaneous insulin infusion, continuous glucose monitoring and automated insulin delivery. Diabetic Med 38(7):14581
Umpierrez GE, Klonoff DC (2018) Diabetes technology update: use of insulin pumps and continuous glucose monitoring in the hospital. Diabetes Care 41(8):1579–1589
Wang X, Shu W, Du J, Du M, Wang P, Xue M, Zheng H, Jiang Y, Yin S, Liang D et al (2019) Mobile health in the management of type 1 diabetes: a systematic review and meta-analysis. BMC Endocrine Disord 19(1):1–10
Qureshi KN, Din S, Jeon G, Piccialli F (2020) An accurate and dynamic predictive model for a smart m-health system using machine learning. Inf Sci 538:486–502
Cappon G, Vettoretti M, Sparacino G, Facchinetti A (2019) Continuous glucose monitoring sensors for diabetes management: a review of technologies and applications. Diabetes Metab J 43(4):383–397
WHO (2022) Hypertension (https://www.who.int/health-topics/hypertension . Online; Accessed 2 July 2022 )
Kitt, J., Fox, R., Tucker, K.L.: Digital health: new approaches in hypertension management. J Cardiol Cardiovasc Sci 4(1) (2020)
Clim A, Răzvan DZ (2019) Game theory in designing mHealth apps for monitoring hypertension. Manag Mark 14(2):220–231
Zhang, C., Zhang, X., Halstead-Nussloch, R.: Assessment metrics, challenges and strategies for mobile health apps. Issues in Inf Syst 15(2) (2014)
Cheung B (2010) This is a brief review of the overlap between hypertension and type-2 diabetes that proposes there is a spectrum ranging from hypertension without dysglycemia to type-2 diabetes without elevated blood pressure The hypertension-diabetescontinuum. J Cardiovasc Pharmacol 55:333–9
Hall ME, do Carmo JM, da Silva AA, Juncos LA, Wang Z, Hall JE (2014) Obesity, hypertension, and chronic kidney disease. Int J Nephrol Renovasc Dis 7:75
Cheung BM, Li C (2012) Diabetes and hypertension: is there a common metabolic pathway? Curr Atheroscler Rep 14(2):160–166
Mahmood S, Shah KU, Khan TM, Nawaz S, Rashid H, Baqar SWA, Kamran S (2019) Non-pharmacological management of hypertension: in the light of current research. Irish J Med Sci (1971) 188(2):437–452
Raveendran AV, Chacko EC, Pappachan JM (2018) Non-pharmacological treatment options in the management of diabetes mellitus. Eur Endocrinol 14(2):31
Chaudhary A, Gustafson D, Mathys A (2018) Multi-indicator sustainability assessment of global food systems. Nat Commun 9(1):1–13
Ma’aruf LM, Garba M (2019) Design and implementation of an expert diet prescription system. Int J Artif Intell Expert Syst 4(6):126–134
Lee H-Y, Park JB (2015) The Korean Society of Hypertension guidelines for the management of hypertension in 2013: its essentials and key points. Pulse 3(1):21–28
Shim J-S, Oh K, Jung SJ, Kim HC (2020) Self-reported diet management and adherence to dietary guidelines in Korean adults with hypertension. Korean Circ J 50(5):432–440
Bonger Z, Shiferaw S, Tariku EZ (2018) Adherence to diabetic self-care practices and its associated factors among patients with type 2 diabetes in addis ababa, ethiopia. Patient Preference Adherence 12:963
Damy T, Benedyga V, Pezel T, Berthelot E, Gauthier J, Habib G, Iliou M-C, Aupetit J-F, Baudry G, De Groote P et al (2022) Prescription, compliance, and burden associated with salt-restricted diets in heart failure patients: results from the French National OFICSel Observatory. Nutrients 14(2):308
Opiyo RO, Nyasulu PS, Olenja J, Zunza M, Nguyen KA, Bukania Z, Nabakwe E, Mbogo A, Were AO (2019) Factors associated with adherence to dietary prescription among adult patients with chronic kidney disease on hemodialysis in national referral hospitals in Kenya: a mixed-methods survey. Renal Replace Ther 5(1):1–14
Awuchi CG, Echeta CK, Igwe VS (2020) Diabetes and the nutrition and diets for its prevention and treatment: a systematic review and dietetic perspective. Health Sci Res 6(1):5–19
Bachman V (2016) Physical activity and risks of breast cancer, colon cancer, diabetes, ischemic heart disease and ischemic stroke events: a systematic review and dose-response meta-analysis for the global burden of disease study 2013
Barone Gibbs B, Hivert MF, Jerome GJ, Kraus WE, Rosenkranz SK, Schorr EN, Spartano NL, Lobelo F, on Lifestyle, A.H.A.C., on Cardiovascular, C.H.C., Nursing;, S., on Clinical Cardiology, C (2021) Physical activity as a critical component of first-line treatment for elevated blood pressure or cholesterol: who, what, and how?: a scientific statement from the American Heart Association. Hypertension 78(2):26–37
WHO (2022) Physical Activity (https://www.who.int/health-topics/physical-activity . Online; Accessed 23 March 2022 )
Sigal RJ, Armstrong MJ, Bacon SL, Boule NG, Dasgupta K, Kenny GP, Riddell MC (2018) Physical activity and diabetes. Can J Diabetes 42:54–63
Cannata F, Vadalà G, Russo F, Papalia R, Napoli N, Pozzilli P (2020) Beneficial effects of physical activity in diabetic patients. J Functional Morphol Kinesiol 5(3):70
Bakker EA, Sui X, Brellenthin AG, Lee DC (2018) Physical activity and fitness for the prevention of hypertension. Curr Opin Cardiol 33(4):394–401
Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B, Campbell WW, Dietz S, DiPietro L, George SM et al (2019) Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc 51(6):1314–1323
Mustafa, A.S., Ali, N., Dhillon, J.S., Alkawsi, G., Baashar, Y.: User engagement and abandonment of mHealth: a cross-sectional survey. In: Healthcare, vol. 10, p. 221 (2022). MDPI
Leitner, J., Chiang, P.-H., Khan, B., Dey, S.: An mHealth lifestyle intervention service for improving blood pressure using machine learning and iomts. In: 2022 IEEE International Conference on Digital Health (ICDH), pp. 142–150 (2022). IEEE
Perfect MM (2020) Sleep-related disorders in patients with type 1 diabetes mellitus: current insights. Nat Sci Sleep 12:101
Maiolino G, Bisogni V, Silvani A, Pengo MF, Lombardi C, Parati G (2020) Treating sleep disorders to improve blood pressure control and cardiovascular prevention: a dream come true?—a narrative review. J Thorac Dis 12(Suppl 2):225
Bathgate CJ, Fernandez-Mendoza J (2018) Insomnia, short sleep duration, and high blood pressure: recent evidence and future directions for the prevention and management of hypertension. Curr Hypertens Rep 20(6):1–10
Kaneko H, Itoh H, Kiriyama H, Kamon T, Fujiu K, Morita K, Michihata N, Jo T, Takeda N, Morita H et al (2020) Restfulness from sleep and subsequent cardiovascular disease in the general population. Sci Rep 10(1):1–10
Berrouiguet S, Barrigón ML, Castroman JL, Courtet P, Artés-Rodríguez A, Baca-García E (2019) Combining mobile-health (mHealth) and artificial intelligence (AI) methods to avoid suicide attempts: the Smartcrises study protocol. BMC Psychiatry 19(1):1–9
El-Rashidy N, El-Sappagh S, Islam S, M El-Bakry H, Abdelrazek S (2021) Mobile health in remote patient monitoring for chronic diseases: principles, trends, and challenges. Diagnostics 11(4):607
Alazzam, M.B., Mansour, H., Alassery, F., Almulihi, A.: Machine learning implementation of a diabetic patient monitoring system using interactive e-app. Comput Intell Neurosci 2021 (2021)
Aczon, M., Ledbetter, D., Ho, L., Gunny, A., Flynn, A., Williams, J., Wetzel, R.: Dynamic mortality risk predictions in pediatric critical care using recurrent neural networks,(2017). arXiv preprint arXiv 1701 (2019)
Sharma, N., Singh, A.: Diabetes detection and prediction using machine learning/IoT: a survey. In: International Conference on Advanced Informatics for Computing Research, pp. 471–479 (2018). Springer
Omboni S, Panzeri E, Campolo L (2020) E-health in hypertension management: an insight into the current and future role of blood pressure telemonitoring. Curr Hypertens Rep 22(6):1–13
Aguilera A, Figueroa CA, Hernandez-Ramos R, Sarkar U, Cemballi A, Gomez-Pathak L, Miramontes J, Yom-Tov E, Chakraborty B, Yan X et al (2020) mHealth app using machine learning to increase physical activity in diabetes and depression: clinical trial protocol for the diamante study. BMJ Open 10(8):034723
Martinez-Ríos E, Montesinos L, Alfaro-Ponce M (2022) A machine learning approach for hypertension detection based on photoplethysmography and clinical data. Comput Biol Med 145:105479 (Elsevier)
Jordan MI, Mitchell TM (2015) Machine learning: trends, perspectives, and prospects. Science 349(6245):255–260
Mishra S, Mallick PK, Tripathy HK, Bhoi AK, González-Briones A (2020) Performance evaluation of a proposed machine learning model for chronic disease datasets using an integrated attribute evaluator and an improved decision tree classifier. Appl Sci 10(22):8137
Kavakiotis I, Tsave O, Salifoglou A, Maglaveras N, Vlahavas I, Chouvarda I (2017) Machine learning and data mining methods in diabetes research. Comput Structural Biotechnol J 15:104–116
Ismail L, Materwala H, Tayefi M, Ngo P, Karduck AP (2022) Type 2 diabetes with artificial intelligence machine learning: methods and evaluation. Arch Comput Methods Eng 29(1):313–333 (Springer)
Bhatt P, Liu J, Gong Y, Wang J, Guo Y et al (2022) Emerging artificial intelligence–empowered mhealth: scoping review. JMIR mHealth uHealth 10(6):35053
Butt, U.M., Letchmunan, S., Ali, M., Hassan, F.H., Baqir, A., Sherazi, H.H.R.: Machine learning based diabetes classification and prediction for healthcare applications. J Healthc Eng 2021 (2021)
Suzuki Y, Suzuki H, Ishikawa T, Yamada Y, Yatoh S, Sugano Y, Iwasaki H, Sekiya M, Yahagi N, Hada Y et al (2022) Exploratory analysis using machine learning of predictive factors for falls in type 2 diabetes. Sci Rep 12(1):1–10 (Springer)
Lai H, Huang H, Keshavjee K, Guergachi A, Gao X (2019) Predictive models for diabetes mellitus using machine learning techniques. BMC Endocr Disord 19(1):1–9
Maniruzzaman M, Rahman M, Ahammed B, Abedin M et al (2020) Classification and prediction of diabetes disease using machine learning paradigm. Health Inf Sci Syst 8(1):1–14
Perveen S, Shahbaz M, Guergachi A, Keshavjee K (2016) Performance analysis of data mining classification techniques to predict diabetes. Procedia Comput Sci 82:115–121
Ghosh P, Azam S, Karim A, Hassan M, Roy K, Jonkman M (2021) A comparative study of different machine learning tools in detecting diabetes. Procedia Comput Sci 192:467–477
Meng X-H, Huang Y-X, Rao D-P, Zhang Q, Liu Q (2013) Comparison of three data mining models for predicting diabetes or prediabetes by risk factors. Kaohsiung J Med Sci 29(2):93–99
Kandhasamy JP, Balamurali S (2015) Performance analysis of classifier models to predict diabetes mellitus. Procedia Comput Sci 47:45–51
Saru, S., Subashree, S.: Analysis and prediction of diabetes using machine learning. International journal of emerging technology and innovative engineering 5(4) (2019)
Maniruzzaman M, Kumar N, Abedin MM, Islam MS, Suri HS, El-Baz AS, Suri JS (2017) Comparative approaches for classification of diabetes mellitus data: Machine learning paradigm. Comput Methods Programs Biomed 152:23–34
Sako, Z., Adibi, S., Wickramasinghe, N.: Addressing data accuracy and information integrity in mHealth solutions using machine learning algorithms. In: Delivering Superior Health and Wellness Management with IoT and Analytics, pp. 345–359. Springer, ??? (2020)
Agrawal H, Jain P, Joshi AM (2022) Machine learning models for non-invasive glucose measurement: towards diabetes management in smart healthcare. Health Technol 12(5):955–970 (Springer)
Padhy, S., Dash, S., Routray, S., Ahmad, S., Nazeer, J., Alam, A.: IoT-based hybrid ensemble machine learning model for efficient diabetes mellitus prediction. Comput Intell Neurosci 2022 (2022)
Chang, V., Bailey, J., Xu, Q.A., Sun, Z.: Pima Indians diabetes mellitus classification based on machine learning (ML) algorithms. Neural Comput Appl, 1–17 (2022). Springer
Haneef R, Kab S, Hrzic R, Fuentes S, Fosse-Edorh S, Cosson E, Gallay A (2021) Use of artificial intelligence for public health surveillance: a case study to develop a machine learning-algorithm to estimate the incidence of diabetes mellitus in france. Arch Public Health 79(1):1–13
Fregoso-Aparicio L, Noguez J, Montesinos L, García-García JA (2021) Machine learning and deep learning predictive models for type 2 diabetes: a systematic review. Diabetol Metab Syndr 13(1):1–22
Islam MM, Rahman MJ, Roy DC, Maniruzzaman M (2020) Automated detection and classification of diabetes disease based on bangladesh demographic and health survey data, 2011 using machine learning approach. Diabetes Metab Syndr 14(3):217–219 (Elsevier)
Sadeghi S, Khalili D, Ramezankhani A, Mansournia MA, Parsaeian M (2022) Diabetes mellitus risk prediction in the presence of class imbalance using flexible machine learning methods. BMC Med Inf Decis Mak 22(1):1–12 (Springer)
Dinh A, Miertschin S, Young A, Mohanty SD (2019) A data-driven approach to predicting diabetes and cardiovascular disease with machine learning. BMC Med Inf Decis Mak 19(1):1–15
Ijaz MF, Alfian G, Syafrudin M, Rhee J (2018) Hybrid prediction model for type 2 diabetes and hypertension using dbscan-based outlier detection, synthetic minority over sampling technique (smote), and random forest. Appl Sci 8(8):1325
Wu H, Yang S, Huang Z, He J, Wang X (2018) Type 2 diabetes mellitus prediction model based on data mining. Inf Med Unlocked 10:100–107 (Elsevier)
Muhammad L, Algehyne EA, Usman SS (2020) Predictive supervised machine learning models for diabetes mellitus. SN Comput Sci 1(5):1–10 (Springer)
Martinez-Ríos E, Montesinos L, Alfaro-Ponce M, Pecchia L (2021) A review of machine learning in hypertension detection and blood pressure estimation based on clinical and physiological data. Biomed Signal Process Control 68:102813
Parati G, Ochoa JE, Bilo G (2017) Moving beyond office blood pressure to achieve a personalized and more precise hypertension management: Which way to go? Hypertension 70(3):20–31
Gupta K, Bajaj V, Ansari IA (2023) A support system for automatic classification of hypertension using BCG signals. Expert Syst Appl 214:119058 (Elsevier)
Leha A, Hellenkamp K, Unsöld B, Mushemi-Blake S, Shah AM, Hasenfuß G, Seidler T (2019) A machine learning approach for the prediction of pulmonary hypertension. PloS One 14(10):0224453
Zhao H, Zhang X, Xu Y, Gao L, Ma Z, Sun Y, Wang W (2021) Predicting the risk of hypertension based on several easy-to-collect risk factors: a machine learning method. Front Public Health 9:619429
Islam MM, Rahman MJ, Roy DC, Tawabunnahar M, Jahan R, Ahmed NF, Maniruzzaman M (2021) Machine learning algorithm for characterizing risks of hypertension, at an early stage in Bangladesh. Diabetes Metab Syndrome 15(3):877–884
AlKaabi LA, Ahmed LS, Al Attiyah MF, Abdel-Rahman ME (2020) Predicting hypertension using machine learning: findings from Qatar Biobank study. Plos One 15(10):0240370
Errington N, Iremonger J, Pickworth JA, Kariotis S, Rhodes CJ, Rothman AM, Condliffe R, Elliot CA, Kiely DG, Howard LS et al (2021) A diagnostic miRNA signature for pulmonary arterial hypertension using a consensus machine learning approach. EBioMedicine 69:103444 (Elsevier)
Islam, S.M.S., Talukder, A., Awal, M.A., Siddiqui, M.M.U., Ahamad, M.M., Ahammed, B., Rawal, L.B., Alizadehsani, R., Abawajy, J., Laranjo, L., et al.: Machine learning approaches for predicting hypertension and its associated factors using population-level data from three South Asian countries. Front Cardiovasc Med 9 (2022)
Sakr S, Elshawi R, Ahmed A, Qureshi WT, Brawner C, Keteyian S, Blaha MJ, Al-Mallah MH (2018) Using machine learning on cardiorespiratory fitness data for predicting hypertension: the Henry Ford Exercise Testing (FIT) project. PLoS One 13(4):0195344
Zhu F, Xu D, Liu Y, Lou K, He Z, Zhang H, Sheng Y, Yang R, Li X, Kong X et al (2020) Machine learning for the diagnosis of pulmonary hypertension. Kardiologiia 60(6):96–101
Golino, H.F., Amaral, L.S.d.B., Duarte, S.F.P., Gomes, C.M.A., Soares, T.d.J., Reis, L.A.d., Santos, J.: Predicting increased blood pressure using machine learning. J Obesity 2014 (2014)
Healthline (2022) How to choose a diabetes app (https://www.healthline.com/health/diabetes/top-iphone-android-apps . Online; Accessed 22 July 2022 )
Salari R, Kalhori SRN, GhaziSaeedi M, Jeddi M, Fatehi F (2020) Development and usability evaluation of a mobile-based and cloud-based system for self-management of people with type 2 diabetes. J Med Internet Res 54(25):68–72
Istepanian RS, Casiglia D, Gregory JW (2017) Mobile health (m-Health) for diabetes management. Br J Healthc Manag 23(3):102–108
Istepanian R, Woodward B (2017) m-Health: fundamentals and applications. The Institute of Electrical and Electronics Engineering. John Wiley and Sons, Inc., Hoboken
Fu HN, Rizvi RF, Wyman JF, Adam TJ (2020) Usability evaluation of four top-rated commercially available diabetes apps for adults with type 2 diabetes. Comput Inf Nurs 38(6):274
Torbjørnsen A, Ribu L, Rønnevig M, Grøttland A, Helseth S (2019) Users’ acceptability of a mobile application for persons with type 2 diabetes: a qualitative study. BMC Health Serv Res 19(1):1–14
Jongsma KR, van den Heuvel JF, Rake J, Bredenoord AL, Bekker MN (2020) User experiences with and recommendations for mobile health technology for hypertensive disorders of pregnancy: Mixed methods study. JMIR mHealth uHealth 8(8):17271
Healthline: About Us. https://www.healthline.com/about/about-us. Online; Accessed 10 July 2022
Ali N, Akram R, Sheikh N, Sarker AR, Sultana M (2019) Sex-specific prevalence, inequality and associated predictors of hypertension, diabetes, and comorbidity among Bangladeshi adults: results from a nationwide cross-sectional demographic and health survey. BMJ Open 9(9):029364
Yu H (2015) Universal health insurance coverage for 1.3 billion people: what accounts for China’s success? Health Policy 119(9):1145–1152
Fernandez-Lazaro CI, García-González JM, Adams DP, Fernandez-Lazaro D, Mielgo-Ayuso J, Caballero-Garcia A, Moreno Racionero F, Córdova A, Miron-Canelo JA (2019) Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study. BMC Fam Pract 20(1):1–12
Shan R, Sarkar S, Martin SS (2019) Digital health technology and mobile devices for the management of diabetes mellitus: state of the art. Diabetologia 62(6):877–887
Organization, W.H et al (2021) Hypertension indicators for improving quality and coverage of services, virtual meeting, 1–2 march 2021: report
WellDoc (2010) Bluestar Diabetes (https://play.google.com/store/apps/details?id=com.welldoc.allstar . Online; Accessed 19 July 2022 )
Studio, M.: Glucose tracker & Diabetic diary. https://play.google.com/store/apps/details?id=melstudio.msugar. [Online; Accessed 16 May 2022
Media, M.: Fooducate. https://play.google.com/store/apps/details?id=com.fooducate.nutritionapp. Online; Accessed 12 June 2022
AzumioInc.: Fooducate. 2022. https://apps.apple.com/us/app/glucose-buddy-diabetes-tracker. [Online; Accessed 15 July 2022
MyFitnessPal: My FitnessPal: Calorie Counter. https://play.google.com/store/apps/details?id=com.myfitnesspal.android. Online; Accessed 22 June 2022
Healthline: Bezzy T2D. https://play.google.com/store/apps/details?id=com.healthline.t2d. Online; Accessed 22 June 2022
mySugr GmbH: mySugr - Diabetes Tracker Log. https://play.google.com/store/apps/details?id=com.mysugr.android.companion. [Online; Accessed 20 Aug 2022]
SirmaMedicalSystems: Diabetes:M - Blood Sugar Diary. https://play.google.com/store/apps/details?id=com.mydiabetes. [Online; Accessed 22 Aug 2022]
Tipsbook: Beat Diabetes. https://play.google.com/store/apps/details?id=com.andromo.dev462136.app489914. Online; Accessed 22 April 2022
OneDrop: One Drop: Better Health Today. https://play.google.com/store/apps/details?id=today.onedrop.android. Online; Accessed 27 June 2022
Cardiio (2020) Cardiio: Heart Rate Monitor (https://apps.apple.com/us/app/cardiio-heart-rate-monitor . Online; Accessed 10 Aug 2022 )
MaxwellSoftware (2021) Blood Pressure Companion (https://apps.apple.com/us/app/blood-pressure-companion . Online; Accessed 20 Aug 2022 )
Taconic (2021) Blood Pressure Monitor (https://apps.apple.com/us/app/blood-pressure-monitor-family . Online; Accessed 21-July-2022 )
PacerHealth: Pacer Pedometer. https://play.google.com/store/apps/details?id=cc.pacer.androidapp. Online; Accessed 10 July 2022
EasyTiger: My Diet Coach. https://www.apps.apple.com/us/app/my-diet-coach-weight-loss. Online; Accessed 12 June 2022
Qardio: Qardio Heart Health. https://play.google.com/store/apps/details?id=com.getqardio.android. Online; Accessed 22-March-2022
HealthWatch, G (2018) HealthWatch 360 (https://play.google.com/store/apps/details?id=com.gbhealthwatch.healthwatch360 . 10 Aug 2022 )
Inc, A (2021) Instant Heart Rate (https://play.google.com/store/apps/details?id=si.modula.android.instantheartrate . Online; Accessed 31 Aug 2022 )
PulsePointFoundation: PulsePoint Respond.https://play.google.com/store/apps/details?id=mobi.firedepartment. Online; Accessed 10 March 2022
Heart, H.: Hello Heart. https://play.google.com/store/apps/details?id=com.helloheart.app.healthplan&hl=en&gl=US. Online; Accessed 13June 2022
Choukou, M.-A.: Sustainability of mhealth solutions for healthcare system strengthening. In: Digital Health, pp. 171–189. Elsevier, ??? (2021)
Istepanian RS, Al-Anzi T (2018) m-health 2.0: new perspectives on mobile health, machine learning and big data analytics. Methods 151:34–40
Nouri R, R Niakan Kalhori S, Ghazisaeedi M, Marchand G, Yasini M (2018) Criteria for assessing the quality of mHealth apps: a systematic review. J Am Med Inf Assoc 25(8):1089–1098
Carroll JK, Moorhead A, Bond R, LeBlanc WG, Petrella RJ, Fiscella K (2017) Who uses mobile phone health apps and does use matter? a secondary data analytics approach. J Med Internet Res 19(4):5604
Anderson K, Burford O, Emmerton L et al (2016) App chronic disease checklist: protocol to evaluate mobile apps for chronic disease self-management. JMIR Res Protocols 5(4):6194
Zahra F, Hussain A, Mohd H (2018) Factor affecting mobile health application for chronic diseases. J Telecommun Electronic Computr Eng 10(1–11):77–81
IBM: Health care. https://www.ibm.com/uk-en/campaign/security-for-industries. Online; Accessed 2-April-2022
IBM (2020) Cost of a data breach 2022 (https://www.ibm.com/reports/data-breach . Online; Accessed 2 June 2022 )
IBM (2022) How much does a data breach cost? (https://www.ibm.com/security/data-breach . Online; Accessed 1 July 2022 )
Benjamin, S., Fudickar, S., Lins, C.: Mobile applications for self-management of chronic diseases: a systematic review. In: Biostec 2022: 15th International Joint Conference on Biomedical Engineering Systems and Technologies, pp. 542–548 (2022). SciTePress Digital Library
Ravn Jakobsen P, Hermann AP, Søndergaard J, Wiil UK, Clemensen J (2018) Help at hand: women’s experiences of using a mobile health application upon diagnosis of asymptomatic osteoporosis. SAGE Open Med 6:2050312118807617
Debon R, Coleone JD, Bellei EA, De Marchi ACB (2019) Mobile health applications for chronic diseases: a systematic review of features for lifestyle improvement. Diabetes Metab Syndr 13(4):2507–2512
Ribu L, Holmen H, Torbjørnsen A, Wahl AK, Grøttland A, Småstuen MC, Elind E, Bergmo TS, Breivik E, Årsand E et al (2013) Low-intensity self-management intervention for persons with type 2 diabetes using a mobile phone-based diabetes diary, with and without health counseling and motivational interviewing: protocol for a randomized controlled trial. JMIR Res Protoc 2(2):2768
Alonso-Domínguez R, Gómez-Marcos MA, Patino-Alonso MC, Sánchez-Aguadero N, Agudo-Conde C, Castaño-Sánchez C, García-Ortiz L, Recio-Rodríguez JI (2017) Effectiveness of a multifactorial intervention based on an application for smartphones, heart-healthy walks and a nutritional workshop in patients with type 2 diabetes mellitus in primary care (EMID): study protocol for a randomised controlled trial. BMJ Open 7(9):016191
Toro-Ramos T, Kim Y, Wood M, Rajda J, Niejadlik K, Honcz J, Marrero D, Fawer A, Michaelides A (2017) Efficacy of a mobile hypertension prevention delivery platform with human coaching. J Hum Hypertens 31(12):795–800
Vo V, Auroy L, Sarradon-Eck A et al (2019) Patients’ perceptions of mHealth apps: meta-ethnographic review of qualitative studies. JMIR mHealth uHealth 7(7):13817
Brewer LC, Hayes SN, Caron AR, Derby DA, Breutzman NS, Wicks A, Raman J, Smith CM, Schaepe KS, Sheets RE et al (2019) Promoting cardiovascular health and wellness among African-Americans: community participatory approach to design an innovative mobile-health intervention. PLoS One 14(8):0218724
Gupta, K., Roy, S., Poonia, R.C., Nayak, S.R., Kumar, R., Alzahrani, K.J., Alnfiai, M.M., Al-Wesabi, F.N.: Evaluating the usability of mHealth applications on type 2 diabetes mellitus using various MCDM methods. In: Healthcare, vol. 10, p. 4 (2021). MDPI
Li J, Zhang C, Li X, Zhang C (2020) Patients’ emotional bonding with mHealth apps: an attachment perspective on patients’ use of mHealth applications. Int J Inf Manag 51:102054
Quelly SB, Norris AE, DiPietro JL (2016) Impact of mobile apps to combat obesity in children and adolescents: a systematic literature review. J Specialists Pediatr Nurs 21(1):5–17
Rubio ÓJ, Trigo JD, Alesanco Á, Serrano L, García J (2016) Analysis of ISO/IEEE 11073 built-in security and its potential IHE-based extensibility. J Biomed Informatics 60:270–285
El-Sappagh S, Ali F, Hendawi A, Jang J-H, Kwak K-S (2019) A mobile health monitoring-and-treatment system based on integration of the SSN sensor ontology and the HL7 FHIR standard. BMC Med Inf Decis Mak 19(1):1–36
Hossain, I., Ang, Y.N., Chng, H.T., Wong, P.S.: Patients’ attitudes towards mobile health in Singapore: a cross-sectional study. Mhealth 5 (2019)
Serlachius A, Schache K, Kieser A, Arroll B, Petrie K, Dalbeth N et al (2019) Association between user engagement of a mobile health app for gout and improvements in self-care behaviors: randomized controlled trial. JMIR mHealth uHealth 7(8):15021
Ashrafi N, Kuilboer JP, Stull T (2018) Semantic interoperability in healthcare: challenges and roadblocks. STPIS@ CAiSE. pp 119–122
Cruz-Ramos, N.A., Alor-Hernández, G., Colombo-Mendoza, L.O., Sánchez-Cervantes, J.L., Rodríguez-Mazahua, L., Guarneros-Nolasco, L.R.: mHealth apps for self-management of cardiovascular diseases: a scoping review. In: Healthcare, vol. 10, p. 322 (2022). MDPI
Ndlovu K, Mars M, Scott RE (2021) Interoperability frameworks linking mHealth applications to electronic record systems. BMC Health Serv Res 21(1):1–10
Paglialonga, A., Patel, A.A., Pinto, E., Mugambi, D., Keshavjee, K.: The healthcare system perspective in mHealth. In: m_Health Current and Future Applications, pp. 127–142. Springer, ??? (2019)
PracticeFusion (2022) EHR vs. EMR: what’s the difference? (https://www.practicefusion.com/blog/ . Online; Accessed 13 April 2022 )
Thangada ND, Garg N, Pandey A, Kumar N (2018) The emerging role of mobile-health applications in the management of hypertension. Curr Cardiol Rep 20(9):1–9
Ndlovu K, Scott RE, Mars M (2021) Interoperability opportunities and challenges in linking mHealth applications and eRecord systems: Botswana as an exemplar. BMC Med Inf Decis Mak 21(1):1–12
Garai, Á., Adamkó, A.: Comprehensive healthcare interoperability framework integrating telemedicine consumer electronics with cloud architecture. In: 2017 IEEE 15th International Symposium on Applied Machine Intelligence and Informatics (SAMI), pp. 000411–000416 (2017). IEEE
Perakis, K., Bouras, T., Ntalaperas, D., Hasapis, P., Georgousopoulos, C., Sahay, R., Beyan, O.D., Potlog, C., Usurelu, D.: Advancing patient record safety and EHR semantic interoperability. In: 2013 IEEE International Conference on Systems, Man, and Cybernetics, pp. 3251–3257 (2013). IEEE
Aamir J, Ali SM, Boulos MNK, Anjum N, Ishaq M (2018) Enablers and inhibitors: a review of the situation regarding mHealth adoption in low-and middle-income countries. Health Policy Technol 7(1):88–97
Cardoso, L., Marins, F., Quintas, C., Portela, F., Santos, M., Abelha, A., Machado, J.: Interoperability in healthcare. In: Health Care Delivery and Clinical Science: Concepts, Methodologies, Tools, and Applications, pp. 689–714. IGI Global, ??? (2018)
Bezerra, C.A.C., Araújo, A.M.C.d., Times, V.C.: An hl7-based middleware for exchanging data and enabling interoperability in healthcare applications. In: 17th International Conference on Information Technology–New Generations (ITNG 2020), pp. 461–467 (2020). Springer
Maxhelaku S, Kika A (2019) Improving interoperability in healthcare using Hl7 Fhir. Proceedings of the 47th International Academic Conference
Gurupur, V.P.: Key observations in terms of management of electronic health records from a mHealth perspective. Mhealth 8 (2022)
Gantayat, S., Misra, A., Panda, B.: A study of incomplete data–a review. In: Proceedings of the International Conference on Frontiers of Intelligent Computing: Theory and Applications (FICTA) 2013, pp. 401–408 (2014). Springer
Grahne G (2009) Incomplete information
Penzenstadler B (2013) What does sustainability mean in and for software engineering. Proceedings of the 1st International Conference on ICT for Sustainability (ICT4S), vol. 94
Chambers DA, Glasgow RE, Stange KC (2013) The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci 8(1):1–11
Pankomera R, van Greunen D (2018) A model for implementing sustainable mHealth applications in a resource-constrained setting: a case of malawi. Electronic J Inf Syst Dev Countries 84(2):12019
Peng Y, Wang H, Fang Q, Xie L, Shu L, Sun W, Liu Q (2020) Effectiveness of mobile applications on medication adherence in adults with chronic diseases: a systematic review and meta-analysis. J Managed Care Specialty Pharm 26(4):550–561
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, Dobbels F, Fargher E, Morrison V, Lewek P et al (2012) A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 73(5):691–705
Lemay J, Waheedi M, Al-Sharqawi S, Bayoud T (2018) Medication adherence in chronic illness: do beliefs about medications play a role? Patient Preference Adherence 12:1687
Fernandez-Lazaro CI, Adams DP, Fernandez-Lazaro D, Garcia-González JM, Caballero-Garcia A, Miron-Canelo JA (2019) Medication adherence and barriers among low-income, uninsured patients with multiple chronic conditions. Res Soc Admin Pharm 15(6):744–753
Vázquez-de Sebastián J, Ciudin A, Castellano-Tejedor C (2021) Analysis of effectiveness and psychological techniques implemented in mHealth solutions for middle-aged and elderly adults with type 2 diabetes: a narrative review of the literature. J Clin Med 10(12):2701
Thomas IF, Lawani AO, James BO (2017) Effect of short message service reminders on clinic attendance among outpatients with psychosis at a psychiatric hospital in Nigeria. Psychiatric Serv 68(1):75–80
Lin, C.-L., Mistry, N., Boneh, J., Li, H., Lazebnik, R.: Text message reminders increase appointment adherence in a pediatric clinic: a randomized controlled trial. Int J Pediatr 2016 (2016)
Attfield, S, Kazai G, Lalmas M, Piwowarski B (2011) Towards a science of user engagement (position paper). WSDM Workshop on User Modelling for Web Applications. pp 9–12
Woldaregay AZ, Issom DZ, Henriksen A, Marttila H, Mikalsen M, Pfuhl G, Sato K, Lovis C, Hartvigsen G (2018) Motivational factors for user engagement with mHealth apps. pHealth. pp 151–157
Birnbaum F, Lewis DM, Rosen R, Ranney ML (2015) Patient engagement and the design of digital health. Acad Emerg Med 22(6):754
Kozak AT, Buscemi J, Hawkins MA, Wang ML, Breland JY, Ross KM, Kommu A (2017) Technology-based interventions for weight management: current randomized controlled trial evidence and future directions. J Behav Med 40(1):99–111
Stephenson A, McDonough SM, Murphy MH, Nugent CD, Mair JL (2017) Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Activity 14(1):1–17
Szinay D, Perski O, Jones A, Chadborn T, Brown J, Naughton F et al (2021) Influences on the uptake of health and well-being apps and curated app portals: think-aloud and interview study. JMIR mHealth uHealth 9(4):27173
Cerrato, P., Halamka, J.: The transformative power of mobile medicine: leveraging innovation, seizing opportunities and overcoming obstacles of mHealth. Academic Press, ??? (2019)
Cechetti NP, Bellei EA, Biduski D, Rodriguez JPM, Roman MK, De Marchi ACB (2019) Developing and implementing a gamification method to improve user engagement: a case study with an m-health application for hypertension monitoring. Telematics Inf 41:126–138
Vaghefi I, Tulu B et al (2019) The continued use of mobile health apps: insights from a longitudinal study. JMIR mHealth uHealth 7(8):12983
Kelders SM, Oinas-Kukkonen H, Oörni A, van Gemert-Pijnen JE (2016) Health behavior change support systems as a research discipline; a viewpoint. Int J Med Inf 96:3–10
Stepanovic, S., Mettler, T.: Gamification applied for health promotion: does it really foster long-term engagement? A scoping review. In: Proceedings of the 26th European Conference on Information Systems, pp. 1–16 (2018). AIS
Alahäivälä T, Oinas-Kukkonen H (2016) Understanding persuasion contexts in health gamification: a systematic analysis of gamified health behavior change support systems literature. Int J Med Informatics 96:62–70
Wang T, Fan L, Zheng X, Wang W, Liang J, An K, Ju M, Lei J et al (2021) The impact of gamification-induced users’ feelings on the continued use of mHealth apps: a structural equation model with the self-determination theory approach. J Med Internet Res 23(8):24546
Tran S, Smith L, El-Den S, Carter S et al (2022) The use of gamification and incentives in mobile health apps to improve medication adherence: scoping review. JMIR mHealth uHealth 10(2):30671
Schmidt-Kraepelin M, Thiebes S, Stepanovic S, Mettler T, Sunyaev A (2019) Gamification in health behavior change support systems-a synthesis of unintended side effects. Proceedings of the 14th International Conference on Wirtschaftsinformatik. pp 1032–1046
Sardi L, Idri A, Fernández-Alemán JL (2017) A systematic review of gamification in e-health. J Biomed Inf 71:31–48
Forman EM, Goldstein SP, Flack D, Evans BC, Manasse SM, Dochat C (2018) Promising technological innovations in cognitive training to treat eating-related behavior. Appetite 124:68–77
Dithmer M, Rasmussen JO, Grönvall E, Spindler H, Hansen J, Nielsen G, Sørensen SB, Dinesen B (2016) “the heart game”: using gamification as part of a telerehabilitation program for heart patients. Games Health J 5(1):27–33
Fleming TM, Bavin L, Stasiak K, Hermansson-Webb E, Merry SN, Cheek C, Lucassen M, Lau HM, Pollmuller B, Hetrick S (2017) Serious games and gamification for mental health: current status and promising directions. Front Psychiatry 7:215
Conway N, Campbell I, Forbes P, Cunningham S, Wake D (2016) mHealth applications for diabetes: user preference and implications for app development. Health Informatics J 22(4):1111–1120
Rolfe DE, Ramsden VR, Banner D, Graham ID (2018) Using qualitative health research methods to improve patient and public involvement and engagement in research. Res Involve Engage 4(1):1–8
Househ M, Grainger R, Petersen C, Bamidis P, Merolli M (2018) Balancing between privacy and patient needs for health information in the age of participatory health and social media: a scoping review. Yearbook Med Informatics 27(01):029–036
Saheb T (2020) An empirical investigation of the adoption of mobile health applications: integrating big data and social media services. Health Technol 10(5):1063–1077
Puspitasari I, Firdauzy A (2019) Characterizing consumer behavior in leveraging social media for e-patient and health-related activities. Int J Environ Res Public Health 16(18):3348
Dicianno BE, Henderson G, Parmanto B (2017) Design of mobile health tools to promote goal achievement in self-management tasks. JMIR mHealth uHealth 5(7):7335
Grady, A., Yoong, S., Sutherland, R., Lee, H., Nathan, N., Wolfenden, L.: Improving the public health impact of eHealth and mHealth interventions. Australian N Zealand J Public Health 42(2) (2018)
Sirois FM, Kitner R, Hirsch JK (2015) Self-compassion, affect, and health-promoting behaviors. Health Psychol 34(6):661
Gedik Z (2019) Self-compassion and health-promoting lifestyle behaviors in college students. Psychol Health Med 24(1):108–114
Holden CL, Rollins P, Gonzalez M (2021) Does how you treat yourself affect your health? the relationship between health-promoting behaviors and self-compassion among a community sample. J Health Psychol 26(12):2330–2341
Terry ML, Leary MR, Mehta S, Henderson K (2013) Self-compassionate reactions to health threats. Personal Soc Psychol Bull 39(7):911–926
Ingolfo, S., Siena, A., Mylopoulos, J.: Establishing regulatory compliance for software requirements. In: International Conference on Conceptual Modeling, pp. 47–61 (2011). Springer
SynopsisInc: Software Standards Compliance mistakes. 2019. https://www.synopsys.com/blogs/software-security/software-standards-compliance/. Online; Accessed 11 Aug 2022
Castellanos Ardila JP, Gallina B, Ul Muram F (2022) Compliance checking of software processes: a systematic literature review. J Softw 34(5):2440
Castellanos-Ardila JP, Gallina B, Governatori G (2021) Compliance-aware engineering process plans: the case of space software engineering processes. Artif Intell Law 29(4):587–627
Usman, M., Felderer, M., Unterkalmsteiner, M., Klotins, E., Mendez, D., Alégroth, E.: Compliance requirements in large-scale software development: an industrial case study. In: International Conference on Product-Focused Software Process Improvement, pp. 385–401 (2020). Springer
Alexander IF (2005) A taxonomy of stakeholders: human roles in system development. Int J Technol Hum Interact (IJTHI) 1(1):23–59
Akhigbe O, Amyot D, Richards G (2019) A systematic literature mapping of goal and non-goal modelling methods for legal and regulatory compliance. Require Eng 24(4):459–481
Fan, M., Yu, L., Chen, S., Zhou, H., Luo, X., Li, S., Liu, Y., Liu, J., Liu, T.: An empirical evaluation of GDPR compliance violations in Android mHealth apps. In: 2020 IEEE 31st International Symposium on Software Reliability Engineering (ISSRE), pp. 253–264 (2020). IEEE
Ologeanu-Taddei R et al (2020) Assessment of mHealth interventions: need for new studies, methods, and guidelines for study designs. JMIR Med Informatics 8(11):21874
Farao J, Malila B, Conrad N, Mutsvangwa T, Rangaka MX, Douglas TS (2020) A user-centred design framework for mHealth. PloS One 15(8):0237910
Perski O, Blandford A, Ubhi HK, West R, Michie S (2017) Smokers’ and drinkers’ choice of smartphone applications and expectations of engagement: a think aloud and interview study. BMC Med Inf Decis Mak 17(1):1–14
Wei Y, Zheng P, Deng H, Wang X, Li X, Fu H et al (2020) Design features for improving mobile health intervention user engagement: systematic review and thematic analysis. J Med Internet Res 22(12):21687
Bhatia A, Matthan R, Khanna T, Balsari S et al (2020) Regulatory sandboxes: a cure for mHealth Pilotitis? J Med Internet Res 22(9):21276
Acknowledgements
Not applicable.
Funding
No external funding secured for the work.
Author information
Authors and Affiliations
Contributions
Bliss Utibe-Abasi Stephen (BUS), Benedicta C. Uzoewulu (BCU), Philip Asuquo (PA), and Simeon Ozuomba (SO). The idea and conceptualization of the study were made by BCU under the guidance of SO. BCU also worked on the approaches to management of diabetes and hypertension, as well as the existing mHealth systems for both diseases. Artificial intelligence in management of both diseases and general challenges with diabetes and hypertension mHealth systems as well as preparation of the manuscript were done by BUS. Expert review of the manuscript and suggestions were made by PA. The final version of the manuscript was approved after evaluation by all listed authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Stephen, B.UA., Uzoewulu, B.C., Asuquo, P.M. et al. Diabetes and hypertension MobileHealth systems: a review of general challenges and advancements. J. Eng. Appl. Sci. 70, 78 (2023). https://doi.org/10.1186/s44147-023-00240-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44147-023-00240-6