Abstract
Background
COVID-19 infection involves a complex interplay of the immunological and inflammatory responses. Low blood-oxygen levels have been a hallmark in COVID-19 patients. The lung tissue damage infiltered by the viral-mediated inflammation decreases oxygen saturation to cause silent hypoxia and cell death. This study aimed to evaluate the association of inflammatory biomarkers with oxygen saturation (SpO2) and mortality in severe COVID-19 patients.
Methods
A total of 190 severe COVID-19 patients were included in this study after confirmed by the RT-PCR assay. The laboratory tests were performed for biochemical assessment. Serum levels of C-reactive protein (CRP), lactate dehydrogenase (LDH), and ferritin were determined and compared between survivors and nonsurvivors using independent sample t-test. The correlation of these inflammatory markers was studied using Spearman’s correlation, and their association with mortality was studied using logistic regression.
Results
All the COVID-19 patients were severe with SpO2< 90% and respiratory rate > 30/min. While the serum levels of CRP, LDH, ferritin, aspartate transaminase (AST), urea, and random blood sugar (RBS) were elevated, hemoglobin (Hb) and SpO2 levels were reduced in COVID-19 patients. LDH and ferritin levels were significantly higher in nonsurvivors compared to survivors with p values of 0.001 and 0.022 respectively. Spearman’s correlation showed a significant correlation of the inflammatory markers with SpO2, serum electrolytes (potassium, chloride), liver enzymes (AST and alanine transaminase (ALT)), and markers of kidney damage (urea, creatinine).
Conclusion
Inflammatory markers could effectively discriminate the risk of mortality in severe COVID-19 patients. As CRP, LDH, and ferritin levels determine the tissue oxygen availability, they seem to be valuable biomarkers in the prognosis of COVID-19.
Similar content being viewed by others
Background
A novel coronavirus, 2019-nCoV, that has been identified to have originated in Wuhan, China, has evolved into a pandemic, and as of today, more than 500 million people have been infected and more than six million have died globally.
COVID-19 inflammation has been linked to disease severity [1]. Accumulative evidence has demonstrated that cytokine storm by immune cells during the cell lysis stage of COVID-19 viral replication raises C-reactive protein (CRP) and lactate dehydrogenase (LDH) levels [2,3,4,5]. It has been demonstrated that the mortality is due to the severe multisystemic end-organ failure as a result of cytokine storm. Hence, measuring the inflammatory markers prove important for prognostication and management of these patients. CRP produced in a liver has been reported to be significantly associated with the higher risks of the COVID-19 infection. The proportion of patients with elevated CRP levels was significantly higher in severe COVID-19 patients than in nonsevere patients and CRP levels in the early stages correlates with the disease severity [6, 7], CRP can act as an early marker of COVID-19 infection and inflammation which could help health workers to enable earlier clinical intervention in high-risk population [8].
Pooled analysis by Henry et al. reported that LDH levels predict COVID-19 severity. Elevated LDH levels associated with 6-fold increase in odds of developing severe covid disease and 16-fold increase in odds of mortality in COVID-19 patients [9]. While fewer studies have reported the predictive role of CRP in COVID-19 mortality, there is a dearth in the study of the association of LDH and ferritin with mortality among severe COVID-19 patients. Hence, we conducted a cohort (survivors-non-survivors) study of ICU-admitted COVID-19 patients to study the association between inflammation and mortality.
Methods
Study design
A cross-sectional study was carried out on severe COVID-19 patients admitted to the tertiary care hospital attached to Kanachur Institute of Medical Sciences, Mangaluru, in January 2022. This study has been approved by the Institutional ethics committee.
Subjects
Sample size was calculated at 95% confidence interval, with a power of 80% based on the study of Szarpac et al. [10] using the formula:
A total of 190 COVID-19 patients were included in the study. SARS-CoV-2 infection was confirmed by the RT-PCR assay conducted in accordance with the standard protocol. All the COVID-19 patients were severe with SpO2 <90% on room air at sea level and respiratory rate >30/min [11]. Patients with cancer; with pre-existing musculoskeletal disease; with chronic diseases of liver, kidney, and heart; with bacterial and non-covid viral infections; and on immunosuppressive drugs for another disease and pregnant and lactating women were excluded.
Samples
In plain vacutainer, 5 ml of venous blood was collected and allowed to clot for 30 min at room temperature and then centrifuged at 2400×g for 10 min to separate serum. The analysis of inflammatory markers (CRP, LDH, ferritin), SpO2, liver markers (AST, ALT, ALP), markers of kidney function (electrolytes, urea, creatinine), and random blood sugar (RBS) was performed.
Methods
Tests for biochemical parameters were performed on the VITROS 5600/XT 7600 Integrated Systems according to the manufacturer’s instructions. CRP was determined based on the principle of the latex agglutination. LDH was determined based on the principle of the enzymatic coupling reaction. LDH catalyzes the conversion of pyruvate and NADH to lactate and NAD+. Oxidation of NADH was monitored by reflectance spectrophotometry, which is used to measure the LDH activity. The ferritin was measured using the principle of immuno-turbidimetry. Agglutination formed due to the reaction between latex-bound ferritin antibodies and the antigen in the sample to form an antigen/antibody complex was measured turbidometrically.
Statistical analysis
SPSS 20.0 (SPSS Inc., Chicago, IL, USA) was utilized for statistical analysis. Values are expressed as mean ± standard deviation. The one-sample t-test was used to determine the significant difference in the mean values of inflammatory markers from reference value. Independent sample t-test was used to compare the values between survivors and nonsurvivors. To know the correlation of these inflammatory markers, Spearman’s correlation was done. To know the association of inflammation with mortality, logistic regression was performed. Receiver operating characteristic (ROC) curves were used to obtain the optimal probability cut-off to predict the mortality. A p value of <0.05 was considered significant.
Results
A total of 190 severe COVID-19 patients were included in this study; 105 patients were males and 85 patients were females. All the COVID-19 patients were severe with SpO2 <90% on room air at sea level. Seventy-five percent (N = 142) of patients were survivors and 25% (N = 48) of patients were nonsurvivors. The mean age of the participants was 53 years. There was no significant difference in age between males and females.
The laboratory findings of the studied patients at the time of diagnosis are presented in Table 1. While the levels of CRP, LDH, ferritin, AST, ALT, urea, RBS, and SBP were elevated, the level of hemoglobin and SpO2 were reduced in COVID-19 patients. The significant differences in the mean values of biochemical parameters between males and females are mentioned in Table 2. Serum ferritin, urea, and creatinine values were significantly higher in male COVID-19 patients than female patients (p < 0.05).
The results of one sample t test showed the levels of LDH, CRP, and ferritin to be significantly higher than the population mean with p value less than 0.001 (Table 3). LDH and ferritin levels were significantly higher in nonsurvivors compared to survivors with p values of 0.001 and 0.022 respectively (Table 4). There was no significant difference in CRP between the two groups. Other parameters that were significantly higher in nonsurvivors compared to survivors were potassium, urea, and creatinine (Table 4).
Spearman’s correlation showed a significant correlation of the inflammatory markers with each other and with serum electrolytes such as potassium and chloride, liver enzymes such as AST and ALT, markers of kidney damage such as serum urea and creatinine, and SpO2 (Table 5). Ferritin also showed a positive correlation with ALP. While there was no correlation of CRP with SpO2, LDH and ferritin showed negative correlation with SpO2 (Table 5).
Further evaluation of the association between inflammatory markers (CRP, LDH, and ferritin) and COVID-19 mortality was performed by Logistic Regression Analysis. CRP had OR of 1.005 (95% CI= 1.002–1.008, p < 0.002). LDH had OR of 1.004 (95% CI= 1.002–1.006, p < 0.001). Ferritin had OR of 1.001 (95% CI = 1–1.001, p = 0.028) (Table 6).
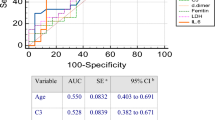
The role of inflammatory markers in predicting the COVID-19 mortality was evaluated using the ROC curve. Survivors were considered negative and severe patients as positive. The area under the ROC curve (ROC-AUC) was assessed (Fig. 1).
COVID-19 mortality was assessed by ROC curve analysis. The ROC-AUC for CRP, LDH, and ferritin were 0.610, 0.748, and 0.709 respectively. LDH and ferritin are the sensitive predictors of COVID-19 mortality (Fig. 1, Table 7).
Discussion
This study provided the baseline laboratory characteristics of severe COVID-19 patients. Twenty-five percent of the severe cases were nonsurvivors. While there was an increase in the levels of inflammatory markers in all severe COVID-19 patients, they were significantly higher in nonsurvivors compared to survivors. Several studies have been conducted to ascertain the relationship between inflammatory markers and the overall outcome of patients with COVID-19 disease. Alroomi showed that ferritin independently predicts in-hospital mortality in Kuwaiti population [12]. A retrospective study of Huang using a large sample size of 1751 Chinese patients showed that LDH associated with higher mortality risk [13]. In contrast, the meta-analysis of Martha concluded that LDH was associated with poor prognosis in COVID-19 patients [14]. Ahmeidi showed that elevation in serum inflammatory marker CRP may be indicative of COVID-19 infection severity and mortality and suggested that these parameters may predict COVID-19 severity [15]. However, their study was limited by inadequate sample size and study design. Yet in another study, El-Shabrawy showed that CRP/albumin ratio predicted 30-day mortality in COVID-19 patients [16].
This study showed that COVID-19 male patients had significantly higher values of ferritin, urea, and creatinine compared to female counterparts. Previously, Gandini showed that higher ferritin levels in males could predict worse outcome in male patients [17]. This is contradictory to the study of Chen, where female COVID-19 patients had significantly higher ferritin levels than male counterparts [18]. Further, a retrospective analysis of 12,413 COVID-19 patients showed that serum creatinine and blood urea nitrogen (BUN) levels are higher in males than females [19].
In the current study, SpO2 was reduced in COVID-19 patients and showed a negative correlation with LDH and ferritin. Though no previous studies reported the correlation of ferritin with SpO2, Poggiali et al. revealed by retrospective observation study that CRP (r = 0.55, p value < 0.0001) and LDH (r = 0.62, p value < 0.0001) showed strong inverse correlation with the respiratory performance (PaO2/FiO2) [20]. Significant elevation of potassium, urea, and creatinine levels in severe COVID-19 nonsurvivors compared to survivors who had normal levels of urea and creatinine, positive correlation of LDH and ferritin with urea and creatinine levels, and positive correlation of LDH with serum potassium levels are indicative of inflammation-mediated renal failure among nonsurvivors. This is in line with the study of Ng et al. among hospitalized COVID-19 patients, which showed higher rate of mortality among patients with end-stage kidney disease than those without this disease [21].
The ROC analysis shows LDH and ferritin can be predictors of mortality in severe COVID-19 patients. Despite showing strong correlation with LDH and ferritin, ROC analysis could not infer the predictive role of CRP in COVID-19 mortality.
The current study had some limitations. The study is a single-center study and used cohort study design without controls and nonsevere patients. Multi-center study with larger sample size must be done including controls. In addition to LDH, CRP, and ferritin, other inflammatory markers such as interleukin-6 (IL-6) and procalcitonin could be correlated with disease severity to predict COVID-19 mortality [22, 23]. Integration of neutrophil/lymphocyte (N/L) ratio and CRP may lead to improved prediction [24], which needs to be addressed in future studies. Intravenous heparin administration in severe COVID-19 patients was done as a line of management to prevent mortality. However, further studies correlating lines of management with the clinical data of ventilated patients are warranted.
COVID-19 infection is accompanied by vigorous immune and inflammatory response that causes severe lung damage to limit the entry of oxygen to the bloodstream, resulting in long-term breathlessness and severe complications including renal failure. Inflammatory markers (ferritin/LDH) could be useful as a predictor for COVID-19 mortality and respiratory failure and could help the physicians to discern at-risk COVID-19 patients to facilitate early treatment. Elevated LDH increases the odds of severe COVID-19 disease and mortality among ICU-admitted patients.
Conclusion
LDH and ferritin can predict mortality in severe COVID-19 patients. Special attention to elevated levels of these inflammatory markers will enable better management.
Abbreviations
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- AUC:
-
Area under the curve
- CRP:
-
C-reactive protein
- Hb:
-
Hemoglobin
- ICU:
-
Intense care unit
- IL-6:
-
Interleukin-6
- LDH:
-
Lactate dehydrogenase
- N/L:
-
Neutrophils/lymphocytes
- RBS:
-
Random blood sugar
- ROC:
-
Receiver operating characteristic
- SpO2 :
-
Oxygen saturation
References
Weiss P, Murdoch DR (2020) Clinical course and mortality risk of severe COVID-19. Lancet 395(10229):1014–1015
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 395(10229):1033–1034
Stebbing J, Phelan A, Griffin I, Tucker C, Oechsle O, Smith D et al (2020) COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect Dis 20(4):400–402
Tay MZ, Poh CM, Renia L, MacAry PA, Ng LFP (2020) The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol 20(6):363–374
Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H et al (2019) Clinical characteristics of refractory coronavirus disease 2019 in Wuhan, China. Clin Infect Dis 73(11):e4208–e4213
Tan C, Huang Y, Shi F, Tan K, Ma Q, Chen Y et al (2020) C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol 92(7):856–862
Luo X, Zhou W, Yan X, Guo T, Wang B, Xia H et al (2020) Prognostic value of C-reactive protein in patients with coronavirus 2019. Clin Infect Dis 71(16):2174–2179
Ali N (2020) Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J Med Virol 92(11):2409–2411
Henry BM, Aggarwal G, Wong J, Benoit S, Vikse J, Plebani M et al (2020) Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis. Am J Emerg Med 38(9):1722–1726
Szarpak L, Ruetzler K, Safiejko K, Hampel M, Pruc M, Kanczuga-Koda L et al (2021) Lactate dehydrogenase level as a COVID-19 severity marker. Am J Emerg Med 45:638–639
Clinical guidance for management of adult COVID-19 patients. AIIMS/ ICMR-COVID-19 National Task Force/Joint Monitoring Group(Dte.GHS) Ministry of Health & Family Welfare, Government of India. Revised on 14/01/2022. Available from: https://www.mohfw.gov.in/pdf/ClinicalGuidanceforManagementofAdultCovid19Patientsupdatedason17thJanuary2022.pdf.
Alroomi M, Rajan R, Omar AA, Alsaber A, Pan J, Fatemi M et al (2021) Ferritin level: a predictor of severity and mortality in hospitalized COVID-19 patients. Immun Inflamm Dis. 9(4):1648–1655
Huang Y, Guo L, Chen J, Wu M, Zhang C, Liu Z et al (2022) Serum lactate dehydrogenase level as a prognostic factor for COVID-19: a retrospective study based on a large sample size. Front Med (Lausanne). 4(8):671667
Martha JW, Wibowo A, Pranata R (2022) Prognostic value of elevated lactate dehydrogenase in patients with COVID-19: a systematic review and meta-analysis. Postgraduate Medical Journal. 98:422–427
Ahmeidi AA, Musa A, Ahmed HS, Elahmar AA, Goota RB, Ahmed IA et al (2020) Inflammatory markers as predictors of mortality in COVID-19 infection. Afr J Lab Med 9:a1298
El-Shabrawy M, Alsadik ME, El-Shafei M, Abdelmoaty AA, Alazzouni AS, Esawy MM et al (2021) Interleukin-6 and C-reactive protein/albumin ratio as predictors of COVID-19 severity and mortality. Egypt J Bronchol 15(1):5
Gandini O, Criniti A, Gagliardi MC, Ballesio L, Giglio S, Balena A et al (2021) Sex-disaggregated data confirm serum ferritin as an independent predictor of disease severity both in male and female COVID-19 patients. J Infect 82(3):414–451
Chen J, He ZX, Fk W (2022) Evaluation of ferritin level in COVID-19 patients and its inflammatory response. Appl Nanosci. https://doi.org/10.1007/s13204-021-02115-9
Liu YM, Xie J, Chen MM, Zhang X, Cheng X, Li H et al (2021) Kidney function indicators predict adverse outcomes of COVID-19. Med (N Y) 2(1):38–48.e2
Poggiali E, Zaino D, Immovilli P, Rovero L, Losi G, Dacrema A et al (2020) Lactate dehydrogenase and C-reactive protein as predictors of respiratory failure in CoVID-19 patients. Clin Chim Acta 509:135–138
Ng JH, Hirsch JS, Wanchoo R, Sachdeva M, Sakhiya V, Hong S et al (2020) Outcomes of patients with end-stage kidney disease hospitalized with COVID-19. Kidney Int 98:1530–1539
Liu X, Wang H, Shi S, Xiao J (2021) Association between IL-6 and severe disease and mortality in COVID-19 disease: a systematic review and meta-analysis. Postgrad Med J. https://doi.org/10.1136/postgradmedj-2021-139939
Feng T, James A, Doumlele K, White S, Twardzik W, Zahid K et al (2021) Procalcitonin levels in COVID-19 patients are strongly associated with mortality and ICU acceptance in an underserved, inner city population. Medicina (Kaunas) 57(10):1070
Mousavi-Nasab SD, Mardani R, Nasr Azadani H, Zali F, Ahmadi Vasmehjani A, Sabeti S et al (2020) Neutrophil to lymphocyte ratio and C-reactive protein level as prognostic markers in mild versus severe COVID-19 patients. Gastroenterol Hepatol Bed Bench 13(4):361–366
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ND: conception, data acquisition, manuscript writing. SS: design of the work, data acquisition, analysis, interpretation of data. MBV: data collection, manuscript review. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional ethical committee clearance was obtained for the study (Ref No.: KIMS/IEC/A001/2022). The subject’s participation was confirmed by collecting informed written consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Devang, N., Sreelatha, S. & B. V., M. Assessment of inflammatory markers and their association with disease mortality in severe COVID-19 patients of tertiary care hospital in South India. Egypt J Bronchol 16, 55 (2022). https://doi.org/10.1186/s43168-022-00159-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-022-00159-1