Abstract
Background
Lower respiratory tract infections are the leading cause of death in children globally and are transmitted by inhaling airborne droplets. The study demonstrated the prevalence of lower respiratory tract infections in children admitted to the Women and Children Hospital Bannu from February through November 2019. The cross-sectional study was conducted by obtaining indoor data from the official record maintained in the children’s wards.
Results
Males accounted for 649 (61.6%) and females 405 (38.4%) cases out of 1054 cases of the disease. Age group of ≤ 6 months showed 36.2% prevalence, followed by > 6 m ≤ 1 y (25.6%), > 1 y ≤ 2 y (17.1%), > 2 y ≤ 5 y (14.3%), > 5 ≤ 10 y (6.0%), and > 10 y ≤ 15 y (0.8%). Pediatric patients of age ≤ 2 y and ≤ 5 y contributed 78.9% and 93.3% to overall disease, respectively. The disease was at its peak in February (17.9%) while lowest in May (5.5%). The age group (≤ 6 m) was the dominant group in all months except August when replaced by the age group (> 6 m ≤ 1 y). The disease revealed higher prevalence during February-April and October-November.
Conclusions
Different age groups showed variation in the prevalence of the disease with an age group of ≤ 5 y contributing the largest share and seasonal peaks in the disease occurred. The present findings help in adopting strategies for effective control of the disease in different age groups of the children for their peak season.
Similar content being viewed by others
Background
Lower respiratory tract infections (LRTIs) include bronchitis, bronchiolitis, lung abscess, tuberculosis, and pneumonia [24]. Many LRTIs are viral [16, 24] and contagious, but some are bacterial in origin [21]. LRTIs are symptomized with coughing, fatigue, tight feeling in the chest, shortness of breath or breathlessness, weakness, and fever [1] and are the leading cause of death among all infections globally [15, 23]. Viral infection accounted for up to 90% of all LRTIs infection in younger children [20]. LRTIs accounted for about 11.9 million of young children hospitalized worldwide [9, 14] and are an important cause of death in children of age < 2 years [2, 5, 8] while acute lower respiratory tract infections (ALRIs) in children < 5 years of age [7, 13]. LRTIs contributed 6.8% of deaths in neonates, 20% of deaths in children aged 1–12 months, and 12% of deaths in children aged 1–4 years [9, 21].
Pneumonia and bronchiolitis/bronchitis are the most common LRTIs in children with symptoms including coughs and an increased respiratory rate [6]. Pneumonia causes the alveoli in the lung to fill with fluid or pus. Pneumonia contributed the largest share in the mortality in the children aged < 5 years globally [11]. Bronchitis is the swelling or inflammation of the bronchial tubes [3]. Seasonal influenza affects both the upper and lower respiratory tracts [15].
It is estimated that about 20 to 30% of all deaths of children under 5 years of age are because of respiratory infections in Pakistan [12, 18]. Pneumonia in children is the second highest contributor to childhood morbidity and mortality in all ethnic groups in Pakistan [10]. The present study was undertaken to determine the demographic prevalence of lower respiratory tract infections in the children (age ≤ 15 y) of the District Bannu and adjoining areas and is the first of its kind to deal with the age- and sex-wise prevalence of the LRTIs in the children in Khyber Pakhtunkhwa. The current finding will contribute to the policymakers in their future planning of healthcare policies and in adopting preventive measures.
Methods
Study population and the outpatient diagnosis
The study includes those children up to 15 years of age who visited the outpatient department (OPDs) of Women and Children Hospital, Bannu, from February through November 2019 and was admitted to the children’s wards. The present study reported 1054 pediatrics patients suffered (Table 1) from lRTIs including males 649 (61.6%) and females 405 (38.4%). A child was considered to have LRTI based on the symptoms and signs including coughing, fatigue, tight feeling in the chest, shortness of breath or breathlessness, wheezing, weakness, and fever and was recommended to be admitted to the children’s wards. The patients were not further diagnosed to determine the type of LRTIs such as pneumonia or tuberculosis, and the data showed only sex- and age-wise prevalence of LRTIs. The personal information of the indoor patients was recorded in the official registers maintained by the ward in-charge. Demographic data (age and gender) were collected. The study protocol was approved by the Ethical Committee of the said hospital. The inclusion criteria for the study population were as follows: (1) children of age ≤ 15 y and (2) children with the sign or symptoms/infections of LRTI.
Collection of in-patient data and its management
The in-patient data were collected from the official record in the unconsolidated form of data of children’s wards. I prepared the consolidated report for each month for the study period and classify the data into six age groups of children: ≤ 6 m, > 6 m ≤ 1 y, > 1 y ≤ 2 y, > 2 y ≤ 5 y, > 5 ≤ 10 y, and > 10 y ≤ 15 y.
Statistical analysis
Pearson’s chi-squared tests and Fisher’s exact tests (a = 0.05) were used to analyze the data, followed by pairwise comparisons post hoc test.
Results
Statistical analysis result
The chi-squared tests (χχ = 15.215, df = 9, p-value = 0.0852) showed gender by months was not significant. The chi-squared tests for age by months (χ2 = 59.942, df = 36, p-value = 0.00737) were significant. Post hoc pairwise multiple comparisons were adjusted with the Benjamini and Hochberg [4] “BH” method with a = 0.01.
Month-wise/seasonal-based prevalence of lower respiratory tract infections (LRTIs)
Out of 1054 pediatric patients who suffered from lRTIs, 649 (61.6%) were males and 405 (38.4%) were females (Table 1), demonstrating monthly/seasonal variation in the prevalence of the disease. Overall, the disease showed the highest prevalence in February (17.9%) and a consistent decrease in prevalence from February through May (up to 5.5%). The disease indicated low prevalence during May through September: ≤ 7.1% (Table 1) because of the increase in temperature from spring through summer. However, LRTIs once again increased from October through November (15.8%). Therefore, the study demonstrated that autumn through spring showed a higher prevalence of the LRTIs than the summer because of the comparatively low temperature (Table 1).
Gender-based prevalence of LRTIs
The male children showed a higher prevalence of overall LRTIs than female children in all months except September of the study period (Table 1).
Age-based prevalence of LRTIs
Age groups play an important role in the overall prevalence of the LRTIs in children as the percentage prevalence of the disease steadily decreased when age shifted from ≤ 6 months toward > 10 y ≤ 15 y (Table 1): the age group (≤ 6 months) showed 36.2%, while the age group (> 10 y ≤ 15 y) showed 0.8% prevalence of LRTIs.
Age groups based month wise/seasonal comparison of the prevalence of LRTIs
Generally, age groups showed a higher prevalence of LRTIs from February through April and during October-November compared to during May-September (Table 1). The age group (≤ 6 m) was the dominant group among all the age groups for all the months except August (Table 1, Fig. 1), which demonstrated that children of age ≤ 6 m are more vulnerable to the disease than other age groups. Age group (≤ 6 m) showed the highest prevalence of 77 cases (40.7%) in February (Table 1), followed by November (64 cases: 38.3%) and the lowest prevalence in August (12 cases: 18.8%), while age group (> 6 m ≤ 1 y) was the dominant group only in August (19 cases: 29.7%) among all the age groups (Table 1, Fig. 1) and revealed the highest prevalence of 50 cases (29.9%) in November (Table 1). Both the age groups (> 1 y ≤ 2 y and > 2 y ≤ 5 y) showed the highest prevalence in February (> 13%) and the age group (> 5 ≤ 10 y: 10.4%) in October (Table 1). Thus, the disease was more prevailed in the early winter through late spring in children because may be of the lower/comparatively lower temperature than summer (Table 1).
Age group (≤ 6 m) contributed month-wise highest prevalence of LRTIs, followed by age group (> 6 m ≤ 1y), age group (> 1 y ≤ 2 y), and age group (> 2 y ≤ 5 y) from February through May (except, > 2 y ≤ 5 y, in May) and from July through September (except, ≤ 6 m, in August) and in November (Fig. 1).
Discussion
Literature on the epidemiology of respiratory diseases in Pakistan is not updated and not well documented [22]. Epidemiological studies on the LRTI generally in Pakistan and particularly in Khyber Pakhtunkhwa are not sufficiently available, and most of these studies are related to molecular epidemiology (viral etiology). Moreover, literature on the age- and sex-wise prevalence/demographic data of LRTIs in children is scarce in Pakistan and is not available in Khyber Pakhtunkhwa.
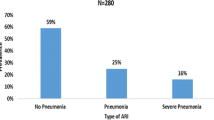
The study reported 1054 patients of LRTIs including 61.6% were males and 38.4% were female children and revealed 61.9% prevalence of LRTIs in children aged ≤ 1 year and 31.4% in aged > 1 y ≤ 5 y were supported by Munir who investigated 840 paediatric patients (2 months up to 5 years) with ARTIs including 539 (64.2%) were male and 301 (35.8%) were female and found 497 (59.16%) patients were of age 2 months to < 12 months and 343 (40.83%) were of age 12 months to 59 months [25].
The higher prevalence of LRTIs in males (61.6%) was also supported by Sultana et al. [22], who reported 1008 patients with respiratory problems including 594 (58.9%) were males and 414 (41.1%) were females and found overall 16 types of respiratory diseases in the patients: tuberculosis accounted for 29.66%, followed by asthma (28.08%) and chronic obstructive pulmonary disease (11.31%). The age group 51–60 years contributed the highest (21.13 %) of the patients, followed by 41–50 years (17.66 %) and 61–70 years (14.19%), and minimum patients (3.08 %) in the age group of 1–10 years. Children are more susceptible to influenza and other LRTIs than adults because of their less developed immune systems, and their intense social mixing patterns probably enhance transmission.
Mirkarimi et al. [17] found 59.4% out of 303 were males hospitalized children including infants suffered from LRTI (pneumonia and bronchitis were the most common LRTIs) in Abuzar Hospital (Iran) during 1 year. Their age ranges 1 month to 15 years and found the highest number of patients were of age < 1 year (50.8%, n = 154).
Nizami et al. [19] found 5884 children with ARTIs including 1097 children who had pneumonia and severe pneumonia with 82.1/1,000 children per year for pneumonia. They isolated Haemophilus influenzae, Streptococcus pneumoniae, and Klebsiella pneumoniae 10.9%, 3.7%, and 8.5% of oropharyngeal swabs, respectively, and estimated the total number of cases of pneumonia to be 213,116 per year due to H. influenzae and 71,864 per year due to S. pneumoniae in children aged < 5 years in Pakistan.
The present study contributes to adopting timely strategies both age-wise and month-wise for effective prevention as well as control of LRTIs in children in the study area. Furthermore, the study also helps in the immunization of children timely and properly. Nevertheless, the present study is limited as the study did not describe the etiology of the LRTIs. Further research is needed to know the causes of LRTIs (viral or bacterial) as well as LRTIs diagnosed into different types, i.e., bronchitis, bronchiolitis, tuberculosis, and pneumonia, and their prevalence rate in children in the study area.
Bottle and formula feeding is the major risk factor responsible for the 78.9% of LRTIs in infants and babies aged ≤ 2 years in the present study. The unhygienic conditions of feeding children play a key role in the spread of the disease in the study area.
Conclusions
Male children and the age group (≤ 6 months) remained the dominant group contributed 649 (61.6%) cases and 36.2% prevalence of lower respiratory tract infections (LRTIs) in the District Bannu, respectively, followed by age group > 6 m ≤ 1 y (25.6%), > 1 y ≤ 2 y (17.1%), > 2 y ≤ 5 y (14.3%), > 5 ≤ 10 y (6.0%), and > 10 y ≤ 15 y (0.8%). Children of age ≤ 5 y contributed 93.3% to the overall disease. The highest prevalence of the LRTIs was observed in February (17.9%), while the lowest was in May (5.5%). A gradual reduction in the overall percentage prevalence occurred when age shifted from ≤ 6 m toward > 10 y ≤ 15 y. All the age groups showed a higher prevalence of the LRTIs in children during late winter through spring and autumn through early winter, while the age groups (≤ 6 m, > 6 m ≤ 1 y, > 1 y ≤ 2 y, > 2 y ≤ 5 y) showed a higher prevalence from February through May (except, > 2 y ≤ 5 y, in May) and from July through September and in November. The study helps promote health in the study area by the adoption of preventive and control measures against LRTIs.
Recommendations
It is recommended that the mother should have (1) proper breastfeeding up to 2 years because 78.9% of children suffering from LRTIs are of age ≤ 2 years and (2) should have regularly attended a child care facility for regular checkups/immunization and treatment.
Availability of data and materials
All data generated or analyzed during this study are included in the tables of this manuscript.
Abbreviations
- LRTs:
-
Lower respiratory tract infection
- ALRIs:
-
Acute lower respiratory tract infections
- RSV:
-
Respiratory syncytial virus
- GBD:
-
Global burden of disease
- OPDs:
-
Outpatient departments
- BH:
-
Benjamini and Hochberg
- NPS:
-
Nasopharyngeal swabs
- RV:
-
Rhinovirus
- MP:
-
Mycoplasma
References
Antibiotic Expert Group (2014) Therapeutic Guidelines: Antibiotic, 15th. edn Therapeutic Guidelines Limited. ISBN 9780992527211
Bartlett AV, Bocaletti PME, Bocaletti MA (1991) Neonatal morbidity and mortality in a rural Guatemalan community: the importance of infectious diseases and their management. Pediatr Infect Dis J 10:752–757
Becker LA, Hom J, Villasis-Keever M, van der Wouden JC (2015) Beta2-agonists for acute cough or a clinical diagnosis of acute bronchitis. Cochrane Database Syst Rev 9:CD001726. https://doi.org/10.1002/14651858.CD001726.pub5
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soci: Ser B 57(1):289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x
Berman S (1991) Epidemiology of acute respiratory infections in children in developing countries. Pediatr Infect Dis J 13:S454–S462
Boloursaz MR, Lotfian F, Aghahosseini F, Cheraghvandi A, Khalilzadeh S, Farjah A, Boloursaz M (2013) Epidemiology of lower respiratory tract infections in children. J Compr Ped 4(2):93–98
Claassen-Weitz S, Lim KYL, Mullally C, Zar HJ, Nicol MP (2021) The association between bacteria colonizing the upper respiratory tract and lower respiratory tract infection in young children: a systematic review and meta-analysis. Clin Microbiol Infect 7:S1198–S743X (21)00282-2
Erling V, Jalil F, Hanson LA, Zaman S (1999) The impact of climate on the prevalence of respiratory tract infections in early childhood in Lahore, Pakistan. J Public Health Med 21(3):331–339
Gul A, Khan S, Arshad M, Anjum SI, Attaullah S, Ali I, Rauf A, Arshad A, Alghanem SM, Khan SN (2020) Peripheral blood T cells response in human parainfluenza virus-associated lower respiratory tract infection in children. Saud J of Biolog Sci 27:2847–2852
Hussain R, Lobo MA, Inam B, Khan A, Qureshi AF, Marsh D (1997) Pneumonia perceptions and management: an ethnographic study in urban squatter settlements of Karachi, Pakistan. Soc Sci Med 45(7):991–1004
Ketenci A, Gochicoa-Rangel L, Yılmaz Ö (2022) Pneumonia in Children. In: Cingi C, Arısoy ES, Bayar MN (eds) Pediatric ENT Infections. Springer, Cham. https://doi.org/10.1007/978-3-030-80691-0_79
Khan TA, Madni SA, Zaidi AK (2004) Acute respiratory infections in Pakistan: have we made any progress? J Coll Physicians Surg Pak 14(7):440–448
Kini S, Kalal BS, Chandy S, Shamsundar R, Shet A (2019) Prevalence of respiratory syncytial virus infection among children hospitalized with acute lower respiratory tract infections in Southern India. World J Clin Pediatr 8(2):33–42
Korsun N, Angelova S, Trifonova I, Georgieva I, Voleva S, Tzotcheva I (2019) Viral pathogens associated with acute lower respiratory tract infections in children younger than 5 years of age in Bulgaria. Braz J Microbiol 50:117–125
Kumar U, Singh BB (2019) Clinical evaluation of prevalence of respiratory tract infection in children from Bihar region. Inter Med Heal Res 5(5):144–148
Meissner HC (2016) Viral bronchiolitis in children. N Engl J Med 374:62–72
Mirkarimi M, Alisamir M, Saraf S, Heidari S, Barouti S, Mohammadi S (2020) Clinical and epidemiological determinants of lower respiratory tract infections in hospitalized pediatric patients. Int J Pediatr 8844420. https://doi.org/10.1155/2020/8844420
Naz R, Gul A, Javed U, Urooj A, Amin S, Fatima Z (2019) Etiology of acute viral respiratory infections common in Pakistan: a review. Rev Med Virol 29:e2024
Nizami SQ, Bhutta ZA, Hasan R (2006) Incidence of acute respiratory infections in children 2 months to 5 years of age in periurban communities in Karachi, Pakistan. J Pakis Med Associ 56(4):163–167
Pattemore PK, Jennings LC. (2008) Epidemiology of respiratory infections. Pedia Respir Medic :435–452. doi: https://doi.org/10.1016/B978-032304048-8.50035-9.
Sonawane AA, Shastri J, Bavdekar SB (2019) Respiratory pathogens in infants diagnosed with acute lower respiratory tract infection in a tertiary care hospital of western India using multiplex real-time PCR. Indian J Pediatr 86(5):433–438
Sultana T, Afzal A, Sultana S, Al-Ghanim K, Shahid T, Jabeen Z et al (2017) Epidemiological estimates of respiratory diseases in the hospital population, Faisalabad, Pakistan. Braz Arch Biol Technol 60:e17160358
Tchatchouang S, Nzouankeu A, Kenmoe S, Ngando L, Penlap V, Fonkoua M-C, Pefura-Yone E-W, Njouom R (2019) Bacterial aetiologies of lower respiratory tract infections among adults in Yaoundé, Cameroon. BioMed Resea Int 2019:4834396
Yang L, Zhang G, Huang L, Ren X, Su Y, Wang C et al (2021) The effect of recombinant human interferon a1b treatment of infants hospitalized with lower respiratory tract infection on subsequent wheezing. J Pediatr (Rio J) 97(6):617–622
Munir S (2009) Acute Respiratory Infection among Children aged 2 Month to 5 Years: Do Children with Initially “No Pneumonia” Progress to Pneumonia?. Ann Pak Inst Med Sci 5(3):154-157
Acknowledgements
I am highly grateful to the then additional director Aman Uallh of the Women and Children Hospital, Bannu, for his permission to obtain the research data and for granting me ethical approval of the study. I am also grateful to Mr. Shafiq-ur-Rehman, in charge (children ward), for his assistance in obtaining the data. Thanks also to Jos Feys, a senior research fellow at the KU Leuven University (Catholic University of Leuven, Belgium), for statistically analyzing the data.
Funding
None.
Author information
Authors and Affiliations
Contributions
I am the sole author of this manuscript and contributed to the study conception and design, material preparation, data collection, data management, and interpretation. The author(s) read and approved the final manuscript.
Author information
I am Dr. Muhammad Ashraf Khan with Ph.D. in Environmental Sciences from the University of Peshawar, and serving as a senior subject specialist (Biology) at the Elementary and Secondary Education Department, Khyber Pakhtunkhwa, Pakistan.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research study has been ethically approved by the medical director of the Women and Children Hospital Bannu with reference no. 1221, dated 07 November 2020. I have willingly participated in the study.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khan, M.A. Epidemiological studies on lower respiratory tract infection in children in the District Bannu, Khyber Pakhtunkhwa, Pakistan. Egypt J Bronchol 16, 17 (2022). https://doi.org/10.1186/s43168-022-00119-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-022-00119-9