Abstract
Background
Chronic suppurative otitis media is a major cause of hearing impairment and morbidity in poor socioeconomic developing countries.
Objectives
To determine the prevalence of chronic suppurative otitis media in a tertiary care hospital and to analyze its clinico-bacteriological aspects.
Methods
This is a cross-sectional, descriptive and analytical study conducted at the ENT and Head and Neck Surgery Department in the Renaissance University Hospital in N'Djamena, Chad. All the patients that were diagnosed with chronic suppurative otitis media from 1 January 2017 to 31 December 2019 were included.
Results
The hospital prevalence was 6.1%. The sex ratio (male/female) was 1.09. The median age of patients was 28 years with [1 to 74 years]. The median time from the onset of otorrhea to coming for medical consultation was 6 years with [4 months to 42 years]. The main symptom associated with otorrhea was hearing impairment which was in 55.6% of cases (n = 50). Perforations ≥ ¾ of the tympanic membrane surface were noted in 51.3% of cases (n = 60). The tympanic cavity floor was erythematous in 49.6% of cases (n = 58) and erythematous with a discharge in 42.7% of cases (n = 50). There was an association between the size of the perforation and the appearance of the tympanic mucosa (p = 0.003), and between the age of the disease and the side of the ear affected with chronic suppurative otitis media (p = 0.016). The culture positivity rate was 86.1% (n = 31) and with two other microbial cases. Staphylococcus aureus was isolated in 28.1% of cases (n = 9) followed by Pseudomonas aeruginosa which was 25% of the cases (n = 8).
Conclusion
Chronic suppurative otitis media affects both children and adults. Delay in medical consultation to the ENT department is relatively high. Staphylococcus aureus and Pseudomonas aeruginosa are the most common causes.
Similar content being viewed by others
Background
Chronic suppurative otitis media (CSOM) is one of the most common childhood diseases, affecting between 65 to 330 million people worldwide, mainly in poor socioeconomic developing countries [1]. The prevalence of CSOM in sub-Saharan African countries ranges from 0.4% to 4.2% [2]. It is a major cause of acquired hearing loss and morbidity in these countries [3, 4].
CSOM is an infection characterized clinically by recurrent middle ear discharge through a persistent perforation of the tympanic membrane more than three months [5, 6]. If not treated early and appropriately, the size of the tympanic perforation may increase over time and destruction of the ossicular chain ensues with a change in the tympanic mucosa. The evolution of such a situation leads to worsening deafness and often fatal intracranial complications.
In the literature, there are many causative agents for CSOM, but Pseudomonas aeruginosa and Staphylococcus aureus are the most common [3, 4, 6,7,8]. The medical management of CSOM is usually empirical based on topical antibiotics such as ciprofloxacin, ofloxacin, or rifampicin in combination with systemic antibiotics (ciprofloxacin, levofloxacin, amoxicillin/clavulanic acid, ceftazidime). Antibiotics can be used alone or in addition to other treatments for CSOM such as antiseptics or ear cleaning [9]. Excessive and inappropriate use of antibiotics is a source of increased antibiotic resistance of pathogens causing CSOM.
In our context, marked by the insufficiency of ENT departments and a low socioeconomic level of the population, access to appropriate and timely care for the disease poses enormous difficulties. To our knowledge, as to date, no study on chronic suppurative otitis media has been conducted in Chad. The objectives of the present study were to determine the prevalence of CSOM and to analyze its clinical and bacteriological aspects in one of the country's university hospital centers.
Methods
This was a cross-sectional, descriptive and analytical study conducted at the ENT and Head and Neck Surgery Department of the Renaissance University Hospital in N'Djamena, Chad. All patients of any age and sex who were seen for chronic suppurative otitis media (more than three months old) from 1 January 2017 to 31 December 2019 were included in the study. A total of 90 patients were seen, 27 of whom had bilateral CSOM. This gives a total of 117 ears for the study. Patients with acute recurrent otitis media (tympanic membrane returning to normal between each episode) as well as those with cholesteatomatous otitis media were excluded.
A bacteriological sample was taken from any patient with otorrhoea who had not been on any antibiotics (oral and systemic) for the previous 7 days. Patients received with ongoing antibiotic treatment were not sampled. A total of 36 ear swabs were taken. Two thin swabs were used after cleaning the external auditory canal with isotonic saline solution. The first swab was used for direct reading and the second for culture. The collected samples were sent directly to the microbiology laboratory for further processing. The swabs were inoculated onto blood agar and the inoculated plates were incubated at 37 °C ± 2 for 12–24 h. These plates were then placed in the Vitek® machine for germ identification and antibiotic susceptibility testing.
Data was collected on pre-established forms including epidemiological parameters (age, sex), medical history of patients (acute otitis media, seromucous otitis, ear trauma, nasopharyngitis), clinical data (duration of disease, symptoms, side of the ear affected, site and size of tympanic perforation, appearance of the tympanic cavity mucosa) and bacteriological data. Perforations > ¾ of the tympanic membrane surface are termed subtotal perforations; those = ¾ of the tympanic membrane are termed large perforations. When the tympanic perforation occupies half of the surface, it is said to be a medium perforation. When it involves a quarter, it is considered a small perforation.
The data were analyzed with SPSS version 26.0. Qualitative data was presented as a percentage. Quantitative variables were summarized as either mean with standard deviation or median with extreme values. Chi-square and Pearson correlation tests were used to test for a relationship between disease duration and otoscopic data (tympanic perforation size, tympanic mucosa appearance, side of ear affected); a difference was said to be statistically significant if p < 0.05. Administrative and ethical considerations were taken into account. All participants gave written informed consent to participate in the study. In the case of children under 16 years old parental consent was obtained.
Results
During the study, 90 patients were included out of a total of 1467 patients that came for consultation, i.e. a hospital prevalence of 6.1%. The median age was 28 years with the range between 1 to 74 years. The male sex represented 52.2% (n = 47) while the female sex represented 47.8% (n = 43), both with a sex ratio of 1.09. Children aged 0–18 years accounted for 35.6% (n = 32) of cases. Those under 30 years of age that were included were 53.4% (n = 48) of cases (Table 1).
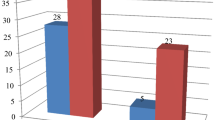
Those who had a history of acute otitis media represented 81.1% of cases (n = 73). The medical history of the patients is presented in Fig. 1.
The median time from onset of otorrhoea to clinical presentation was 6 years with extremes ranging from 4 months to 42 years. Figure 2 gives details of the duration of CSOM in patients.
Clinically, hearing impairment, otalgia and ear pruritus were noted in 55.6% (n = 50); 31.1% (n = 28); and 15.6% (n = 14) of cases respectively (Fig. 3). CSOM was bilateral in 30% of cases (n = 27) and unilateral in 70% of cases (n = 63); with 34.4% of cases (n = 31) on the right and 35.6% of cases (n = 32) on the left. The otoscopic profile of the 117 ears is presented in Table 2. From this table, 71.8% of cases (n = 84) had central tympanic perforations; 51.3% of cases (n = 60) had perforations ≥ ¾ of the tympanic membrane surface. The appearance of the mucosa of the tympanic cavity was erythematous in 49.6% (n = 58) of cases and erythematous with a discharge in 42.7% (n = 50) of cases. There is an association between the size of the perforation and the appearance of the tympanic mucosa (p = 0.003) in Table 3, and between the age of the disease and the side of the ear affected with CSOM (p = 0.016) in Table 4.
Ear swabs were taken from 40% of cases (n = 36). The culture positivity rate was 86.1% (n = 31). Two germs were identified in one patient at a time, giving a total of 32 germs. Staphylococcus aureus was isolated in 28.1% of cases (n = 9), followed by Pseudomonas aeruginosa in 25% of cases (n = 8) and Proteus mirabilis in 9.4% of cases (n = 3) (Table 5). Table 6 shows the sensitivity of the bacteria to antibiotics. The most sensitive antibiotics against Staphylococcus aureus were levofloxacin (44%), vancomycin (44%) and tigecycline (44%). Pseudomonas aeruginosa showed the highest susceptibility to imipenem (75%), ciprofloxacin (63%), ceftazidime (63%) and amikacin (63%). Proteus mirabilis was 67% more sensitive to imipenem, ceftriaxone and trimethoprim/sulfamethoxazole.
Discussion
Chronic suppurative otitis media is still relevant in poor socioeconomic developing countries, particularly in sub-Saharan Africa [10,11,12]. The prevalence of CSOM in this study is within the limits of those obtained in the African literature [2, 13]. The high risk of the disease in this part of the world is probably related to poverty, poor access to health care and a lack of understanding that acute otitis media can eventually lead to chronic suppurative otitis media [14]. CSOM affected all age groups in this series. Children accounted for 35.6% of cases. CSOM is thought to develop in early childhood, often as a result of poorly managed acute otitis media, with the potential to spill over into adulthood, accounting for recurrent episodes of chronic ear discharge that can last for many years [1, 15, 16]. In the present study, males were slightly more than females, similar to other studies such as those by Ologe and Alabbasi [16, 17]. However, a female predominance is noted in some studies [2, 18, 19]. These conflicting results could mean that gender has no impact on the occurrence of CSOM.
In the present study, we observe an extremely long delay between the onset of the disease to clinical presentation. Delayed consultation is mentioned in several publications [2, 18, 20,21,22]. There are many reported causes for the delay. In our context, this could be explained by a large number of the Chadian population living in poverty, which means that health care services are often consulted as a second choice after the traditional practitioner which is very cheap. In addition, self-medication is often inappropriate, access to specialized care is difficult due to the lack of facilities and qualified personnel, and the population's lack of knowledge about the disease.
Clinically, the main symptom associated with otorrhea was hearing loss (55.6%; n = 50); this is consistent with findings from Angola (60%) [10], South Africa (68%) [22] and India (68%) [3]. Otalgia was reported in 31.1% (n = 28) of our patients. Filipe in Angola observed more cases than ours, which was 67% [10]. In other studies, only discomfort and mild pain are usually described [12]. Other symptoms such as ear pruritus, tinnitus, ear fullness and otorrhagia noted in this study, although recognized, are rarely reported in the literature.
Central tympanic perforations were largely predominant in this study, followed by anterosuperior perforations. Both forms have long been described [23]. Large perforations ≥ ¾ of the tympanic membrane surface were more common in 51.3% of cases (n = 60) with a highly inflamed tympanic mucosa. CSOM eventually starts to infect the other ear after a long period of time. All these clinical data reflect the delay in the management of CSOM in our developing countries [24].
From a bacteriological point of view, not all patients in this study were sampled. Most of the patients seen in consultation were already on antibiotic therapy, which did not allow for bacteriological sampling. This situation elucidates that self-medication is increasing in our country. The culture positivity rate and the bacteria isolated from our patients are close to those reported in the literature [3, 7, 8]. The high frequency of Staphylococcus aureus can be attributed to its ubiquitous nature in the external ear canal and upper respiratory tract [8]. Pseudomonas aeruginosa is the most common gram-negative bacteria implicated in CSOM [4]. But the etiological aspects of CSOM can vary considerably depending on factors such as climate variations, socio-economic and demographic status, and patient self-hygiene [25, 26]. Vancomycin, levofloxacin and tigecycline were more effective (44%) against Staphylococcus aureus. In contrast, Pseudomonas aeruginosa showed the highest sensitivity to imipenem (75%), ciprofloxacin (63%), ceftazidime (63%) and amikacin (63%). The susceptibility of bacteria to antibiotics in CSOM varies from study to study. However, many authors have reported a high level of resistance to ampicillin, amoxicillin/clavulanate, cotrimoxazole, amoxicillin and cefuroxime [4, 8, 26, 27]. Ongoing and periodic assessment of the microbiological profile and antimicrobial susceptibility is imperative for optimal treatment and to combat antimicrobial resistance in CSOM [8, 28].
Conclusion
Chronic suppurative otitis media is a relatively common disease in Chad. Medical management is quite late, therefore inevitably leading to hearing loss. Staphylococcus aureus and Pseudomonas aeruginosa are the most isolated bacteria from ear secretions. Vancomycin, levofloxacin and tigecycline have varying degrees of activity against Staphylococcus aureus and imipenem is very active against Pseudomonas aeruginosa. Improving the management of CSOM requires strengthening health care facilities and raising awareness among the population. Good management of ENT conditions in general and acute otitis media in particular would considerably reduce the prevalence of CSOM.
Availability of data and materials
The data used and/or analyzed during this study is available from the corresponding author upon reasonable request.
Abbreviations
- CSOM:
-
Chronic suppurative otitis media
- ENT:
-
Ear, Nose and Throat
- SPSS:
-
Statistical Package for the Social Science
References
Orji F (2013) A survey of the burden of management of chronic suppurative otitis media in a developing country. Ann Med Health Sci Res. 3(4):598–601. https://doi.org/10.4103/2141-9248.122126
Nshimirimana JPD, Mukara KB (2018) Causes of Delayed Care Seeking for Chronic Suppurative Otitis Media at a Rwandan Tertiary Hospital. Int J Otolaryngol. 2:5386217. https://doi.org/10.1155/2018/5386217
Kombade SP, Kaur N, Patro SK, Nag VL (2021) Clinico-bacteriological and antibiotic drug resistance profile of chronic suppurative otitis media at a tertiary care hospital in Western Rajasthan. J Family Med Prim Care 10(7):2572–2579. https://doi.org/10.4103/jfmpc.jfmpc_2480_20
Tesfa T, Mitiku H, Sisay M, Weldegebreal F, Ataro Z, Motbaynor B, Marami D, Teklemariam Z (2020) Bacterial otitis media in sub-Saharan Africa: a systematic review and meta-analysis. BMC Infect Dis 20(1):225. https://doi.org/10.1186/s12879-020-4950-y
Li MG, Hotez PJ, Vrabec JT, Donovan DT (2015) Is chronic suppurative otitis media a neglected tropical disease? PLoS Negl Trop Dis 9(3):e0003485. https://doi.org/10.1371/journal.pntd.0003485
Indorewala S, Adedeji TO, Indorewala A, Nemade G (2015) Tympanoplasty outcomes: a review of 789 cases. Iran J Otorhinolaryngol 27(79):101–108
Wan Draman WNA, MdDaud MK, Mohamad H, Hassan SA, Abd Rahman N (2021) Evaluation of the current bacteriological profile and antibiotic sensitivity pattern in chronic suppurative otitis media. Laryngoscope Investig Otolaryngol 6(6):1300–1306. https://doi.org/10.1002/lio2.682
Khatun MR, Alam KMF, Naznin M, Salam MA (2021) Microbiology of Chronic Suppurative Otitis Media: An update from a Tertiary Care Hospital in Bangladesh. Pak J Med Sci 37(3):821–826. https://doi.org/10.12669/pjms.37.3.3942
Brennan-Jones CG, Head K, Chong LY, Burton MJ, Schilder AG, Bhutta MF (2020) Topical antibiotics for chronic suppurative otitis media. Cochrane Database Syst Rev 1(1):CD013051. https://doi.org/10.1002/14651858.cd013051.pub2
Filipe M, Karppinen M, Kuatoko P, Reimer Å, Riesbeck K, Pelkonen T (2020) Suppurative otitis media in Angola: clinical and demographic features. Trop Med Int Health 25(10):1283–1290. https://doi.org/10.1111/tmi.13466
Karppinen M, Bernardino L, Dos Anjos E, Pätäri-Sampo A, Pitkäranta A, Peltola H, Pelkonen T (2019) Etiology of Childhood Otorrhea in Luanda, Angola, and a Review of Otitis Media in African Children. Pediatr Infect Dis J 38(6):577–581. https://doi.org/10.1097/INF.0000000000002254
Mukara KB, Lilford RJ, Tucci DL, Waiswa P (2017) Prevalence of Middle Ear Infections and Associated Risk Factors in Children under 5 Years in Gasabo District of Kigali City Rwanda. Int J Pediatr 2017:4280583. https://doi.org/10.1155/2017/4280583
Ibekwe TS, Nwaorgu OG (2011) Classification and management challenges of otitis media in a resource-poor country. Niger J Clin Pract 14(3):262–269. https://doi.org/10.4103/1119-3077.86764
Orji FT, Dike BO, Oji O (2015) Determinants of non-healing ear discharge in chronic suppurative otitis media in a developing country. Eur Arch Otorhinolaryngol 272(10):2713–3278. https://doi.org/10.1007/s00405-014-3255-4
Elemraid MA, Brabin BJ, Fraser WD, Harper G, Faragher B, Atef Z, Al-Aghbari N, Mackenzie IJ (2010) Characteristics of hearing impairment in Yemeni children with chronic suppurative otitis media: a case-control study. Int J Pediatr Otorhinolaryngol 74(3):283–286. https://doi.org/10.1016/j.ijporl.2009.12.004
Ologe FE, Nwawolo CC (2003) Chronic suppurative otitis media in school pupils in Nigeria. East Afr Med J 80(3):130–134. https://doi.org/10.4314/eamj.v80i3.8681
Alabbasi A, Alsaimary I, Najim J (2010) Prevalence and patterns of chronic suppurative otitis media and hearing impairment in Basrah city. J Med Med Sci 1(4):129–133
SHC, MMK, Handi P, Khavasi P, Doddmani SS, Riyas M (2014) To Study the Level of Awareness About Complications of Chronic Suppurative Otitis Media (CSOM) in CSOM Patients. J ClinDiagn Res. 8(2):59–61. https://doi.org/10.7860/JCDR/2014/8009.4008
Shyamala R, Reddy PS (2012) The study of bacteriological agents of chronic suppurative otitis media–aerobic culture and evaluation. J Microbiol Biotechnol Res 2(1):152–162
Mukara KB, Waiswa P, Lilford R, Tucci DL (2017) Knowledge and care seeking practices for ear infections among parents of under five children in Kigali, Rwanda: a cross-sectional study. BMC Ear Nose Throat Disord 17:7. https://doi.org/10.1186/s12901-017-0040-1
Poole NF, Skilton MK, Martin TC, Smith MC (2016) Knowledge, attitudes, beliefs and practices related to chronic suppurative otitis media and hearing impairment in Pokhara. Nepal J Laryngol Otol 130(1):56–65. https://doi.org/10.1017/S0022215115002996
Tiedt NJ, Butler IR, Hallbauer UM, Atkins MD, Elliott E, Pieters M, Joubert G, Seedat RY (2013) Paediatric chronic suppurative otitis media in the Free State Province: clinical and audiological features. S Afr Med J 103(7):467–470. https://doi.org/10.7196/samj.6636
Billon-Galland L, Hermann R, Coudert A, Truy E (2021). Otite moyenne chronique non cholestéatomateuse : physiopathologie et formes cliniques. EMC - Oto-rhinolaryngologie [Article 20–095-A-10] https://doi.org/10.1016/S0246-0351(21)58455-4
Tall A, Ndiaye M, Diom ES, Nao EE, Deguenonvo R, Diallo BK et al (2012) Myringoplastie par la technique des boutonnières. J Tun ORL 28:7–12
Uddén F, Filipe M, Reimer Å, Paul M, Matuschek E, Thegerström J, Hammerschmidt S, Pelkonen T, Riesbeck K (2018) Aerobic bacteria associated with chronic suppurative otitis media in Angola. Infect Dis Poverty 7(1):42. https://doi.org/10.1186/s40249-018-0422-7
Endaylalu K, Abera B, Mulu W (2020) Extended spectrum beta lactamase producing bacteria among outpatients with ear infection at FelegeHiwot Referral Hospital. North West Ethiopia PLoS One 15(9):e0238891. https://doi.org/10.1371/journal.pone.0238891
Tadesse B, Shimelis T, Worku M (2019) Bacterial profile and antibacterial susceptibility of otitis media among pediatric patients in Hawassa Southern Ethiopia: cross-sectional study. BMC Pediatr 19(1):398. https://doi.org/10.1186/s12887-019-1781-3
Getaneh A, Ayalew G, Belete D, Jemal M, Biset S (2021) Bacterial Etiologies of Ear Infection and Their Antimicrobial Susceptibility Pattern at the University of Gondar Comprehensive Specialized Hospital, Gondar, Northwest Ethiopia: A Six-Year Retrospective Study. Infect Drug Resist 14:4313–4322. https://doi.org/10.2147/IDR.S332348
Acknowledgements
The authors are grateful to all the patients who agreed to participate in this study and to all the staff of the ENT and Head and Neck Surgery Department of the Renaissance University Hospital for their contribution.
Funding
The authors did not receive support from any organizations for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design and development of this work. AAT was responsible for analyzing the data and writing the manuscript. The preparation of the material and data collection were carried out by MSMM and YAA. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been authorized by the ethics committee of the Renaissance University Hospital (Reference n° 208/MSP/DGHR/DM/DAF/20) and has been complied with the 2013 Declaration of Helsinki. All participants gave written informed consent to participate in the study. in the case of children under 16 years old parental consent was obtained.
Consent for publication
A verbal consent was obtained from participants (or from their parent or legal guardian in the case of children under 16) for the publication of the data.
Competing interests
The authors have nothing to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Taoussi, A.A., Malloum, M.S.M. & Ali, Y.A. Prevalence and clinico-bacteriological aspects of chronic suppurative otitis media at the Renaissance University Hospital in N'Djamena, Chad. Egypt J Otolaryngol 39, 72 (2023). https://doi.org/10.1186/s43163-023-00437-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00437-9