Abstract
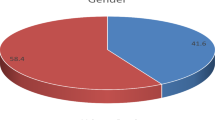
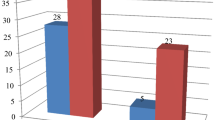
Chronic suppurative otitis media (CSOM) has a substantial worldwide prevalence and is a major cause of hearing impairment. In cases of CSOM unresponsive to local antibiotics, superimposed fungal infection should be suspected. The aim of the present study was to study the spectrum of cases with fungal otitis media. The study was conducted over a period of 12 years (2006–2017). Fifteen cases of CSOM clinically not suspected to be of fungal etiology that underwent surgery with identification of fungal organisms on histopathology were included in the study. Age of the patients ranged from 12 to 75 years (mean age: 37.1 ± 22.7 years). Of 15 cases, 9 (60.0%) were males and 6 (40.0%) were females. It was a unilateral presentation in all. The complaints observed were ear discharge in all followed by itching (86.7%), pain (46.7%), decreased hearing (26.7%) and blocking sensation (13.3%). Histomorphologic typing of fungus was possible in 13/15 patients. Isolated aspergillus was identified in eight patients while mucor alone was seen in three patients. Mixed infection with Aspergillus + Candida and Aspergillus + Mucor was seen in one patient each. Categorization of fungus could not be done in rest of the two patients due to paucity of fungal profiles. Histopathological identification of fungal organisms in otomycosis provides a quick and fairly reliable diagnosis. Culture is considered the gold standard but it may not always be available or fruitful. Less turnaround time and accurate diagnosis facilitates prompt and optimal therapy in fungal otitis media thus preventing adverse outcomes.


Similar content being viewed by others
References
Goycoolea MV, Hueb MM, Ruah C. Otitis media: the pathogenesis approach. Definitions and terminology. Otolaryngol Clin N Am. 1991;24:757–61.
Aarhus L, Tambs K, Kvestad E, Engdahl B. Childhood otitis media: a cohort study with 30-year follow-up of hearing (The HUNT Study). Ear Hear. 2015;36:302–8.
Monasta L, Ronfani L, Marchetti F, Montico M, Vecchi Brumatti L, Bavcar A, et al. Burden of disease caused by otitis media: systematic review and global estimates. PLoS ONE. 2015;7:e36226.
Juyal D, Negi V, Sharma M, Adekhandi S, Prakash R, Sharma N. Significance of fungal flora in chronic suppurative otitis media. Ann Trop Med Public Health. 2014;7:120–3.
Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in 21st century. Clin Microbiol Rev. 2011;24:247–80.
Prakash R, Juyal D, Negi V, Pal S, Adekhandi S, Sharma M, et al. Microbiology of chronic suppurative otitis media in a tertiary care setup of Uttarakhand state, India. N Am J Med Sci. 2013;5:282–7.
Yadav RK, Gaurav K, Bansal M, Jaiswal A. Fungal profiling in patients with chronic suppurative otitis media: a microbiological study. Int J Contemp Med Res. 2016;3:2271–4.
Barati B, Okhovvat SA, Goljanian A, Omrani MR. Otomycosis in central Iran: a clinical and mycological study. Iran Red Crescent Med J. 2011;13:873–6.
Agarwal P, Devi LS. Otomycosis in a rural community attending a tertiary care hospital: assessment of risk factors and identification of fungal and bacterial agents. J Clin Diagn Res. 2017;11:14–8.
Talwar P, Chakrabarti A, Kaur P, Pahwa RK, Mittal A, Mehra YN. Fungal infections of ear with special reference to chronic suppurative otitis media. Mycopathologia 1988;104:47–50.
Kumar A. Fungal spectrum in otomycosis patients. JK Sci. 2005;7:152–5.
Munguia R, Daniel SJ. Ototopical antifungals and otomycosis: a review. Int J Pediatr Otorhinolaryngol. 2008;72:453–9.
Ho T, Vrabec JT, Yoo D. Otomycosis: clinical features and treatment implications. Otolaryngol Head Neck Surg. 2006;135:787–91.
Pradhan B, Tuladhar NR, Amatya RM. Prevalence of otomycosis in outpatient department of otolaryngology in Tribhuvan University Teaching Hospital, Kathmandu, Nepal. Ann Otol Rhinol Laryngol. 2003;112:384–37.
Viswanatha B, Sumatha D, Vijayashree MS. Otomycosis in immunocompetent and immunocompromised patients: comparative study and literature review. Ear Nose Throat J. 2012;91:114–21.
Mgbor N, Gugnani H. Otomycosis in Nigeria: treatment with mercurochrome. Mycoses 2001;44:395–7.
Kirschner R, Sun PL, Huang SL, Chen CL, Yang CP. A case of bilateral otomycosis associated with Aspergillus flavus and A. terreus in Taiwan. J Mycol Med. 2017;27:412–6.
Schrader N, Isaacson G. Fungal otitis externa-its association with fluoroquinolone eardrops. Pediatrics 2003;111:1123.
Jia X, Liang Q, Chi F, Cao W. Otomycosis in Shanghai: aetiology, clinical features and therapy. Mycoses 2012;55:404–9.
Gupta E, Bhalla P, Khurana N, Singh T. Histopathology for the diagnosis of infectious diseases. Indian J Med Microbiol. 2009;27:100–6.
Sangoi AR, Roogers WM, Longacre TA, Montoya JG, Baron EJ, Banaei N. Challenges and pitfalls of morphologic identification of fungal infections in histologic and cytologic specimens: a ten-year retrospective review at a single institution. Am J Clin Pathol. 2009;131:364–75.
Reed JA, Hemann BA, Alexander JL, Brigati DJ. Immunomycology: rapid and specific immunocytochemical identification of fungi in formalin-fixed, paraffin-embedded material. J Histochem Cytochem. 1993;41:1217–21.
Lischewski A, Amann RI, Harmsen D, Merkert H, Hacker J, Morschhäuser J. Specific detection of Candida albicans and Candida tropicalis by fluorescent in situ hybridization with an 18S rRNA-targeted oligonucleotide probe. Microbiology 1996;142:2731–40.
Vennewald I, Klemm E. Otomycosis: diagnosis and treatment. Clin Dermatol. 2010;28:202–11.
Author information
Authors and Affiliations
Contributions
RSP conceptualized the study. RSP, SKS, AD, JC did the data interpretation. RSP, SKS and RK did collection and analysis of data, literature search and prepared the manuscript. RSP, SKS, JC and AD revised the final manuscript critically for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Punia, R.S., Singhal, S.K., Kundu, R. et al. Fungal Suppurative Otitis Media (Histopathology) Among Patients in North India. Head and Neck Pathol 13, 149–153 (2019). https://doi.org/10.1007/s12105-018-0918-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-018-0918-2