Abstract
Objective
Endoscopic ear surgery (EES) is a growing and well-recognized field in the modern era. EES had a stepwise journey of development. This journey is pretty comparable to the endoscopic sinus surgery development.
Methods
Online literature search was performed to give a concise review on the development and recent applications of EES and in addition to clarify the reported advantages and disadvantages of EES.
Results
EES has a more recent application than ESS that started decades after endoscopic sinus surgery (ESS). The use of endoscope in ear surgery gives a wide-angled detailed view of the middle ear structures. It gives the ability to look around the corners offering less disease persistence than the microscopic approaches. EES is useful in cases of narrow and angled external auditory canal as it bypasses the narrowest segment of EAC. However, it lacks the 3D perception and enables one hand surgery which could be difficult to manage bleeding. Applications of EES extended from tympanoplasty, stapedotomy, cholesteatoma surgery, and middle ear ventilation in chronic inflammatory conditions to the neurotologic applications in lateral skull base surgery.
Conclusion
EES is an extremely growing field with many applications in otology and neurotology. The advantages of endoscopic applications outweigh the disadvantages. It has a stepwise learning curve and offer better teaching ability.
Similar content being viewed by others
Introduction
It is evident that endoscopic sinus surgery (ESS) became the standard and the most accepted for nose and sinus surgery worldwide [1]. ESS had a stepwise progress since its early start till developing now to the most advanced transnasal advanced skull base surgery [2]. However, endoscopic ear surgery (EES) had a more later start as it started decades after ESS [3]. It was hard for the endoscope in the start to join ear surgery due to the presence of microscope which is the workhorse of ear surgery [4]. Getting the endoscopic advantages of a wide-angled view and the ability to look around the corners forced the advancement in EES [5].
The aim of this review is to present a short history of the start of both ESS and EES and how we reached now in EES. In addition, the authors try to explain the importance of engaging EES in otology and neurotology different pathologies through deep literature review.
Methods
PubMed and Google were searched using the keywords of endoscopy, endoscopic ear surgery, endoscopic sinus surgery, and transcanal to identify the literature required for review
Endoscopic sinus surgery history
The word “endoscopy” was first reported by Desormeaux who was a urologist from Paris [6]. The story of endoscopic sinus surgery started when Hirschmann used a modified cystoscope to inspect the maxillary sinus in 1901. Following that, various ENT surgeons started to develop the inferior antrostomy to approach the maxillary sinus antrum through the inferior meatus [1]. However, this technique was not widely accepted for long period of time [6]. Messerklinger revitalized endoscopy and applied it to rhinological and sinus surgery [6]. After that, David Kennedy, Heinz Stammberger, and Wolfgang Draf popularized the modern ESS and they modified the endoscopic approaches for maxillary, sphenoid, and frontal sinuses [6]. David kennedy introduced the term functional endoscopic sinus surgery (FESS) with the idea of eradication of the disease and ventilation of the sinuses through their natural openings [2]. Following that, the endoscope was introduced in the field of endoscopic pituitary surgery and endoscopic skull base surgery introducing the concept of extended endoscopic skull base surgery [7, 8]. More recently, Kassam and Carrau have worked on more extended skull base endoscopic procedures [8].
The journey of ESS have passed by many steps starting by using the endoscope for examination of the nasal cavity and sinuses, followed by utilizing the endoscope in endoscopic assisted open procedures then going to exclusive endoscopic endonasal procedures to treat sinus problems and developing the concept of FESS [9]. The advancement of the techniques grew faster and pushed the work in the field of extended and advanced endoscopic sinus surgery treating many pathologies in the pterygopalatine, infratemporal fossa, and lacrimal system [10,11,12,13]. The more development forced the engagement of the endoscope in neurosurgical procedures starting by transsphenoidal pituitary surgery followed by reconstruction of skull base defects and then the extended endoscopic skull base procedures treating pathologies all the way backward from the posterior wall of frontal sinus till the clivus and even the atlanto axial joint [14]. The endoscopic endonasal techniques showed great versatility and the development went stepwise [9]. The important notification is that by the more advancement in the ESS and the more widespread use of the technique, the performance of open procedures went much lower down and even some open procedures were abandoned especially by the newer generations [9].
Endoscopic ear surgery history
The endoscopic ear surgery (EES) journey started much later than the ESS [15]. The early reports started may be in 1992 and later on when Muaaz Tarabichi started talking about the role of endoscope in ear surgery and he published about that in 1997 [5, 16]. Before that, there was a report on probability of endoscopic myringoplasty by El Guindy in Egypt in 1992 [16]. The use of endoscope in ear surgery was somewhat strange in this era and the thinking to combine it with the workhorse of ear surgery which is the microscope was unaccepted by the great and well-known otologists at the time [5]. With time and more popularity of the endoscopic application in ear surgery few reports started to appear from Egypt like Badr-El-Dine study and Abdel Baki study in 2002 [17, 18]. Following that, Ayache in 2007 proposed “the creation of an international Society of otoendoscopy” (later to be renamed the International Working Group on Endoscopic Ear Surgery [IWGEES]) to collaborate for development of the technique. The founding members included Muaaz Tarabichi (UAE), Daniele Marchioni (Italy), Livio Pre-sutti (Italy), Dave Pothier (Canada), Mohamed Badr-el-dine (Egypt), and Seiji Kakehata (Japan) [5]. Following that rapid progress started to appear in the field of EES. Kapadiya and Tarabichi published a nice article demonstrating the number of publications in EES in the last four decades and they showed by diagram how much there was an incredible increase in publications in this field in the last decade compared to the previous decades (Fig. 1) [15]. In this review, we are going to show the value of EES in the management of different ear pathology.
Number of publications categorized by the pattern of utilization of the endoscope in ear surgery per the last four decades [15]
Cohen et al. presented a classification of the engagement of endoscope in otology and they classified that into three waves [19]. The first wave (Cohen class 1) was the diagnostic and documentation aspect of the endoscope like Poe and Bottrill work on use of the transtympanic endoscopy for the confirmation of perilymphatic fistula and the identification of other middle ear pathologic conditions [20]. The second wave (Cohen class 2) involved the use of the endoscope to assist in removal of disease, as an adjunct to the microscope like what Ayache et al. performed in the management of cholesteatoma [21]. The third wave (Cohen class 3) involved the transcanal endoscopic ear surgery (TEES) with the use of endoscope as the main workhorse for ear surgery that now had many applications in the field of otology and neurotology [4]. In the following paragraphs, we are going to present some of the main applications for TEES and how it has developed till being implicated in more advanced work.
EES in cholesteatoma surgery
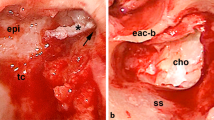
The starting idea of engaging endoscope in ear surgery was in the management of cholesteatoma [5]. Acquired cholesteatoma usually starts by retraction of the tympanic membrane forming a sac that advances into the tympanic cavity, sinus tympani, the attic, and sometimes the hypotympanum and protympanum [5]. In advanced cases, the sac advances more posteriorly in the mastoid. Therefore, the most logical approach is to clear the origin which is the tympanic cavity through a transcanal approach and following the disease process posteriorly through transmastoid approach if needed [15]. However, the most practiced approach for cholesteatoma was the microscopic transmastoid approach [15]. Most surgical failures associated with the postauricular approach seem to occur within the tympanic cavity and its difficult-to-reach extensions rather than in the mastoid [22]. The view during microscopic surgery is defined and limited by the narrowest segment of the ear canal [22]. This basic limitation has forced surgeons to create a parallel port through the mastoid to gain access to the attic, the facial recess, and the hypotympanum [23]. In contrast, transcanal endoscopic approach (TEA) bypasses the narrow segment of the ear canal and provides a wide view that enables surgeons to look “around the corner.” Even with a zero-degree endoscope, the surgeon can look well at the posterior and anterior spaces in the middle ear and clear the disease [23] (Fig. 2).
One of the main difficulties of cholesteatoma surgery is insurance of total excision of the disease which is not easy with microscopic surgery [21]. Badr-el-Dine in 2002 reported an incidence of about 23% intraoperative residual of cholesteatoma when looking by the endoscope after completion of the microscopic work [17]. He reported that sinus tympani was the most common site of residual regardless the procedure type either with intact canal wall or with canal wall down mastoidectomy [17]. He early reported on the importance of incorporation of the endoscope in the surgical work for cholesteatoma and proposed that this would much decrease the residual cholesteatoma rate [17]. Following that many reports emphasized on the role of EES in cholesteatoma surgery [21, 22]. More recently, TEES was engaged in the management of cases of external auditory canal (EAC) cholesteatoma even in the advanced stages [24].
Role of EES in endoscopic anatomy and physiology of middle ear
Understanding the importance of EES forced the progress in detailed description of endoscopic anatomy of the middle ear with studying every single compartment of the middle ear with its configurations, structures, ridges, and bridges [25]. The rationale for that is to define the disease spread in each area and how to decrease the rate of disease persistence or recurrence [26]. The retrotympanum was extensively studied endoscopically and divided into 4 spaces with the main description of the sinus tympani and facial recess. The structures in this space were described like the ponticulus and subiculum with their variations [27]. The attic also was revisited endoscopically with its two main parts the anterior and posterior epitympanic spaces with clarification of the attic diaphragm [28]. The protympanum was also described endoscopically with its two main conformations with description of the protinuculum separating it from the hypotympanum [29]. The round window area was extensively studied with description of the clinical importance of the fustis and finiculus conformations [30]. The hypotympanum also was studied with classification of the jugular bulb height in the middle ear [31]. The knowledge of detailed endoscopic anatomy of these spaces is important for EES [32]. In addition, the presence of the bony crests, bridges, and sinuses in the middle ear affect greatly the disease spread and the surgical procedures [33] (Fig. 3).
The middle ear cavity by 0° endoscope: m. malleus, I incus, star: stapedius tendon attached to stapes head, P pyramidal eminence with the ponticulus originating from it, S: styloid eminence, the blue arrow refers to oblique fustis with subcochlear canaliculus below, ST sinus tympani, and SST sinus subtympanicus. The yellow arrow: the protinaculum. AG annular groove, HY hypotympanum, and PR protympanum. We can consider 2 spaces lateral to P, S (facial recess and lateral sinus) and 3 spaces medial (posterior sinus, sinus tympani, and sinus subtympanicus)
Another important issue in the chronic ear surgery is the physiological routes of ventilation of the middle ear spaces [5]. Marchioni et al. have published in 2013 on this essential issue [34]. Microscopic access through the mastoid is focused on the most posterior part of the air cell system, and therefore, the most downstream in terms of ventilation [5]. The upstream parts of the ventilation system, the Eustachian tube isthmus, protympanum, anterior mesotympanum, and the tympanic isthmus are barely visualized with the posterior, mastoid-based, and microscopic approach [5]. Failures in chronic ear surgery have been shown to correlate to persistent ventilation failure and Eustachian tube dysfunction [35]. However, TEA allows easy visualization of the main anterior ventilation routes with the improved ability of their management [5].
Endoscopic tympanoplasty
Tympanoplasty is a commonly used procedure for the treatment of chronic otitis media, and it involves eradication of the disease in the middle ear, repair of the perforated tympanic membrane, and restoration of hearing [36]. Endaural, transcanal, and postauricular microscopic approaches are the main for these procedures [37]. However, more soft tissue dissection is needed in the postauricular and endaural approaches. The microscopic transcanal approach is limited by the narrowest segment of the canal and the view is usually limited [38]. Transcanal endoscopic approach for tympanoplasty is getting more popularized due to being a more minimally invasive surgery [39]. It provides wide angled view of the spaces in the middle ear, ossicles, and ventilation routes with limited soft tissue dissection [40]. Recent studies showed comparable results to the microscopic-based procedures [39] (Fig. 4).
A Endoscopic trimming of the edge of tympanic membrane perforation. B Good endoscopic view of the anterior edge of the perforation with the ability to adjust the graft in underlay fashion to the anterior edge in narrow EAC. Arrow refers to the anterior edge of the perforation with the endoscopic ability to accommodate the graft in underlay fashion
Endoscopic stapedotomy and ossiculoplasty
Transcanal stapes surgery for otosclerosis has been a gold standard procedure for patients with otosclerosis [41]. Operating microscope is the most commonly used tool for this elegant procedure till now [41]. The microscope provides a detailed magnified view with good depth perception and with the ability to work with both hands which provides more stability [42]. However, the microscopic view is limited by the narrowest part of the EAC and it gives limited view to the axis of the microscope [43]. In addition, in narrow and tortuous EAC, the use of microscope could be difficult and limited [43]. However, due to the wide angled view of the endoscope, endoscopic stapedotomy has been proposed in the past 2 decades with many reported advantages [44]. The main advantages are lesser bone removal, chorda tympani handling, better visibility of the footplate area, and lesser operating time [45] (Fig. 5). In addition, the use of endoscope gives better teaching experience for the new generations [44].
The application of the endoscope in ossicular chain reconstruction is a recent issue [40]. Recent studies have demonstrated the comparable audiometric outcomes of endoscopic ossicular chain reconstruction (OCR) to the traditional microscopic procedures [46]. The increased visualization, wide surgical field provided by the endoscope and the ability to look around the corners provide values and comfort for the surgeon during reconstruction [47]. Excellent visualization of middle ear structures and recesses, mainly the oval window niche, stapes anterior crus and its suprastructure is an important factor for precision during ossiculoplasty, and this can be achieved better by the endoscopic view [47] (Fig. 6). However, the main disadvantages of endoscopic OCR are the single-handed surgery and the long surgical learning curve which are not hindering drawbacks [47].
EES in neurotology
The progress in the field enabled the EAC to be a natural corridor for endoscopic surgery of various diseases of the middle ear till the internal auditory canal (IAC) [26]. This development recently proposed the transcanal endoscopic facial nerve surgery for the treatment of facial nerve diseases located on its tympanic segment and geniculate ganglion (GG) [48]. The clinical role of TEA in management of cases with posttraumatic facial nerve paralysis has been clinically published in the past few years [49, 50]. This approach offered the most direct and least invasive approach for the most commonly affected nerve segments by the trauma and spared the normal mastoid tissue with avoidance of the external incision [50] (Fig. 7).
A Endoscopic view of the right ear after incus removal and nibbling of malleus head showing bone fragment and hematoma compressing the GG, M. refers to the malleus. B Decompression of the GG [50]
The further progress of the EES allowed the EAC to be a natural way to inner ear lesions and to the internal auditory canal (IAC) [51]. Reports were published on the endoscopic transcanal transpromontorial approach in cases of acoustic neuroma localized to IAC or with minimal extension beyond [51]. There is now much interest in this approach with more published articles in this issue [52, 53]. This transcanal approach can be less invasive than the already documented approaches like the retrosigmoid, translabyrinthine, and middle cranial fossa approaches [51]. In addition, the wide-angled view enabled good visualization of the boundaries and optimum dissection of the tumor from the nerves with good rate of facial nerve function preservation postoperatively [51].
Advantages and disadvantages
The arguments for and against the endoscope have been diverse [3]. However, this conflict is rising more in the way of progress of EES than ESS that has been greatly established in relation to the open procedures [3]. The conflict for the involvement of TEES was much in the early start of the application [5]. More recently, being accepted as a more direct and less invasive tool, this conflict decreased a bit [54]. TEES gives a better alignment of surgical access with underlying anatomy, disease process, and ventilation [15]. The superior visualization capabilities with wide-angled view and the ability to look around corners provided by the endoscope give more control over the disease process and increase the protection of the important structures [5]. However, EES has certain disadvantages like single-handed work which can add some difficulty to control bleeding [3]. Some reports on possible thermal damage to the middle ear structures as the light is emitted from the tip of the endoscope are also controversial [3]. The stepwise learning curve is another issue as it takes some time to accustom to holding the endoscope by one hand and working with the other hand [35]. However, having the skills of ESS which is more popular and more widespread facilitate the learning curve for all ENT surgeons [3].
Microscopes are important for otological surgeries as they provide excellent lighting with depth perception with binocular vision and the ability to perform two handed surgeries [41]. However, the microscopic view is restricted to the area where the light goes and by the narrowest segment of the EAC [44]. Therefore, in cases of narrow and tortuous canals, more soft tissue cutting and dissection is needed [44]. In addition, more bone drilling like canaloplasty, atticotomy, and mastoidectomy sometimes may be needed apart from required ossicles removal in some cases [43]. On the other hand, the endoscope bypasses the narrowest segment of the EAC and manage the narrow canals without need for much tissue dissection [44]. However, the authors argue that there is no contrary or conflict between endoscope and microscope, but they are complementary tools to perform the required job. It is essential to have a standby microscope in the operative room on performing TEES and vice versa.
Conclusion
EES had a more recent and stepwise evolution than ESS. The journey started from developing endoscopic assisted ear surgery till reaching to exclusive TEES. The applications of TEES have increased over the years having the EAC as a natural corridor for many middle and inner ear pathologies. The stepwise learning curve is important for precision of the techniques.
Availability of data and materials
Not applicable.
References
Kane KJ (2020) The early history and development of functional endoscopic sinus surgery. J Laryngol Otol 134(1):8–13. https://doi.org/10.1017/S0022215119002457
Kennedy DW (2006) Technical innovations and the evolution of endoscopic sinus surgery. Ann Otol Rhinol Laryngol Suppl 196:3–12. https://doi.org/10.1177/00034894061150s902
Emre IE, Cingi C, Bayar Muluk N, Nogueira JF (2020) Endoscopic ear surgery. J Otolaryngol 15(1):27–32. https://doi.org/10.1016/j.joto.2019.11.004
Ryan P, Wuesthoff C, Patel N (2020) Getting started in endoscopic ear surgery [published correction appears in J Otol. 2020 Dec;15(4):180]. J Otolaryngol 15(1):6–16. https://doi.org/10.1016/j.joto.2018.10.002
Tarabichi M, Arsiwala Z (2021) History of endoscopic ear surgery. Otolaryngol Clin N Am 54(1):1–9. https://doi.org/10.1016/j.otc.2020.09.002
Prevedello DM, Doglietto F, Jane JA Jr, Jagannathan J, Han J, Laws ER Jr (2007) History of endoscopic skull base surgery: its evolution and current reality. J Neurosurg 107(1):206–213. https://doi.org/10.3171/JNS-07/07/0206
Cavallo LM, Somma T, Solari D et al (2019) Endoscopic endonasal transsphenoidal surgery: history and evolution. World Neurosurg 127:686–694. https://doi.org/10.1016/j.wneu.2019.03.048
Chandra RK, Conley DB, Kern RC (2009) Evolution of the endoscope and endoscopic sinus surgery. Otolaryngol Clin N Am 42(5):747–vii. https://doi.org/10.1016/j.otc.2009.07.010
Chan M, Carrie S (2018) Training and assessment in functional endoscopic sinus surgery. J Laryngol Otol 132(2):133–137. https://doi.org/10.1017/S0022215117002183
Chitsuthipakorn W, Seresirikachorn K, Kanjanawasee D, Snidvongs K (2020) Endoscopic sphenopalatine foramen cauterization is an effective treatment modification of endoscopic sphenopalatine artery ligation for intractable posterior epistaxis. Eur Arch Otorhinolaryngol 277(9):2463–2467. https://doi.org/10.1007/s00405-020-06005-8
Kumar S, Mishra AK, Sethi A et al (2019) Comparing outcomes of the standard technique of endoscopic DCR with its modifications: a retrospective analysis. Otolaryngol Head Neck Surg 160(2):347–354. https://doi.org/10.1177/0194599818813123
Mueller SK, Freitag SK, Lefebvre DR, Bleier BS (2018) Endoscopic DCR using bipedicled interlacing mucosal flaps. Laryngoscope. 128(4):794–797. https://doi.org/10.1002/lary.26730
Karkas A, Zimmer LA, Theodosopoulos PV, Keller JT, Prades JM (2021) Endonasal endoscopic approach to the pterygopalatine and infratemporal fossae. Eur Ann Otorhinolaryngol Head Neck Dis 138(5):391–395. https://doi.org/10.1016/j.anorl.2020.12.009
Wang EW, Zanation AM, Gardner PA et al (2019) ICAR: endoscopic skull-base surgery. Int Forum Allergy Rhinol 9(S3):S145–S365. https://doi.org/10.1002/alr.22326
Kapadiya M, Tarabichi M (2019) An overview of endoscopic ear surgery in 2018. Laryngoscope Investig Otolaryngol 4(3):365–373. https://doi.org/10.1002/lio2.276 Published 2019 May 24
El-Guindy A (1992) Endoscopic transcanal myringoplasty. J Laryngol Otol 106(6):493–495. https://doi.org/10.1017/s0022215100119966
Badr-el-Dine M (2002) Value of ear endoscopy in cholesteatoma surgery. Otol Neurotol 23(5):631–635. https://doi.org/10.1097/00129492-200209000-00004
Abdel Baki F, El Dine MB, El Saiid I, Bakry M (2002) Sinus tympani endoscopic anatomy. Otolaryngol Head Neck Surg 127(3):158–162. https://doi.org/10.1067/mhn.2002.127588
Cohen MS, Basonbul RA, Barber SR, Kozin ED, Rivas AC, Lee DJ (2018) Development and validation of an endoscopic ear surgery classification system. Laryngoscope. 128(4):967–970. https://doi.org/10.1002/lary.26802
Poe DS, Bottrill ID (1994) Comparison of endoscopic and surgical explorations for perilymphatic fistulas. Am J Otolaryngol 15(6):735–738
Ayache S, Tramier B, Strunski V (2008) Otoendoscopy in cholesteatoma surgery of the middle ear: what benefits can be expected? Otol Neurotol 29(8):1085–1090. https://doi.org/10.1097/MAO.0b013e318188e8d7
Chiao W, Chieffe D, Fina M (2021) Endoscopic management of primary acquired cholesteatoma. Otolaryngol Clin N Am 54(1):129–145. https://doi.org/10.1016/j.otc.2020.09.014
Marchioni D, Mattioli F, Alicandri-Ciufelli M, Presutti L (2009) Transcanal endoscopic approach to the sinus tympani: a clinical report. Otol Neurotol 30(6):758–765. https://doi.org/10.1097/MAO.0b013e3181b0503e
Li Y, Sheng Y, Xia C et al (2021) Transcanal endoscopic ear surgery for advanced external auditory canal cholesteatoma in naim stage III and IV. Otol Neurotol 42(10):e1698–e1705. https://doi.org/10.1097/MAO.0000000000003378
Marchioni D, Molteni G, Presutti L (2011) Endoscopic anatomy of the middle ear. Indian J Otolaryngol Head Neck Surg 63(2):101–113. https://doi.org/10.1007/s12070-011-0159-0
Marchioni D, Alicandri-Ciufelli M, Mattioli F et al (2013) From external to internal auditory canal: surgical anatomy by an exclusive endoscopic approach. Eur Arch Otorhinolaryngol 270(4):1267–1275. https://doi.org/10.1007/s00405-012-2137-x
Bonali M, Anschuetz L, Fermi M et al (2017) The variants of the retro- and hypotympanum: an endoscopic anatomical study. Eur Arch Otorhinolaryngol 274(5):2141–2148. https://doi.org/10.1007/s00405-017-4492-0
Tarabichi M, Marchioni D, Kapadia M (2016) The epitympanum revisited: endoscopic anatomy. Indian J Otolaryngol Head Neck Surg 68(4):490–495. https://doi.org/10.1007/s12070-016-1000-6
Jufas N, Rubini A, Soloperto D et al (2018) The protympanum, protiniculum and subtensor recess: an endoscopic morphological anatomy study. J Laryngol Otol 132(6):489–492. https://doi.org/10.1017/S0022215118000464
Marchioni D, Soloperto D, Colleselli E, Tatti MF, Patel N, Jufas N (2016) Round window chamber and fustis: endoscopic anatomy and surgical implications. Surg Radiol Anat 38(9):1013–1019. https://doi.org/10.1007/s00276-016-1662-5
Bonali M, Fermi M, Alicandri-Ciufelli M et al (2020) Correlation of radiologic versus endoscopic visualization of the middle ear: implications for endoscopic ear surgery. Otol Neurotol 41(9):e1122–e1127. https://doi.org/10.1097/MAO.0000000000002787
Şahin B, Orhan KS, Aslıyüksek H, Kara E, Büyük Y, Güldiken Y (2020) Endoscopic evaluation of middle ear anatomic variations in autopsy series: analyses of 204 ears. Braz J Otorhinolaryngol 86(1):74–82. https://doi.org/10.1016/j.bjorl.2018.10.002
Nogueira JF, Mattioli F, Presutti L, Marchioni D (2013) Endoscopic anatomy of the retrotympanum. Otolaryngol Clin N Am 46(2):179–188. https://doi.org/10.1016/j.otc.2012.10.003
Marchioni D, Piccinini A, Alicandri-Ciufelli M, Presutti L (2013) Endoscopic anatomy and ventilation of the epitympanum. Otolaryngol Clin N Am 46(2):165–178. https://doi.org/10.1016/j.otc.2012.10.002
Marchioni D, Rubini A, Soloperto D (2021) Endoscopic ear surgery: redefining middle ear anatomy and physiology. Otolaryngol Clin N Am 54(1):25–43. https://doi.org/10.1016/j.otc.2020.09.003
Pontes-Madruga TC, Nogueira Neto FB, Suzuki FAB, Testa JRG, Onishi ET (2021) Endoscopic tympanoplasty with inlay cartilage graft in an university hospital. Braz J Otorhinolaryngol 87(4):434–439. https://doi.org/10.1016/j.bjorl.2019.10.002
Akyigit A, Sakallıoglu O, Karlidag T (2017) Endoscopic tympanoplasty. J Otolaryngol 12(2):62–67. https://doi.org/10.1016/j.joto.2017.04.004
Sun Y, Wang EH, Yu JT et al (2020) A novel surgery classification for endoscopic approaches to middle ear cholesteatoma. Curr Med Sci 40(1):9–17. https://doi.org/10.1007/s11596-020-2141-0
Anzola JF, Nogueira JF (2016) Endoscopic techniques in tympanoplasty. Otolaryngol Clin N Am 49(5):1253–1264. https://doi.org/10.1016/j.otc.2016.05.016
Kim MS, Chung J, Kang JY, Choi JW (2020) Transcanal endoscopic ear surgery for traumatic ossicular injury. Acta Otolaryngol 140(1):22–26. https://doi.org/10.1080/00016489.2019.1685682
Bartel R, Sanz JJ, Clemente I et al (2021) Endoscopic stapes surgery outcomes and complication rates: a systematic review. Eur Arch Otorhinolaryngol 278(8):2673–2679. https://doi.org/10.1007/s00405-020-06388-8
Mostafa M, Elkahwagi M, AbdEl-fattah AM et al (2021) Role of ionomeric bone cement in primary stapedotomy for otosclerosis. Int J Otorhinolaryngol Clin 13(1):1–6
Hoskison EE, Harrop E, Jufas N, Kong JHK, Patel NP, Saxby AJ (2021) Endoscopic stapedotomy: a systematic review. Otol Neurotol 42(10):e1638–e1643. https://doi.org/10.1097/MAO.0000000000003242
Moneir W, Abd El-Fattah AM, Mahmoud E, Elshaer M (2018) Endoscopic stapedotomy: merits and demerits. J Otolaryngol 13(3):97–100. https://doi.org/10.1016/j.joto.2017.11.002
Das A, Mitra S, Ghosh D, Sengupta A (2021) Endoscopic stapedotomy: overcoming limitations of operating microscope. Ear Nose Throat J 100(2):103–109. https://doi.org/10.1177/0145561319862216
Yan X, Liu P, Ji C et al (2021) Outcomes of ossicular disruption in traumatic facial paralysis: a case series. Acta Otolaryngol 141(3):222–225. https://doi.org/10.1080/00016489.2020.1833081
Yawn RJ, Hunter JB, O'Connell BP et al (2017) Audiometric outcomes following endoscopic ossicular chain reconstruction. Otol Neurotol 38(9):1296–1300. https://doi.org/10.1097/MAO.0000000000001527
Marchioni D, Soloperto D, Rubini A, Nogueira JF, Badr-El-Dine M, Presutti L (2016) Endoscopic facial nerve surgery. Otolaryngol Clin N Am 49(5):1173–1187. https://doi.org/10.1016/j.otc.2016.05.006
Alicandri-Ciufelli M, Fermi M, Di Maro F, Soloperto D, Marchioni D, Presutti L (2020) Endoscopic facial nerve decompression in post-traumatic facial palsies: pilot clinical experience. Eur Arch Otorhinolaryngol 277(10):2701–2707. https://doi.org/10.1007/s00405-020-05997-7
Elkahwagi M, Salem MA, Moneir W, Allam H (2022) Traumatic facial nerve paralysis dilemma. Decision making and the novel role of endoscope. J Otolaryngol 17(3):116–122. https://doi.org/10.1016/j.joto.2022.03.003
Marchioni D, Soloperto D, Masotto B et al (2018) Transcanal transpromontorial acoustic neuroma surgery: results and facial nerve outcomes. Otol Neurotol 39(2):242–249. https://doi.org/10.1097/MAO.0000000000001658
Pradhan S, Chappity P, Nayak A, Pradhan P, Parida PK (2021) Exclusive endoscopic transcanal approach to lateral skull base lesions: institutional experience of 3 cases. J Otolaryngol 16(1):55–60. https://doi.org/10.1016/j.joto.2020.08.004
Moon IS, Cha D, Nam SI, Lee HJ, Choi JY (2019) The feasibility of a modified exclusive endoscopic transcanal transpromontorial approach for vestibular Schwannomas. J Neurol Surg B Skull Base 80(1):82–87. https://doi.org/10.1055/s-0038-1667061
Badr-El-Dine M, James AL, Panetti G, Marchioni D, Presutti L, Nogueira JF (2013) Instrumentation and technologies in endoscopic ear surgery. Otolaryngol Clin N Am 46(2):211–225. https://doi.org/10.1016/j.otc.2012.10.005
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
WM: Conception and design of the study, collecting of data and sharing in writing the article. ME: Collecting of data and sharing in writing the article. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moneir, W., Elkahwagi, M. Endoscopic ear surgery: then and now, review article. Egypt J Otolaryngol 38, 115 (2022). https://doi.org/10.1186/s43163-022-00304-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00304-z