Abstract
Background
Lichen planus is an immune-mediated chronic inflammatory condition of unknown origin that affects the skin and the mucosa. Lichen planus in the larynx is not common, and there are few cases reported in literature. We report an unusual case of lichen planus in the vocal fold.
Case presentation
We present a case of a 62-year-old Caucasian male with a 2-month history of persistent dysphonia and a smoking habit of about 10 cigarettes per day. He has no previous history of systemic disease, and he was not taking any drug for treatment. Fiber-optic laryngoscopy showed a single white rough lesion in the middle third of the right vocal fold. The diagnosis was performed with direct laryngoscopy. Complete excisional biopsy was used as a treatment method. Chest X-ray and blood test were normal. The biopsy reported lichen planus and mild dysplasia. The voice quality improved after the laryngeal microsurgery, and a close follow-up was advised.
Conclusions
There are few cases of lichen planus in the vocal fold reported in the literature, presenting as a unilateral and isolated lesion or concomitant with oral and genital lesions. Other cases mainly report lesions that affect more than one area of the larynx, with undefined margins or with marked cicatrization. Oral or topical corticosteroids, in this case, were not required because of total extirpation of the lesion but may be necessary in case of recurrence. Although lichen planus of vocal fold is very uncommon, it should be consider in differential diagnosis of leukoplakia of the larynx and once diagnosed could be manage with corticosteroid drugs avoiding aggressive treatment.
Similar content being viewed by others
Background
Dysphonia is very common symptom in patients consulting in Otolaryngological Clinics. It can be caused by several diseases. Among these, chronic laryngitis, premalignant and malignant lesions, must be ruled out in individuals who smoke and suffer a persistent dysphonia for more than 4 weeks [1]. The differential diagnosis of a single white lesion in the vocal fold (leukoplakia) includes keratosis, parakeratosis, squamous papilloma, several grades of dysplasia, and carcinoma in situ.
Lichen planus in the vocal fold is a most unusual diagnosis. Lichen planus is an immunologically mediated inflammatory disease generally affects the skin and mucous membranes in the oral cavity, oropharynx, esophagus, and genitalia [2, 3].
There are very few published cases of lichen planus affecting the larynx; most of them describe diffuse lesions mainly supraglottis. Even less cases do involve the vocal fold, presenting as isolated white lesions [4], and/or may coexist with oral and genital lichen planus [5]. Recently, Leoncini et. al. report a case of lichen planus affecting both vocal folds, with a velvety whitish plaque in one of them [6]. The main symptom of lichen planus of the vocal fold is dysphonia, but Ashis et al. described the case presenting with dysphonia and dyspnea due to upper airway narrowing by the lichen planus in the anterior 2/3 of the vocal folds [5].
Case presentation
Our patient was a 62-year-old man who presented with a 2-month history of slow progressive dysphonia, without any complaint of dyspnea, dysphagia, cough, or weight loss. The dysphonia was persistent throughout the day. He had no previous similar episodes. His personal history was unremarkable, except for a smoking habit of around ten cigarettes a day. He did not report any relevant voice demand at work and had a negative family history of head and neck cancer.
Clinical thorough examination of the oral cavity, oropharynx, nose, and neck was normal. Fiber-optic laryngoscopy revealed a single, rough, white unilateral lesion in the middle third of the right vocal fold (Fig. 1). There were no lesions in other parts of the larynx. The right vocal fold also showed some atrophy. The Voice Handicap Index (VHI-10) score was 15, and the GRBAS was 7 (G2R2B0A1S2).
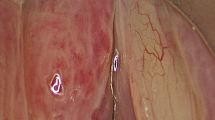
The patient was clinically diagnosed as “leukoplakia,” and at direct laryngoscopy, the lesion was found to involve the superficial mucosa only. We found no other lesions in the vocal fold. The histopathological examination of the biopsy specimen revealed paving mucosa with several apoptotic keratinocytes and intraepithelial lymphocytes (Fig. 2). A moderate inflammatory lymphocyte bandlike infiltrate was seen under the mucosa. An area of mild dysplasia was observed in one of the specimen edges. The diagnosis of lichen planus was made with the above findings. A dermatological consultation ruled out skin lesions. After surgery, the patient’s voice improved significantly, with the following scores: VHI-10 4 and GRBAS 2 (G0R0B1A1S0). After surgery, he received voice therapy to improve the voice quality and breathiness. Because of the finding of mild dysplasia and the atypical histopathology, a close follow-up was advised. He showed no recurrence after 6 months of follow-up.
Discussion
Lichen planus is a chronic inflammatory condition, of unknown origin, which basically affects the skin on the flexor surfaces of the extremities, the scalp and nails, and the mucosa of the oral cavity and genitalia. Other uncommonly affected sites are the esophagus, pharynx, larynx, and conjunctivae [7]. The oral cavity is the most frequent site of clinical presentation, with a prevalence between 1% and 3% in the general population, while its incidence is estimated at around 2.2% [7]. It affects females more than males in a proportion of 1.4:1 [3], and the age of onset is between 30 and 60, with greater incidence in Caucasians.
Its oral form—also known as oral lichen planus—is the most common, with a prevalence between 1% and 2% in the general population [8]. Oral lichen planus (OLP) can be the sole clinical presentation of the disease or can be associated with other lesions in genitalia, extremities, or gastrointestinal tract. The cause is still unknown, but it can be triggered by medication such as nonsteroidal anti-inflammatory drugs, beta-blockers, antimalarials, diuretics, oral hypoglycemics, penicillamine, and retroviral drugs. Lesions in the skin have been associated with hepatitis C virus, most prevalent in the Mediterranean and Japan [9]. The pathogenic mechanism of LP involves apoptosis of epithelial cells at the basal layer, due to an antigen expressed by Langerhans cells. T-cells CD4+ and CD8+ and natural killer cells also participate in the apoptosis of keratinocytes. The activated epithelial cell releases cytokines that promote chemotaxis of lymphocytes that induce LPO lesions [10]. The classical presentation of OLP is a lesion with white or gray (or white gray) lines in the oral mucosa, called Wickham’s striae, which can organize as reticular or annular patterns, or in patches and strings. Cases of lichen planus in the mucosa of hypopharynx and larynx have been described as white plaque lesions (putetice). One case of laryngeal LP described in the literature involved the false vocal fold and arytenoids, with marked cicatrization and hypertrophy. There are few cases of lichen planus in the vocal folds described in the literature.
The histopathological examination of OLP of the biopsy reveals degenerative keratinocytes, parakeratosis, basal cell liquefactive degeneration and the presence of degenerated keratinocytes and cystoid bodies (colloid or Civatte bodies), and mononuclear infiltration by T-cells (Fig. 1).
Pigmentary incontinence is common in skin lesions. A lymphohistiocytic bandlike infiltrate occupies the upper dermis or submucosa is very usual. Lesions may become completely atrophic (flattening of the epidermis), with variable number of colloid bodies and pigment incontinence with almost no inflammation.
The most important differential diagnosis of lichen planus in the larynx is with squamous cell carcinoma. Other lesions to be considered in this differential diagnosis are the following entities: keratosis, parakeratosis, granulomas, squamous papilloma, and dysplasia.
The potential for malignant transformation of OLP ranges from 1.2 to 9.52 percent [11], but for obvious reasons, there is no data on the risk for laryngeal lesions. In a cohort of 13,100 women in Finland diagnosed of LP between 1969 and 2012, mainly OLP, Halonen et al. [12] found that 1520 were eventually diagnosed with cancer in areas such as the lip, tongue, oral cavity, esophagus, larynx, and vulva. Their conclusion, with this finding, was that patients with LP could benefit from a multidisciplinary approach since they have a higher to develop cancer than the regular population. They have to be advised to report any symptom in the upper airway.
In our case, mild dysplasia was found in the biopsy, and since the patient was an active smoker, a strict follow-up was mandatory.
The treatment of mucosal lichen planus is based in corticosteroids, depending on the symptoms and the type of lesions. Intralesional injections are recommended for erosive forms, in single dose. If there is no improvement, topical corticosteroids during several weeks are indicated. Oral corticosteroids are prescribed for persistent lesions. Other options of treatment are topical tacrolimus and diode laser therapy. Although malignant transformation in OLP is rare, a close follow-up is mandatory for these patients.
Conclusions
Lichen planus is a very uncommon disease, and when it affects the larynx, it arises differential diagnosis with dysplasia and squamous cell carcinoma. Once the pathology diagnosis is obtained, oral corticoids treatment should be established if there is remaining lesion or recurrence. Further studies are needed to know the potential malignant transformation of lichen planus in the vocal folds.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stachler R, Francis D, Schwartz S (2009) Clinical practice guideline: hoarseness (dysphonia) (update). Otolaryngol Head Neck Surg 131:1–31. https://doi.org/10.1016/j.medcli.2017.06.024
Rennie CE, Dwivedi R, Khan AS et al (2011) Lichen planus of the larynx. J Laryngol Otol. 125:432–435. https://doi.org/10.1017/S002221511000280X
Jayasri Krupaa R, Leena Sankari S, Masthan KM et al (2015) Oral lichen planus: an overview. J Pharm Bioallied Sci 7:S158–S161
Kiakujori K, Kamalian N (2010) Vocal cord lesion due to lichen planus. Casp. J Intern Med 1(1):36.38
Ashis G, Emerson LP, Michael RC et al (2014) Lichen planus of larynx manifesting as airway compromise: a rare presentation. Int J Otorhinolaryngol Clin 6(3):95–97. https://doi.org/10.5005/jp-journals-10003-1164
Leoncini G, Marin MG, Squeglia C et al Laryngeal lichen planus mimicking vocal fold dysplasia. Auris Nasus Larynx. https://doi.org/10.1016/j.anl.2021.04.002
Gorouhi F, Davari P, Fazel N (2014) Cutaneous and mucosal lichen planus: a comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis. Sci World J. https://doi.org/10.1155/2014/742826
Bulfamante AM, D’Agostino Fiorenza U, Pipolo GC (2021) Identification of putative laryngeal and pharyngeal lichen planus lesions: an endoscopic preliminary evaluation in 16 patients. Clin Otolaryngol 46(84-87). https://doi.org/10.1111/coa.13633
Kusari A, Ahluwalia J (2018) Lichen planus. Images in clinical clinics. N Engl J Med 379:567
García-Pola MJ, González-Álvarez L, García-Martin JM (2017) Tratamiento del liquen plano oral. Revisión sistemática y protocolo de actuación. Med Clín 149:351–362
Liu W, Ma L, Song C et al (2020) Research trends and characteristics of oral lichen planus: a bibliometric study of the top-100 cited articles. Medicine 99:2
Halonen P, Jakobsson M, Heikinheimo O Cancer risk of lichen planus: a cohort study of 13,100 women in Finland. Int. J. Cancer. 2018;142:18–22.
Acknowledgements
None
Funding
None
Author information
Authors and Affiliations
Contributions
Conception—RG, RI, BB, and GJ. Design—RG. Supervision—BB and GJ. Data collection and/or processing—RG. Analysis and/or interpretation—RG. Literature review—RG. Writing of the manuscript—RG. Critical review—BB and GJ. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the Ethics Committee of Hospital Universitario HLA Moncloa. Written consent was obtained from the patient to participate in the study.
Consent for publication
Written informed consent from the participant was obtained for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pino, G.R., Pérez, I.R., Guede, B.B. et al. Dysphonia of exceptional origin: lichen planus of the vocal fold — a case report of a very uncommon area affected by lichen planus. Egypt J Otolaryngol 38, 48 (2022). https://doi.org/10.1186/s43163-022-00238-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00238-6