Abstract
Background
Burkholderia pseudomallei is a causative agent of melioidosis, a fatal infectious disease highly prevalent in the tropics where traditional medicinal plants are widely used for the treatment of various human ailments. In this study, we aimed to evaluate the in vitro antibacterial activity of common eligible herbs and medicinal plants against B. pseudomallei. Thermal and gastric stability, antibacterial spectrum, bactericidal activity, and cell cytotoxicity were also tested to verify the possible usage of these plants in the treatment of melioidosis.
Results
Eighteen eligible herbs and twenty-one medicinal plants were collected. Herb juices and aqueous plant samples extracted at different temperatures were prepared for antibacterial testing. A higher proportion of aqueous plant extracts (17/21; 80.9%) against B. pseudomallei was observed, in comparison with that of herb juices (8/18; 44.5%). Two herb juices and twelve aqueous plant extracts were selected for further tests. The juices of A. sativum and A. tuberosum decreased their antimicrobial activity when treated at higher temperatures whereas the aqueous plant extracts increased their antimicrobial activity when prepared at 70 and 100 °C. The herb juices showed a broader spectrum of antimicrobial activity than the aqueous plant extracts. All samples showed less cytotoxicity on the HT29, HepG2, and HEK293 cell lines. At the 2× minimal inhibitory concentration (MIC), aqueous extracts of Blechnum orientale, Breynia fruticose, Psidium guajava, Rhodomyrtus tomentosa, Rosa odorata, and Schima wallichii showed similar bactericidal activity to that of amoxicillin clavulanic acid. The antimicrobial activity of Mangifera indica, Punica granatum, and R. tomentosa remained under the stimulated gastric conditions.
Conclusion
Our data indicate that traditional medicinal plants prepared by decoction could be effectively used to treat melioidosis via the oral route. Further in vivo investigations are needed to explore other alternative therapies for the prevention and treatment of tested pathogenic bacterial species.
Similar content being viewed by others
Background
The Gram-negative bacillus Burkholderia pseudomallei is a causative agent of melioidosis, a fatal infectious disease in humans and a wide variety of captive and wild-life animal species [1]. The bacterium occupies ubiquitously in the paddy soil and surface water environments in the tropics and sub-tropics, including but not limited to Southeast Asia and northern Australia [2]. Melioidosis can manifest a diverse clinical presentation, ranging from chronic skin lesions, multiple internal organ abscesses, gastrointestinal and genitourinary tract infections, to acute pneumonia and septicaemia, with a mortality rate up to 50% in certain endemic areas [1, 3]. A recent modeling study on the global burden of melioidosis estimated that there are about 165,000 cases infected with B. pseudomallei per year worldwide, of which 89,000 deaths occur [2]. These estimations imply a significant health risk of melioidosis at global level, in comparison with other common infectious diseases such as leptospirosis, measles, and dengue [2].
Human infections with the bacterium may be acquired via three main routes of (i) inoculation through minor cuts or skin abrasions when directly exposed to contaminated soils or water, (ii) inhalation of the bacterial aerosols generated by extreme weather events, and (iii) ingestion of uncooked foods and/or untreated drinking water [4, 5]. All of the infection routes are more likely to affect a large group of people living in rural areas of the tropics because of their daily working activities on the agricultural fields, the possible use of inadequate water suppliers such as untreated bore and well water [5, 6], and the impact of poor sanitation and hygiene standards. Recently, B. pseudomallei has been recognized as an enteric pathogen and some virulent factors required for gastrointestinal infections were determined [7]. In the chronic mouse model of infection via oral or intragastric routes, the bacterium can persistently colonize the stomach, small intestine, and colon and subsequently spread to the liver and spleen [7, 8]. In human melioidosis, a number of cases related to gastrointestinal infections are gradually reported [9] and the clinical manifestations on the hospital admission are associated with fever, abdominal pain, and abscess formation in multiple internal organs [10].
B. pseudomallei is intrinsically resistant to many commercially available antibiotic groups and the treatment of melioidosis requires a specific prolonged course of antibiotic therapy [1]. Up to now, report on antibacterial activity of natural compounds originated from herbs or medicinal plants against B. pseudomallei is still limited. Preliminary findings in India and Thailand showed that methanolic extracts of some indigenous traditional medicinal plants such as Barringtonia acutangula (L.), Cassia fistula Linn, Limnophila geoffrayi Bonati, Luffa acutangula (Linn.), and Tamarindus indica Linn could inhibit the growth of B. pseudomallei when tested under in vitro conditions [11,12,13]. In Vietnam, methanol extracts from medicinal plants of Cratoxylum formosum subsp. pruniflorum (Kurz), Euphorbia hirta, Pedilanthus tithymaloides, Pluchea indica, and Pogostemon cablinin have been shown broad spectrum antibacterial activity against both Gram-positive and Gram-negative bacteria tested, including Bacillus cereus, Bacillus subtilis, Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa [14].
From very ancient times, medicinal plants have been used to treat various human diseases, including infectious diseases caused by pathogenic bacteria, fungi, and viruses [15]. Because of the availability, inexpensiveness, and safety, traditional medicinal plants are still effectively used for primary health care in many rural areas of the developing countries [16], including Southeast Asia countries where melioidosis is highly endemic but misdiagnosis is not uncommon [2]. In the traditional medicine of tropical countries with diverse botanical heritage such as China, India, Australia, Mexico, and South Africa, medicinal plants have commonly utilized to treat skin infections, sore throat, chest pain, stomach ache, abdominal pain, diarrhea, and genitourinary disorders caused by infectious agents [12, 17,18,19,20]. Researchers have also focused on the potential usages of the traditional medicinal plants for the treatment of some important infectious diseases such as tuberculosis, salmonellosis, or other food poisoning diseases [21,22,23]. In the customary practice, indigenous people use either fresh or dry plant materials to make the medicinal preparations. For the oral route of administration, fresh plants can be directly cooked with foods or ground and squeezed to get the juices for drinking. The preparations of dry plant materials can be processed with drinking water at different temperatures which are referred to as cool infusion, hot infusion, and decoction [20].
Despite the requirements of either a heat treatment step or an aqueous extraction at different temperatures during the preparation of traditional medicinal plants, the study on the thermal stability of the antibacterial activity is limited. Moreover, stability of the antibacterial activity after exposure to gastric conditions should be taken into account for the medicinal plant preparations administered via the oral route. In this study, we aimed to investigate the in vitro antibacterial activity of some common Vietnamese eligible herbs and traditional medicinal plants against B. pseudomallei. The stability of the antibacterial activity was assessed after treatment at different temperatures and after exposure to stimulated gastric conditions. The antibacterial spectrum, bactericidal activity, and cell cytotoxicity of the samples were also investigated.
Methods
Sample collection and processing
During the autumn of 2019, 18 eligible herbs and 21 medicinal plant samples were collected to test for the in vitro antimicrobial activity against B. pseudomallei. The samples were selected based on the encyclopedia of the Vietnamese traditional medicinal plants [24, 25], the customary usages suggested by local traditional healers, and the popular distribution of the medicinal plants. Certain parts of the herbs and plants were collected, including leaf, flower, fruit, bulb, or the whole of the plant. The eligible herbs daily consumed as a spice of foods and meals were purchased from supermarkets. The traditional medicinal plants were gathered from household gardens or forest conservation zones in suburban areas of Hanoi, a capital located in the north of Vietnam. These samples were transferred to the laboratory within a day, washed several times with distilled water, and blotted with clean paper towels to eradicate the residue of distilled water. The plant identification was based on morphological characteristics. Scientific names of the herb and plants were listed using the Angiosperm Phylogeny Group IV system for flowering plants [26] or cladistic analysis of Kenrick and Crane [27] for vascular plants. The plant samples were deposited at the Department of Bio-geography, Institute of Geography, Vietnam Academy of Science and Technology, Hanoi.
For the eligible herbs, fresh materials were grounded homogeneously using a portable electric blender. The homogenized samples were squeezed using a double-layer cloth bag. The obtained juices were treated at different temperatures of 25, 70, and 100 °C for an hour. The juices were then centrifuged at 3500 g for 10 min. The obtained supernatants were filtrated through 0.22-µm pore size membrane filters before further in vitro tests as described below. A part of filtrates was dry at 70 °C until constant weight that served for concentration calculation.
In order to compare the antimicrobial activity between the fresh herb juices and dry plant extracts, the collected medicinal plants were processed as follows: the fresh plant materials were dried in a dehumidifying chamber at room temperature until constant weight. The dried plant samples were pulverized into fine powders. An equal amount of distilled water that evaporated during the dehumidification was added to the fine powders and the plant pastes were treated at different temperatures of 25, 70, and 100 °C for an hour. After squeezing through a double-layer cloth bag, the aqueous extracts were then centrifuged at 3500 g for 10 min and filtrated as described above.
Bacterial strains and culture conditions
Six B. pseudomallei strains designated as VTCC 70001, VTCC 70018, VTCC 70027, VTCC 70156, VTCC 70157, and VTCC 70158 were used in this study. The strain selection was based on the bacterial sequence type (ST) commonly found in the collection of Vietnamese B. pseudomallei strains published in the public databases for molecular typing and microbial genome diversity (https://pubmlst.org/bpseudomallei/) [28]. These strains were isolated from both clinical and environmental samples during the nationwide melioidosis surveillance in the last several years [29]. Additionally, seven other enteric or foodborne bacteria, including Staphylococcus aureus VTCC 70159, Listeria monocytogenes VTCC 70147, Escherichia coli VTCC 70160, Salmonella enterica VTCC 70080, Aeromonas dhakensis VTCC 70106, Vibrio vulnificus VTCC 70092, and Campylobacter jejuni VTCC 70176, were selected for testing of the antimicrobial spectrum. These strains were routinely isolated from clinical specimens and the bacterial species were identified using biochemical characteristics and the 16S rDNA sequence analysis. Information of all tested bacterial strains is provided in Table 1.
From frozen stocks, the bacterial strains were streaked on Columbia agar supplemented with 5% sheep blood. After overnight incubation at 37 °C, individual colonies of the fresh cultures were suspended in 0.9% sterile saline solution to a 0.5 McFarland standard. The resulting bacterial cell suspensions were further used for antibacterial assays as described below. All of the testing bacterial species were incubated aerobically, except C. jejuni which was incubated at the microaerobic condition of 10% CO2, 5% O2, and 85% N2 using an anaerobic chamber (Bactrox Hypoxia chamber, Shel Lab, USA). All of the working steps with the viable bacteria were performed in a class II biological safety cabinet in the restricted area. The hazardous biological agents and materials were completely autoclaved and managed following the safety regulations of the institute.
Antibacterial activity assays
Antibacterial activity of the herb juices and aqueous plant extracts was determined by broth microdilution method, following the guideline of the Clinical and Laboratory Standards Institute [30]. The method was performed in the sterile 96-well plates. Briefly, 50 µl of each herb juice or aqueous plant extract was added into wells at the first plate column while 25 µl of sterile distilled water was added into the other wells. A serial twofold dilution of the samples was carried out by multi-channel pipetting. Then, an equal amount (25 µl) of double-strength cation-adjusted Mueller Hinton broth (Becton, Dickinson and Company, USA) was added into the wells. To inoculate the bacterium, 100 µl of the 0.5 McFarland bacterial cell suspension was diluted into 4.9 ml of cation-adjusted Mueller Hinton broth. An equal amount (50 µl) of this bacterial seed was added into all wells, except for the negative control wells. After incubation of the plates at 37 °C for 24 h, minimal inhibitory concentration (MIC) of the herb juices or aqueous plant extracts was determined by the lowest dilution that prevented the growth of the tested bacterium. Minimum bactericidal concentration (MBC) was defined as the minimum dilution of the juices and extracts that no bacterial colonies observed when plating out on Mueller Hinton agar. Meropenem (Sigma Aldrich, USA) and sterile distilled water were used as positive and negative controls in all experiments, respectively. The experiments were repeated at least twice in duplicate.
Antibacterial activity under stimulated gastric conditions
The stability of the antibacterial activity against B. pseudomallei was tested under the simulated gastrointestinal conditions at 37 °C on a rotary shaker, following the USP 41-National Formulary 36 [31]. Briefly, the herb juices or aqueous plant extracts were treated for two hours in a mixture of 35 mM NaCl and 3.2 mg/ml pepsin (Sigma Aldrich, USA) adjusted to pH 2.0 by 0.1 N HCl. The herb juices or aqueous plant extracts were subsequently exposed for four hours to the mimicking digestive intestine mixture of 50 mM KH2PO4 and 10 mg/ml pancreatin (Sigma Aldrich, USA) adjusted to pH 7.0 by 1 N NaOH. Before the antimicrobial activity testing, the treated herb juices or aqueous plant extracts were heated at 99 °C for 10 min in order to inactivate the digestive enzymes. The stability of the antibacterial activity against B. pseudomallei was evaluated by the determination of both MIC and MBC values as described above.
Time-kill kinetics assay
The herb juices or aqueous plant extracts diluted at the MIC, 2× MIC, and 4× MIC values were added with an equal amount of double strength cation-adjusted Mueller Hinton broth. Then, an equal amount of the bacterial seed prepared in cation-adjusted Mueller Hinton broth was added into the test samples. After incubation at 37 °C for 0, 2, 4, 6, and 8 h, the viable bacterial cells, expressed as colony forming unit (CFU) per ml at each dilution, were determined by the plate counting method. Doxycycline and amoxicillin clavulanic acid (2:1) purchased from Sigma Aldrich (USA) were used as positive controls for bacteriostatic and bactericidal activities, respectively [32]. All experiments were performed in duplicate at each dilution.
Cytotoxicity assay
The cytotoxicity of herb juices or aqueous plant extracts was evaluated on three human cell lines of the colon adenocarcinoma HT29, the hepatocellular carcinoma HepG2, and the embryonic kidney HEK293, using the MTT assay. The cell lines were cultured at 37 °C in a humidified atmosphere with 5% CO2. The high glucose (4.5 g/l) Dulbecco’s Modified Eagle’s Medium (DMEM; PAN Biotech, Germany) was used for HEK293 cell, and low glucose (1.5 g/l) DMEM was used for HT29 and HepG2 cells. The culture media were supplemented with 10% fetal bovine serum (FBS) and 1% of penicillin-streptomycin (10,000 U/ml; Gibco, USA). For the MTT assay, 175 µl of cell suspensions were seeded into flat-bottomed 96-well plates at an approximate density of 2 × 104 cells/well. After 24 h of incubation, 25 µl of the diluted herb juices or aqueous plant extracts were added into each well. The cells were further incubated for 24 h. After removing the culture medium, the wells were added with 50 μl of 3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl-2H tetrazolium bromide (MTT; Biobasic, Canada) solution (2 mg/ml) and 50 μl of the fresh serum-free medium. After another incubation for 3 h, the dye solutions were discarded and the wells were added with 100 μl of DMSO. The plates were then incubated in dark for 15 min at room temperature. After gently shaking, the optical density of the wells was read at 490 nm using a microplate reader (800TS BioTek, USA). Appropriate culture medium and DMSO (Sigma-Aldrich, France) were used for negative and positive controls, respectively. All experiments were performed in duplicate. The cytotoxic effect was determined by the inhibitory concentration (IC50) which reduced the cell viability to 50% of the negative control.
Results
Antibacterial activity of herb juices and its thermal stability
Of 18 herb juices tested, 8 (44.5%) samples showed the antibacterial activity against B. pseudomallei VTCC 70157. Only six herb juices showed the bactericidal activity (Table 2 and Additional file 1: Table S1). The herb juice of Allium tuberosum showed the strongest antibacterial activity, with the MIC value at 0.09 mg/ml. The other juices showed a low antibacterial activity, with the MIC range from 1.05 to 4.69 mg/ml. The antibacterial activity of Allium sativum and Curcuma longa was completely lost when treated above 70 °C. The antibacterial activity of A. tuberosum and Allium fistulosum still remained at 70 °C but the MIC values increased greatly from 0.09 to 0.70 mg/ml and 1.83 to 3.24 mg/ml when treated at the boiling temperature of 100 °C, respectively. A slight heat-unstable property was also observed in the juice of Tamarindus indica. Surprisingly, juices of Limnophila aromatica and Paederia lanuginosa only exhibited the antimicrobial activity when treated at high temperatures. The increase of the antimicrobial activity was also observed in the juice of Perilla frutescens, with the MIC decreasing from 2.27 to 1.10 mg/ml (Additional file 1: Table S1).
Antibacterial activity of aqueous medicinal plant extracts prepared at different temperatures
Of 21 aqueous extracts, 17 (80.9%) dry medicinal plants showed the antibacterial activity against B. pseudomallei VTCC 70157. Except for Plumeria rubra, the dry plant materials increased strongly their inhibitory and bactericidal activities when the aqueous extractions were performed at high temperatures, especially at the boiling temperature of 100 °C (Table 2 and Additional file 1: Table S1). At the boiling temperature preparation, 12 aqueous extracts showed the antibacterial activity with the MIC range from 0.21 to 1.40 mg/ml (Table 2). They included the dry leaves of Blechnum orientale, Breynia fruticose, Euphorbia hirta, Euphorbia thymifolia, Excoecaria cochinchinensis, Mangifera indica, Phyllanthus amarus, Psidium guajava, Punica granatum, Rhodomyrtus tomentosa, Rosa odorata, and Schima wallichii. The dry leaves of the other five plant species showed less antibacterial activity, with the MIC range from 1.89 to 13.22 mg/ml (Additional file 1: Table S1).
Stability of antibacterial activity under gastric conditions
Herb juice and aqueous plant extracts with the MIC value below 1.15 mg/ml were selected for further tests (Table 2). Additionally, a common spice of A. sativum (garlic) used in daily meals was also selected. Under gastric conditions of low pH and hydrolytic properties of pepsin and pancreatin, antimicrobial activity of the non-heat treated A. tuberosum juice was decreased from the MIC value of 0.09 to 0.18 mg/ml, but the MBC value still remained. Antimicrobial activity and bactericidal activity of A. sativum juice were also decreased from the MIC value of 3.15 to 12.60 mg/ml and the MBC value of 12.60 to 100.80 mg/ml, respectively (Table 2). At the same treated conditions, aqueous plant extracts of M. indica, P. granatum and R. tomentosa, prepared at 100 °C, still remained the antimicrobial activity against B. pseudomallei. Other plant extracts showed an increase in the MIC values twice, except for B. orientale. The MBC values of these extracts also increased in a range from two to four times, except for S. wallichii.
Spectrum of antibacterial activity
Two herb juices and twelve aqueous plant extracts were further tested for the antibacterial spectrum. All samples showed a relative antibacterial activity against the other five B. pseudomallei strains, in comparison with that of the VTCC 70157 strain (Table 3). The herb juices of A. tuberosum and A. sativum were active against all of the six enteric bacterial species, whereas the aqueous plant extracts showed less antimicrobial activity against L. monocytogenes, E. coli, and S. enterica. C. jejuni was hypersensitive to the juices and aqueous plant extracts. The lowest MIC and MBC values were 0.38 and 0.76 µg/ml (> 0.01 mg/ml) when tested with the A. sativum juice, respectively.
Bactericidal activity
Using time-kill kinetics assay, none of the juices and aqueous plant extracts showed the bactericidal activity against B. pseudomallei at their 1× MIC values over eight hours of exposure (Fig. 1). At the 2× MIC values, viable cell count of B. pseudomallei did not detect after four, four, six, and eight hours of exposure to the aqueous extracts of B. fruticose, R. tomentosa, R. odorata, and S. wallichii, respectively. A slight reduction of the cells was observed in the juice of A. sativum and the aqueous extracts of B. orientale and P. amarus. At the 4× MIC values, A. sativum juice and B. orientale, P. amarus, E. thymifolia, P. guajava, and P. granatum aqueous extracts showed the bactericidal activity. Amoxicillin clavulanic acid started showing the bactericidal activity at its MIC value after six hours of contact with the bacterium. At its 2× MIC and 4× MIC, B. pseudomallei was completely killed after four hours. No bactericidal activity was observed at doxycycline’s 1× MIC, 2× MIC, and 4× MIC.
Cytotoxicity
The juice of A. sativum had the highest cytotoxicity on all human cancer and normal cell lines and its IC50 values were below the MIC value (Table 2). A. tuberosum juice and B. orientale aqueous extract also presented the IC50 value below the MIC values when tested on the HT29 and HepG2 cell lines, respectively. The other aqueous extracts had less cytotoxicity, with the IC50 values above the MIC values on all of the cell lines tested.
Discussion
Traditional medicinal plants are widely used for treating various human diseases, including foodborne illnesses or gastrointestinal infections in suburban areas of the tropics. Investigations on the antibacterial activity of traditional medicinal plants normally use different polar organic solvents to extract the bioactive compounds. The obtained crude extracts are subsequently fractionated to purify the compounds prior to determination of their bioactive properties such as the MIC and MBC values or elucidation of their chemical structure [15]. In contrast, traditional fresh medicinal plants administered via oral route are commonly prepared with cooked foods or the dry medicinal preparations are made by cool infusion, hot infusion, and decoction [20, 24]. These crude extractions require drinking water instead of organic solvents and an additional heat treatment step. Therefore, the efficiency of the extraction method and the stability of the antibacterial activity during the heat treatment or under gastric conditions should be taken into account for the customary practices of the medicinal plants. In a collection of the fresh eligible herbs and dry medicinal plants commonly found in northern Vietnam, we found a higher proportion of the dry medicinal plants (17/21; 80.9%) showing the antibacterial activity against B. pseudomallei, in comparison with that of herb juices (8/18; 44.5%). Of eight fresh eligible herbs showing the antibacterial activity, only one (12.5%) A. tuberosum juice had the MIC value of 0.09 mg/ml. The other seven (87.5%) juices had the MIC values above 1 mg/ml (range from 1.05 to 4.69 mg/ml). In contrast, seven (41.1%) out of seventeen dry medicinal plants had the MIC values above 1 mg/ml when their aqueous extracts were prepared at the boiling temperature (Table 2). The data indicate that the aqueous extracts from dry plant samples were more likely to have strong antibacterial activity than the juices from the fresh eligible herbs.
Previous studies showed that some plant crude extracts remained their antimicrobial activity at 100 °C or even 121 °C, but some others lost their activity after treating just with 60 °C [33, 34]. In our collected herb and plant species, the antibacterial activity of the dry medicinal plants increased remarkably when the aqueous extractions were performed at the boiling temperature. This indicates that the antibacterial compounds of the tested samples are thermal stability and the preparation of these medicinal plants by decoction is likely to be an effective method used for treating bacterial infections in the traditional medicine. The increase in the antibacterial activity was probably due to the higher efficiency of the extraction step at high temperatures [35]. It is important to note that the fresh herb juices from three Allium species decreased or completely lost their antibacterial activity after the heat treatment. This heat-unstable antibacterial activity might limit the usage of these Allium species for treating bacterial infections when cooked well with foods. The Allium species have been known to produce flavonoids and organosulfur compounds such as alliin, methiin, propiin, and isoalliin. Those active compounds may possess both antimicrobial and antioxidant activities [36, 37] but only a decrease in the antioxidant activity was reported after heat treatment in frying oil [37]. Interestingly, the juices of L. aromatic, P. lanuginose, and P. frutescens increased their antimicrobial activity when treated at the boiling temperature. The increase in their antibacterial activity remains unknown but it provides evidence that these herbs, prepared traditionally by cooking or boiling, can be effectively useful for treating enteric bacterial infections. In fact, the indigenous people commonly use the sliced leaves of P. lanuginosa and P. frutescens to cook with chicken eggs and rice soup to treat diarrhea or other digestive disorders, respectively. The dry aerial part of L. aromatic prepared by decoction is used orally to treat various human diseases, including infectious diseases [25].
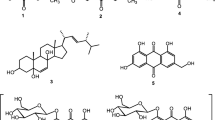
Traditional medicinal plants have been known to possess a wide variety of secondary metabolites (phytocomponents) which display antimicrobial activity against various microbial pathogens. These bioactive compounds are chemically grouped into classes of flavonoids, phenolic acids, quinones, tannins, alkaloids, glycosides, saponins, lectins, steroids, and polypeptides [15]. Due to the presence of hydrolytic enzymes in the human digestive tract and the low pH in the stomach, chemical alteration or degradation of these compounds may occur after exposure to stimulated gastric conditions, resulting in a decrease in their bioactivity [38]. Of 14 herb juices and aqueous plant extracts selected, we found that the antimicrobial activity against B. pseudomallei of three aqueous plant extracts of M. indica, P. granatum, and R. tomentosa was constant under the stimulated gastric conditions, which indicated the gastric stability of the antimicrobial activity. The other samples showed a slight reduction in the inhibitory activity. The decrease in the antibacterial activity of A. tuberosum and A. sativum might be due to a heating step at 99 °C for 10 min to inactivate the hydrolytic enzymes in the stimulated gastric fluid. These data may support the speculation that the traditional practices of the medicinal plants administered via the oral route can treat gastrointestinal infections caused by B. pseudomallei.
Unheated juices of A. tuberosum and A. sativum showed a broad spectrum of antibacterial activity against all tested pathogenic bacteria. Clear inhibition zones were also observed when the antimicrobial activity of the juices was carried out using agar well diffusion method (data not shown). This was in contrast to a study by Panomket et al. [13] who showed no clear zone of methanolic or aqueous extracts of A. sativum (and T. indica) against B. pseudomallei. However, our data are in agreement with the previous study which showed the highest antibacterial activity of A. tuberosum and A. sativum essential oils against five common foodborne pathogens [37]. In contrast to the Allium species, most of the aqueous plant extracts showed less antibacterial activity against E. coli and S. enterica (Table 3) although both bacterial species are Gram-negative bacteria. Even in Gram-positive bacteria, the aqueous samples were more active against S. aureus than L. monocytogens. This might reflect modes of action or killing mechanisms of plant antimicrobials on different targets other than on cell wall components [39]. Except for E. coli and S. enterica, the aqueous plant extracts showed stronger antibacterial activity against other Gram-negative bacteria. This is in contrast to a previous study that showed higher antibacterial activity of methanolic plant extracts against Gram-negative bacteria [14]. Our disagreement may be due to the difference in the extraction method, which used distilled water instead of methanol solvent.
A. sativum (garlic) is a food ingredient that is daily consumed in every meal. In some circumstances, indigenous adults can eat garlic directly to treat sore throat, pharyngitis, and other digestive disorders. In the cytotoxicity test, all of the tested samples showed less toxicity on three cell lines than the garlic juice. In the review by Zhao et al. [40], R. tomentosa is considered as weak cytotoxicity and its IC50 value of the ethanol extract was 15-fold higher than the MIC90 value. In the acute toxicity test, a previous study showed that the aqueous extracts of P. guajava and P. amarus leaves did not induce any mortality or any histological renal and fetal disorders of the treated rats [21]. Using the brine shrimp lethality test, Gyawali et al. [41] showed that the crude methanolic extract of the S. wallichii bark was mildly toxic and it was suggested to use for human consumption for drug purposes. Together with our cytotoxicity test, the data confirm the safety of the selected aqueous plant extracts in the traditional medicine.
Trimethoprim sulfamethoxazole, doxycycline, and amoxicillin clavulanic acid are oral antibiotics currently recommended for the treatment of melioidosis in the eradication phase [1]. Because the MIC of trimethoprim sulfamethoxazole against B. pseudomallei is difficult to determine by broth dilution method [32], thus the other two antibiotics were selected as positive controls in the time-kill kinetics assay. At the 2× MIC value, amoxicillin clavulanic acid completely killed B. pseudomallei after four hours of exposure. The same bactericidal activity was found in the aqueous plant extracts of B. fruticose and R. tomentosa (Fig. 1). At the 4× MIC, the aqueous plant extracts of B. orientale, P. guajava, R. ordorata, and S. wallichii also showed the same bactericidal activity as that of amoxicillin clavulanic acid. R. tomentosa showed the highest bactericidal activity, with a complete killing of B. pseudomallei within two hours of exposure. The data indicate that the bactericidal activity of some aqueous plant extracts is relatively comparable to that of commercial synthetic antibiotics. This provides more evidence on the possible usage of traditional medicinal plants in the treatment of melioidosis.
All of the selected medicinal plants showed the antibacterial activity against B. pseudomallei are commonly found in northern Vietnam, a tropical region where melioidosis is highly endemic [29]. Some plants have been extensively investigated and comprehensively reviewed with many aspects, including the distribution, traditional usage, phytochemical composition, pharmacology, and potential industrial applications in the treatment of human diseases. M. indica, P. granatum, and P. guajava are fruit trees that are cultivated popularly in many countries in the tropical and subtropical climates. In traditional medicine of several countries, the leaves of the plants are mainly used orally or topically to treat diarrhea or skin and wound infections [42, 43]. R. tomentosa is a flowering plant native to Southeast Asia and a part of India and China. The plant is used to treat diarrhea and other non-infectious diseases [40]. E. hirta is popular in the tropical regions and widely used as a decoction or infusion to treat various infectious diseases [44]. E. thymifolia distributes throughout India and the tropics. The plant is used for treating various diseases, including diarrhea and urinary tract infections [45]. P. amarus is widely spread throughout the tropical and subtropical countries and commonly used in the Indian Ajurvedic system of medicine [46]. The plant was reported on the list of traditional medicine plants using for the treatment of salmonellosis in Benin [21]. B. orientale is native to Asia countries, Australia, and Pacific Islands. Proanthocyanidin of the fern has been reported as a potential natural source of antioxidant, antibacterial, and anti-cancer properties [47]. E. cochinchinensis and S. wallichii are also popular distribution in the tropics and used in the traditional medicine. However, very little information related to human health effects has been reported for these medicinal plants. Further investigations on the chemical structures as well as biological properties of the bioactive compounds are needed.
Conclusions
Due to the diverse clinical presentation, melioidosis can manifest clinical signs and symptoms similar to those caused by other enteric bacteria. The disease is highly endemic in the tropics, which concurs with the popular usage of traditional medicinal plants by indigenous people for treating various human diseases. Our study demonstrated that many herbs and medicinal plants commonly distributed in the tropics exhibited the antimicrobial activity against B. pseudomallei and other food-borne or enteric pathogens. Aqueous extracts of B. fruticose, R. tomentosa, B. orientale, P. guajava, R. ordorata, and S. wallichii prepared at the boiling temperature showed a bactericidal activity. Because of heat-stable properties, customary preparations by hot infusion or decoction are effective methods for dry medicinal plants but not for fresh herbs in the treatment of bacterial infections. The herb juices and aqueous plant extracts were less toxicity and their antibacterial activity was relatively stable under the stimulated gastric conditions. Our findings provide an important clue on the potential usage of traditional medicinal plants in the treatment of melioidosis. It also indicates that the current random usage of the plants by indigenous people may contribute to the therapeutic agents in the treatment of the disease infected via the oral route. Due to the popular distribution and safety of these plants, further in vivo investigations are needed in order to explore alternative therapies in the prevention and treatment of the disease.
Availability of data and materials
Data will be available by corresponding author upon reasonable request.
Abbreviations
- 16S rDNA:
-
16S ribosomal deoxyribonucleic acid
- CFU:
-
Colony forming unit
- CLSI:
-
Clinical and laboratory standards institute
- DMEM:
-
Dulbecco’s modified eagle’s medium
- IC:
-
Inhibitory concentration
- MIC:
-
Minimal inhibitory concentration
- MBC:
-
Minimal bactericidal concentration
- ST:
-
Sequence type
- VTCC:
-
Vietnam type culture collection
- MTT:
-
3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl-2H tetrazolium bromide
References
Wiersinga WJ, Virk HS, Torres AG, Currie BJ, Peacock SJ, Dance DAB, Limmathurotsakul D (2018) Melioidosis. Nat Rev Dis Primers 4:17107. https://doi.org/10.1038/nrdp.2017.107
Limmathurotsakul D, Golding N, Dance DA, Messina JP, Pigott DM, Moyes CL, Rolim DB, Bertherat E, Day NP, Peacock SJ, Hay SI (2016) Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol 1:15008. https://doi.org/10.1038/nmicrobiol.2015.8
Currie BJ, Ward L, Cheng AC (2010) The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl Trop Dis 4:e900. https://doi.org/10.1371/journal.pntd.0000900
Limmathurotsakul D, Kanoksil M, Wuthiekanun V, Kitphati R, deStavola B, Day NP, Peacock SJ (2013) Activities of daily living associated with acquisition of melioidosis in northeast Thailand: a matched case-control study. PLoS Negl Trop Dis 7:e2072. https://doi.org/10.1371/journal.pntd.0002072
Limmathurotsakul D, Wongsuvan G, Aanensen D, Ngamwilai S, Saiprom N, Rongkard P, Thaipadungpanit J, Kanoksil M, Chantratita N, Day NP, Peacock SJ (2014) Melioidosis caused by Burkholderia pseudomallei in drinking water, Thailand, 2012. Emerg Infect Dis 20:265–268. https://doi.org/10.3201/eid2002.121891
McRobb E, Kaestli M, Mayo M, Price EP, Sarovich DS, Godoy D, Spratt BG, Currie BJ (2013) Melioidosis from contaminated bore water and successful UV sterilization. Am J Trop Med Hyg 89:367–368. https://doi.org/10.4269/ajtmh.13-0101
Sanchez-Villamil JI, Tapia D, Borlee GI, Borlee BR, Walker DH, Torres AG (2020) Burkholderia pseudomallei as an enteric pathogen: identification of virulence factors mediating gastrointestinal infection. Infect Immun. https://doi.org/10.1128/IAI.00654-20
Goodyear A, Bielefeldt-Ohmann H, Schweizer H, Dow S (2012) Persistent gastric colonization with Burkholderia pseudomallei and dissemination from the gastrointestinal tract following mucosal inoculation of mice. PLoS ONE 7:e37324. https://doi.org/10.1371/journal.pone.0037324
Teparrukkul P, Kongkasame W, Chitsaeng S, Wongsuwan G, Wuthiekanun V, Peacock SJ, Limmathurotsakul D (2017) Gastrointestinal tract involvement in melioidosis. Trans R Soc Trop Med Hyg 111:185–187. https://doi.org/10.1093/trstmh/trx031
Jagtap N, Shah H, Kancharla A, Tandan M, Pal P, Lakhtakia S, Ramchandani M, Reddy DN (2017) Gastrointestinal manifestations of melioidosis: a single center experience. Indian J Gastroenterol 36:141–144. https://doi.org/10.1007/s12664-017-0741-9
Muthu SE, Nandakumar S, Rao UA (2005) The effect of methanolic extract of Tamarindus indica Linn. on the growth of clinical isolates of Burkholderia pseudomallei. Indian J Med Res 122:525–528
Perumal Samy R, Manikandan J, Al Qahtani M (2013) Evaluation of aromatic plants and compounds used to fight multidrug resistant infections. Evid Based Complement Altern Med 2013:525613. https://doi.org/10.1155/2013/525613
Panomketa P, Wanrama S, Srivorasmasa T, Pongpromb N (2012) Bioactivity of plant extracts against Burkholderia pseudomallei. Asian Biomed 6:619–623. https://doi.org/10.5372/1905-7415.0604.100
Vu TT, Kim H, Tran VK, Le Dang Q, Nguyen HT, Kim H, Kim IS, Choi GJ, Kim JC (2016) In vitro antibacterial activity of selected medicinal plants traditionally used in Vietnam against human pathogenic bacteria. BMC Complement Altern Med 16:32. https://doi.org/10.1186/s12906-016-1007-2
Mickymaray S (2019) Efficacy and mechanism of traditional medicinal plants and bioactive compounds against clinically important pathogens. Antibiotics. https://doi.org/10.3390/antibiotics8040257
WHO (2013) Traditional medicine strategy 2014–2023. Hong Kong SAR, China
Sharma A, Flores-Vallejo RDC, Cardoso-Taketa A, Villarreal ML (2017) Antibacterial activities of medicinal plants used in Mexican traditional medicine. J Ethnopharmacol 208:264–329. https://doi.org/10.1016/j.jep.2016.04.045
Vuuren SF (2008) Antimicrobial activity of South African medicinal plants. J Ethnopharmacol 119:462–472. https://doi.org/10.1016/j.jep.2008.05.038
Packer J, Naz T, Yaegl Community E, Harrington D, Jamie JF, Vemulpad SR (2015) Antimicrobial activity of customary medicinal plants of the Yaegl Aboriginal community of northern New South Wales, Australia: a preliminary study. BMC Res Notes 8:276. https://doi.org/10.1186/s13104-015-1258-x
Au DT, Wu J, Jiang Z, Chen H, Lu G, Zhao Z (2008) Ethnobotanical study of medicinal plants used by Hakka in Guangdong, China. J Ethnopharmacol 117:41–50. https://doi.org/10.1016/j.jep.2008.01.016
Legba B, Dougnon V, Deguenon E, Agbankpe J, Senou M, Aniambossou A, Gbaguidi C, Sintondji K, Baba-Moussa L, Dougnon J (2019) Toxicological characterization of six plants of the Beninese Pharmacopoeia used in the treatment of Salmonellosis. J Toxicol 2019:3530659. https://doi.org/10.1155/2019/3530659
Gupta R, Thakur B, Singh P, Singh HB, Sharma VD, Katoch VM, Chauhan SV (2010) Anti-tuberculosis activity of selected medicinal plants against multi-drug resistant Mycobacterium tuberculosis isolates. Indian J Med Res 131:809–813
Mostafa AA, Al-Askar AA, Almaary KS, Dawoud TM, Sholkamy EN, Bakri MM (2018) Antimicrobial activity of some plant extracts against bacterial strains causing food poisoning diseases. Saudi J Biol Sci 25:361–366. https://doi.org/10.1016/j.sjbs.2017.02.004
Do TL (2004) Medical plants and drugs from Vietnam. Medical Publisher House, Hanoi
Do HB, Dang QC, Bui XC, Nguyen TD, Do TD, Pham VH, Vu NL, Pham DM, Pham KM, Doan TN, Nguyen T, Tran T (2006) Medicinal plants and animals in Vietnam. Science and Technics Publishing House, Ha Noi
Group TAP, Chase MW, Christenhusz MJM, Fay MF, Byng JW, Judd WS, Soltis DE, Mabberley DJ, Sennikov AN, Soltis PS, Stevens PF (2016) An update of the Angiosperm Phylogeny Group classification for the orders and families of flowering plants: APG IV. Bot J Linn Soc 181:1–20. https://doi.org/10.1111/boj.12385
Kenrick P, Crane PR (1997) The origin and early diversification of land plants: a cladistic study. Smithsonian Institution Scholarly Press, Washington
MLST (2021) Public databases for molecular typing and microbial genome diversity. https://pubmlst.org/organisms/burkholderia-pseudomallei/. Accessed 20 June 2021
Trinh TT, Nguyen LDN, Nguyen TV, Tran CX, Le AV, Nguyen HV, Assig K, Lichtenegger S, Wagner GE, Do CD, Steinmetz I (2018) Melioidosis in Vietnam: recently improved recognition but still an uncertain disease burden after almost a century of reporting. Trop Med Infect Dis. https://doi.org/10.3390/tropicalmed3020039
CLSI (2015) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; Approved standard-tenth edition. CLSI document M07-A10. Wayne: Clinical and Laboratory Standards Institute
Pharmacopeia US (2018) National Formulary: USP 41-NF 36. In Carbomer Homopolymer; United States Pharmacopeial Convention: Rockville
Dance DA, Wuthiekanun V, Chaowagul W, White NJ (1989) The antimicrobial susceptibility of Pseudomonas pseudomallei. emergence of resistance in vitro and during treatment. J Antimicrob Chemother 24:295–309. https://doi.org/10.1093/jac/24.3.295
Ibrahim N, Kebede A (2020) In vitro antibacterial activities of methanol and aqueous leave extracts of selected medicinal plants against human pathogenic bacteria. Saudi J Biol Sci 27:2261–2268. https://doi.org/10.1016/j.sjbs.2020.06.047
Ginovyan MM (2017) Effect of heat treatment on antimicrobial activity of crude extracts of some Armenian herbs. Chem Biol 51:113–117
Zhang QW, Lin LG, Ye WC (2018) Techniques for extraction and isolation of natural products: a comprehensive review. Chin Med 13:20. https://doi.org/10.1186/s13020-018-0177-x
Putnik P, Gabric D, Roohinejad S, Barba FJ, Granato D, Mallikarjunan K, Lorenzo JM, Bursac Kovacevic D (2019) An overview of organosulfur compounds from Allium spp.: from processing and preservation to evaluation of their bioavailability, antimicrobial, and anti-inflammatory properties. Food Chem 276:680–691. https://doi.org/10.1016/j.foodchem.2018.10.068
Mnayer D, Fabiano-Tixier AS, Petitcolas E, Hamieh T, Nehme N, Ferrant C, Fernandez X, Chemat F (2014) Chemical composition, antibacterial and antioxidant activities of six essentials oils from the Alliaceae family. Molecules 19:20034–20053. https://doi.org/10.3390/molecules191220034
Vermaak I, Viljoen AM, H. HJ, and Vuuren SF, (2009) The effect of simulated gastrointestinal conditions on the antimicrobial activity and chemical composition of indigenous South African plant extracts. S Afr J Bot 75:594–599
Khameneh B, Iranshahy M, Soheili V, Fazly Bazzaz BS (2019) Review on plant antimicrobials: a mechanistic viewpoint. Antimicrob Resist Infect Control 8:118. https://doi.org/10.1186/s13756-019-0559-6
Zhao Z, Wu L, Xie J, Feng Y, Tian J, He X, Li B, Wang L, Wang X, Zhang Y, Wu S, Zheng X (2020) Rhodomyrtus tomentosa (Aiton.): a review of phytochemistry, pharmacology and industrial applications research progress. Food Chem 309:125715. https://doi.org/10.1016/j.foodchem.2019.125715
Gyawali R, Adhikari S, Gautam S, Guragain P, Pokharel S, Pradhan N, Sijapati S, Shrestha TM (2015) Antimicrobial and cytotoxic properties of selected medicinal plants from Kavrepalanchowk. Nepal Banko Janakari 25:15–19
Diaz-de-Cerio E, Verardo V, Gomez-Caravaca AM, Fernandez-Gutierrez A, Segura-Carretero A (2017) Health effects of Psidium guajava L. leaves: an overview of the last decade. Int J Mol Sci. https://doi.org/10.3390/ijms18040897
Vucic V, Grabez M, Trchounian A, Arsic A (2019) Composition and potential health benefits of pomegranate: a review. Curr Pharm Des 25:1817–1827. https://doi.org/10.2174/1381612825666190708183941
Rajeh MA, Zuraini Z, Sasidharan S, Latha LY, Amutha S (2010) Assessment of Euphorbia hirta L. leaf, flower, stem and root extracts for their antibacterial and antifungal activity and brine shrimp lethality. Molecules 15:6008–6018. https://doi.org/10.3390/molecules15096008
Mali PY, Panchal SS (2013) A review on phyto-pharmacological potentials of Euphorbia thymifolia L. Anc Sci Life 32:165–172. https://doi.org/10.4103/0257-7941.123001
Patel JR, Tripathi P, Sharma V, Chauhan NS, Dixit VK (2011) Phyllanthus amarus: ethnomedicinal uses, phytochemistry and pharmacology: a review. J Ethnopharmacol 138:286–313. https://doi.org/10.1016/j.jep.2011.09.040
Lai HY, Lim YY, Kim KH (2017) Isolation and characterisation of a proanthocyanidin with antioxidative, antibacterial and anti-cancer properties from fern Blechnum orientale. Pharmacogn Mag 13:31–37. https://doi.org/10.4103/0973-1296.197659
Acknowledgements
We would like to thank Mr. Minh C. Nguyen and Mrs. Ha T. T. Hoang for their initial works on the sample preparation and antibacterial susceptibility testing. We thank Dr. Tai A. Vu for the plant identification works.
Study involving plants
All eligible herbs and medicinal plants were collected in northern Vietnam. Plant identification was authenticated by Dr. Tai Vu Anh, a botanical membership of the Vietnam National Association of Ecology and Biological Resources and the Vietnam Plant Data Center. Permissions and/or licenses for the study were not required.
Funding
This work was supported by the Vietnam National University, Hanoi under grant no. QG.19.48. We received the funding for study design, sample collection, plant identification and antibacterial activity tests.
Author information
Authors and Affiliations
Contributions
TTT contributed to the design of the study; TTT and TAV collected the samples; TAV identified the plant samples; LNHB, HVN and DTHN performed the experiments and analysis the data; TTT and NXD drafted the paper; all authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Testing of antibacterial activity of 25 other herb juices and aqueous plant extracts against B. pseudomallei VTCC 70157 (ST 46).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Trinh, T.T., Vu, T.A., Bui, L.N.H. et al. Thermal and gastric stability of antimicrobial activity of juices and aqueous extracts prepared from common eligible herbs and traditional medicinal plants against Burkholderia pseudomallei and other enteric bacteria. Futur J Pharm Sci 8, 35 (2022). https://doi.org/10.1186/s43094-022-00424-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-022-00424-6