Abstract
Background
Practitioners’ enrollment, adherence, and retention rates influence estimates of effectiveness in knowledge translation (KT) studies and remain important concerns for implementation researchers. This review aimed to systematically summarize the current evidence on feasibility measures as gauged by enrollment, adherence, and retention rates in KT evaluation studies targeting rehabilitation practitioners treating musculoskeletal disorders (MSDs).
Methods
We searched five electronic databases from the inception to October 2022. We included KT studies that 1) had designs recommended by the Effective Practice and Organisation of Care, 2) targeted rehabilitation practitioners managing patients with MSDs, 3) delivered KT interventions according to the Expert Recommendations for Implementing Change classification, and 4) reported on the feasibility measures (e.g., enrollment, adherence, and retention). Descriptive statistics were conducted to report on study-, practitioners- and intervention-related factors influencing enrollment, adherence, and retention rates. Meta-regression weighted by the sample size of included studies was used to estimate the effect of factors on overall enrollment, adherence, and retention rates.
Results
Findings from 33 KT studies reported weighted enrolment, adherence, and retention rate of 82% (range: 32%-100%), 74% (range: 44%-100%), and 65% (range: 36%-100%) respectively for both intervention and control groups. Factors positively influencing enrollment, adherence, and retention rates included designing short study period with short duration intervention.
Conclusions
Intense (e.g., high frequency, short duration) single KT intervention was more appealing for practitioners. Future evaluation studies should clearly report follow-up data, and practitioners’ prior training, Results may not apply to non-MSD healthcare providers.
Similar content being viewed by others
Background
Musculoskeletal disorders (MSDs) are one of the most common health conditions experienced worldwide and are costly to the healthcare system [1], with one in six adults (15.6%) reporting chronic MSDs [2]. The most common chronic MSDs are osteoarthritis (OA), neck pain (NP), and low back pain (LBP). The World Health Organization estimates that 10% of individuals 60 years or older have significant clinical problems (e.g., functional limitation) that are attributed to OA [3]. Likewise, over 80% of the population experience LBP and NP during their lifetime [4,5,6]. Importantly, MSDs are associated with a high economic burden globally [7,8,9]. In 2010, the Public Health Agency of Canada highlighted that MSDs are associated with a higher economic burden than any other group of diseases, estimated at $37 billion [10].
Rehabilitation practitioners such as physiotherapists (PTs), occupational therapists (OTs), chiropractors (DCs) deliver care to over 11 million Canadians with MSDs, with estimates pointing to an increase to 15 million patients seeking care by 2031 [11]. Despite the availability of clinical practice guidelines to inform practice in rehabilitation [12,13,14,15,16], substantial research-practice gaps among rehabilitation clinicians persist [17,18,19,20]. The lack of adherence to recommended care can lead to negative effects on the health outcomes of individuals and communities and lead to inefficient use of limited health care resources [21, 22]. Knowledge Translation (KT) aims to promote the use of research evidence in healthcare systems [23]. Although, KT researchers evaluated the relative effectiveness of different KT interventions in changing healthcare professionals’ practice behaviour [24, 25], there is uncertainty regarding which KT interventions are likely to be effective in increasing the use of research findings [24, 26]. As KT interventions are multilevel interventions (e.g., professional, patient, or organizational level), other factors that may have impacted the success of the intervention [27, 28]. Low participant enrollment, adherence and retention rates (i.e., maintaining clinicians’ engagement throughout the course and up to the end of a trial) are major factors that can contribute to the success or failure of KT intervention [29] and influence the estimation of the effectiveness of any intervention [30] in healthcare research [31]. Difficulties in participants’ enrollment may lead to untimely delays in study initiation, financial burden, and failure to meet enrollment goals (i.e., underpowered trials) resulting in very expensive trials [31]. Thus, maximizing enrollment, adherence, and retention rates requires thoughtful planning, and specific strategies embedded in the trial process, and careful monitoring [31]. Assessing those rates may help researchers develop more appealing KT interventions that practitioners will more easily accept and sustain into their everyday practices, and improve the design of future trials, and consequently, increase their validity and generalizability [32]. Although successful enrollment and retention strategies have been described in clinical trials focusing on adults [33] and children [34], we are not aware of prior reviews having systematically assessed the enrollment, adherence, and retention rates in KT studies. This systematic review aimed to 1) estimate the enrollment, adherence, and retention rates of KT interventions targeting rehabilitation practitioners in charge of patients with MSDs, and 2) identify factors likely to impact on the enrollment, adherence, and retention rates.
Methods
Searches
A search strategy was developed in collaboration with a health-sciences librarian to ensure that we captured the maximum number of studies in rehabilitation sciences (Supplementary Material 1: Appendix 1). The search strategy was adapted from a previous review from this team [35], using subject headings (MeSH), keywords, and abstract/text words for MSDs, KT, and rehabilitation, and their synonyms. We searched published literature in scientific journals in the following five databases from the inception to October 2022: OVID MEDLINE, EMBASE, PsycINFO, CINAHL, and Cochrane databases, in English language. All identified citations were exported into EndNote after removing duplicates.
Study inclusion and exclusion criteria
Three independent reviewers (DG, OE, KM) screened the titles and abstracts of studies identified by applying the eligibility criteria. The same reviewers then independently assessed full-text reports of potentially eligible studies. Reviewers met periodically to resolve disagreements and reach a consensus on the eligibility of studies at all stages.
Inclusion criteria
Study design
As recommended by the Effective Practice and Organisation of Care (EPOC) systematic reviews [36], we included the following study designs: Randomized Clinical Trials (RCTs), cluster randomized controlled trials, non-randomized controlled trials (NRCTs), or before-and-after studies.
Participants
All types of rehabilitation practitioners (e.g., PTs, OTs, Osteopaths, or DCs) managing patients with MSDs.
Intervention
KT interventions directed toward rehabilitation practitioners were selected according to the Expert Recommendations for Implementing Change (ERIC) classification [37], which provide comprehensive catalogue of KT interventions that can be used in isolation or combination in implementation research and practice (Supplementary Material 1: Appendix 2).
Outcomes
Three feasibility measures were considered: enrollment rate (defined as the proportion of participants who accepted to participate in the study over all eligible participants invited for the study, considering that the number of eligible practitioners was calculated after excluding individuals who did not meet the study’s inclusion criteria), adherence rate (defined as the proportion of participants who completed the intervention over all participants who were assigned to the intervention group), and retention rate (defined as the proportion of participants who completed through to the first follow-up point over the participants who started the study in each group “intervention group [IG] or control group [CG]”).
Exclusion criteria
Studies failing to report follow-up data for the participating practitioners were excluded. Studies published in abstract form, as conference proceedings, or protocol forms were also excluded.
Data extraction strategy
A structured extraction sheet was created to collect and extract data from the eligible studies. We extracted data related to study characteristics (i.e., year of publication, country, study design, study duration, number of the study group, study duration, number of follow-up points, number of outcomes); KT interventions (i.e., type of KT intervention based on ERIC classification, number and duration of the KT interventions, mode of delivery, intensity of the intervention); practitioners (i.e., age, profession and types of MSDs managed; number of practitioners who were approached, eligible to participate, excluded, refused to participate, accepted to participate, and assigned to each study group “if applicable”; number of practitioners who adhered to the KT intervention, and who participated at least in the first follow-up point; and reasons for refusal to participate, and for dropping-out in each study group. The data were extracted by the principal investigator (DG) and reviewed by a second reviewer (OE).
Study quality assessment
Quality assessment was not considered since the focus of this review was on enrollment, adherence, retention rates, and not the effectiveness and effect size of KT interventions likely to be impacted by criteria such as randomization process and missing data [38].
Data synthesis and presentation
Statistical analyses were performed using the Statistical Analysis Systems (SAS version 9.3) [39] guided by two KT experts (AB and SA). Descriptive statistics were conducted to describe variables that possibly affected enrollment, adherence, and retention rates as proportion (%). Moreover, variables were categorized according to their nature and the frequency of data for study characteristics and practitioners- and intervention-related variables described above.
Meta-regression weighted by the sample size [38] of included studies was used to estimate the overall enrollment, adherence, and retention rates. Meta-regression was used since the outcome had a specific range (0–100%). The study, intervention, and practitioners-related variables aforementioned were used as the factors (i.e., predictors) of the enrollment, adherence, and retention rates. The overall enrollment and retention rates were calculated for intervention and control groups, and the overall adherence rate was estimated for intervention groups only. A meta-regression model was used to assess the correlation between the potential variables and enrollment, adherence, and retention rates. These three rates were treated as continuous variables. A p-value of less than 0.05 was considered as statistically significant.
Results
Descriptive statistics
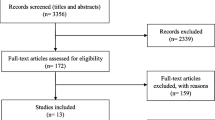
The search strategy yielded 6088 records after duplicate removal. Screening for titles and abstracts identified 105 potentially eligible articles of which 33 studies met our inclusion criteria [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69] (See Fig. 1. PRISMA flowchart). Table 1 provides a description of the study- practitioners- and KT intervention characteristics of the included studies.
Studies’ characteristics
The included studies were published between 2004 and 2022 in Europe (61%, n = 20), North America (27%, n = 9), Australia (9%, n = 3) or elsewhere (3%, n = 1). Most of the studies (61%, n = 20) were controlled trials, such as RCT (n = 8) [40, 43, 46, 49, 53, 55, 56, 68], cluster-RCT (n = 5) [42, 58, 59, 61, 67], pragmatic RCT (n = 1) [45], prospective controlled trials (CT) (n = 1) [52], single-blind RCT (n = 1) [47], and non-RCT (n = 1) [44], mixed methods trial (n = 1) [70, 71], and before-and-after control study (n = 1) [41]. The remaining studies were before-and-after studies (39%, n = 13) [48, 50, 51, 54, 57, 60, 62,63,64,65,66, 69, 72]. Study duration ranged from 2 to 26 months. The median of the follow-up points was one follow-up. More than half (57%, n = 19) [40,41,42, 44, 45, 47, 49, 51,52,53,54, 57, 58, 61, 65, 67,68,69, 71] of the included studies had one follow-up point or two follow-up points (30%, n = 10) [43, 46, 50, 55, 56, 59, 60, 64, 66, 72], while few studies had more than two follow-up points (12%, n = 4) [48, 62, 63, 70].
Practitioners’ characteristics
The practitioners’ mean age was provided in 21 studies [40,41,42,43, 45, 47,48,49,50, 53,54,55,56,57, 60,61,62, 65, 67, 70, 72]; ranging from 28 to 47.5 years for intervention groups (x̅ = 40 years; SD = 5.1) and 33 to 54.3 years for control groups (x̅ = 43 years; SD = 4.7). Most of the studies targeted PTs (70%, n = 23) [40, 42,43,44, 47, 48, 50,51,52,53,54,55,56, 58,59,60,61,62, 65, 66, 68, 69, 72]. The remaining studies targeted a mixed types of practitioners (PTs, OTs, DCs) (13%, n = 4) [49, 57, 63, 64], DCs (12%, n = 4) [41, 46, 67, 70], OTs (3%, n = 1) [45], or osteopaths (3%, n = 1) [71]. The types of disorders includes back pain (45%, n = 15) [41,42,43, 48,49,50, 60,61,62,63, 65, 68, 70,71,72], MSKs in general (27%, n = 9) [44,45,46, 51,52,53,54, 59, 69], NP (18%, n = 6) [40, 47, 57, 58, 66, 67], and OA (6%, n = 2) [55, 56], and rheumatoid arthritis (3%, n = 1) [64].
KT interventions’ characteristics
Based on the ERIC classification [37], the predominant type of KT interventions were educational meetings (97%, n = 32) [40,41,42,43,44,45,46,47,48, 50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72], distribution of educational materials (58%, n = 19) [40,41,42,43,44,45, 48, 49, 51, 52, 54,55,56, 58, 60, 61, 63, 64, 70], audit and feedback (30%, n = 10) [40, 42, 45, 48, 53, 54, 56, 60,61,62], local opinion leaders (24%, n = 8) [41, 51, 56,57,58,59, 62, 70], reminders (21%, n = 7) [44,45,46, 52, 53, 62, 70], facilitation (15%, n = 5) [40, 47, 55, 61, 68], educational outreach visits (12%, n = 4) [40, 41, 58, 62], ongoing consultation (12%, n = 4) [40, 44, 52, 69], and developing centralize technical assistance (12%, n = 4) [44, 52, 60, 72]. Developing educational materials [44, 64, 69], and creating a learning collaborative [45, 60, 69] were used in equal frequency (9%, n = 3). Providing clinical supervision [40, 60] and intervening with patients to enhance adherence [44, 64] (6%, n = 2), preparing patients to be active participants [52], local consensus discussions [60], conducting ongoing training [69], and using mass media [41] (3%, n = 1) were uncommon (Table 2). An equal proportion of studies combined two to three interventions (42%, n = 14) [42, 43, 46,47,48, 51, 53,54,55, 57, 59, 63, 68, 72] or more than three interventions (39%, n = 13) [40, 41, 44, 45, 52, 56, 58, 60,61,62, 64, 69, 70]. Few studies employed a single intervention (18%, n = 6) [49, 50, 65,66,67, 71]. The majority of the studies delivered the KT intervention in person (76%, n = 25) [40,41,42,43,44,45,46,47,48, 50,51,52,53,54,55,56,57,58,59,60,61,62, 65, 66, 72] or online (21%, n = 7) [63, 64, 67,68,69,70,71]. Only one study used postal dissemination (3%, n = 1) [49].
The other groups (named as control groups) either received no intervention (n = 6) [41, 44, 49, 52, 55, 71], or educational interventions (n = 5) (e.g., external coach [61], opinion leader, audit and feedback [56], practicing skills [45], peer assessment approach [53], and outreach visit, clinical supervision, ongoing consultation [40]), educational materials only (n = 4) [42, 58, 67, 70], less frequent educational sessions (n = 3) [43, 47, 68], or a similar intervention but on different topics (n = 2) [46, 59].
Enrollment, adherence, and retention data
-
1)
Enrollment rate: Overall, 7146 eligible practitioners from 27 KT studies were invited to participate, of whom 5880 agreed to participate [40, 43,44,45,46,47,48,49, 51,52,53, 55, 56, 58,59,60,61,62, 64,65,66,67,68, 70,71,72]. The overall unweighted enrollment rate was 84% and the weighted enrollment rate was 82%, ranging from 32% [51] to 100% in eleven studies [40, 43, 49, 59,60,61, 65, 67, 68, 71, 72], including 8 controlled trials (CTs) [40, 43, 49, 59, 61, 67, 68, 71] and 3 before-and-after studies [60, 65, 72].
-
2)
Adherence rate: The included studies reported the number of practitioners who participated in the educational meetings only, not for every type of KT interventions separately. Thus, the adherence rate was calculated for educational meetings only, however, the calculated adherence rate can well exemplify the adherence rate for the other associated KT interventions in each study as educational meetings were mostly delivered concurrently with other intervention such as distribution of education materials, local opinion leaders, facilitation, audit and feedback, etc. Overall, 4775 practitioners were assigned to attend the educational meetings; 3537 did in fact attend as per protocol, with an overall unweighted adherence rate of 88% and a weighted adherence rate of 74% (73% for before-and-after studies [48, 51, 60, 62,63,64,65,66, 69, 72] and 78% for controlled trials [40, 43,44,45,46,47, 49, 52, 53, 55, 56, 58, 59, 61, 67, 68, 70, 71]). A 100% adherence was reached in 14 studies [40, 43, 47, 48, 50, 51, 53, 54, 57,58,59, 65, 70, 72], of which half were controlled trials [40, 43, 47, 53, 58, 59, 70]. The length of educational meetings ranged from 1 to 8 h. However, the lowest adherence (44%) was observed in a before-and-after study targeting individuals with LBP [63]. The educational sessions was available for online browsing for up to 3 weeks.
-
3)
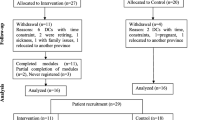
Retention rate: The number of practitioners who completed the first follow-up point was reported in 28 studies (before-and-after studies [n = 9] [51, 54, 57, 62, 63, 65, 66, 69, 72] and controlled trials [n = 19] [40, 42,43,44,45,46,47, 49, 52, 53, 55, 56, 58, 59, 61, 67, 68, 70, 71]). For before-and after studies, 1031 practitioners out of 2094 completed the first follow-up point, with a retention rate of 49% (range: 36% to 100%). For controlled trials, the retention rate was 80% for interventions groups (1672 / 2085) and 81% for control groups (1494 / 1838), with an overall rate of 81% for both groups. The overall unweighted retention rate across all studies was 85% and the weighted retention rate was 65%, ranging from 36% in a before-and-after study targeting mixed types of practitioners [63] to 100% in 7 studies, including 3 CTs [40, 43, 47] and 4 before-and-after studies [54, 65, 69, 72]. Figures 2, 3, and 4 present forest plots for the enrollment, adherence, and retention rates.
Reasons for refusal to participate
Only 8 studies [42, 45, 48, 55, 56, 62, 67,68,69] (27%) reported on the reasons for refusing to participate, namely lack of time (n = 4) [45, 48, 56, 68], lack of interest (n = 6) [42, 45, 48, 56, 62, 67], having a health condition preventing them from participating (n = 3) [45, 55, 67], or unavailability during the study time (n = 2) [56, 69]. Other reasons reported only once were distance from the intervention site [56], holidays [56], other priorities [56], work obligations [68], work schedule conflict [55, 68], moved out of country [67], fail to submit consent [45], retired [67], joining politics [67], and invalid address [67].
Reasons for drop outs
Thirteen studies [42, 44, 45, 52, 53, 56, 57, 59, 61, 62, 67,68,69] (43%) reported the reasons for participants’ drop out throughout the course of the studies after consenting to participate, including: personal life changes (n = 9) (i.e., change of job, retirement, maternal leave or pregnancy) [42, 45, 53, 56, 57, 59, 62, 67, 68], lack of time (n = 5) [42, 53, 56, 57, 67], unknown reason (n = 3) [42, 56, 61], work conflict (n = 3) [45, 56, 69], unable to contact the participant (n = 3) [44, 52, 57], lack of interest (n = 2) [42, 45], lack of compliance (n = 2) [62, 69], being out of town (n = 1) [67], and transportation problem (n = 1) [45].
Factors influencing enrollment, adherence, and retention rates
In general, the meta-regression showed that all the aforementioned factors (i.e., variables related to studies, interventions, and practitioners) significantly affected the rates of enrollment, adherence, and retention. All comparisons were significant at P-value < 0.0001 (Table 3).
-
1)
Factors influencing enrollment rate: For study-related factors, the enrollment rate was 12% higher in Europe compared to North America. Further, before-and-after studies had about 12% lower enrollment rate compared with controlled trials; implementing a study with more than one study group was associated with a 12% higher enrollment rate, while having more than one follow-up point was associated with an 11% greater enrollment rate. For practitioners-related factors, enrollment rate was higher for mixed types of MSDs practitioners by 15% compared to delivering intervention to single type of practitioners (e.g., OTs, PTs, DCs). Also, enrollment rate was higher for practitioners managing BP and NP by 33% and 19%, respectively, compared to practitioners who manage mixed type of MSDs. As for KT intervention-related factors, enrolment rate was lower when employing two to three interventions, or more than three interventions (38% and 16%) higher respectively compared to employing single intervention; but 16% higher when delivering KT intervention online (virtually) compared to in-person; 19% higher when delivering educational meeting for more than 4 h; and 29% higher when conducting the educational meetings more than one time.
-
2)
Factors influencing adherence rate: Interestingly, adherence rate for study-related factors was 28% lower in Europe when compared to North America, 13% lower when implementing a study for over 6 months; 11% lower when there was more than one follow-up point; but 27% higher when measuring more than two professional outcomes. For the practitioners-related factors, adherence rate was lower when recruiting mixed types of practitioners, DCs and DOs, OTs, compared to PTs by 32%, 17%, and 5%, respectively. Also, adherence rate was higher for practitioners managing NP by 13%, and lower by 11% for practitioners managing BP, both compared to practitioners who manage mixed type of MSDs. As for the KT intervention-related factors, adherence rate was 22% lower when employing two to three interventions; 32% lower when delivering KT intervention online compared to in-person mode; but 16% greater when implementing a meeting length more than 4 h; 12% higher when conducting the educational meetings more than one time; and 29% higher when delivering the KT intervention for a long period (e.g., 1 month up to 6 months).
-
3)
Factors influencing retention rate: Similarly for study-related factors, retention rate was 17% higher in other countries (i.e., Australia) compared to North America. Retention rate was 31% lower when in before-and-after study compared to controlled trials; 22% lower when implementing a study for over 6 months; but 31% greater when implementing a study in more than one study group. The retention rate was also 28% lower when having more than one follow-up point; and 14% higher when measuring more than two professional outcomes. Concerning the practitioners-related factors, retention rate was 16% higher when recruiting OTs, but lower 15% when recruiting mixed types of MSKs practitioners compared to recruiting PTs. Also, retention rate was lower for practitioners managing BP by 12% compared to practitioners who manage mixed type of MSDs. As for the KT intervention-related factors, retention rate was 31% and 13% lower when employing two to three interventions or more than three interventions vs employing a single intervention, respectively. Compared to in-person mode of delivery, retention rate was also 35% lower for online KT interventions, but 15% higher for postal dissemination. Retention rate was 13% greater when conducting the educational meetings more than one time and 29% higher when delivering the KT intervention for a long period (e.g., 1 month up to 6 months).
Discussion
To our knowledge, this is the first review estimating the enrolment, adherence, and retention rates of KT interventions targeting rehabilitation practitioners managing patients with MSDs. Results of the current review showed high enrolment rate (82%) in KT studies, and relatively high adherence (74%) and retention rates (65%) across studies.
This review supported that designing a study with more than one group of practitioners with a controlled arm is associated with higher feasibility rates. Similar findings were reported by Lixin Song et al. [74] when examining the enrollment and retention rates clinical trials of patients with cancer and their caregivers. Studies of shorter period (less than 6 months) with only one follow-up point with multiple outcome measures were associated with higher feasibility rates. These findings are possibly explained by the difficulties for practitioners to commit to their regular work schedule over a long period, thereby limiting their ability to report outcomes over multiple follow-up points.
We uncovered a number of appealing intervention-related features for rehabilitation practitioners that seems to promote all three feasibility measures. First, employing a single intervention for a short period of time (1 month up to 6 months) is significantly associated with the higher rates. Systematic reviews of KT studies have suggested that single active KT interventions may be as effective as multi-component intervention in changing practice [26, 75,76,77]. The complexity of interventions may dampen the key messages and diminish the ability of practitioners to digest the presented information [78]. Previous studies reported a higher enrollment rate when recruiting participants for studies with ≥ 4 months intervention duration [74, 79]. Second, implementing a long educational meeting (more than 4 h) for more than one time is associated with higher rates; this possibly means that practitioners prefer for instance to concentrate on a full day workshop offered multiple times (i.e., long-term engagement), instead of having several short meetings during their busy working day when being exposed to the content of the KT intervention. Lastly, delivering KT intervention virtually or in-person mode provided mixed results with virtual mode being associated with a higher enrolment rate, whereas in-person mode was associated with greater adherence and retention rates; these findings support that online interventions could be considered as time and effort saving modes of delivery. Feasibility rates don’t seem to be harmonically affected by the practitioners’ profession or the type of MSDs they manage. Considering those intervention-related factors may secure higher practitioners’ involvement in the KT studies for longer duration.
Strengths and limitations
This systematic review followed rigorous methodology, including a comprehensive search strategy developed in collaboration with a medical science librarian, the use of multiple electronic databases. However, this review is not without limitations. First, several studies failed to report on the number of practitioners who were eligible to participate in the study. Second, other variables that could be influential, such as practitioners’ educational backgrounds and practitioners’ beliefs in KT interventions, could not be included in the analyses as sufficient information on these variables was not available. Third, assessing the impact of each type of KT interventions separately on the feasibility rates was not possible due to the overlapping of the KT interventions in each study. Fourth, the included studies fail to reported the number of participants received each KT intervention separately. Finally, this review was restricted to KT interventions targeting MSDs rehabilitation practitioners only. Thus results may not apply to other healthcare disciplines.
Conclusion
This systematic review identified 33 studies employing KT interventions to promote the uptake of research evidence by MSDs rehabilitation practitioners, including PTs, OTs, DCs, and osteopaths. Findings showed that enrolment, adherence, and retention rates ranged between 65 and 82% across the KT studies. Moreover, this review showed that single intense (e.g., high frequency, short duration) KT intervention was more appealing for practitioners. Interventions which require less effort and less commitment, and which save participants’ time have higher feasibility rates. KT researchers should consider the time required from healthcare practitioners to participate in a KT studies to maximize the feasibility rates, and consequently increase the generalizability of their findings.
Availability of data and materials
N/A
Abbreviations
- CTs:
-
Controlled Trials
- DCs:
-
Chiropractors
- EPOC:
-
Effective Practice and Organisation of Care
- ERIC:
-
Expert Recommendations for Implementing Change
- KT:
-
Knowledge Translation
- LBP:
-
Low back pain
- MSDs:
-
Musculoskeletal Disorders
- NP:
-
Neck pain
- NRCTs:
-
Non-Randomized Controlled Trials
- OA:
-
Osteoarthritis
- OTs:
-
Occupational Therapists
- PTs:
-
Physiotherapists
- RCTs:
-
Randomized Clinical Trials
References
Sebbag E, Felten R, Sagez F, Sibilia J, Devilliers H, Arnaud L. The world-wide burden of musculoskeletal diseases: a systematic analysis of the World Health Organization Burden of Diseases Database. Ann Rheum Dis. 2019;78(6):844–8.
Parsons S, Ingram M, Clarke-Cornwell A, Symmons D. A Heavy Burden: the occurrence and impact of musculoskeletal conditions in the United Kingdom today. 2011.
Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–56.
Hogg-Johnson S, van der Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther. 2009;32(2):S46–60.
Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. Clin Spine Surg. 2000;13(3):205–17.
Côté P, Cassidy JD, Carroll L. The treatment of neck and low back pain: who seeks care? who goes where? Med Care. 2001;39(9):956–67.
Hayden J, Chou R, Hogg-Johnson S, Bombardier C. Systematic reviews of low back pain prognosis had variable methods and results—guidance for future prognosis reviews. J Clin Epidemiol. 2009;62(8):781-96.e1.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2224–60.
Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20.
santé. Icdisl. Tendances des dépenses nationales de santé, 1975 à 2013. 2013.
Group. COCS. Arthritis Community Research and Evaluation Unit. Building a collective policy agenda for musculoskeletal health and mobility. 2010. http://www.cihr-irsc.gc.ca/e/27028.html.
Burridge J, Murphy MA, Buurke J, Feys P, Keller T, Klamroth-Marganska V, et al. A systematic review of international clinical guidelines for rehabilitation of people with neurological conditions: what recommendations are made for upper limb assessment? Front Neurol. 2019;10:567.
Jolliffe L, Lannin NA, Cadilhac DA, Hoffmann T. Systematic review of clinical practice guidelines to identify recommendations for rehabilitation after stroke and other acquired brain injuries. BMJ Open. 2018;8(2):e018791.
Ni M, Hazzard JB, Signorile JF, Luca C. Exercise guidelines for gait function in Parkinson’s disease: a systematic review and meta-analysis. Neurorehabil Neural Repair. 2018;32(10):872–86.
Pogrebnoy D, Dennett A. Exercise programs delivered according to guidelines improve mobility in people with stroke: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2020;101(1):154–65.
Tomaschek R, Gemperli A, Rupp R, Geng V, Scheel-Sailer A. A systematic review of outcome measures in initial rehabilitation of individuals with newly acquired spinal cord injury: providing evidence for clinical practice guidelines. Eur J Phys Rehabil Med. 2019;55(5):605–17.
Metzler MJ, Metz GA. Analyzing the barriers and supports of knowledge translation using the PEO model. Can J Occup Ther. 2010;77(3):151–8.
Ellen ME, Lavis JN, Ouimet M, Grimshaw J, Bédard P-O. Determining research knowledge infrastructure for healthcare systems: a qualitative study. Implement Sci. 2011;6(1):60.
King G, Wright V, Russell DJ. Understanding paediatric rehabilitation therapists’ lack of use of outcome measures. Disabil Rehabil. 2011;33(25–26):2662–71.
Camden C, Swaine B, Tétreault S, Carrière M. Going beyond the identification of change facilitators to effectively implement a new model of services: lessons learned from a case example in paediatric rehabilitation. Dev Neurorehabil. 2011;14(4):247–60.
Straus SE, Tetroe J, Graham I. Defining knowledge translation. CMAJ. 2009;181(3–4):165–8.
Chalmers I. If evidence-informed policy works in practice, does it matter if it doesn’t work in theory? Evid Policy. 2005;1(2):227–42.
LaPlante M, Carlson D. National Institute on Disability and Rehabilitation Research. Disability in the United States: prevalence and causes. 1992.
Scott SD, Albrecht L, O’Leary K, Ball GD, Hartling L, Hofmeyer A, et al. Systematic review of knowledge translation strategies in the allied health professions. Implement Sci. 2012;7(1):1–17.
Rebbeck T, Macedo LG, Maher CG. Compliance with clinical guidelines for whiplash improved with a targeted implementation strategy: a prospective cohort study. BMC Health Serv Res. 2013;13(1):213.
LaRocca R, Yost J, Dobbins M, Ciliska D, Butt M. The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health. 2012;12(1):1–15.
LaRocca R, Yost J, Dobbins M, Ciliska D, Butt M. The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health. 2012;12(1):751.
Sudsawad P. A conceptual framework to increase usability of outcome research for evidence-based practice. Am J Occup Ther. 2005;59(3):351–5.
Bhattacharyya OK, Estey EA, Zwarenstein M. Methodologies to evaluate the effectiveness of knowledge translation interventions: a primer for researchers and health care managers. J Clin Epidemiol. 2011;64(1):32–40.
Pigott TD. Missing predictors in models of effect size. Eval Health Prof. 2001;24(3):277–307.
Cui Z, Seburg EM, Sherwood NE, Faith MS, Ward DS. Recruitment and retention in obesity prevention and treatment trials targeting minority or low-income children: a review of the clinical trials registration database. Trials. 2015;16(1):564.
Wittes J. Missing inaction: preventing missing outcome data in randomized clinical trials. J Biopharm Stat. 2009;19(6):957–68.
Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28.
Schoeppe S, Oliver M, Badland HM, Burke M, Duncan MJ. Recruitment and retention of children in behavioral health risk factor studies: REACH strategies. Int J Behav Med. 2014;21(5):794–803.
Zoubi FMA, Menon A, Mayo NE, Bussières AE. The effectiveness of interventions designed to increase the uptake of clinical practice guidelines and best practices among musculoskeletal professionals: a systematic review. BMC Health Serv Res. 2018;18(1):435.
Taxomony E. Effective Practice and Organisation of Care (EPOC). 2015.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):1–14.
Arafah AM, Bouchard V, Mayo NE. Enrolling and keeping participants in multiple sclerosis self-management interventions: a systematic review and meta-analysis. Clin Rehabil. 2017;31(6):809–23.
Inc SI. SAS Products, SAS® Enterprise Guide®. 2013.
Cleland JA, Fritz JM, Brennan GP, Magel J, Jull G. Does continuing education improve physical therapists’ effectiveness in treating neck pain? A randomized clinical trial...Including commentary. Phys Ther. 2009;89(1):38–50.
Ammendolia C, Hogg-Johnson S, Bombardier C, Pennick V, Glazier R. Implementing evidence-based guidelines for radiography in acute low back pain a pilot study in a chiropractic community. J Manipulative Physiol Ther. 2004;27(3):170–9.
Bekkering GE, Hendriks HJ, van Tulder MW, Knol DL, Hoeijenbos M, Oostendorp RA, et al. Effect on the process of care of an active strategy to implement clinical guidelines on physiotherapy for low back pain: a cluster randomised controlled trial. Qual Saf Health Care. 2005;14(2):107–12.
Beneciuk JM, George SZ. Pragmatic implementation of a stratified primary care model for low back pain management in outpatient physical therapy settings: two-phase, sequential preliminary study. Phys Ther. 2015;95(8):1120–34.
Bernhardsson S, Larsson ME, Eggertsen R, Olsén MF, Johansson K, Nilsen P, et al. Evaluation of a tailored, multi-component intervention for implementation of evidence-based clinical practice guidelines in primary care physical therapy: a non-randomized controlled trial. BMC Health Serv Res. 2014;14(1):105.
Buchanan H, Siegfried N, Jelsma J, Lombard C. Comparison of an interactive with a didactic educational intervention for improving the evidence-based practice knowledge of occupational therapists in the public health sector in South Africa: a randomised controlled trial. Trials. 2014;15(1):1–11.
Bussières AE, Laurencelle L, Peterson C. Diagnostic imaging guidelines implementation study for spinal disorders: a randomized trial with postal follow-ups. J Chiropractic Educ. 2010;24(1):2–18.
Chipchase LS, Cavaleri R, Jull G. Can a professional development workshop with follow-up alter practitioner behaviour and outcomes for neck pain patients? A randomised controlled trial. Man Ther. 2016;25:87–93.
Demmelmaier I, Denison E, Lindberg P, Åsenlöf P. Tailored skills training for practitioners to enhance assessment of prognostic factors for persistent and disabling back pain: four quasi-experimental single-subject studies. Physiother Theory Pract. 2012;28(5):359–72.
Evans DW, Breen AC, Pincus T, Sim J, Underwood M, Vogel S, et al. The effectiveness of a posted information package on the beliefs and behavior of musculoskeletal practitioners: the UK chiropractors, osteopaths, and musculoskeletal physiotherapists low back pain managemENT (COMPLeMENT) randomized trial. Spine. 2010;35(8):858–66.
Fruth SJ, Van Veld RD, Despos CA, Martin RD, Hecker A, Sincroft EE. The influence of a topic-specific, research-based presentation on physical therapists’ beliefs and practices regarding evidence-based practice. Physiother Theory Pract. 2010;26(8):537–57.
Gross DP, Lowe A. Evaluation of a knowledge translation initiative for physical therapists treating patients with work disability. Disabil Rehabil. 2009;31(11):871–9.
Käll I, Larsson MEH, Bernhardsson S. Use of outcome measures improved after a tailored implementation in primary care physiotherapy: a prospective, controlled study. J Eval Clin Pract. 2016;22(5):668–76.
Maas MJ, van der Wees PJ, Braam C, Koetsenruijter J, Heerkens YF, van der Vleuten CP, et al. An innovative peer assessment approach to enhance guideline adherence in physical therapy: single-masked, cluster-randomized controlled trial. Phys Ther. 2015;95(4):600–12.
Overmeer T, Boersma K, Main CJ, Linton SJ. Do physical therapists change their beliefs, attitudes, knowledge, skills and behaviour after a biopsychosocially orientated university course? J Eval Clin Pract. 2009;15(4):724–32.
Peter W, van der Wees PJ, Verhoef J, de Jong Z, van Bodegom-Vos L, Hilberdink WK, et al. Effectiveness of an interactive postgraduate educational intervention with patient participation on the adherence to a physiotherapy guideline for hip and knee osteoarthritis: a randomised controlled trial. Disabil Rehabil. 2015;37(3):274–82.
Peter WF, van der Wees PJ, Verhoef J, de Jong Z, van Bodegom-Vos L, Hilberdink WKHA, et al. Postgraduate education to increase adherence to a Dutch physiotherapy practice guideline for hip and knee OA: a randomized controlled trial. Rheumatology (United Kingdom). 2013;52(2):368–75.
Rebbeck T, Macedo LG, Maher CG. Compliance with clinical guidelines for whiplash improved with a targeted implementation strategy: a prospective cohort study. BMC Health Serv Res. 2013;13(1):1–8.
Rebbeck T, Maher CG, Refshauge KM. Evaluating two implementation strategies for whiplash guidelines in physiotherapy: a cluster-randomised trial. Aust J Physiother. 2006;52(3):165–74.
Stevenson K, Lewis M, Hay E. Do physiotherapists’ attitudes towards evidence-based practice change as a result of an evidence-based educational programme? J Eval Clin Pract. 2004;10(2):207–17.
Tilson JK, Mickan S, Howard R, Sum JC, Zibell M, Cleary L, et al. Promoting physical therapists’ use of research evidence to inform clinical practice: part 3–long term feasibility assessment of the PEAK program. BMC Med Educ. 2016;16(1):1–13.
Van Dulmen SA, Maas M, Staal JB, Rutten G, Kiers H, Nijhuis-van der Sanden M, et al. Effectiveness of peer assessment for implementing a Dutch physical therapy low back pain guideline: cluster randomized controlled trial. Phys Ther. 2014;94(10):1396–409.
Schröder K, Öberg B, Enthoven P, Kongsted A, Abbott A. Confidence, attitudes, beliefs and determinants of implementation behaviours among physiotherapists towards clinical management of low back pain before and after implementation of the BetterBack model of care. BMC Health Serv Res. 2020;20(1):1–14.
Sugavanam T, Williamson E, Fordham B, Hansen Z, Richmond H, Hall A, et al. Evaluation of the implementation of the Back Skills Training (BeST) programme using online training: a cohort implementation study. Physiotherapy (United Kingdom). 2020;109:4–12.
Williamson E, Srikesavan C, Thompson J, Tonga E, Eldridge L, Adams J, et al. Translating the Strengthening and Stretching for Rheumatoid Arthritis of the Hand Programme from clinical trial to clinical practice: an effectiveness-implementation study. Hand Ther. 2020;25(3):87–97.
Karvonen E, Paatelma M, Kesonen JP, Heinonen AO. Knowledge translation from continuing education to physiotherapy practice in classifying patients with low back pain. J Man Manip Ther. 2015;23(2):68–74.
Carlfjord S, Landen Ludvigsson M, Peolsson A, Peterson G. Adoption of a research-based program for neck disorders implemented in primary care physiotherapy: a short- and long-term follow-up survey study. Physiother Theory Pract. 2019;37(1):89–98. https://doi.org/10.1080/09593985.2019.1608610.
Dhopte P, French SD, Quon JA, Owens H, Bussieres A, Canadian Chiropractic Guideline I. Guideline implementation in the Canadian chiropractic setting: a pilot cluster randomized controlled trial and parallel study. Chiropr Man Therap. 2019;27:31.
Richmond H, Hall AM, Hansen Z, Williamson E, Davies D, Lamb SE. Using mixed methods evaluation to assess the feasibility of online clinical training in evidence based interventions: a case study of cognitive behavioural treatment for low back pain. BMC Med Educ. 2016;16:163.
Hurley DA, Keogh A, Mc Ardle D, Hall AM, Richmond H, Guerin S, et al. Evaluation of an e-learning training program to support implementation of a group-based, theory-driven, self-management intervention for osteoarthritis and low-back pain: pre-post study. J Med Internet Res. 2019;21(3):e11123.
Eilayyan O, Thomas A, Hallé M-C, Tibbles AC, Jacobs C, Ahmed S, et al. Promoting the use of a self-management strategy among novice chiropractors treating individuals with spine pain: a mixed methods pilot clustered-clinical trial. PLoS One. 2022;17(1):e0262825.
Draper-Rodi J, Vogel S, Bishop A. Effects of an e-learning programme on osteopaths’ back pain attitudes: a mixed methods feasibility study. Pilot Feasibility Stud. 2021;7(1):1–18.
Longtin C, Decary S, Cook CE, Martel MO, Lafrenaye S, Carlesso LC, et al. Optimizing management of low back pain through the pain and disability drivers management model: a feasibility trial. PLoS One. 2021;16(1):e0245689.
Demmelmaier I, Denison E, Lindberg P, Åsenlöf P. Tailored skills training for practitioners to enhance assessment of prognostic factors for persistent and disabling back pain: Four quasi-experimental single-subject studies. Physiother Theory Pract. 2012;28(5):359–72. https://doi.org/10.3109/09593985.2011.629022.
Song L, Qan’ir Y, Guan T, Guo P, Xu S, Jung A, et al. The challenges of enrollment and retention: a systematic review of psychosocial behavioral interventions for patients with cancer and their family caregivers. J Pain Symptom Manage. 2021;62(3):e279–304.
Tseng DS. Organisational changes are more effective than education and reminders for raising adult immunisation and cancer screening rates. Evid Based Healthc. 2002;4(6):186–7.
Grimshaw J, Eccles M, Thomas R, MacLennan G, Ramsay C, Fraser C, et al. Toward evidence-based quality improvement: evidence (and its limitations) of the effectiveness of guideline dissemination and implementation strategies 1966–1998. J Gen Intern Med. 2006;21(S2):S14–20.
Squires JE, Sullivan K, Eccles MP, Worswick J, Grimshaw JM. Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implement Sci. 2014;9(1):1–22.
Dobbins M, Hanna SE, Ciliska D, Manske S, Cameron R, Mercer SL, et al. A randomized controlled trial evaluating the impact of knowledge translation and exchange strategies. Implement Sci. 2009;4(1):1–16.
Trivedi RB, Szarka JG, Beaver K, Brousseau K, Nevins E, Yancy WS Jr, et al. Recruitment and retention rates in behavioral trials involving patients and a support person: a systematic review. Contemp Clin Trials. 2013;36(1):307–18.
Acknowledgements
We thank Dr Kedar Mate for helping with the title and abstract screening.
Funding
This research was funded by the Richard and Edith Strauss Research Foundation.
Author information
Authors and Affiliations
Contributions
DG conceived the idea, conceptualised the manuscript and conducted the study-specific analysis. OE contributed to the screening process and to the data analysis. All authors (DG, OE, SA, and AB) were involved in data interpretation and in drafting and critically revising the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
N/A
Consent for publication
The datasets used and analyzed during the study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gaid, D., Eilayyan, O., Ahmed, S. et al. Enrollment, adherence and retention rates among musculoskeletal disorders rehabilitation practitioners in knowledge translation studies: a systematic review and meta-regression. Implement Sci Commun 5, 51 (2024). https://doi.org/10.1186/s43058-024-00585-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-024-00585-w