Abstract
Background
Prostate cancer is well known as the commonest cancer in men and the second leading cause of cancer-related death. CT, MRI and bone scintigraphy are considered the commonly widely used imaging diagnostic tools for detection, staging and follow-up of prostate cancer. Prostate-specific membrane antigen (PSMA) is a membrane glycoprotein, that can be concentrated in prostate cancer cells up to 100 times higher than in normal cells. PSMA-targeted imaging modalities have now proven their efficacy in diagnosis, staging and follow-up of prostate cancer. The use of 68Ga PSMA PET-CT has efficiently improved the detection of loco-regional and metastatic disease. 68Ga PSMA PET-CT also has an effective role in the primary diagnosis, staging, and detecting biochemical recurrence after curative treatment and in metastasis-targeted therapy. This work aims to review the role of 68Ga PSMA PET-CT in anatomical staging of prostate cancer in correlation with histopathological staging.
Results
Zonal correlation between 68Ga PSMA findings and biopsy results showed sensitivity ranging between 76.9 and 90.6% and specificity ranging from 85.7 to 100%. There was high significant correlation between the SUVmax uptake and the biopsy results, between the SUVmax uptake and the local staging as well as between the Gleason score and 68Ga PSMA PET/CT findings.
Conclusions
68Ga PSMA PET/CT is a highly promising imaging modality with an effective role in detection of prostate cancer showing high sensitivity and specificity in prediction of zonal histopathological results and loco-regional Gleason score staging with significant positive correlation between the SUV uptake results, Gleason score and the PSA levels.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Prostate cancer is well known as one of the most common cancer in men and second main leading cause of men cancer-related death. CT, MRI and bone scintigraphy are considered the most commonly used imaging modalities for diagnosis, staging and for post-therapy follow-up of prostate cancer. Prostate-specific membrane antigen (PSMA) is a membrane glycoprotein, that expresses significant higher concentration values on prostate cancer cells compared to normal prostate cells [1]. 68Ga PSMA targeting imaging agents are now widely available and being commonly used due to their high efficient diagnostic accuracy. 68Ga PSMA PET has been combined with multi-slice CT, for proper and better diagnostic and prognostic performance [2].
Recently, a multidisciplinary panel of healthcare providers and prostate cancer imaging experts developed an appropriate criteria for 68Ga PSMA imaging, including patients with newly diagnosed intermediate, high risk prostate cancer, castration-resistant prostate cancer (CRPC) and biochemical recurrence [3].
68Ga PSMA-PET has also been studied to detect and localize prostatic carcinoma. Some studies have been conducted to evaluate the relation between different pathological zones 68Ga PSMA uptake and the histopathological subtypes [4].
PET/CT imaging modality has already proved its accuracy and efficiency in prostate cancer detection and characterization and also has shown accurate relation between anatomical imaging and differential zonal histopathology [5].
This work aims to review the added value of 68Ga PSMA PET-CT in anatomical prostate cancer staging in correlation with histopathological staging.
Methods
A retrospective study that was conducted at Ain Shams University Hospitals from March 2023 till September 2023. 40 patients were included in the study with age range between 55 and 84 years old with mean age of 69.55 years old (Table 1).
The main source of data for this study was the PET/CT scans and PACS archiving system of Ain Shams University hospitals.
-
Ethical Considerations
-
An informed consent was obtained from all patients after explaining the procedure details of the study.
-
The study has been initiated after the approval of the research ethical committee, faculty of medicine and Ain Shams University.
-
The patient privacy and confidentiality of data were guaranteed during the various phases of the study.
-
-
Study Tools and procedure Clinical history and imaging findings of the included patients were retrospectively obtained from the picture archiving and communications system (PACS) of nuclear medicine unit in Ain Shams University.
-
Study Population
-
Inclusion Criteria
All patients were referred for 68Ga PSMA PET/CT scan with pathologically proved prostatic carcinoma, for initial staging.
-
Exclusion criteria
Patients who underwent any intervention or previously treated.
Any patient without pathological diagnosis of cancer prostate.
-
-
Patient preparation for PET/CT scans
-
Patients were instructed to fast from all types of food for a minimum of 4–6 h prior to the examination.
-
Patients were asked to be well hydrated before the study, and during the uptake time, then they were asked to empty their urinary bladder before the study.
-
Patients were asked to bring all related previous investigations, biopsy reports, and PSA level.
-
Serum creatinine was done within at least one month. It has to be within normal level (1.5 mg /dl) for IV contras administration.
-
-
Medications/intravenous contrast
-
Approximately 0.049–0.060 mCi/kg of 68GA-PSMA injected intravenously with saline infusion.
-
After confirming normal level of the serum creatinine, approximately 1–2 ml/kg of iodinated non-ionic low-osmolar contrast medium injected intravenously for the contrast-enhanced CT scans.
-
-
Procedure Time 120–180 min
-
Technique
-
After revision of our patient pathology report, all the patients are diagnosed as adenocarcinoma type of prostate cancer with different Gleason score was included in the study.
-
Combined PET/CT scan using a hybrid PET/CT system (PHILIPS; Ingenuity TF 128 PET/CT scanner; USA) was performed for all patients. The rules of patient preparation were followed strictly.
-
Approximately 0.049–0.060 mCi/ kg of 68Ga PSMA was injected intravenously with saline infusion followed by 60 min of rest; then, the PET scans were obtained.
-
The study was done in supine position with both arms elevated above head and scan on the whole body from the skull base down to the mid-thighs.
-
Then followed by diagnostic CT transmission scan using similar parameters.
-
A diagnostic contrast-enhanced CT scan was done initially covering the identical transverse field of view using the following parameters: 350 mA, 120 kV, 0.5-tube rotation time, and 5-mm slice thickness.
-
PET scan should start from the mid-thigh to skull base to exploit the reduced 68Ga-PSMA ligand uptake in the urinary bladder and with several bed positions [5,6,7] were performed each with approximately 15-cm axial field of view per bed position with 4-mm in-plane spatial resolution and covered the same field of view of the CT. The time of acquisition emission data was about 2–4 min for each bed position and in time range between 13 and 17 min.
-
A workstation with fusion software (PHILIPS WORKSTATION) was used to view all CT, PET, and PET/CT images, and they were reconstructed in multi-planar reformation and viewed in different planes for all as well as “3D maximum intensity projection (MIP) images” PET image in a video mode.
-
A radiological teamwork, including three nuclear medicine radiologists, reviewed and interpreted the PET, CT, and fused PET/CT images.
-
Prostate was divided into six zones (similar to the pathological report), right basal (RB) zone, left basal (LB) zone, right mid (RM) zone, left mid (LM) zone, right apical (RA) and left apical (LA) zones.
-
Each zone was radiologically assessed both visually for PSMA uptake and quantitatively by SUV max.
-
These radiological findings were correlated with the Gleason score in the histopathology report.
-
Results
-
Forty patients with pathologically proven cancer prostate were referred to 68Ga PSMA PET /CT for initial staging before initiating any treatment.
-
The ages of the included patients in this study ranged from 55 to 84 years, with mean age of 69.55 years (Table 2).
-
Prostate was divided into six zones (similar to the pathological report), and each zone was radiologically assessed visually for PSMA uptake and quantitatively by SUV max.
-
These radiological findings were correlated with the Gleason score (GS) in the histopathology report (Table 3).
-
Pathology reports and PSA level were available in all patients (Table 4).
-
The PSA levels ranged from 5.2 to 796 ng/ml, with mean value of 20.5 ng/ml.
-
The GS of the studied patients ranged from 6 to 10, with mean value of 7.
-
The Gleason grading system of the studied patients ranged from grade 1 (GS ≤ 6) (n = 2;5.5%), grade 2 (GS 3 + 4 = 7) (n = 10;27.7%), grade 3 (GS 4 + 3 = 7) (n = 7;19.4%), grade 4 (GS 8) (n = 13;36.1%), and grade 5 (GS 9 or 10) (n = 4;11.3%) (Table 5).
Diagnostic performance of 68Ga PSMA PET/CT for local staging
Relation between 68Ga PSMA PET/CT results and biopsy results (Tables 3 and 6)
-
Zonal correlation between PSMA findings and biopsy results showed sensitivity ranging between 76.9 and 90.6%, specificity ranging between 85.7 and 100%, PPV ranging from 95.2 to 100% and NPV ranging from 50 to 81.3% in detection of prostatic cancer lesion in 68Ga PSMA PET/CT studies in different prostatic zones.
-
According to TNM staging [5], two patients (5%) were staged as T0, fifteen patients (37.5%) were staged as T2, eighteen patients (45%) were staged as T3, and five patients (12.5%) were staged as T4 (Table 5).
Relation between SUVmax uptake and biopsy results (Table 7)
There was highly significant correlation between the SUVmax uptake and the biopsy findings where the median SUVmax uptake for cancer prostate lesion was 20.065, while the median SUVmax of normal prostatic tissue was 1.6 with P value < 0.001.
Relation between the PET/CT findings, SUVmax and local staging (Tables 8 and 9)
-
There was highly significant correlation between the SUVmax uptake and the local staging where the SUVmax uptake was higher when the local staging was high with P value ranging from 0.01 to < 0.001.
-
Mild significant relationship was seen between the PET/CT findings and the local staging with P value ranging from 0.03 to < 0.001.
Relation between 68Ga PSMA PET/CT findings and Gleason score (Table 10)
There was highly significant correlation between the Gleason score and 68Ga PSMA PET/CT findings with P value 0.003 where high PSMA sensitivity was found with mean Gleason score of 7. Few false negative results noted with very high Gleason score at 8.
Relation between SUVmax uptake and Gleason score (Table 10)
These was significant correlation between the Gleason score and SUVmax results with P value 0.03.
Relation between PSA level and Gleason score (Table 11)
These was significant correlation between the Gleason score and PSA levels with P value 0.02.
Discussion
The main aim of this study was to determine the correlation between 68Ga-PSMA expression in the primary prostate cancer patients including SUV and the PSA value as well as Gleason score in those cases.
68Ga Prostate-specific membrane antigen (PSMA) PET has been recently emerging as a new promising imaging modality for evaluation of prostate cancer, with higher sensitivity and sensitivity compared to other conventional imaging modalities [6].
Prostate-specific membrane antigen (PSMA) is a transmembrane glycoprotein that showed significant overexpression in prostate cancer cells in which radiolabeled small molecules can avidly bind to the active prostate cancer cells, resulting in significant high tumor-to-background contrast images [7].
Current study-based evidences demonstrate higher sensitivity and specificity parameters of 68Ga PSMA PET /CT compared to the conventional imaging, for better morphological and functional evaluation of prostate cancer lesions [8].
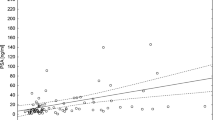
In this study, there was high significant correlation between the Gleason score and 68Ga PSMA PET/CT findings with P value 0.003 where high PSMA sensitivity found with mean Gleason score of 7 and this was in line with other studies (Fig. 1).
A 72-year-old male patient, presented with newly diagnosed prostatic carcinoma and referred for initial staging. His PSA level is 9.4 ng/ml. and Gleason score: 4 + 3 = 7. A MIP image of the PET/CT, B Axial PET/CT fused images and C Sagittal PET/CT fused images showing prostatic bilobar moderate 68GAa PSMA-avid focal lesions occupying the peripheral zones of mid-gland and apex. The lesions show SUVmax of 8.9
This finding is matching with other various studies that have similar conclusion;
In an another study conducted by Altun et. al. [9] including 98 patient and found that total PSA level was significantly higher in Gleason score > 7 than in the group with Gleason level ≤ 7 (p = 0.001). In addition, PSMA SUVmax levels of the group with a Gleason score of > 7 revealed to be significantly higher than the group with a Gleason score of ≤ 7 (p = 0.03).
Rahbar et al. [10] prospectively evaluated 68Ga-PSMA PET /CT in six patients who underwent prostatectomy for Gleason ≥ 3 + 4 tumors and found that 68Ga-PSMA PET had a sensitivity and specificity of 92% for detecting prostate cancer lesions.
Fendler et al. [11] also prospectively evaluated 68Ga-PSMA PET in 21 patients with biopsy-proven prostate carcinoma in which the prostate was sectioned into six-segmental model with a sensitivity and specificity of 67% and 92%, respectively. False-negative results were noted in 6 out of 12 segments with a Gleason score of 6, 12 out of 27 segments with a Gleason score of 7, 4 out of 19 segments with a GS of 8, 10 out of 41 segments with a Gleason score of 9, and only one segment with a Gleason score of 10.
Determining the accuracy of an imaging modality to detect prostate cancer requires appropriate imaging/histopathologic concordance as the distribution of prostate cancer within the gland can be heterogeneous and the deformation can occur during surgery and histopathologic work up.
Zamboglou et al. [12] have conducted a prospective study of 8 men who went 68Ga-PSMA PET/CT scans prior to prostatectomy and revealed a statistically significant correlation of 68Ga-PSMA PET/CT with histopathological results.
Another prospective study conducted by Courtney et al. [13] for 302 patients with pretherapy to prostate cancer and found out a significant sensitivity and specificity of 68Ga-PSMA PET (85% and 98%, respectively) in loco-regional prostate cancer staging.
Luiting et al. [14] also reviewed retrospectively the diagnostic performance of 68Ga-PSMA PET/CT for primary prostate cancer staging, where patient-based sensitivity and specificity were 4–100% and 90–95%, lesion-based sensitivity and specificity ranges were 50–58% and 96–100%, respectively. That was concordant with the results in this study that proved significant relationship between the PET/CT findings and the local staging with P value ranging from 0.03 to < 0.001.
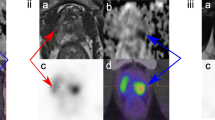
Those findings are correlated with our study results, in which there was highly significant correlation between the SUVmax uptake and the histopathological results where the median SUVmax uptake for cancer prostate lesion was 20.065, while the median SUVmax of normal prostatic tissue was 1.6 with P value < 0.001 (Fig. 2).
A 74-year-old male patient, presented with newly diagnosed prostatic carcinoma and referred for initial staging. His PSA level is 53.5 ng/ml. and Gleason score: 4 + 4 = 8. A MIP image of the PET/CT showing B Axial PET/CT fused images and C Sagittal PET/CT fused images showing: Markedly 68Ga PSMA avid prostatic mass occupying the peripheral zones of the whole gland and extending to the transitional zones (white arrow) achieving 36 SUVmax. Multiple enlarged PSMA avid regional and distant retroperitoneal lymph nodes (Blue arrow). Few 68Ga PSMA avid bony deposits noted mainly at right femoral head and right humeral head (Yellow arrow)
Another study conducted by Meissner et al. [15] stated SUVmax cut-off value was 4.0.
This discrepancy in SUV cut-offs values maybe attributed to multiple variations such as scanners, tracers, reconstruction parameters and others.
Demerci et al. [16] reported in their study the correlation coefficients between PSA values and SUVmax that ranged between 0.071 and 0.57. And the correlation coefficients between SUVmax and Gleason scores ranged between 0.096 and 0.5.
Meißner et al. [17] conducted a cohort study on 37 patients and reported significant correlation between Gleason score and SUV uptake and moderate correlation between tumor volume and Gleason scores.
Christian et al. [18] combined in their study GS, SUV max and PSA values, where the median SUVmax was higher in patients with PSA levels ≥ 10 ng/ml.
Few false negative results reported in our study with Gleason score of 8 and some other false negative results also elicited with very low Gleason score (Fig. 3).
A 65-year-old male patient, presented with newly diagnosed prostatic carcinoma and referred for initial staging. His PSA level is 14.6 ng/ml. and Gleason score: 3 + 3 = 6. A MIP image of the PET/CT, B Axial PET/CT fused images and C Sagittal PET/CT fused images showing low grade 68Ga PSMA focal lesion occupying the right posterior peripheral zone of base, mid-gland and apex. The lesion shows SUVmax of 5.6
This was matching with a study conducted by JIRI et al. [19], that revealed that poorly differentiated or anaplastic tumor cell subtypes can express relatively lower Gleason score of 5 only have a weak correlation with 68Ga-PSMA accumulation.
This could be explained as the most aggressive tumors subtypes have highly altered cells that stop expressing PSMA in high concentration and hence show low 68Ga-PSMA accumulation.
Pitfalls of 68Ga-PSMA PET/CT
The main pitfall in the current study is the relative limited number of sample volume due to some factors like patient non-compliance or financial obstacle factor.
Some PSMA pitfalls are related to its expression in multiple benign conditions, mainly in inflammatory pathologies.
The pitfall of overlapping between malignant prostatic lesions and benign prostate lesions.
Some benign lesions can mimic prostate cancer cells and their metastatic disease, including inflammatory lymph nodes, various benign osseous conditions, including Paget’s disease, hemangiomas and fractures.
Conclusions
Overall, the current study could conclude that the accuracy of 68Ga-PSMA PET/CT is superior in sensitivity and specificity to that of conventional imaging in prostate cancer diagnostic workup.
The Gleason score and PSA level were significantly correlated with SUV uptake of 68Ga-PSMA PET/CT imagings.
Based on those findings, we recommend the promising use of 68Ga-PSMA PET/CT for the primary staging of prostate cancer, especially in tumors with GS > 7 or patients with PSA level ≥ 20.065 ng/ml; however, false negative results can occur with very low or very high Gleason scores due to non-differentiated cells.
68Ga-PSMA PET/CT is recommended for many other aspects; metastasis workup in primary prostate cancer and for the detection of biochemical recurrent lesions after radical resection or radiotherapy status.
The superior diagnostic accuracy of 68Ga-PSMA PET/CT for primary staging of prostate cancer proved to have a positive impact on clinical management outcome in those patients.
Availability of data and materials
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CRPC:
-
Castration-resistant prostate cancer
- CT:
-
Computed tomography
- GS:
-
Gleason score
- LB:
-
Left basal zone
- LM:
-
Left mid zone
- LA:
-
Left apical zone
- MIP:
-
Maximum intensity projection
- PACS:
-
Picture archiving and communication system
- PC:
-
Prostate cancer
- PET:
-
Positron emission tomography
- PSMA:
-
Prostate-specific membrane antigen
- RB:
-
Right basal zone
- RM:
-
Right middle zone
- RA:
-
Right apical zone
References
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics. Cancer J Clin 73(1):17–48. https://doi.org/10.3322/caac.21763
Jadvar H, Calais J, Fanti S, Feng F, Greene KL, Gulley JL et al (2022) Appropriate use criteria for prostate-specific membrane antigen PET imaging. J Nucl Med 63(1):59–68. https://doi.org/10.2967/jnumed.121.263262
Ristau BT, O’Keefe DS, Bacich DJ (2014) The prostate-specific membrane antigen: lessons and current clinical implications from 20 years of research. Urol Oncol 32(3):272–279. https://doi.org/10.1016/j.urolonc.2013.09.003
Lawhn-Heath C, Salavati A, Behr SC, Rowe SP, Calais J (2021) Fendler WP: prostate-specific membrane antigen PET in prostate cancer. Radiology 299(2):248–260. https://doi.org/10.1148/radiol.2021202771
Eiber M, Herrmann K, Calais J, Hadaschik B, Giesel FL, Hartenbach M, Hope T, Reiter R, Maurer T, Weber WA, Fendler WP (2018) Prostate cancer molecular imaging standardized evaluation (PROMISE): proposed miTNM classification for the interpretation of PSMA-Ligand PET/CT. J Nucl Med 59:469–478
Bailey J, Piert M (2017) Performance of 68Ga-PSMA PET/CT for prostate cancer management at initial staging and time of biochemical recurrence. Curr Urol Rep 18:84
Rauscher I, Maurer T, Fendler WP et al (2016) (68)Ga-PSMA ligand PET/CT in patients with prostate cancer: How we review and report. Cancer Imaging 16:14
Rhee H, Thomas P, Shepherd B et al (2016) Prostate specific membrane antigen positron emission tomography may improve the diagnostic accuracy of multiparametric magnetic resonance imaging in localized prostate cancer. J Urol 196:1261–1267
Altun Tuzcu Ş, Uyar A, Güzel F et al (2021) The relationship between 68Ga-PSMA uptake and Gleason score and PSA levels in patients with prostate cancer. Anatolian Curr Med J 3(4):327–332
Rahbar K, Weckesser M, Huss S et al (2016) Correlation of intraprostatic tumor extent with (6)(8)Ga-PSMA distribution in patients with prostate cancer. J Nucl Med 57:563–567
Fendler WP, Schmidt DF, Wenter V et al (2016) 68Ga-PSMA PET/CT detects the location and extent of primary prostate cancer. J Nucl Med 57:1720–1725
Zamboglou C, Schiller F, Fechter T et al (2016) (68)Ga-HBED-CC-PSMA PET/CT versus histopathology in primary localized prostate cancer: a voxel-wise comparison. Theranostics 6:1619–1628
Courtney LH et al (2021) Prostate-specific membrane antigen PET in prostate cancer. Radiology 299:2
Luiting HB, van Leeuwen PJ, Busstra MB et al (2020) Use of gallium-68 prostate-specific membrane antigen positron- emission tomography for detecting lymph node metastases in primary and recurrent prostate cancer and location of literature. BJU Int 125(2):206–14
Meissner VH, Rauscher I, Schwamborn K et al (2022) Radical prostatectomy without prior biopsy following multiparametric magnetic resonance imaging and prostate-specific membrane antigen positron emission tomography. Eur Urol 82:156–160
Demirci E, Kabasakal L, Şahin OE, Akgün E, Gültekin MH, Doğanca T et al (2019) Can SUVmax values of Ga-68-PSMA PET/CT scan predict the clinically significant prostate cancer? Nucl Med Commun 40:86–91
Meißner S, Janssen J-C, Prasad V, Brenner W, Diederichs G, Hamm B et al (2017) Potential of asphericity as a novel diagnostic parameter in the evaluation of patients With 68Ga-PSMA-HBED-CC PET-positive prostate cancer lesions. EJNMMI Res 7:85. https://doi.org/10.1186/s13550-017-0333-9
Christian U et al (2017) 68Ga-PSMA-11 PET/CT in primary staging of prostate cancer: PSA and Gleason score predict the intensity of tracer accumulation in the primary tumour. Eur J Nucl Med Mol Imaging 44:941–949. https://doi.org/10.1007/s00259-017-3631-6
Jiří F et al (2023) Assessment of prostate carcinoma aggressiveness: relation to 68Ga-PSMA-11-PET/MRI and Gleason score. Anticancer Res 43(1):449–453
Acknowledgements
We appreciate the support of radiology department in Ain Shams University hospitals and the cooperation of the whole team including the expert radiographers.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ME is responsible for coordinating the data, writing the manuscript and revising it. NT is responsible for performing the statistics and coordinating them as well as revision of the manuscript. OY is responsible for gathering the cases and describing the figures details.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was reviewed and approved by the local ethical committee of “Research Ethics Committee at the Faculty of Medicine, Ain Shams University.” It ruled that no formal ethics approval was required in this retrospective study, and so no reference number was given by the IRB.
Consent for publication
This research is based on retrospective study, yet, written consent for publication was obtained for these cases.
Competing interests
No financial or non-financial competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsadawy, M.E.I., Omar, Y. & Taha, N.M. The added value of 68Ga-PSMA PET/CT in anatomical staging of prostatic carcinoma in correlation with the histopathological zonal staging. Egypt J Radiol Nucl Med 55, 179 (2024). https://doi.org/10.1186/s43055-024-01351-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01351-7