Abstract
Background
Hepatic arterial anatomy is important in performing many surgical and endovascular procedures. Familiarity with variations in the hepatic arterial anatomy is essential to achieving adequate embolization. In some patients, in addition to anatomic variations of the hepatic arteries, different extrahepatic collateral arteries may provide partial or total vascular supply to hepatocellular carcinoma (HCC), which makes transcatheter arterial chemoembolization (TACE) technically challenging. We aim to evaluate the different feeding vessels of HCC using multi-detector computed tomography angiography (MDCTA) as a pre-procedural step before planning suitable management.
Results
One hundred patients with 150 focal HCC lesions were involved in our study. The anatomy of the blood supply and the morphological characteristics of HCC, including the size, location, and history of previous hepatitis, were quantitatively assessed and statistically analysed. The number of patients who had classic hepatic arterial supply for the HCC lesions in our study was 54 (54%). The number of patients with additional extrahepatic supply is 26, while the number of patients with anatomical vascular variants is 20. Among these 26 patients with extrahepatic (parasitic) blood supply, six patients were supplied by the right inferior phrenic artery, four patients were supplied by the right internal mammary artery, and two patients were supplied by each other type of extrahepatic feeder, which are the left inferior phrenic artery, left internal mammary artery, left gastric artery, cystic artery, right lumbar artery, direct branch from the aorta, omental arteries, right renal artery, and LHA from the LGA. Twelve of the 20 patients with anatomical vascular variants had replaced RHA from the SMA; four patients had replaced LHA from the LGA; two patients had replaced RHA from the GDA; and two patients had replaced CHA from the SMA. Only 50 cases of CT findings were correlated with the data from the interventional procedures of these patients.
Conclusions
Because of the differences in HCC blood supply between typical, parasitic, and anatomical vascular variants, MDCTA has significant clinical significance prior to TACE and any interventional procedure.
Similar content being viewed by others
Background
Hepatocellular carcinoma (HCC) is the most common primary cancer of the liver. It is the second-leading cause of cancer deaths worldwide [1]. Liver transplantation, radical excision, and tumour ablation are considered curative alternatives for treating patients with HCC. TACE is an important therapeutic alternative for unresectable HCC [2].
Previous studies have found that perihepatic arteries such as the internal mammary artery (IMA), intercostal artery (ICA), inferior phrenic artery (IPA), gastric artery (GA), superior mesenteric artery (SMA), gastroduodenal artery (GDA), cystic artery (CA), renal artery (RA), and also the lumbar artery (LA) may supply HCC lesions [3,4,5,6,7,8,9].
The anatomical variants of the hepatic artery were reported by Michelsin in 1953 after cadaver dissections [10]. Hiatt et al. revisited this classification based on surgical liver findings [11].
The anatomical variances of HA are quite common, most frequently due to the separate origination of the right and left HA and the presence of accessory HA. Thus, TACE might be incomplete; failure to identify such anatomical variations preoperatively may render TACE unsuccessful and/or even cause complications. So, it is necessary to evaluate the origin, course, and distribution of the hepatic arterial tree before the therapy [12]. Before beginning treatment, interventional radiologists should have adequate mapping for the feeding arteries of HCC, including hepatic artery variants as well as accessory and parasitic perihepatic arteries [12].
Digital subtraction angiography (DSA) is the main imaging method for detecting feeding arteries in HCC, including HA and ectopic blood supply. Its application is limited due to its invasiveness, cost, and inability to identify all possible blood vessels during the examination [13]. MDCTA, including multi-planar reconstruction (MPR), curved planar reconstruction (CPR), maximum intensity projection (MIP), and volume rendering (VR), is considered a noninvasive technique alternative to DSA for displaying hepatic and perihepatic vessels and determining the tumour-feeding vessels before TACE [13].
For effective treatment of HCC, it is important to inject the chemoembolized material into the artery or arteries that supply the tumour(s). These arteries should be identified by imaging in the pre-treatment assessment. It is critical to understand common hepatic arterial anatomy and variants, as well as to identify any extrahepatic branches that have vascularized the tumour [14].
Many previous studies showed that MDCTA could identify most of the tumour-feeding vessels. MDCTA was also suggested to be conducted for any tumours to locate the feeding vessel before chemoembolization. Few studies, however, have confirmed whether the morphological features of HCC (size, site, and location) and the therapeutic history can influence the formation of ectopic supply.
The aim of this study is to report the different arteries that may vascularize HCC. We try to determine whether the morphological features of HCC and the therapeutic history could affect the occurrence of ectopic feeding arteries. These arteries must be anticipated, recognized, and reported on sectional imaging in the pre-treatment assessment and catheterized during chemoembolization. This will help to reduce the radiation exposure dose while also allowing the surgeon or radiologist to be aware of anatomy and variation, saving time and effort, and preventing complications.
Methods
The study was a prospective study. It was approved by our university hospital's ethical committee. It included HCC patients who underwent an abdominal CT angiography (CTA) scan from April 2020 to April 2021 at the department of radiology. Informed, written consent was obtained from all patients. The number of these individuals was 100 (68 men and 32 women, age range 36–86, with a median age of 61 years). Thirty patients had previous chemoembolization with a residual or recurrent active lesion. HCC was proven either with the pathological analysis of the biopsy specimen or with a combination of clinical, laboratory, and radiological data. Diagnostic criteria for the non-invasive diagnosis of the HCC were that the lesion showed early arterial enhancement with early contrast wash-out combined with cirrhosis and an AFP level above 500 ng/ml. Inclusion criteria: patient confirmed to have HCC larger than 3 cm (except for residual lesions after previous intervention); whatever the site and the number of lesions, they did not exceed 3 focal lesions. Patients with severe ascites, metastatic HCC, allergy to iodinated intravenous contrast agents, impaired renal function (defined as serum creatine greater than 1.5 mg/dL), pregnancy, and an inability to undergo CT due to hemodynamic instability were excluded.
All patients were subjected to full history taking regarding previous intervention by chemoembolization. Laboratory studies included all the routine laboratory workups with stress on the levels of creatine, blood urea nitrogen, and alpha-fetoprotein CTA examination.
Patient preparations
All patients were instructed to fast for 6–8 h prior to the examination. They were asked to continue adequate simple fluid intake for up to 3 h prior to the examination to ensure adequate hydration and provide negative contrast in the oesophagus and stomach. Patients were taught how to hold their breath during examinations when requested. Patients were positioned supine on the CT table. A 18–20-gauge catheter was placed into a superficial vein within the antecubital fossa, forearm, or dorsum of the hand. A catheter was placed into the superficial vein within the antecubital fossa, forearm, or dorsum of the hand. The injected arm was placed at the patient’s side to eliminate kinking of the subclavian vein at the thoracic inlet during injection, and the other arm was placed above the patient’s head.
Technique
All MDCT angiograms were performed on a 32-channel MDCT scanner (Siemens, Germany). Immediately prior to scanning, 500–1000 ml of plain water were administered orally to all patients. Water was used as a negative contrast agent to distend the stomach and improve visualization of the gastric wall and intestine. All patients underwent cranio-caudal scanning in the supine position during a single breath hold. The scanning area was from pulmonary hilum level to iliac crest level. CT was performed initially without contrast medium. A non-enhanced sequence was performed with a collimation of 6 mm for the localization of subsequent sequences. With the use of a power injector, 80–110 ml of nonionic contrast media heated to 37 °C were injected at a rate of 5 ml/s. The arterial phase started 4 s after the attenuation in the descending aorta reached 100 HU, which took about 10 s. The scan starts from the dome of the liver to its caudal end and takes 7 s. The portal venous phase started 7 s after the end of the arterial phase, and the scan range started from the dome and covered all the abdomen and pelvis in 15 s. Delayed scans start 5 min after the end of the portal venous phase and cover the same range as the portal venous phase. Narrow collimation is used (6 mm) to provide detailed resolution with fewer artefacts on the reformation images, as shown in Table 1.
Image processing and interpretation
CT images produced during the arterial phase were sent to the workstation DICOM viewer for post-processing and analysis in order to fulfil the study's objectives. Images from the arterial phase were studied. The imaging analysis was based on the original images as well as the three-dimensional (3D) post-processing images [maximum intensity projections and shaded surface display] (MIP and SSD), as well as multiplanar reformation (MPR), for a quick overview of the vascular morphology, and volume renderings for the final evaluation and documentation. Three radiologists with more than 10 years’ experience in abdominal angiography reviewed the sequences and wrote reports in consensus. The anatomical findings were classified as normal, anatomical vascular variant, and extrahepatic blood supply. The frequency of various anomalies was calculated. The findings of CT angiographic data sets were compared with interventional procedures in only 50 cases, which served as the standard of reference.
Statistical analysis
The data were fed to the computer and analysed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp.) Qualitative data were described using numbers and percents. Quantitative data were described using range (minimum and maximum), mean, standard deviation, and median. The difference between extrahepatic and vascular variants with different tumour sizes was assessed using Chi-square rest, with statistical significance set at < P 0.05.
Results
Our prospective study included 150 HCCs from 100 patients; demographic data were grouped in Table 2, and all the patients were grouped according to size, site, and location. The total number of examined tumours is 150; the number of tumours restricted to one segment is 120 (70.36%), while the number of tumours involving two segments is 30 (17.64%), and only 20 tumours involving three segments (12%) Table 2.
The number of patients who had classic hepatic arterial supply for the HCC lesions is 54 (52.94%), while only two patients (1.96%) had atypical post-celiac artery compression neovascularization. The number of patients with extrahepatic supply is 26 (25.49%), and the number of patients with anatomical vascular variants is 20 (19.61%), due to two patients having both anatomical vascular variants and parasitic blood supply.
The total number of patients with additional extrahepatic (parasitic) blood supply is 26, while the number of extrahepatic arteries is 28 because two of the patients had dual parasitic blood supply for the same tumour (the tumour was supplied by the right inferior phrenic artery and by a direct branch from the aorta) as in Table 3.
The tumours supplied by the right inferior phrenic artery were located at segments VII/VIII and segment I (subdiaphragmatic location). The tumours supplied by the right internal mammary artery were located in segment IV. The tumours supplied by the cystic artery were located in segment V. The tumour supplied by a direct branch from the aorta, was located at segment VII. The tumors supplied by the right lumbar arteries and the right renal arteries were located at segment VI. Tumours supplied by the left gastric artery were found in segment III, those supplied by the left inferior phrenic artery and left internal mammary artery in segment II, and those supplied by the omental arteries in segment IV, as shown in Table 4.
The total number of patients with ectopic blood supply was 26; the number of tumours with ectopic arteries have size less than 5 cm was 6/26 (23%) and the number of tumours with ectopic arteries greater than 5 cm was 20/26 (77%) with a significant P value < 0.05 compared to the size of HCC lesions supplied by normal hepatic arteries.
The number of patients who had replaced RHA from the SMA is 12 (12%), and only two patients (2%) had replaced CHA from the SMA. The number of patients who have replaced LHA from the LGA is four (4%), while only two (2%) have replaced RHA from the GDA. Thirty cases had a previous history of chemoembolization with residual or recurrent disease, with 10 cases due to improper or inadequate chemoembolization and 20 cases with additional extrahepatic supply (15 cases with subcapsular locations and larger sizes than 5 cm). The CT findings were correlated with the data from the interventional procedures of only 50 patients, and all the CT findings were seen as similar to those in the intervention procedure (Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9, 10).
A 49-year-old female patient diagnosed by triphasic as having hepatocellular carcinoma at segment VII, A coronal CT with MIP, B arteriography showed the common hepatic artery (green arrow) raised from the celiac artery (red arrow), then split into the proper hepatic artery (white arrow) and the GDA (yellow arrow). The lesion at segment VII (blue arrow) supplied by the hepatic artery as regards its classic branching pattern
A 66-year-old male patient diagnosed by triphasic CT as having hepatocellular carcinoma at segments VII and VIII. A Coronal CT with MIP revealed the right hepatic artery (green arrow) was replaced by the superior mesenteric artery, with the right hepatic artery supplying the HCC lesion at segments VII and VIII (grey arrow). B An axial CT with MIP revealed that the left hepatic artery (blue arrow) raised from the celiac trunk (yellow arrow). C An axial CT with MIP revealed that the lesion received parasitic blood supply from the right inferior phrenic artery (red arrows)
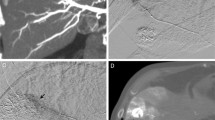
A 56-year-old male patient diagnosed by triphasic CT as having hepatocellular carcinoma at segment VI. A Coronal CT with MIP revealed that the right hepatic artery (white arrow) was replaced by the GDA (black arrow). The right hepatic artery supplied an HCC lesion at segment VI (black arrowhead). B Arteriography revealed that the lesion was injected and catheterized through the replaced RHA (white arrowhead) from the GDA
A 59-years-old male patient diagnosed by triphasic CT as having hepatocellular carcinoma at segment IV-b and encroaching on segment V (inter-lobar location). A Coronal CT with MIP revealed that Hepatocellular carcinoma involving segment IV-b and encroaching on segment V (inter-lobar location), evidenced by the (red line) discriminating both lobes, B and C CT sagittal view & 3D view: they revealed that the patient had a compressed celiac trunk between median arcuate ligament (red arrow). D coronal CT with MIP revealed that the blood flow circulated through the SMA (red arrows), then the blood passed through a highly tortuous gastroduodenal arcade (that was seen quite hypertrophied) as it carried the whole burden of the celiac circulation (green arrow heads). Many vascular loops were noted (purple arrows). The blood joined the hepatic artery through the gastro-duodenal artery (yellow arrow heads), where it flowed retrogradely towards the splenic and left gastric arteries (blue arrow heads). It also flowed antegrade in the proper hepatic artery (orange arrow heads). The prominent tumour feeding, joined the HCC focus from its superior aspect (white arrowheads)
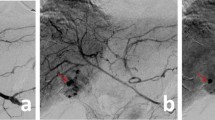
A 55-year-old male patient was diagnosed by tri-phasic CT as having hepatocellular carcinoma at segment V. A The coronal CT arterial phase and MIP displayed that the HCC lesion at segment V (green arrow) was supplied by the cystic artery (red arrow). B Arteriography displayed that the lesion was catheterized and injected through the cystic artery (white arrow)
A 72-year-old female patient diagnosed by triphasic CT with segment II (left lobe) exophytic hepatocellular carcinoma (A), coronal CT arterial phase, and MIP post TACE (B), The axial CT arterial phase and MIP post-TACE revealed that the posterior aspect of the exophytic HCC lesion at segment II (green arrow) was supplied by the left inferior phrenic artery (red arrow)
A 49-year-old male diagnosed by triphasic CT as having hepatocellular carcinoma at segment VII A Coronal CT arterial phase and MIP post-TACE revealed a thin branch from the aorta that directly supplied the inferior aspect of the lesion (red arrowheads). B Arteriography displayed a branch that rose directly from the aorta (yellow arrow heads) and supplied the lesion. The lesion was catheterized and injected through the right inferior phrenic artery
A 61-year-old female patient diagnosed by tri-phasic CT as having hepatocellular carcinoma at segment IV. A The axial CT arterial phase displayed that the HCC lesion was located at segment IV (yellow arrow); B coronal MIP reconstruction demonstrated that the HCC (yellow arrow) lesion was supplied by the right internal mammary artery (blue arrows)
A 69-year-old male diagnosed by triphasic CT as having large hepatocellular carcinoma at the subcapsular area of segment VII. A Coronal CT and MIP displayed that the right phrenic artery (green arrow heads) was sharing in the supply of the lesion. B Arteriography showed that the lesion was catheterized and injected through the right phrenic artery (red arrow heads)
A 72-year-old male patient diagnosed by triphasic CT as having exophytic hepatocellular carcinoma at segments II and III. A The axial CT arterial phase displayed the exophytic HCC lesion located at segments II and III (red arrow). B The axial CT with MIP displayed that the HCC lesion (red arrow) was supplied by the left gastric artery (blue arrow heads)
Discussion
Understanding differences in hepatic arterial anatomy is essential for successful embolization. In some patients, besides anatomic variations of the hepatic arteries, various extrahepatic collateral (EHC) arteries may provide a partial or total vascular supply to HCC; these variations in specific situations make TACE technically challenging, with the development of micro-catheters in recent years facilitating intervention from small blood vessels [14].
To successfully perform TACE, interventional radiologists should have adequate mapping of the feeding arteries of HCC, including hepatic artery variants as well as accessory and parasitic perihepatic arteries, before treatment [13, 14].
Our study results were matched with those of Hefaiedh et al. [15], Tangkijvanich et al. [16], Walter et al. [17], Shaker et al. [18], and Kirchner et al. [19], who studied the variation in vascular supply of HCC patients as regarded to age incidence and sex prominence, as well as their relations to HBV and HCV, lobe prominence, and the number of HCC lesions, either solitary or multiple lesions.
our study, we found that the right lobe of the liver was more frequently occupied by focal lesions (56%), and the majority of tumours were restricted to one or two liver segments (70.36%). This data was consistent with Shaker et al. [18] and Kirchner et al. [19].
We found that the total number of lesions was between 3 and 5 cm and accounted for 50.59% of the total number of lesions. This matched the findings of Kirchner et al. [19] and Yuen MF et al. [20].
The majority of patients (52.94%) had classic hepatic arterial supply. 19.61% of patients had anatomical vascular variations, compared to 25.49% of patients who had additional extrahepatic supply. According to Yuen MF et al. [20], 69.2% of all lesions were fed only by HA, and 30.8% were fed by ectopic arteries, either with or without HA. Only one patient (1.96%) in our study had atypical supply after celiac artery compression, which was consistent with the findings of Lee et al. [21].
In our study, the right inferior phrenic artery, left inferior phrenic artery, right internal mammary artery, cystic artery, left gastric artery, direct from the aorta, lumbar artery, omental arteries, and the right renal artery all contribute to the supply of HCCs, similar to what was found by Moustafa et al. [22], Kim et al. [23], Miyayama et al. [24], and Ishikawa et al. [25].
One patient in the current study was supplied by the right renal artery, which accounts for 7.69% of patients and is located at segment VI. Another study conducted by Lee et al. [26] found that the right renal artery accounts for 3.5–12.0% of the EHC arterial blood supply to HCC. Ishikawa et al. [25] also stated that the superior capsular artery is reported to have an important role in providing these feeders.
In our study, the lesion that was supplied by the cystic artery was located at segment V. This finding is consistent with that of Moustafa et al. [22], who reported that the cystic artery can provide parasitic feeders to HCC located adjacent to the gall bladder fossa, and this occurs more frequently when the hepatic artery is attenuated owing to prior TACE procedures. It can also provide an EHC arterial supply to HCC located in other portions of the right hepatic lobe and in the medial segment of the left hepatic lobe.
We reported that one patient with hepatocellular carcinoma at segment VII was supplied by the inferior phrenic artery as well as a direct branch from the aorta (dual extrahepatic supply); this finding had not previously been reported.
In the present study, segments VII, VIII, and I were the sites of the tumours supplied by the inferior phrenic artery. A study by Moustafa et al. [22] revealed that the interventional radiologist should be highly suspicious that the right IPA is an EHC artery if the hepatic lesion is in close proximity to the right hemi-diaphragm or is situated in liver segment VII and if the HCC lesions in the caudate lobe receive 88% of their EHC arterial blood supply from the right IPA [27, 28].
In the current study, the majority of HCC supplied by ectopic arteries is larger than 5 cm and accounts for 77% of total patients with additional ectopic blood supply. This is consistent with Wang et al. [29], who found that most of the ectopic blood supply in HCC formed among the tumours, with the sizes ranging from 5 to 10 cm in diameter. Another study conducted by Chung et al. [30] stated that 63% of tumours over 6 cm in size and 3% of tumours under 4 cm in size are vascularized by extrahepatic arteries. Yuen MF et al. [20] stated that with the increased size of HCC, HA would be insufficient to supply nutrition for the tumour, especially when HA was blocked by interventional radiology. The peri-hepatic artery would participate in the blood supply for HCC due to the anatomical basis of ectopic blood supply.
As regarded the hepatic artery variants, our study reported that 12 patients (12%) had replaced the RHA from the superior mesenteric artery and only two patients (2%) had replaced the CHA from the SMA. This was consistent with the findings of Gruttadauria et al. [31], who discovered that the replaced or accessory RHA from the SMA was the most commonly encountered variant, accounting for 15% of the population. Only four patients in this study received LHA from the LGA, accounting for 4%. This contradicts the findings of Gruttadauria et al. [31], who discovered that the replaced or accessory LHA arising from the LGA was the second most common variant, occurring in 12% of cases.
Our study also demonstrated that the subcapsular location of the lesion should be considered when looking for extrahepatic supply, as the subcapsular location in both hepatic lobes was statistically significant P value < 0.05 compared to the HCC with normal arterial supply, and we found a significant number of previously chemoembolized HCC showed activity, which could be due to improper mapping prior to embolization to diagnose extrahepatic supply.
Our study had some limitations, as only 50 cases were correlated with the data of the interventional procedures because DICOM was not available for the intervention procedure, some patients who were prepared for TACE didn’t have CTA DICOM, and some patients who had HCC on tri-phasic CT refused diagnostic angiography.
Conclusions
MDCTA can provide effective information about the blood supply of HCC. The formation and patterns of the blood supply for HCC were closely related to tumour size and the superficial anatomic location of tumours; these findings would be helpful for the pre-TACE preparation of patients with HCC. We concluded that it is mandatory to do CTA as a preparation step for TACE that is good for detection of HCC blood supply, prevents recurrence after TACE, and gives a good prognosis. Another benefit noted in our study was that pre-TACE CTA provided a good plan for the intervention radiologists, which reduced and saved more time and, accordingly, reduced patients' radiation exposure.
Availability of data and materials
All data are available as sheets collected by authors.
Abbreviations
- MDCT:
-
Multi detector computed tomography
- CTA:
-
Computed tomography angiography
- TACE:
-
Transhepatic chemoembolization
- HCC:
-
Hepatocellular carcinoma
- CT:
-
Computed tomography
- DICOM:
-
Digital imaging and communication in medicine
- AFP:
-
Alpha-fetoprotein
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 10:3322
Ko HK, Ko GY, Yoon HK et al (2007) Tumor response to transcatheter arterial chemoembolization in recurrent hepatocellular carcinoma after living donor liver transplantation. Korean J Radiol 8:320–327
Cheng LF, Ma KF, Fan WC et al (2010) Hepatocellular carcinoma with extrahepatic collateral arterial supply. J Med Imaging Radiat Oncol 54:26–34
Nakai M, Sato M, Kawai N et al (2001) Hepatocellular carcinoma: involvement of the internal mammary artery. Radiology 219(1):147–152
Kim HC, Chung JW, Jae HJ et al (2008) Hepatocellular carcinoma: prediction of blood supply from an internal mammary artery with multi-detector row CT. J Vasc Interv Radiol 19:1419–1444
Park SI, Lee DY, Won JY et al (2008) Extrahepatic collateral supply of hepatocellular carcinoma by the intercostal arteries. J Vasc Interv Radiol 14(4):461–468
Kim HC, Chung JW, An S et al (2008) Hepatocellular carcinoma: detection of blood supply from the right inferior phrenic artery by the use of multi-detector row CT. J Vasc Interv Radiol 19(11):1551–1558
Miyayama S, Yamashiro M, Okuda M et al (2010) Hepatocellular carcinoma supplied by the right lumbar artery. Cardiovasc Intervent Radiol 33(1):53–60
Rajan DK, Ginzburg VE (2005) Hepatocellular carcinoma supplied the ileocolic branch of the superior mesenteric artery. Clin Radiol 60(6):723–726
Michels NA (1953) Collateral arterial pathways to the liver after ligation of the hepatic artery and removal of the celiac trunk. Cancer 6:708–724
Hiatt JR, Gabbay J, Busuttil RW (1994) Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg 220:50–52
Coskun M, Kayahan EM, Ozbek O et al (2005) Imaging of hepatic arterial anatomy for depiction vascular variations in living related liver donor candidate with multi detector computed tomography : comparison with conventional angiography. Transplant Proc 37(2):1070–1073
Sscoo R, Bertini M, Petruzzi P et al (2009) Clinical impact of selective transarterial chemoembolization on hepatocellular carcinoma: a cohort study. World J Gastroenterol 15(15):1843–1848
Cazejust J, Bessoud B, Colignon N et al (2014) Hepatocellular carcinoma vascularization: From the most common to the lesser known arteries. J Diagn Interv Imaging 6:27–36
Hefaiedh R, Ennaifer R, Romdhane H et al (2013) Gender difference in patients with hepatocellular carcinoma. Tunis Med 91:505–508
Tangkijvanich P, Mahachai V, Suwangoo P et al (2004) Gender difference in clinicopathologic features and survival of patients with hepatocellular carcinoma. World J Gastroenterol 10(11):1547–1550
Walter SR, Thein HH, Gidding HF et al (2011) Risk factors for hepatocellular carcinoma in a cohort infected with hepatitis B or C. J Gastroenterol Hepatol 26(12):1757–1764
Shaker MK, Abdella HM, Khalifa MO et al (2013) Epidemiological characteristics of hepatocellular carcinoma in Egypt: a retrospective analysis of 1313 cases. Liver Int 33(10):1601–1606
Kirchner G, Kirovski G, Hebestreit A et al (2010) Epidemiology and survival of patients with hepatocellular carcinoma in Southern Germany. Int J Clin Exp Med 3(2):169–179
Yuen MF, Cheng CC, Lauder IJ et al (2000) Early detection of hepatocellular carcinoma increases the chance of treatment: Hong Kong experience. Hepatology 31(2):330–335
Lee KH, Sung KB, Lee DY et al (2002) Trans catheter arterial chemoembolization for hepatocellular carcinoma: anatomic and hemodynamic considerations in the hepatic artery and portal vein. Radiographics 22(5):1077–1091
Moustafa AS, Abdel Aal AK, Ertel N et al (2017) Chemoembolization of hepatocellular carcinoma with extrahepatic collateral blood supply: anatomic and technical considerations. Radiographics 31:160122
Kim HC, Chung JW, Lee W et al (2005) Recognizing extrahepatic collateral vessels that supply hepatocellular carcinoma to avoid complications of transcatheter arterial chemoembolization. Radiographics 25(Suppl 1):25–39
Miyayama S, Matsui O, Taki K et al (2006) Extrahepatic blood supply to hepatocellular carcinoma: angiographic demonstration and transcatheter arterial chemoembolization. Cardiovasc Intervent Radiol 29(1):39–48
Ishikawa M, Yamagami T, Kakizawa H et al (2014) Transarterial therapy of hepatocellular carcinoma fed by the right renal capsular artery. J Vasc Interv Radiol 25(3):389–395
Lee IJ, Chung JW, Kim HC et al (2009) Extrahepatic collateral artery supply to the tumor thrombi of hepatocellular carcinoma invading inferior vena cava: the prevalence and determinant factors. J Vasc Interv Radiol 20(1):22–29
Hieda M, Toyota N, Kakizawa H et al (2008) Evaluation of hepatocellular carcinoma supplied by the right inferior phrenic artery at initial treatment. J Comput Assist Tomogr 32(6):877–881
Gwon DI, Ko GY, Yoon HK et al (2007) Inferior phrenic artery: anatomy, variations pathologic conditions, and interventional management. Radiographics 27(3):6
Wang YL, Li MH, Cheng YS et al (2005) Influential factors and formation of extrahepatic collateral artery in unresectable hepatocellular carcinoma. World J Gastroenterol 11(17):2637–2642
Chung JW, Kim HC, Yoon JH et al (2006) Transcatheter arterial chemoembolization of hepatocellular carcinoma: prevalence and causative factors of extrahepatic collateral arteries in 479 patients. Korean J Radiol 7(4):257–266
Gruttadauria S, Foglieni CS, Doria C et al (2001) The hepatic artery in liver transplantation and surgery: vascular anomalies in 701 cases. Clin Transplant 15(58):359–363
Acknowledgements
Staff member of Tanta University hospital especially radiology.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
RA correlated the study concept and design and had the major role in analysis, HM collected data in all stage of manuscript, performed data for analysis, BA supervised the study with significant contribution to design the methodology, manuscript revision and preparation. AM correlated the finding with clinical finding and managed the cases. All authors have and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consents taken from the patients, the study approved from ethical committee of faculty of medicine Tanta University number 33725/03/20.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abou Khadrah, R.S., Abedelmalik, M.H., Alameldeen, M.A.E. et al. Hepatocellular carcinoma vascularization: CT angiography variations identifying arteries feeding the tumour. Egypt J Radiol Nucl Med 54, 183 (2023). https://doi.org/10.1186/s43055-023-01133-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01133-7