Abstract
Background
Imaging requests are the first line of communication between the referring physician and the radiology department. The information provided allows the imaging team to choose the optimal examination for the clinical question. There are no imaging referral guidelines in Saudi Arabia. The Radiological Society of Saudi Arabia (RSSA) and Arabsafe have surveyed to develop an imaging referral tool in Saudi Arabia. This study aims to determine the most critical clinical information that should be included in an imaging request form in Saudi Arabia.
Methodology
A questionnaire was sent to the RSSA members to rank —using the Likert scale— the importance of 8 pieces of clinical information to discern what must be included in the imaging request form.
Results
The response rate was 80% of the RSSA members, which included 75 respondents, mostly Radiology consultants and residents in training. Radiologists carried different specialties and came from 4 main provinces in the Kingdom. 90.6% of Radiologists ranked the clinical question with relevant details as very important. The contact information of the requesting clinician came next in the ranking, with 82.3% scoring it as very important. The “very important” scores were 64.9% for the past medical history, 67.3% for past surgical history, 49.2% for laboratory, 38.3% for risk factors, and 56.7% for prior radiological studies. The RSSA-Arabsafe imaging request template was proposed because of the respondents’ votes to include all eight points: a clear clinical question relevant to the requested exam, the contact information of the referring physician, relevant surgical history, relevant medical history, past radiological tests if any, patient demographics, and relevant laboratory tests.
Conclusions
The RSSA-Arabsafe template is the first tool to improving imaging referrals and hence patients’ safety and services in Radiology departments in Saudi Arabia. It is crucial for healthcare institutions to actively implement standardized imaging request forms, such as the proposed RSSA-Arabsafe template, to reduce inappropriate referrals, enhance communications and optimize resource utilization.
Similar content being viewed by others
Background
Justifying imaging examinations that use ionizing radiation has become legal in many countries. [1] To do so, reviewing the referrals for appropriateness is needed. Many worldwide published referral guidelines and appropriate criteria databases have been evidence-based for over 25 years. These tools help identify the most appropriate imaging modality for given conditions and symptoms. Their positive impact has changed the quality of radiological services provided. Some of these available tools are the American College of Radiology (ACR) Appropriateness Criteria, the Royal College of Radiologists (RCR) iRefer, and the European Society of Radiology (ESR) iGuide [2,3,4].
The imaging request is the first line of communication between the referring physician and the radiology department. Without a doubt, the information provided on a request form allows the imaging team to choose the optimal scan parameters and ensure the correct acquisition technique is applied.
Appropriate clinical history has a direct impact on diagnosis accuracy. For example, research on early stroke diagnosis reported an increase in CT sensitivity from 38 to 52% when proper clinical history is provided [5].
Inappropriate clinical information in radiology requests is still of concern in Saudi Arabia as it is in the rest of the world. Published studies have shown that around 19–62% of the requests included misleading or inaccurate clinical information [5]. 30% of radiology referrals are found to be unjustified. Many radiology studies are performed without enough clinical information [6]. Reason for the exam ranges from the continuous pressing of one key on the keyboard to ambiguous words such as “pain,” “patient fell,” and “chief complaint” [5].
There are no published Saudi imaging request guidelines, especially for studies that utilize ionizing radiation. Inadequate clinical information, lack of referral criteria, and the absence of regulations for imaging justification led to unnecessary radiation exposure and wasteful resources. Imaging departments are challenged daily with referrals that fail to identify a clinical question or indication to perform the study.
The Radiological Society of Saudi Arabia (RSSA) has been promoting radiation safety throughout its activities and is one of the prominent supporters of Arabsafe. Jointly, RSSA and Arabsafe have surveyed to develop a tool for better imaging referrals in Saudi Arabia. The purpose of this study is to identify and prioritize the key clinical information that should be included in an imaging request form, with the aim of improving the appropriateness and quality of radiology referrals in Saudi Arabia. These efforts align with the Bonn Call for Action and local authorities’ attempts to establish guidelines for the diagnostic imaging practice.
Methods
A focused group of six radiologists with more than 15 years of experience was created. These radiologists were from different subspecialties, including abdominal imaging, cardiothoracic imaging, neuroimaging, musculoskeletal imaging, pediatric imaging, and women's imaging. They developed a questionnaire using google forms which were electronically distributed among ninety-four active RSSA members in the various regions of Saudi Arabia.
The questionnaire consisted of two main sections: participants’ demographics (position, age, gender, affiliation, and subspecialty) and what the participant thought was crucial clinical information that must be written in any Radiology study request form. They were given eight specific points to rank their importance using the Likert scale. Likert scale ranged from very important, to important, to neutral, to unimportant to very unimportant. The eight points were:
-
1.
Patient's demographics
-
2.
Clinical question to be answered by the study (with relevant details)
-
3.
Relevant past medical history
-
4.
Relevant past surgical history
-
5.
Pertinent labs
-
6.
Pertinent risks factors
-
7.
The presence of prior radiologic tests relevant to the requested study
-
8.
Contact information of the requesting clinician
The survey was conducted over 1 month by sending out emails and messages to the members of the RSSA. Responses were electronically analyzed in google docs and Excel Microsoft Corporation, 2018. Categorical data were described by frequencies with their percentages. Bar and pie charts were populated via Microsoft Excel.
Results
Of the ninety-four active RSSA members, seventy-five members fully completed the survey. This number represents an 80% response rate. The respondents’ demographics are shown in Table 1. The respondents came from the four main provinces of the Kingdom: Makkah, Madinah, Riyadh, and the Eastern Province. The distribution of the respondents by position is shown in Fig. 1.
Most respondents were general radiologists (30%), followed by abdominal radiologists (17.5%) and pediatric radiologists (12.5%), as shown in Fig. 2.
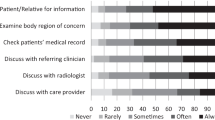
Figure 3 shows the radiologists' ranking of the level of importance for the different pieces of clinical information provided in the Radiology request. 100% of Radiologists ranked the clinical question with relevant details as important (with 90.6% ranking it as very important). The contact information of the requesting clinician came next in the ranking, with 82.3% scoring it as very important. Other clinical information scores for ¨very important¨ were as follows: past medical history (64.9%), past surgical history (67.3%), laboratory (49.2%), risk factors (38.3%), and prior radiological studies (56.7%).
Based on the importance to all the provided clinical information, an RSSA-Arabsafe imaging request template was proposed, as shown in Table 2. It included all 8 points since more than 80% of the participants scored all the provided clinical information as important.
Discussion
The Bonn Call for Action is a joint statement issued by the International Atomic Energy Agency (IAEA) and the World Health Organization (WHO) in December 2012, following the International Conference on Radiation Protection (ICRP) in Medicine in Bonn, Germany. The statement outlines a series of commitments to improve medical radiation protection. It calls for increased collaboration between international organizations and experts in the field and emphasizes the need for education and training in radiation protection for healthcare professionals. It calls for developing and implementing effective policies and guidelines for radiation protection and promoting research and innovation in this field. The statement also recognizes developing countries’ challenges in ensuring radiation safety in medicine and calls for increased support and assistance in this area [7].
There are several campaigns established in many countries under the umbrella of the International Society of Radiology (ISR) to implement the Bonn Call for Action, and Arabsafe is one of them [8]. Arabsafe, the initiative to adhere to the Bonn Call for Action in the Arab World, was inaugurated in 2017 and is a member campaign of the ISR Quality and Safety Alliance.
The RSSA and Arabsafe imaging request template (Table 2) is the first step to optimizing imaging requests in Saudi Arabia and improving radiation protection. This template proposes a framework for clinical teams to provide Radiologists with the necessary information to select the optimal imaging modality for the clinical question.
Numerous studies have been published worldwide to establish imaging request criteria or standards. For example, Castillo et al. [9] published standards for essential clinical information required in CT requests in the Australian emergency department (ED). The study involved a panel of 16 experts in ED radiology and clinical medicine [9].
An eight-category point system was used by Gunderman et al. “to ensure that the imaging is indicated, to ensure that the appropriate study is requested, to ensure that appropriate facilities are available, to prevent complications, to tailor the examination to key findings, to ensure that proper quality of images is provided to the referring physician, to derive the relevant differential diagnosis and to ensure that a specific clinical question is answered” [10].
Similarly, a grading system was developed by Abedi et al. [5] based on the guidelines for the communication of diagnostic imaging findings by the American College of Radiology (ACR). The Reason for Exam Imaging Reporting and Data System (RIRADS) is used to standardize the practice and solve the issue of inappropriate requests. According to RIRADS, “clinical information should include an indication for the exam, working diagnosis, chronicity, and location of signs and symptoms, mechanism of ailment, pertinent positives and negatives, any pertinent lab values, pertinent past medical and surgical histories, and any other significant clinical information” [5].
The Royal Australian and New Zealand College of Radiologists (RANZCR) has also developed structured customizable referral templates under the Quality Use of Diagnostic Imaging (QUDI) program to solve the issue of ambiguous referrals as well [11].
The RSSA-Arabsafe imaging request template was built in a similar method as Castillo et al. group [9], for the same purposes as Gunderman et al. [10] and with similar information to include as RIRADS [5]. And like the RANCR, the RSSA wishes to set guidance through the imaging request template for all the improvements—in patients’ care specifically and the health care systems wholly—this initiative can carry [12].
The diverse representation of radiology subspecialties in our survey is a crucial aspect of this study (Fig. 2). With 75 participants spanning various fields, we have gathered a comprehensive perspective on the information required in an imaging request template. This variation in expertise ensures that the resulting consensus on essential clinical information transcends individual subspecialties, reflecting a unified understanding of the needs across radiology as a whole. This agreement on a core set of universal information promotes effective communication, ultimately enhancing the quality of patient care and diagnostic accuracy.
Slovis et al. affirm that with the lack of appropriate clinical data, performing the correct study and optimizing it is jeopardized. Radiology teams are responsible for the quality of images, starting with choosing the correct study. If not provided with an indication or proper patient history, the chances of errors continue to occur [13].
Poor communication between referring physicians and radiologists is frequently cited as a cause for diagnostic errors and poor quality [14]. A lot of the literature studied ways to optimize radiology reports. Nonetheless, an essential part of communication is providing appropriate clinical information. Our participants from across the Kingdom and various subspecialties unanimously agreed that the clinical question and relevant details are essential to the imaging request.
Availability of the contact information of the requesting physician is an essential part of the imaging request, as 82.3% of our participants ranked it as very important. This information is essential to communicate to the clinical teams urgent and critical results. Cohen et al. mention some of the errors found in imaging requests, including wrong physician names and no contact numbers as essential ones [14].
Since the 1990s and 2000s, radiologists have anticipated that computerized integration between the hospital information system (HIS) and the picture archiving and communication system (PACS) would resolve poor imaging requests [13, 15]. However, the issue prevails even with governing bodies mandating justification and optimization for patient safety [16].
To address this, hospitals and imaging centers should adopt request templates such as RSSA-Arabsafe template (Table 2) into their HIS and PACS. Implementing this template may present challenges, including resistance to change, lack of technical support, and the need for ongoing education and training for healthcare workers. To overcome these challenges, stakeholders should engage healthcare professionals in the development and implementation process, provide ongoing education, training, and support for proper template use, and allocate resources to address technical issues such as software updates and data security. Establishing communication channels between clinical teams, radiology departments, and IT personnel is essential, as is monitoring and evaluating the effectiveness of implementation, adjusting as needed. By addressing these challenges, healthcare organizations can successfully implement the RSSA-Arabsafe templates, improving patient outcomes and optimizing diagnostic imaging resources.
This referral template can also be electronically integrated with published clinical decision support systems (CDS). There are successful examples of integration that include the UK’s Royal College of Radiologists (RCR) referral guidelines with the iRefer platform and the American College of Radiology (ACR) Appropriateness Criteria [2, 4]. Both provide evidence-based guidelines for appropriate imaging decisions.
In 2017, experts from 19 European countries of the European Society of Radiology (ESR) identified areas for improvement regarding imaging referrals. They urgently recommended implementing evidence-based imaging referral guidelines and justification using clinical decision support systems, with healthcare teams working collaboratively [17]. Radiologists were suggested to have the “gatekeeper role” in amending or returning requests that do not meet the standards. Consequently, the ESR iGuide was founded, integrating the ACR appropriateness criteria into a CDS. This tool is freely available for individual clinicians and can be licensed institutionally [3].
Referring clinicians and radiographers play a crucial role in the successful implementation and adherence to the RSSA-Arabsafe template. Education and continuous feedback are indispensable components in ensuring that imaging requests meet acceptable standards. Moreover, the sustained and proper use of the template demands persistent efforts from both clinical teams and radiology departments.
Gunderman et al. demonstrated that after implementing imaging request templates, the number of non-compliant requests notably decreased. However, achieving long-term improvement necessitated time and dedication. The authors concluded that educating referring physicians is a vital factor for compliance with the established criteria for imaging requests. [10]
Additionally, a survey examining radiographers' responses to incomplete or missing request forms revealed that when requests were unjustified, 69% of radiographers would consult the radiologist or referring physician, but only 36% would return an inappropriate referral to the physician [18]. This highlights the importance of educating radiographers in maintaining appropriate imaging referrals. As the primary point of contact with patients, radiographers assume a critical “gatekeeper role,” as underscored by the ESR. By empowering both referring clinicians and radiographers with the knowledge and tools to effectively use the RSSA-Arabsafe template, we can achieve better patient outcomes and optimize the use of diagnostic imaging resources.
Despite some limitations and biases, the study found consensus among the small number of participants across various specialties, ages, and career positions on the importance of the identified pieces of clinical information. One potential limitation is sampling bias, as participants were primarily members of the RSSA and may not represent the broader radiology community in all provinces of the kingdom. By focusing on RSSA members, the study could have missed perspectives from radiologists in other provinces or those not affiliated with the society. Nevertheless, the strong agreement among respondents in selecting “important” and “very important” on the Likert scale suggests that their collective opinions are likely valid and meaningful for radiology practice in the given context. Expanding the sample size may not significantly change the study's findings, but future research could consider including a more diverse group of radiologists to further validate the results.
The RSSA and Arabsafe are dedicated to fostering a safer and higher-quality diagnostic imaging practice. By conducting continuous research and employing effective implementation strategies, the goals of standardized imaging request forms and improved quality and safety of patient care in radiology can be realized.
The next step in this initiative should be implementing the RSSA-Arabsafe template in a medical facility and thoroughly examining the implementation process from all aspects. This includes addressing information technology challenges, integration with HIS and PACS, and educating clinical teams and radiology staff on the importance and constituents of a complete referral form.
Through collaborative efforts with governing agencies in the Kingdom, the RSSA can facilitate the implementation of such initiatives across the region. Moreover, the RSSA can leverage its educational events and social media outreach to reinforce proper radiology practices, ultimately making a significant impact on the quality and safety of imaging services.
In conclusion, the RSSA-Arabsafe template has the potential to revolutionize imaging requests and elevate the standard of care in radiology in Saudi Arabia. By embracing this tool and overcoming implementation challenges, healthcare organizations can ensure the well-being of their patients and contribute to a safer, more effective diagnostic imaging landscape.
Conclusions
In conclusion, standardized imaging request forms are an essential tool to improve the quality and safety of patient care, enhance radiology workflow and efficiency, and reduce healthcare costs. Implementing standardized imaging request forms can help ensure that essential clinical information is consistently and accurately communicated between clinicians and radiologists, resulting in improved patient outcomes and increased patient satisfaction. It is paramount that healthcare institutions prioritize developing and implementing standardized imaging request forms to improve the quality and safety of healthcare services.
Availability of data and materials
The datasets generated and/or analyzed during the current study is available in the RSSA database.
Abbreviations
- RSSA:
-
Radiological Society of Saudi Arabia
- HIS:
-
Hospital information system
- PACS:
-
Picture archiving and communication system
- ACR:
-
American College of Radiology
- ESR:
-
European Society of Radiology
- CDS:
-
Clinical decision support systems
- ISR:
-
International Society of Radiology
- RANZCR:
-
Royal Australian and New Zealand College of Radiologists
- WHO:
-
World Health Organization
- RCR:
-
Royal College of Radiologists
- RIRADS:
-
Reason for Exam Imaging Reporting and Data System
- ICRP:
-
International Conference on Radiation Protection
- CT:
-
Computed tomography
- ED:
-
Emergency department
References
Chilanga CC, Lysdahl KB, Olerud HM et al (2020) Radiographers’ assessment of referrals for CT and MR imaging using a web-based data collection tool. Radiography. https://doi.org/10.1016/j.radi.2020.04.001
iRefer from the Royal College of Radiologists. https://www.irefer.org.uk/
European Society of Radiology (ESR) communications@ myesr. org. (2019) Methodology for ESR iGuide content. Insights Imaging 10:32. https://doi.org/10.1186/s13244-019-0720-z
Subramaniam RM, Kurth DA, Waldrip CA, Rybicki FJ (2019) American college of radiology appropriateness criteria: advancing evidence-based imaging practice. Semin Nucl Med 49:161–165. https://doi.org/10.1053/j.semnuclmed.2018.11.011
Abedi A, Tofighi S, Salehi S et al (2019) Reason for exam imaging reporting and data system (RI-RADS): a grading system to standardize radiology requisitions. Eur J Radiol. https://doi.org/10.1016/j.ejrad.2019.108661
Mork-Knudsen H, Lysdahl KB, Chilanga CC (2022) Workplace factors facilitating the radiographers’ assessment of referrals for diagnostic imaging: a qualitative study. Radiography. https://doi.org/10.1016/j.radi.2021.07.013
IAEA, WHO (2013) Bonn call for action: 10 actions to improve radiation protection in medicine in the next decade
ISR’s Quality and Safety Alliance (ISRQSA) (2017) ISR welcomes formal establishment of Arabsafe. http://www.isradiology.org/quality-arabsafe
Castillo C, Steffens T, Livesay G et al (2022) <scp>IMPACT</scp> (Information medically pertinent in acute computed tomography) requests: delphi study to develop criteria standards for adequate clinical information in computed tomography requests in the Australian emergency department. J Med Radiat Sci 69:421–430. https://doi.org/10.1002/jmrs.607
Gunderman RB, Phillips MD, Cohen MD (2001) Improving clinical histories on radiology requisitions. Acad Radiol 8:299–303. https://doi.org/10.1016/S1076-6332(03)80498-1
Pitman GA (2017) Quality of referral: what information should be included in a request for diagnostic imaging when a patient is referred to a clinical radiologist? J Med Imaging Radiat Oncol. https://doi.org/10.1111/1754-9485.12577
Radiological Society of Saudi Arabia (RSSA). RSSA. https://rssa.sa/. Accessed 14 May 2023
Slovis TL, Frush D (2005) Getting back to basics. Pediatr Radiol 35:839–840
Cohen MD (2007) Accuracy of information on imaging requisitions: does it matter? J Am Coll Radiol. https://doi.org/10.1016/j.jacr.2007.02.003
Schuster DM, Elon Gale M (1996) The malady of incomplete, inadequate, and inaccurate radiology requisition histories: a computerized treatment. Am J Roentgenol 167:855–859
IAEA (2018) IAEA SAFETY STANDARDS for protecting people and the environment radiation protection and safety in medical uses of ionizing radiation
Remedios D, Brkljacic B, Ebdon-Jackson S et al (2018) Collaboration, campaigns, and champions for appropriate imaging: feedback from the Zagreb workshop. Insights Imaging. https://doi.org/10.1007/s13244-018-0602-9
Chilanga CC, Olerud HM, Lysdahl KB (2022) Radiographers’ actions and challenges when confronted with inappropriate radiology referrals. Eur Radiol 32:4210–4217. https://doi.org/10.1007/s00330-021-08470-z
Acknowledgements
Radiological Society of Saudi Arabia (RSSA) and The Arabsafe Initiative.
Funding
No sources of funding for the research.
Author information
Authors and Affiliations
Contributions
SA interpreted the data and drafted the work. MK interpreted the data and substantively revised the drafted work. LJ design the work and acquisition. AB acquired and substantively revised the drafted work. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albahiti, S., Khafaji, M., Jamjoom, L. et al. Improving inappropriate radiology referrals: a template for imaging requests in Saudi Arabia. Egypt J Radiol Nucl Med 54, 138 (2023). https://doi.org/10.1186/s43055-023-01082-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01082-1