Abstract
Background
Radiology professionals are frequently confronted with referrals containing insufficient clinical information, which hinders delivery of safe and quality medical imaging services. There is however lack of knowledge on why and how referral information is important for radiographers in clinical practice. This study explores what purposes referral information is used/ useful for the radiographers, and the benefits of involving them in assessing referrals.
Methods
A cross sectional study was conducted of radiographers recruited through the International Society of Radiographers and Radiological Technologists (ISRRT) networks. A questionnaire was developed and distributed consisting of 5-point Likert scale questions on a) use/usefulness of referral information for 12 listed purposes and b) the benefits of radiographers assessing referrals for 8 possible reasons. The questionnaire was validated using a test–retest reliability analysis. Kappa values ≥0.6 were accepted. SPSS software was used for data analysis and chi-square tests to determine associations between using referral information and background variables.
Results
Total respondents were 279 (n = 233 currently in clinical practice and n = 46 in other positions). The participants in clinical practice ranked high all 12 listed purposes for use of referral information, and all except one received ≥60% ‘frequent’/‘very frequent’ responses. Use for patient identification purposes received the highest score (97% ‘frequently’/‘very frequently’ responses), followed by ensuring imaging of the correct body region (79% ‘very frequently’ responses). Radiographers not currently working in clinical practice ranked the ‘usefulness’ of listed items similarly. Significant associations between frequent use of referral information and education level were not observed, and only three items were significantly associated with modality of practice. All items on benefits of radiographers assessing referrals received ≥75% ‘agree’/‘strongly agree’ scores. The items ranked highest were promotes radiographers’ professional responsibility and improves collaboration with radiologists and referring clinicians, with 72 and 67% strongly agreed responses, respectively.
Conclusion
Radiographers use referral information frequently for several purposes. The referral information is needed for justifying and optimising radiological procedures, hence crucial for ensuring patient safety and high-quality services. This further emphasis why radiographers perceive several benefits of being involved in assessing the referral information.
Similar content being viewed by others
Background
When requesting a radiological procedure, the referring clinician sends a referral (request) form containing the patients’ relevant clinical information to the radiology department [1]. This information is vital for patients’ quality care and utilisation of services in radiology departments [2, 3]. The radiologists and radiographers assess the referral information to determine whether the requested radiological examination is warranted and appropriate to confirm or rule out diagnosis of a given condition or disease [4]. Selecting the most appropriate examination prevents patients’ exposure to unnecessary radiation doses in instances where ionising radiation is used [5]. The patients’ safety when conducting radiological examinations is also dependent on the information in the referral. The radiologists and radiographers will need information about the patients’ identity [2], general physical condition and pre-existing illnesses to ensure safety during the procedure [6]. This could be particularly critical when the procedure requires using contrast-media to better visualise anatomy, [7] as contrast media is known to cause adverse effects in patients with certain pre-existing medical conditions [8,9,10,11].
The referral information determines patient and procedure information such as radiographic patient positioning, procedure projections and exposure parameters [6, 12]. High quality referral information also enables better radiologist – radiographer communication on visualisation of pathology and suitable radiographic technique to employ to obtain imaging of diagnostic value [13]. The radiographers could further liaise with the radiologists on acceptable images, taking account of the patients’ condition. The radiology report sent to the referring clinician of the outcome of the procedure is also influenced by the referral information. Studies show that referrals of high information quality improve image interpretation accuracy, clinical relevance, and reporting confidence for the radiologists [14]. The referral information is therefore useful for verifications about a patient and procedures [15], and procedure decision-making [6, 16] along the medical-imaging care continuum.
Referral information accordingly influences the quality of the outcome of the services provided in radiology departments. Inadequate referral information is reported as a cause of false positive diagnosis and incidental findings in medical imaging [17, 18], which instigates futile patient follow-up investigation and treatment, and consequently leading to unnecessary overuse of health resources and services [18]. Scheduling of the radiology examination according to priority or urgency is effectively conducted using the information on the referral [16]. The referral quality therefore potentially affects practicing according to healthcare priority setting criteria.
Despite the many indications outlined above on the value of referral information there is little evidence of why and how this is important in clinical practice for radiographers. This study aimed to map the value of referral information and assessment from the perceptive of radiographers working in clinical and non-clinical settings. The objectives were two-fold; to explore a) for what purpose the radiographers make use of referral information or consider it useful and b) the possible benefits of involving radiographers in assessing referrals.
Methods
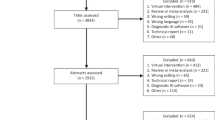
This research is the second part of a larger study on radiographers’ involvement in the process of assessing imaging referrals. The first part of the study analysed the radiographers’ actions and challenges when confronted with unjustified radiology referrals and the paper [19] provides more detail on methods.
Study settings
A cross sectional study was conducted of radiographers internationally who follow activities organised by the International Society of Radiographers and Radiological Technologists (ISRRT). The ISRRT is the professional organisation representing radiographers globally and its mission is to improve the standards of delivery and practice of diagnostic imaging and radiation therapy worldwide [20]. The target group were radiographers currently working in clinical practice in various imaging modalities (clinical radiographers) and those not in clinical practice but have clinical experience in diagnostic radiography (non- current clinical radiographers i.e. radiography administrators, researchers and educators).
Participant recruitment and data collection
An online survey was distributed using a web form (‘Nettskjema’) [21] for 5 months, initially in April 2020 and between September and December 2020. The recruitment of participants and data collection was conducted using ISRRT networks (see [19]). Non-probabilistic, convenience sampling methods were employed to collect the data. The targeted sample population was selected because it constitutes of radiographers who are assumed to be active in the profession and familiar or well orientated with practice regulations in their respective countries.
Questionnaire
A questionnaire was piloted and validated using a test–retest reliability analysis. In the first part of this section of the study, questions about perceived usefulness of referral information were asked. The questions were phrased slightly different for radiographers working in clinical and non-clinical settings. After the statement ‘Information in the referral can be useful for a number of reasons. The radiographers working in clinical setting were asked to rate how often they make use of the referral information for 12 listed number of purposes, while radiographers not currently working in a clinical setting were asked to rate their agreement on the usefulness of the same 12 purposes. A five-point Likert response scale was used in both cases ‘Very frequently, Frequently, Occasionally, Rarely, Never’ and ‘Strongly agree, Agree, Undecided, Disagree, Strongly disagree’, for clinical radiographers and non- current clinical radiographers respectively.
For the second main question, all the participants were asked to rate their agreement (scale: strongly agree, agree, undecided, disagree, strongly disagree), on possible benefits of involving radiographers in assessing radiology referrals. A set of 8 possible benefits were listed. The background section included demographics and professional characteristics of the participants.
Data analysis
The data was analysed using IBM SPSS statistical software version 26. Descriptive analysis was used to show frequency in percentages. The data was split in to 2 cohorts: radiographers in clinical and non-clinical settings to compare variations in responses between the two groups. To analyse difference in how subgroup of clinical radiographers reported their use of referral information, the scales were dichotomised into frequently to never (1) and very frequently (2), based on the response pattern. A chi-square test of independence was used to determine association between the clinical radiographers perceived use of referral information, with the independent variables: dichotomised education level (Bachelor’s degree/equivalent versus master/PhD degree), and 3 split modality of practice (Conventional radiography versus One advanced modality which included CT, MRI, Ultrasound, Mammography or Nuclear medicine, versus Multiple modalities). A p value ≤0.05 was considered statistically significant.
Ethics statement
Ethical approvals were obtained from the Norwegian centre for research data (NSD) reference number 472337 in Norway. All the participants consented to the study through the online portal.
Results
Respondents and settings characteristics
The total number of respondents were 279 (n = 233 clinical radiographers, n = 46 non-current clinical radiographers), as in Table 1. Most of the respondents where from Asia (Indonesia/Taiwan) (28%), United Kingdom (UK) (23%), Scandinavia (Norway/Denmark) (12%), and Australia (11%). The mean age was 38 years. A total 74% of the participants had education level at bachelor’s degree or equivalent. Modality of practice of the participants was reported as follows; 35% conventional radiography, 32% one advanced modality and 33% multiple modalities.
Use/usefulness of referral information
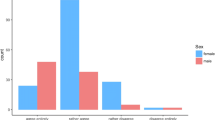
The radiographers in clinical practice reported to very frequently use information in the referral for a variety of reasons (Fig. 1). The radiographers not-currently in clinical settings were also mostly in agreement to the usefulness of the referral information as reported by those in clinical practice (Fig. 2). Details on both groups’ responses follows subsequently.
Clinical radiographers
Some of the reasons for use of the referral information concerns verification of the patient, which all received high scores. The clinical radiographers rated using the referral information for patient identification highest with combined score of ‘frequently’/‘very frequently’ responses of 97%. Using the referral information to ensure imaging of the correct body region was rated quite high at 79% ‘very frequently’ used responses. This was followed by scores ‘very frequently’ using the information for obtaining previous imaging information (59%).
Other reasons for using the referral information for processes are related to patient positioning, where a rank of ‘very frequently’ responses was obtained for ensuring correct patient position (66%) and selection of appropriate projections (63%). The lowest rank related to patient positioning aspects was ‘very frequently’ to use the information for ensuring the patients’ comfort during the procedure (36%) and assessing if the patient can tolerate to undergo the procedure (35%).
A third group of items concerned use the referral information for procedure decisions, were the highest number of ‘very frequently’ used responses was given for selecting the appropriate exposure parameters, selecting the appropriate imaging modality, and administration of pharmaceuticals (such contrast media, radioisotopes) as 50, 48 and 47% respectively. The lowest rank in this category was ‘very frequently’ using the information in accessing lab results, rated by 32% of respondents.
The overall lowest score was obtained for using the referral to inform the patient of possible diagnosis stated, with 63% ‘never/rarely/occasionally’ responses.
A chi square test performed (Table 2) showed significant association between a few of the variables (items) on the purposes of radiographers’ frequent use of referral information and modality of practice. No significant associations were observed between the use of referral information in the listed items and the dependent variable education level.
Non-current clinical practice radiographers
A similar rating in agreement on usefulness of referral information by the non-current clinical radiographers was observed (Fig. 2). The radiographers not currently working in clinical practice ranked high the usefulness of referral information for patient verification as follows; combined ‘agree’/‘strongly agree’ on patient identification (100%) and ‘strongly agreed’ on ensuring imaging of the correct body region responses (63%). However, agreement as useful to obtain previous imaging information was ranked lower by the non-current clinical radiographers, 46% ‘strongly agreed’ compared to ‘very frequent’ used score stated by 59% clinical radiographers.
Using the referral information for processes of patient position was rated ‘strongly agreed’ for ensuring correct patient position 52% and selecting the appropriate projections 50%. Using the referral information for assessing if the patient can tolerate to undergo the procedure and ensuring the patients’ comfort during the procedure were ranked low in this category as 30 and 26% respectively.
In procedure decisions, the non-current clinical practice radiographers rated use for administration of pharmaceuticals and selecting the appropriate imaging modality as 48 and 46% ‘strongly agreed’ responses respectively. In this category using the information for ‘selecting the appropriate exposure parameters’, and ‘accessing lab results’, was ranked lowest as 33 and 22%, ‘strongly agreed’ responses. Use of the referral information in ‘informing the patient of possible diagnosis’ was however rated higher compared to the clinical radiographers, with combined ranked as useful ‘strongly agreed’/‘agreed scores’ 57% (non- current clinical radiographers) versus 37% ‘very frequent’/‘frequent’ used scores’ (clinical radiographers).
Benefits of involving radiographers in referral assessment
In general, the clinical and non-current clinical radiographers provided similar responses on the benefit of involving radiographers in referral assessment. All the listed items (Fig. 3) contained benefits to the patients in shape of quality of care and services, some directly and others more indirect originating from benefits of the healthcare professionals providing the care and services. In total these categories are ranked similarly. Among the items related to direct benefits for quality of care and services, the high ranked were ‘promotes radiographers’ professional responsibility’, ‘enables efficient use of radiology services’, ‘improves the radiographer-patient communication’, and ‘reduces incidences and errors’, receiving 72, 57, 56 and 52% ‘strongly agreed’ responses respectively. Improves the patients’ radiology report was low ranked (‘strongly agreed’ responses by 38% radiographers).
In the category of benefits to the healthcare professionals, the items that ranked high were ‘improves radiographers’ collaboration with radiologists and referring clinicians’ and ‘promotes sharing of tasks among radiology staff’, with 67 and 53% ‘strongly agree’ responses respectively. The lowest score in this category was ‘reduces the burden of the radiologists’ workload’ (37% ‘strongly agree’ responses).
Discussion
Our study shows radiographers in various imaging modalities frequently making use of referral information for several activities across the imaging care continuum to manage the patient. The crucial value of referral information may not be well known outside the radiology environment. This lack of awareness may be one of the reasons why referrals lacking vital clinical information seems to be a persistent problem [22,23,24,25]. Our study shows that radiographers need proper referral information to ensure patient safety, high quality care and services in radiology departments.
Use of referral information for radiographers’ clinical practice
Our study shows radiographers using the referral information to identify the patient, verify information about the patient and the procedure. Almost all the respondents in our study stated the referral information to be very useful to identify the patient. Ensuring that the radiological procedure is delivered to the correct patient is the starting point of patient safety [15]. The participants further ranked high using the referral information for correct patient position and selection of appropriate radiographic projections which ensures that imaging of diagnostic value is obtained and enable an accurate diagnosis. Patient identification and ensuring the appropriate imaging procedure are selected and conducted optimally further adhere to the two core principles of radiation protection in medicine termed ‘justification’ and ‘optimisation’. The justification principle affirms that the benefits of medical imaging for patients should outweigh the radiation risks and other possible risks [5]. This entails that the radiographers evaluate the referral information against the requested radiological procedure and ensure that the correct imaging modality is selected before performing the procedure. This further ensures that the patient is not exposed to unnecessary risks due to the procedure. Optimisation ensures that radiation doses when used are kept as low as reasonably achievable (ALARA), and imaging of diagnostic value is obtained [5]. During optimisation the imaging procedure, doses, parameters, use of contrast media, and other drugs must be adapted to the individuals’ specific clinical question [7]. Optimisation of procedures will therefore require that the radiographers select the most appropriate radiographic projects and exposure parameters to ensure that the procedure is optimally conducted with the minimum possible radiation exposures to the patient.
Using the referral information for assessing laboratory results and administration of pharmaceuticals is observed in our study mainly in clinical radiographers working in advanced imaging modalities. This was anticipated as most advanced imaging procedures use contrast medium which causes some adverse reactions in certain patients [26]. For example, checking of laboratory results such as blood tests that show estimated glomerular filtration rate can determine kidney function status in patients receiving contrast enhanced imaging [11], and ensures safety use of contrast media during imaging procedures.
In the chi square test analysis in our study, no significant associations were observed between the items on radiographer’s use of clinical information and the dependent variable education level. This indicates that referral information is frequently used by all radiographers’ and at all levels in clinical practice. Our results support those by Lundvall, et al. [27] that states that the radiographers’ professional work and responsibilities in image production involves a process of planning, producing the images, and evaluation, where one of the main features of their professional work is patient safety.
Benefits of radiographers’ assessing referrals
Our study show that the radiographer’s assessing referrals directly or indirectly facilitates provision of quality care and services in radiology departments. First, the respondents in our study ranked highly that radiographers’ assessing referrals improves professional collaboration with radiologists and referring clinicians and promotes sharing of professional tasks. This indicates that radiographers assessing referrals has benefits for the professionals working within the patients’ referral pathway, which indirectly enhances quality of care and health services. Interprofessional collaborative practice occurs when professionals with different backgrounds work together to deliver the highest quality of healthcare [28]. This provides platforms for better professional communication and teamwork which further support quality patient management across the care pathway [29]. Professional task sharing does not only assist with efficient distribution and organises of work tasks, but also facilitates transfer of knowledge and skills among professions. Knowledge sharing among the radiology professionals is reported to assist with professional development and creates a supporting environment for the radiographers [30]. Supporting environments are further reported to increase job satisfaction of healthcare professionals [31], in turn facilitating provision of quality care.
Second the respondents in our study ranked highly that radiographers assessing referrals promotes professional responsibility. Professional responsibility in healthcare relates to how one performs their work based on ethical values and expected professional standards [32]. Professional responsibility therefore promotes commitment to ensuring quality care. The third factor the respondents ranked high for benefits of radiographers assessing referrals in our study was that it enables efficient use of radiology services. Our findings are supported by Sheth et al. [33], that report that not only does radiographers’ involvement in assessing referrals improve patients’ safety and experience, but also provides an efficient workflow in radiology department. The other benefits to radiographers assessing referral ranked high in our study included, improves the radiographer-patient communication, and reduces incidences and errors. Studies show that through patient communication, radiographers gather vital information about the patient which adds to the patient’s clinical history and is valuable for overall health management [27]. This further reduces incidences and errors [6] and improves the justification and optimisation processes [34]. Ensuring occurrence of justification and optimisation in radiology departments further prevents over-utilisation of radiology resources as unwarranted and repeated imaging is avoided and high- quality imaging of diagnostic value is provided.
Strength and limitations of study
This study had some limitations. The number of participants were quite low as expected of online survey and the recruitment process. In addition, language contributed to non-responses as the survey was only in English. The difference in organisational processes in radiography departments and country practice legislations could have influenced the radiographers’ responses on how they make use of referral information within their respective institutions. A focused study of individual centres in selected countries could provide better detail on ways and differences radiographers use the referral information. The analysis of responses in the study were however based on expected or required standard practice. The responses on the benefits to assessing referral could be biased towards the radiography profession as the included sample group were only radiographers. The recruitment process indicates that the sample group are not representative for radiographers world-wide, which is an obvious limitation. On the other hand, this sample of radiographers are assumed to be well versed in the profession and assumed to be quite knowledgeable and experienced about the current and expected practices in their various clinical practices and respective countries. This could have strengthened our findings.
Conclusion
Information in the referral is vital for radiographers’ clinical practice and is used frequently for several purposes. The referral information is needed for justifying and optimising radiological procedures, hence crucial for ensuring patient safety and high-quality care and services. It is therefore vital that radiographers are trained to systematically evaluate and supplement referral information in clinical practice. Radiographers’ involvement in assessing referrals further promotes provision of quality professional work based on ethical values and standards.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALARA:
-
As Low As Reasonably Achievable
- CT:
-
Computed Tomography
- ISRRT:
-
The International Society of Radiographers and Radiological Technologists
- MRI:
-
Magnetic Resonance Imaging
References
Vom J, Williams I. Justification of radiographic examinations: what are the key issues? J Med Radiat Sci. 2017;64(3):212–9.
Pitman AG. Quality of referral: what information should be included in a request for diagnostic imaging when a patient is referred to a clinical radiologist? J Med Imaging Radiat Oncol. 2017;61(3):299–303.
Armao D, Semelka RC, Elias J Jr. Radiology’s ethical responsibility for healthcare reform: tempering the overutilization of medical imaging and trimming down a heavyweight. J Magn Reson Imaging. 2012;35(3):512–7.
The Ionising Radiation (Medical Exposure) Regulations IR(ME)R 2017: The Ionising Radiation (Medical Exposure) Regulations 2017. No. 1322. Available from https://www.legislation.gov.uk/uksi/2017/1322/contents/made. Accessed 31 Mar 2022.
International Atomic Energy Agency (IAEA). IAEA Safety Standards for protecting people and the environment: Radiation Protection and Safety in Medical Uses of Ionizing Radiation. IAEA Safety Standards Series No SSG-46. Vienna: IAEA; 2018. Available from: https://www-pub.iaea.org/MTCD/Publications/PDF/PUB1775_web.pdf. Accessed 31 Mar 2022.
Wallin A, Gustafsson M, Anderzen Carlsson A, Lunden M. Radiographers’ experience of risks for patient safety incidents in the radiology department. J Clin Nurs. 2019;28(7–8):1125–34.
European Society of Radiology ESR. European Federation of Radiographer Societies EFRS: patient safety in medical imaging: a joint paper of the European Society of Radiology (ESR) and the European Federation of Radiographer Societies (EFRS). Insights Imaging. 2019;10(1):45.
van der Molen AJ, Reimer P, Dekkers IA, Bongartz G, Bellin MF, Bertolotto M, et al. Post-contrast acute kidney injury. Part 2: risk stratification, role of hydration and other prophylactic measures, patients taking metformin and chronic dialysis patients : recommendations for updated ESUR contrast medium safety committee guidelines. Eur Radiol. 2018;28(7):2856–69.
Davenport MS, Perazella MA, Yee J, Dillman JR, Fine D, McDonald RJ, et al. Use of intravenous iodinated contrast Media in Patients with kidney disease: consensus statements from the American College of Radiology and the National Kidney Foundation. Radiology. 2020;294(3):660–8.
Beckett KR, Moriarity AK, Langer JM. Safe use of contrast media: what the radiologist needs to know. Radiographics. 2015;35(6):1738.
Moos SI, van Vemde DN, Stoker J, Bipat S. Contrast induced nephropathy in patients undergoing intravenous (IV) contrast enhanced computed tomography (CECT) and the relationship with risk factors: a meta-analysis. Eur J Radiol. 2013;82(9):e387–99.
Abohaikel AS, Musa HH, Lysdahl KB. Radiographers’ perception of suboptimal referrals for plain radiography – a qualitative study. Radiogr Open. 2018;4(1):17.
Lundvall L-LC, Dahlström N, Abrandt DM. Professional challenges in medical imaging for providing safe medical service. Prof Professionalism. 2021;11(2):e3091.
Castillo C, Steffens T, Sim L, Caffery L. The effect of clinical information on radiology reporting: a systematic review. J Med Radiat Sci. 2020:60–74.
Field C. Adapting verification processes to prevent wrong radiology events. Harrisburg: Pennsylvania Patient Safety Authority; 2018.
Fatahi N, Krupic F, Hellstrom M. Quality of radiologists’ communication with other clinicians--As experienced by radiologists. Patient Educ Couns. 2015;98(6):722–7.
Lumbreras B, Donat L, Hernandez-Aguado I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol. 2010;83(988):276–89.
Salerno S, Laghi A, Cantone MC, Sartori P, Pinto A, Frija G. Overdiagnosis and overimaging: an ethical issue for radiological protection. Radiol Med. 2019;124:714–20.
Chilanga CC, Olerud HM, Lysdahl KB. Radiographers’ actions and challenges when confronted with inappropriate radiology referrals. Eur Radiol. 2022;32(6):4210–17.
International society of radiographer and radiological technologists (ISRRT) World health organisation (WHO) and the ISRRT. Available from: https://www.isrrt.org/who#:~:text=As%20an%20officially%20recognized%20NGO%20the%20ISRRT%20facilitates,WHO%20on%20a%20variety%20of%20topics%20and%20projects. Accessed 21 Jan 2022.
University Of Oslo (UiO). Short introduction to Nettskjema 2018 Available from: https://www.uio.no/english/services/it/adm-services/nettskjema/about-nettskjema.html. Accessed 30 Nov 2019.
Rawle M, Pighills A. Prevalence of unjustified emergency department x-ray examination referrals performed in a regional Queensland hospital: a pilot study. J Med Radiat Sci. 2018;65(3):184–91.
Almén A, Leitz W, Richter S. National Survey of justification of CT examinations in Sweden. Swedish Rad Saf Authority. 2009: SSM 03. Available from: https://www.osti.gov/etdeweb/servlets/purl/948944. Accessed 31 Mar 2022.
Ihuhua P, Pitcher RD. Is the devil in the detail? The quality and clinical impact of information provided on requests for non-trauma emergency abdominal CT scans. Acta Radiol. 2016;57(10):1217–22.
Vilar-Palop J, Hernandez-Aguado I, Pastor-Valero M, Vilar J, Gonzalez-Alvarez I, Lumbreras B. Appropriate use of medical imaging in two Spanish public hospitals: a cross-sectional analysis. BMJ Open. 2018;8(3):e019535.
Brenner DJ, Hricak H. Radiation exposure from medical imaging: time to regulate? JAMA. 2010;304(2):208–9.
Lundvall L-L, Dahlgren MA, Wirell S. Professionals’ experiences of imaging in the radiography process – a phenomenological approach. Radiography. 2014;20(1):48–52.
Gittell JH, Godfrey M, Thistlethwaite J. Interprofessional collaborative practice and relational coordination: improving healthcare through relationships. J Interprof Care. 2013;27(3):210–3.
Strudwick RM, Day J. Interprofessional working in diagnostic radiography. Radiography. 2014;20(3):235–40.
Mork-Knudsen H, Lysdahl KB, Chilanga CC. Workplace factors facilitating the radiographers’ assessment of referrals for diagnostic imaging - a qualitative study. Radiography. 2021;28(1):24–30.
Choi J, Kim DE, Yoon JY. Person-centered care environment associated with care staff outcomes in long-term care facilities. J Nurs Res. 2021;29(1):e133.
Soltabian M, Molazem Z, Mohammadi E, Sharif F, Rakhsan M. Professional Responsibilty : an ethical concept extracted from practices of Iranian nurses during drug administration. Int J Pharm Res. 2018;10(3):346–53.
Sheth S, Mudge B, Fishman EK. The pre-CT checklist: a simple tool to improve workflow and patient safety in an outpatient CT setting. Clin Imaging. 2020;66:101–5.
Makanjee CR, Bergh A, Hoffmann WA. Patients’ journeys through multi- level diagnostic imaging referrals. South African Radiographer. 2015;53(1):11–6.
Acknowledgements
We wish to thank the International Society of Radiographers and Radiological Technologists (ISRRT) and their respective affiliated national societies that facilitated the research and assisted in the distribution of the research questionnaire.
Funding
This research was conducted as part of a PhD Scholarship at the University of South-eastern Norway (USN). No personal funding was received by the authors.
Author information
Authors and Affiliations
Contributions
In the planning of the research all authors HO, KL and CC were involved. The design of the questionnaire and validation analysis were mainly done by CC and KL. HO contributed to the edit, revision, and validation analysis of the questionnaire. KL and HO facilitated the distribution of the questionnaire. The distribution of the questionnaire and follow up of data collection was conducted by CC. The sorting of data was conducted by CC. All the authors CC, HO and KL discussed and reviewed all the processed data and the final data analysis. The manuscript was written by CC. HO and KL edited and reviewed all parts of the manuscript. All the authors approved submission of the final manuscript. CC submitted the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Norwegian centre for research data (Norsk senter for forskningsdata) NSD review board in Norway granted the ethical approval for this study, reference number 472337. Written information about the study was given to all the participants and informed consent obtained using an online portal. All methods used for data collection and processing were performed in accordance with the NSD standard ethical guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chilanga, C.C., Olerud, H.M. & Lysdahl, K.B. The value of referral information and assessment – a cross sectional study of radiographers’ perceptions. BMC Health Serv Res 22, 893 (2022). https://doi.org/10.1186/s12913-022-08291-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08291-w