Abstract
Background
Vitamin D deficiency is a known morbidity among pregnant women. Maternal hypovitaminosis D results in poor fetal transplacental vitamin D accretion and decreased stores in the neonate. This in turn may lead to hypocalcemia in neonates, having presentations from being asymptomatic and tremors to hypocalcemic seizures. There are fewer case reports of hypocalcemic neonatal seizures as a result of maternal vitamin D deficiency.
Case presentation
A term male neonate developed multiple episodes of multifocal seizures on day six of life associated with hypocalcemia. He was also found to have hyperphosphatemia, raised alkaline phosphatase, and elevated parathormone levels with normal serum magnesium and renal function tests. Neonate and maternal serum vitamin D3 levels were also low. A diagnosis of late-onset hypocalcemic seizure secondary to maternal hypovitaminosis D was made and the baby made an uneventful recovery with parenteral calcium and oral vitamin D supplementation. On follow-up with therapy, the baby remained asymptomatic with normal serum calcium, phosphate, and vitamin D3 levels.
Conclusion
Hypovitaminosis D must also be considered as a contributing factor for late-onset hypocalcemic seizure in neonates.
Similar content being viewed by others
Background
Vitamin D deficiency is a global morbidity among pregnant women. [1]. Maternal hypovitaminosis D results in poor fetal transplacental vitamin D accretion and decreased stores in the neonate [2, 3]. Hypocalcemia as a result of hypovitaminosis D in neonates may have varying presentations from asymptomatic, tremors to hypocalcemic seizure manifestations [4]. As per the literature, there are fewer case reports of neonatal hypocalcemia with symptomatic manifestation as a result of maternal vitamin D deficiency. We hereby report a neonate with late-onset hypocalcemic seizure secondary to maternal vitamin D deficiency and made an uneventful recovery. This article will enlighten the readers and will definitely change the approach to the management of such cases in the near future.
Case presentation
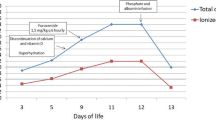
A 6-day-old term male neonate developed multiple episodes of multifocal tonic-clonic convulsions, lasting for 30–50 s. He was the firstborn of non-consanguineous marriage to apparently healthy parents of normal stature. The antenatal period was uneventful without any significant similar family history. The baby was born vigorously by elective cesarean section, weighing 3.84 kg, and was immediately roomed in with the mother. The baby was on exclusive breastfeeds since birth, with normal urine output. The baby was discharged on day four and was feeding well without any such events during home stay till presentation to the hospital. On examination, the baby was irritable and the anterior fontanel was at level. Capillary refill time was normal and there were no facial dysmorphisms or skeletal malformations. Other systemic examinations were normal. Investigations revealed normal blood glucose and low serum calcium 6.7 mg/dL, ionized calcium 0.70 mmol/L (normal levels 1.20–1.38 mmol/L). Blood urea was 13 mg/dL and serum creatinine was 0.4 mg/dL. Cerebrospinal fluid (CSF) analysis, serum protein, and albumin levels were normal with a negative septic screen. Arterial blood gas showed normal pH and bicarbonate, normal serum ammonia level, and negative urine ketones. The baby was started on a parenteral bolus of 10% calcium gluconate at a dose of 2 mL/kg followed by daily maintenance of 8 ml/kg for 72 h. Further investigations revealed elevated serum phosphate of 9.1 mg/dL (normal: 3.8–6.5 mg/dL) and alkaline phosphatase (ALP) of 536 IU/L (normal: 145–420 IU/L). Serum magnesium was 1.8 mg/dL (normal: 1.5–2.5 mg/dL). The thyroid function test was normal. The serum vitamin D3 level was low, (12 ng/mL, normal 30–100 ng/mL) with a mildly elevated parathormone (PTH) level of 78.3 pg/mL (normal: 12–72 pg/mL), at a serum calcium level of 6.7 mg/dL. Maternal serum vitamin D3 level was 6.9 ng/mL. Neonate cranial and abdominal ultrasonography did not reveal any abnormality. With evidence of hypocalcemia, hyperphosphatemia, normal renal function, elevated serum PTH, and low vitamin D3 levels, a diagnosis of late-onset hypocalcemic seizure secondary to maternal hypovitaminosis D was made. The baby was started thereafter on daily oral calcium supplementation at a dose of 50 mg/kg/day and cholecalciferol 2000 IU/day. Baby responded with the above medications. The baby had a good prognostic outcome. Serum calcium normalized and phosphorus level started decreasing after 1 week of therapy. On follow-up at 6 months, the baby was asymptomatic with normal serum calcium, phosphate, and alkaline phosphatase levels, with normal neurodevelopmental outcomes. The baby was continued on oral cholecalciferol (400 IU/day) and calcium supplements thereafter.
Discussion
Maternal vitamin D deficiency during pregnancy and lactation is a significant risk factor for rickets in infancy [1,2,3]. However, neonatal hypocalcemic seizure as a consequence of maternal vitamin D deficiency is not reported much in the literature. Vitamin D insufficiency in healthy pregnant women is not uncommon [5]. Newborn babies of such mothers have reduced vitamin D stores [6]. In addition, the breast milk of such mothers is also vitamin D deficient [7]. Neonates born to mothers with vitamin D deficiency or insufficiency may also develop vitamin D deficiency and late-onset hypocalcemia manifestation [8, 9]. Exclusive breastfeeding without vitamin D supplementation is another risk factor for vitamin D deficiency in neonates and infants. Late-onset hypocalcemia may also be caused by high phosphate intake like cow’s milk. However, there was no such association in our case [10]. Late-onset hypocalcemia caused by excessive phosphate load is usually accompanied by raised PTH and ALP levels [9]. Our case illustrates the importance of looking for vitamin D status in neonates presenting with seizures and hypocalcemia, as this is easily treatable. It is also debatable whether maternal vitamin D supplementation can prevent such a condition, however, there is a paucity of data regarding this. In our case, we ruled out the common causes of late-onset neonatal hypocalcemia (increased oral phosphate load, hypomagnesemia, renal insufficiency, hypoparathyroidism, metabolic alkalosis, and phototherapy) [11]. Our baby had no history of prematurity, maternal diabetes, perinatal asphyxia and sepsis, neonatal jaundice requiring phototherapy or artificial formula, or cow’s milk intake. The baby also did not have facial dysmorphism. Transient hypoparathyroidism may also present with hypocalcemia and hyperphosphatemia, but our baby had an elevated PTH level.
Conclusions
In a case of a neonate presenting with late-onset hypocalcemic seizure, maternal as well as neonatal hypovitaminosis D should also be considered apart from other common risk factors.
Availability of data and materials
Not applicable.
Abbreviations
- CSF:
-
Cerebro spinal fluid
- ALP:
-
Alkaline phosphatase
- PTH:
-
Parathormone
References
Balasubramanian S (2011) Vitamin D deficiency in breastfed infants and the need for routine vitamin D supplementation. Indian J Medic Res 133(3):250–252
Craig M, Zacharin MR, Rodda CP, Batch JA, Morley R, Cranswick NE et al (2006) Prevention and treatment of infant and childhood vitamin D deficiency in Australia and New Zealand: a consensus statement. Med J Australia 85(5):268–272
Camadoo L, Tibbott R, Isaza F (2007) Maternal vitamin D deficiency associated with neonatal hypocalcaemic convulsions. Nutrit J 6:23
Thomas TC, Smith JM, White PC, Adhikari S (2012) Transient neonatal hypocalcemia: presentation and outcomes. Pediatrics 129:1461–1467
Khalessi N, Kalani M, Araghi M, Farahani Z (2015) The Relationship between maternal Vitamin D deficiency and low birth weight neonates. J Fam Reprod Health 9(3):113–117
Karras SN, Fakhoury H, Muscogiuri G (2016) Maternal vitamin D levels during pregnancy and neonatal health: evidence to date and clinical implications. Therapeu Adv Musculoskeletal Dis 8(4):124–135
Khalesi N, Bahaeddini SM, Shariat M (2012) Prevalence of maternal vitamin D deficiency in neonates with delayed hypocalcaemia. Acta Med Iran 50(11):740–745
Collins M, Young M (2017) Benign neonatal shudders, shivers, jitteriness, or tremors: early signs of vitamin D Deficiency. Pediatrics 140(2):e20160719
Kim HS (2007) Calcium and phosphate metabolism and disorders in the newborn. Korean J Pediatr 50:230–235
Jain A, Agarwal R, Sankar MJ, Deorari A, Paul VK (2010) Hypocalcemia in the newborn. Indian J Pediatr 77:1123–1128
Agarwal R, Deorari A, Paul VK (2019) AIIMS Protocols in Neonatology, 2nd edn. Noble Vision (Medical Book Publishers), Delhi.
Acknowledgements
We acknowledge the support of the parent for consenting. We also acknowledge all our nursing and paramedical staffs in patient care, and our family for their unconditional support.
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
AKM and RKY conceptualized and drafted the initial manuscript and reviewed and revised the manuscript. KS revised and finalized the editing of the manuscript. NMB critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Verbal and written informed consents were given by the patient’s parents for the publication of this case.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mallick, A.K., Yadav, R.K., Sannalli, K. et al. Maternal hypovitaminosis D presenting as late-onset hypocalcemic seizure in a term neonate: a case report. Egypt Pediatric Association Gaz 71, 15 (2023). https://doi.org/10.1186/s43054-023-00164-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-023-00164-z