Abstract
Background
Uric acid plays a pivotal role in the regulation of mood and behavior. The study aimed to elucidate the role of serum uric acid as a biomarker in patients with schizophrenia, bipolar affective disorder (BAD), and major depressive disorder (MDD) and to examine its relation to symptom domains and severity of illness.
Results
A total of 150 participants with schizophrenia, BAD, and MDD and 50 healthy controls were recruited. Patients were assessed using Structured Clinical Interview for DSM-IV Axis I Diagnosis (SCID-I), Positive and Negative Syndrome Scale (PANSS), the Young Mania Rating Scale (YMRS), and the Hamilton Depression Rating Scale (HAM-D). General Health Questionnaire (GHQ-28) was applied to healthy controls. Then, a blood draw from all participants was performed to measure serum uric acid level. According to this study, there was a statistically significant difference between patients with schizophrenia, BAD, MDD, and healthy controls, with regard to serum uric acid level (P = 0.007). On correlating symptom domains and severity of schizophrenia, bipolar, and MDD with serum uric acid level, there was only a statistically significant negative correlation between YMRS and serum uric acid level (P = 0.022).
Conclusions
Serum uric acid could be a valuable biomarker in patients with schizophrenia, bipolar, and MDD especially in patients with bipolar disorder.
Similar content being viewed by others
Background
The purinergic system is related to the adenine nucleotides (ATP, ADP, & AMP), the nucleoside adenosine, guanine nucleotides (GTP & GDP), and the nucleoside guanosine [1]. Adenosine, a purine ribonucleoside, is considered a neurobiological substrate that has a great influence on signaling cascade, synaptic transmission, various neurotransmitter pathways, and regulation of brain immune responses. It acts as a neuroprotective agent with anti-inflammatory properties [2].
Uric acid constitutes the end product of purine catabolism. It is formed primarily in the liver and excreted by the kidney into the urine [3]. Research work provided evidence for the link between serum uric acid level and a wide variety of psychological consequences such as mood, aggression, and anxiety [4,5,6].
The link between purinergic pathway and bipolar disorder could be attributed to the genetic alteration in adenosine (A1 & A2) receptor function and/or level of expression, with the resultant accelerated purinergic transformation and decreased adenosinergic transmission, leading to dysfunctional neurotransmitters’ pathways related to manic behavior [7, 8]. Studies linking serum uric acid level to bipolar disorder found that serum uric acid level was correlated with impulsivity, psychomotor agitation, irritated mood, and hyperthymic temperament. On the contrary, serum uric acid level was linked to depressed mood independently of the disorder phase, suggesting that serum uric acid could be a useful biomarker to differentiate bipolar disorder from major depressive disorder [9, 10].
The link between purinergic pathway and major depressive disorder could be attributed to the P2rx7 receptor-mediated excessive glutamate release and subsequent activation of extra-synaptic NMDA receptors and subsequently change in the level of neurotrophic factors [11]. Studies assessing serum uric acid level in patients with major depression revealed lower levels in depressed patients compared to healthy controls [12]. Meanwhile, serum uric acid level increased after treatment with antidepressants [13].
The link between purinergic pathway and schizophrenia could be attributed to the stimulation of nucleotide receptors which provide a pro-dopaminergic and anti-glutamatergic effects [14]. Studies examining serum uric acid level in patients with schizophrenia revealed conflicting results. Earlier studies demonstrated reduced serum uric acid level in chronic, as well as first-episode neuroleptic-naive patients [15]. Recent studies found an increase in the concentration of uric acid during acute phase of the illness. Hence, it could play a role in the development or progression of schizophrenia [14, 16].
The present study uses a series of established psychometric clinical tests and measures serum uric acid level as a biochemical marker to elucidate the role of serum uric acid level as a biomarker in patients with schizophrenia, BAD, and MDD and to examine its relation to symptom domains and severity of illness.
This study was based on the hypothesis that serum uric acid level would be high in patients diagnosed with bipolar disorder and low in patients diagnosed with MDD and schizophrenia compared to healthy controls, and it was hypothesized that serum uric acid level would correlate significantly with symptom domains and severity of schizophrenia, BAD, and MDD. Thus, serum uric acid level could open a new field as a diagnostic and prognostic method in patients with schizophrenia, BAD, and MDD.
Methods
Participants and procedure
A total of 200 participants were recruited from the Okasha Institute of Psychiatry, Ain Shams University Hospitals. Using a PASS II program, a sample size of 50 patients with major depressive disorder, 50 patients with bipolar disorder, 50 patients with schizophrenia, and 50 healthy controls were allocated into 4 equal groups whose means had to be compared. The total sample of 200 participants achieved 90% power to detect differences among the means versus the alternative of equal means using an F-test with a 0.05000 significance level. The size of the variation in the means was represented by their standard deviation = 0.93. The common standard deviation within a group is assumed to be 1.00.
The diagnosis of major depressive disorder, bipolar disorder, and schizophrenia was made according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) [17]. Subsequently, patients had a series of clinical, psychological tests, and biochemical assessment in a fixed order.
Male and female patients with schizophrenia, BAD, and MDD, with age ranged 18–65, from the inpatient wards or outpatient clinics were included in the current study after giving informed consent, while patients with coexisting neuropsychiatric disorders, having any disorder that clearly interferes with serum uric acid level, such as gout, chronic inflammatory disease, diabetes, renal failure, or serum creatinine value ≥ 41.5 mg/dl, were excluded.
Patients with schizophrenia, bipolar, and MDD were receiving their prescribed psychotropic medications whether typical or atypical antipsychotic, anti-Parkinson, mood stabilizer, or antidepressant according to their diagnosis.
Healthy controls were recruited from the staff working at Okasha Institute of Psychiatry, Ain Shams University Hospital. They were demographically matched to patients with schizophrenia, BAD, and MDD. General Health Questionnaire (GHQ-28) was applied to exclude any mental illness.
Psychometric assessment of the patient group
Clinical assessment
Patients were interviewed, and demographic characteristics were collected in a designed Okasha Institute psychiatric sheet. Then, the psychometric clinical tests were conducted by the researcher.
Structured Clinical Interview for DSM-IV axis I diagnosis (SCID-I) [17]: Arabic version [18]
The scale was designed to be simpler and more efficient, compared to other existing tools and, consequently, to take less time in administration. It is based on semi-structured interview and administered through the clinician, for use in psychiatric patients. It allows a wide coverage of psychiatric disorders according to DSM-IV and consists of nine diagnostic categories (mood episode, mood disorder differential, psychotic symptom, psychotic disorder differential, adjustment disorder, somatoform disorder, anxiety, eating disorder, and substance use).
The Positive and Negative Syndrome Scale (PANSS) [19]: Arabic version [20]
The scale was intended to assess schizophrenia symptom domains: positive, negative, and general psychopathology. The PANSS is based on a standardized, clinical interview that determines the presence and severity of schizophrenia symptom domains within the past week. The scale consists of 30 items: seven items covering positive symptoms, seven items covering negative symptoms, and 16 items covering general psychopathology symptoms. Symptom severity could be determined according to the 7-point scale (1 = absent; 7 = extreme). The test has high inter-rater reliability (0.80) and demonstrates excellent criterion-related validity and constructs validity.
The Young Mania Rating Scale (YMRS) [21]
The scale was intended to assess manic symptoms. It is based on both patient’s subjective report of his/her clinical condition and the clinical observations taken during the clinical interview. The scale consists of 11 items; four items are graded on a 0 to 8 scale (irritability, speech, thought content, and disruptive/aggressive behavior), while the remaining seven items are graded on a 0 to 4 scale. The variation in grading the items, with the four items given twice the weight of the others, was to compensate for poor cooperation from severely manic patients.
The hamilton depression rating scale (HAM-D) [22]: Arabic version [23]
The scale was intended to assess depression. It is clinician administered. The scale consists of 17 items (HDRS17), corresponding to depression symptom dimensions experienced over the past week. The scale does not cover the atypical symptoms of depression (e.g., hypersomnia, hyperphagia). In interpretation of results, a score from 0–7 is generally accepted to be within the normal range (or in the clinical remission stage), while a score of ≥ 20 indicates at least moderate severity.
Psychometric assessment of the control group
General health questionnaire (GHQ-28) [24]
The GHQ was intended to detect any psychiatric disorder among the general population and within community or nonpsychiatric clinical settings such as primary care or general medical outpatients. It detects the difference between the respondent’s current state and if that differs from his/her usual state. Therefore, it is sensitive to short-term psychiatric disorders.
Biochemical assessment for the patient and control group
A blood draw to measure serum uric acid was performed on the same day of hospital admission (for inpatients) or on the day of clinic visit (for outpatients). Then, blood samples were centrifuged at 4000 rpm for 15 min and stored at − 80 °C. After that, the samples were examined using a STAT fax stand-alone chemistry analyzer. The serum uric acid level has a lower threshold set, ranging from 2 to 4 mg/dL. The upper threshold is 6 mg/dL for women and 7 mg/dL for men. Hyperuricemia is defined as serum uric acid concentrations > 6 mg/dL for females and 7 mg/dL for men [25], while hypouricemia is defined as serum uric acid concentrations below the normal range [26].
Ethical consideration
Agreement for this research was obtained from the authority of Ain Shams University, Ethical and Research Committee, and an informed oral and written consent were obtained from all participants enrolled in the current research, after a very clear explanation, providing information about the purpose of the study.
Statistical analysis
The collected data were revised, coded, tabulated, and introduced to a PC using Statistical Package for Social Science (SPSS 20). Data were presented, and suitable analysis was done, according to the type of the data obtained for each parameter. Regarding descriptive statistics, the researcher used the following: (1) mean, standard deviation (± SD), and range for numerical data and (2) frequency and percentage for nonnumerical data. Concerning analytical statistics, the researcher used the following: (1) Student T-Test to assess the statistical significance of the difference between two study groups means; (2) chi-square test was to examine the relationship between two qualitative variables; (3) one-way ANOVA test to compare between more than two groups, with quantitative data and parametric distribution; (4) ANOVA test to control for the confounding factors; and (5) correlation analysis (Pearson’s method) to assess the strength of association between two quantitative variables. The correlation coefficient denoted symbolically “r” defines the strength (magnitude) and direction (positive or negative) of the linear relationship between two variables. In interpretation of results, r = 0–0.19 was regarded as a very weak correlation, while r = 0.8–1 was regarded as a very strong correlation. P-value was used to indicate level significance: P > 0.05 = non-significant, while P < 0.05 = significant.
Results
Sociodemographic characteristics of participants
Comparing patients with schizophrenia, bipolar, and MDD and control group with regard to sociodemographic data, there was a highly statistically significant difference between the patient group and control group regarding education, occupation, and marital status (P < 0.001). Meanwhile, there was a statistically significant difference between the patient group and control group in gender (P = 0.003). There was no statistically significant difference between the patient group and control group with regard to age (P > 0.05) and residency (P = 0.312) (Table 1).
Clinical characteristics of the sample:
-
a) On assessing patients with bipolar disorder using Young Mania Rating Score (YMRS), most patients scored moderate to severe degree (76% & 24%, respectively) with YMRS range from 26 to 45 (33.2., 33.200 ± 5.35) (Table 2).
-
b) Using HAM-D scale to assess the severity of depression, the vast majority of patients scored severe degree (20, 40%), followed by the very severe degree (17, 34%), while only 6 patients (12%) had moderate severity (Table 2).
-
b) Using HAM-D scale to assess the severity of depression, the vast majority of patients scored severe degree (20, 40%), followed by the very severe degree (17, 34%), while only 6 patients (12%) had moderate severity (Table 2).
-
c) With regard to PANSS, patients with schizophrenia scored 22.24 ± 6.93 in the positive symptom domain, 23.300 ± 10.95 in the negative symptom domain, and 31.98 ± 12.38 in the general psychopathology domain (Table 2).
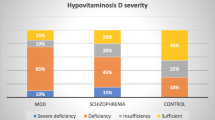
The relationship between serum uric acid levels in patients with schizophrenia, bipolar, MDD, and healthy controls
Regarding serum uric acid level, there was a statistically significant difference between patients with schizophrenia, bipolar, MDD, and healthy controls (P = 0.007); patients with schizophrenia had the highest level (range from 2.9 to 10.9 mg/dl, 6.226 ± 2.050). Meanwhile, patients with MDD had the lowest values (range from 1.6 to 8.3 mg/dl, 4.960 ± 1.714) (Table 3).
On performing Tukey’s test to determine the statistically significant relationship between each two sets (patients with bipolar disorder and control group), patients with MDD and control, patients with schizophrenia and control, patients with bipolar disorder and MDD, patients with bipolar disorder and schizophrenia, and patients with schizophrenia and MDD), there was only a statistically significant difference between patients with schizophrenia and MDD (P = 0.004) (Table 3).
Correlation of symptom domains and severity of schizophrenia, bipolar, and MDD with serum uric acid level
On correlating serum uric acid level with symptom domains and severity of schizophrenia, bipolar, and MDD, there was only a statistically significant negative correlation between YMRS and serum uric acid level (P = 0.022) (Table 4).
Discussion
Research work had recently focused on blood‐based biomarkers that could be an easy, cheep, accessible, and a valuable tool in diagnosing psychiatric disorders [8].
To our knowledge, this is the first study to examine the potential role of serum uric acid as a biochemical marker in patients with schizophrenia, bipolar, and MDD compared to healthy controls in one research.
The primary goal of the study was to explore the relationship between serum uric acid level among patients with schizophrenia, bipolar, and MDD compared to healthy controls.
Serum uric acid level in patients with schizophrenia, bipolar, and MDD compared to healthy controls
Patients with schizophrenia had the highest level of uric acid level (mean = 6.2 mg/dl), followed by patients with bipolar disorder (mean = 5.8 mg/dl) and then the control group (mean = 5.6 mg/dl). Meanwhile, patients with MDD had the lowest values (mean = 4.9 mg/d) (f = 4.210; P = 0.007).
-
a)
Bipolar disorder
In the current study, patients with bipolar disorder had higher serum uric acid levels compared to healthy controls, yet it was statistically non-significant (P = 0.952). Studies carried out on patients with bipolar disorder during both acute and chronic phases revealed that serum uric acid was significantly higher in patients with bipolar disorder compared to healthy controls [27,28,29,30]. Indeed, comparing the serum UA levels in patients suffering from bipolar disorder during manic phase, depression, and remission phases, the serum UA levels were significantly higher during manic phase [31,32,33]. Therefore, we support that increased UA levels were associated with a state of manic episode, which may be used as a routine check in the manic phase in bipolar disorder [34].
-
b)
Major depressive disorder
In the current study, patients with MDD had lower serum uric acid levels, compared to healthy controls, yet it was statistically non-significant (P = 0.215). Black et al. [35] tested 2875 participants; 609 had remitted MDD and/or anxiety disorder(s); 1648 had current MDD and/or anxiety disorders, and 618 healthy controls; and the authors found a statistically significant lower serum uric acid in subjects with current MDD and/or anxiety disorders, compared to healthy controls (P < 0.001). In contrast to the previous findings, Tao et al. [36] recruited inpatient adolescent males with depression and found a statistically significant higher serum uric acid compared to control group (t = 8.92, P < 0.001). This could be due to the age criteria of this study, whereas adolescent males tend to have higher metabolic rates.
-
iii)
Schizophrenia
In the current study, patients with schizophrenia had higher serum uric acid levels, compared to healthy controls, yet it was statistically non-significant (P = 0.434). Gültekin et al. [37] found that serum uric acid in male patients with schizophrenia was significantly higher compared to healthy controls. In contrast to our finding, Yao et al. [15] found that plasma uric acid levels were significantly lower in patients with schizophrenia compared to healthy controls. Indeed, Reddy et al. [38] studied first-episode neuroleptic naïve-patients with schizophrenia and found that patients with first-episode schizophrenia had significantly lower uric acid as compared to healthy controls.
The role of serum uric acid among patients with schizophrenia, BAD, and MDD
In the current study, there was a statistically significant difference between patients with schizophrenia, bipolar, MDD, and healthy controls, regarding serum uric acid level (P = 0.007). Patients with schizophrenia had the highest level (range from 2.9 to 10.9 mg/dl, 6.226 ± 2.050), followed by patients with bipolar disorder (range from 2.4 to 9.3 mg/dl, 4.960 ± 1.714), and then, patients with MDD had the lowest values (range from 1.6 to 8.3 mg/dl, ±). On performing Tukey’s test to determine the statistically significant relationship between each two sets of the 4 groups, there was only a statistically significant difference between patients with schizophrenia and MDD (P = 0.004).
In contrast to our finding, Gültekin et al. [37] compared serum uric acid levels between 59 patients with schizophrenia and 55 patients with bipolar disorder; serum uric acid levels were higher in patients with bipolar disorder than those with schizophrenia, yet with no statistically significant difference between them (P = 0.108). Indeed, Malewska et al. [39] concluded that serum uric acid concentration did not differ between patients with schizophrenia and patients with bipolar disorder.
The findings of Bartoli et al. [40] were not consistent with our finding; the authors recruited 128 subjects with bipolar disorder and 118 with MDD; patients with bipolar mania were found to have statistically significant higher levels of serum uric acid (5.27 ± 1.63 mg/dl) when compared with MDD (4.59 ± 1.62 mg/dl) (P < 0.05). In a retrospective study done to asses MDD patients’ liability for bipolarity, it was found that depressed patients with higher levels of serum UA are at greater risk of experiencing a manic or hypomanic episode (t = 9.72, P < 0.001), and serum UA levels actually demonstrated a very good‐to‐excellent prognostic accuracy as a biomarker for conversion to BD in depressed subjects [8]. The differences in study design, diagnostic methodology, or sample characteristics are possible explanations for the apparent discrepant findings.
Correlation of serum uric acid level with symptom domains and severity of schizophrenia, bipolar, and MDD
In the current study, the authors found a significant negative correlation between YMRS and serum uric acid (P = 0.022). In contrast to our finding, the study of Marchado-Vieira et al. [27] found no correlation between uric acid levels and YMRS scores in patients with bipolar disorder. Indeed, in the study of Salvadore et al. [29] done on patients with first-episode mania, serum uric acid levels were not found to be correlated with episode severity. Gültekin et al. [37] followed up serum uric acid weekly in correlation with YMRS, among patients in the manic phase. The authors found a correlation between the reduction in the uric acid levels measured at the baseline and after the end of the first week and the reduction in YMRS scores. This could be due to the fact that 75% of our sample of patients with bipolar disorder had moderate symptom severity, while only 25% had severe symptom severity, and none had mild symptom severity.
With regard to patients with schizophrenia, the current study did not find any correlation between positive symptoms score, negative symptoms score, nor general psychopathology score and serum uric acid levels. In agreement with our finding, Malewska-Kasprzak et al. [14] correlated serum uric acid with different phases of schizophrenia; the authors found no difference in uric acid concentration among patients with schizophrenia during acute and remission phases of the illness.
The current study found no significant correlation between the Hamilton Depression Scale value and serum uric acid level. In agreement with our finding, in the study of Wen et al. [12], the authors did not find any statistically significant difference between serum uric acid in patients with MDD with scores > 35 and patients with scores < 35 (P = 0.392).
Possible limitations in the current study include the following: first, patients were recruited from Okasha Institute of Psychiatry, a tertiary healthcare center; so, most patients had moderate to severe symptom severity. Second, the study did not take into consideration the duration of illness and previous and current managements. Third, the exclusion criteria were only met by history taking; no further investigations were done to detect any undiagnosed illness.
Conclusions
In conclusion, the current study found that patients with schizophrenia, bipolar, and MDD had a statistically significant difference in serum uric acid levels compared to healthy controls; patients with schizophrenia had the highest level, while patients with MDD had the lowest values. Indeed, serum uric acid levels were statistically negatively correlated with YMRS. Thus, uric acid as the end product of the purinergic pathway does not reflect the dysfunction in each disease, as it is not simply a dysfunction in substrates of the pathway, but also receptors, which are not reflected by uric acid as metabolite.
The authors recommend that future research on this topic should recruit larger sample size from multiple centers for better generalize the results. Indeed, control of the risk factors for hyperuricemia should be carried out through screening tests for metabolic syndrome, e.g., HBA1c and lipid profile. Further research measuring adenosine, or adenosine receptors marker, might be more specific to the purinergic dysfunction.
Availability of data and materials
The datasets used during the current study are available from the corresponding author upon request.
Abbreviations
- SCID-I:
-
Structured clinical interview for DSM-IV axis I diagnosis
- PANSS:
-
Positive and negative syndrome scale
- YMRS:
-
Young mania rating scale
- HAM-D:
-
Hamilton depression rating scale
- GHQ-28:
-
General health questionnaire
- DSM-IV:
-
Diagnostic and statistical manual of mental disorders, 4th edition
- MDD:
-
Major depressive disorder
- BAD:
-
Bipolar affective disorder
- ATP, ADP, AMP:
-
adenine nucleotides
- GTP, GDP:
-
guanine nucleotides
References
Lara DR, Souza DO (2000) Schizophrenia : a purinergic hypothesis. Med Hypotheses 54:157–166. https://doi.org/10.1054/mehy.1999.0003
Sasidharan A, Kumar S, John JP, Philip M, Subramanian S, Jain S, Kutty BM (2017) Elevated serum adenosine deaminase levels in neuroleptic-naïve patients with recent-onset schizophrenia. Asian J Psychiatr 29:13–15. https://doi.org/10.1016/j.ajp.2017.03.034
Maiuolo J, Oppedisano F, Gratteri S, Muscoli C, Mollace V (2016) Regulation of uric acid metabolism and excretion. Int J Cardiol 213:8–14. https://doi.org/10.1016/j.ijcard.2015.08.109
Morelli M, Carta AR, Kachroo A, Schwarzschild MA (2010) Pathophysiological roles for purines: adenosine, caffeine and urate. Prog Brain Res 183:183–208. https://doi.org/10.1016/S0079-6123(10)83010-9
Cieślak M, Czarnecka J, Roszek K (2016) The roles of purinergic signaling in psychiatric disorders Acta Biochim. Pol 63:1–9. https://doi.org/10.18388/abp.2015_1004
Bartoli F, Crocamo C, Bava M, Castagna G, Di Brita C, Riboldi I, Trotta G, Verrengia E, Clerici M, Carrà G (2018) Testing the association of serum uric acid levels with behavioral and clinical characteristics in subjects with major affective disorders: a cross-sectional study. Psychiatry Res 269:118–123. https://doi.org/10.1016/j.psychres.2018.08.039
Deckert J, Nöthen MM, Albus M, Franzek E, Rietschel M, Ren H, Stiles GL, Knapp M, Weigelt B, Maier W, Beckmann H, Propping P (1998) Adenosine A1 receptor and bipolar affective disorder: systematic screening of the gene and association studies. Am J Med Genet 81:18–23. https://doi.org/10.1002/(sici)1096-8628(19980207)81:1%3c18::aid-ajmg4%3e3.0.co;2-j
Dos Santos Oliveira PM, Santos V, Coroa M, Ribeiro J, Madeira N (2019) Serum uric acid as a predictor of bipolarity in individuals with a major depressive episode. Bipolar Disord 21:235–243. https://doi.org/10.1111/bdi.12708
Cheffer A, Castillo AR, Gonçalves MC, Naaldijk Y, Nascimento IC, Burnstock G, Ulrich H (2018) Purinergic system in psychiatric diseases. Mol Psychiatry 23:94–106. https://doi.org/10.1038/mp.2017.188
Chatterjee SS, Ghosal S, Mitra S, Mallik N, Ghosal MK (2018) Serum uric acid levels in first episode mania, effect on clinical presentation and treatment response: data from a case control study. Asian J Psychiatr 35:15–17. https://doi.org/10.1016/j.ajp.2018.04.030
Sperlagh B, Csolle C, Ando RD, Goloncser F, Kittel A, Baranyi M (2012) The role of purinergic signaling in depressive disorders. Neuropsychopharmacol Hung 14:231–238 (PMID: 23269209)
Wen S, Cheng M, Wang H, Yue J, Wang H, Li G, Zheng L, Zhong Z, Peng F (2012) Serum uric acid levels and the clinical characteristics of depression. Clin Biochem 45:49–53. https://doi.org/10.1016/j.clinbiochem.2011.10.010
Chaudhari K, Khanzode S, Khanzode S, Dakhale G, Saoji A, Sarode S (2010) Clinical correlation of alteration of endogenous antioxidant-uric acid level in major depressive disorder. Indian J Clin Biochem 25:77–81. https://doi.org/10.1007/s12291-010-0016-z
Malewska-Kasprzak MK, Permoda-Osip A, Rybakowski JK (2019) Disturbances of purinergic system in affective disorders and schizophrenia. Psychiatr Pol 3:577–587. https://doi.org/10.12740/PP/97335
Yao JK, Reddy R, Van Kammen DP (1998) Reduced level of plasma antioxidant uric acid in schizophrenia. Psychiatry Res 80:29–39. https://doi.org/10.1016/s0165-1781(98)00051-1
Yao JK, Condray R, Dougherty GGD, Keshavan MS, Montrose DM, Matson WR, McEvoy J, Kaddurah-Daouk R, Reddy RD (2012) Associations between purine metabolites and clinical symptoms in schizophrenia. PLoS One 7(8):e42165. https://doi.org/10.1371/journal.pone.0042165
First MB, Spitzer RL, gibbon M, Williams JB (1995) Structured clinical interview for DSM-IV Axis I Disorders (SCID-I), Handbook of Psychiatric Measures, Washington, American Psychiatric Association.
El Missiry A, Sorour A, Sadek A, Fahy T, Abdel Mawgoud MAT (2003) Homicide and psychiatric illness: an Egyptian study. Faculty of Medicine, Ain Shams University, Cairo
Kay SR, Fiszbein A, Opler LA (1987) The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276. https://doi.org/10.1093/schbul/13.2.261
Okasha A, Sadek A, Seif Al Dawla A, Okasha T, Sayed M, Youssef A (2005) Outcome of schizophrenia: a ten-year study of a sample of Egyptian patients. Egypt J Psych 24:21–32
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133:429–435. https://doi.org/10.1192/bjp.133.5.429
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62. https://doi.org/10.1136/jnnp.23.1.56
Alhadi AN, Alarabi MA, Alshomrani AT, Shuqdar RM, Alsuwaidan MT, Mcintyre RS (2018) Arabic translation, validation and cultural adaptation of the 7-item Hamilton Depression Rating Scale in two community samples. Sultan Qaboos Univ Med J 18:167–172. https://doi.org/10.18295/squmj.2018.18.02.008
Goldberg DP, Hillier VF (1979) A scaled version of the General Health Questionnaire. Psychol Med 9:139–145. https://doi.org/10.1017/s0033291700021644. (PMID: 424481)
Chizyński K, Rózycka M (2005) Hyperuricemia. Pol Merkur. Merkur Lekarski 19:693–696 (PMID 16498814)
Gois PHF, Souza ERM (2020) Pharmacotherapy for hyperuricaemia in hypertensive patients. Cochrane Database Syst Rev 2:9. https://doi.org/10.1002/14651858.CD008652.pub4
Machado-Vieira R, Soares JC, Lara DR, Luckenbaugh DA, Busnello JV, Marca G (2008) A double-blind, randomized, placebo-controlled 4-week study on the efficacy and safety of the purinergic agents allopurinol and dipyridamole adjunctive to lithium in acute bipolar mania. J Clin Psychiatry 69:1237–1245. https://doi.org/10.4088/JCP.v69n0806
De Berardis D, Conti CM, Campanella D, Carano A, Di Giuseppe B, Valchera A (2008) Evaluation of plasma antioxidant levels during different phases of illness in adult patients with bipolar disorder. J Biol Regul Homeost Agents 22:195–200 (PMID: 18842173)
Salvadore G, Viale CI, Luckenbaugh DA, Zanatto VC, Portela LV, Souza DO, Zarate CA, Machado-Vieira R (2010) Increased uric acid levels in drug-naïve subjects with bipolar disorder during a first manic episode. Prog Neuropsychopharmacol Biol Psychiatry 34:819–821. https://doi.org/10.1016/j.pnpbp.2010.02.027
Albert U, De Cori D, Aguglia A, Barbaro F, Bogetto F, Maina G (2015) Increased uric acid levels in bipolar disorder subjects during different phases of illness. J Affect Disord 173:170–175. https://doi.org/10.1016/j.jad.2014.11.005
Kesebir S, TatlidilYaylaci E, Süner Ö, Gültekin BK (2014) Uric acid levels may be a biological marker for the differentiation of unipolar and bipolar disorder: the role of affective temperament. J Affect Disord 165:131–134. https://doi.org/10.1016/j.jad.2014.04.053
Bartoli F, Crocamo C, Maria G, Castagna G, Trotta G, Clerici M, Carrà G (2016) Exploring the association between bipolar disorder and uric acid : a mediation analysis. J Psychosom Res 84:56–59. https://doi.org/10.1016/j.jpsychores.2016.03.014
De Berardis D, Conti CM, Campanella D, Carano A, Di Giuseppe B, Valchera A (2014) Serum uric acid levels and different phases of illness in bipolar I patients treated with lithium. Psychiatry Res 225:604–608. https://doi.org/10.1016/j.psychres.2014.11.038
Machado-Vieira R (2012) Purinergic system in the treatment of bipolar disorder: uric acid levels as a screening test in mania. J Clin Psychopharmacol 32:735–736. https://doi.org/10.1097/JCP.0b013e318268391d
Black CN, Bot M, Scheffer PG, Snieder H, Penninx BWJ (2018) Uric acid in major depressive and anxiety disorders. J Affect Disord 225:684–690. https://doi.org/10.1016/j.jad.2017.09.003
Tao R, Li H (2015) High serum uric acid level in adolescent depressive patients. J Affect Disord 174:464–466. https://doi.org/10.1016/j.jad.2014.12.031
Gültekin BK, Kesebir S, Kabak SG, Ergün FF, TatlidilYaylaci E (2014) Are uric acid levels different from healthy subjects in bipolar affective disorder and schizophrenia?: Relationship between clinical improvement and episode severity in male patients. Noro Psikiyatr Ars 51:229–232. https://doi.org/10.4274/npa.y6827
Reddy R, Keshavan M, Yao JK (2003) Reduced plasma antioxidants in first-episode patients with schizophrenia. Schizophr Res 62:205–212. https://doi.org/10.1016/s0920-9964(02)00407-3
Malewska M, Rybakowski F, Rybakowski JK (2017) A study of uric acid concentration in bipolar disorder and schizophrenia. Eur Neuropsychopharmacol 27:755–756. https://doi.org/10.1016/S0924-977X(17)31383-4
Bartoli F, Crocamo C, Dakanalis A, Brosio E, Miotto A, Capuzzi E, Clerici M, Carrà G (2017) Purinergic system dysfunctions in subjects with bipolar disorder: a comparative cross-sectional study. Compr Psychiatry 73:1–6. https://doi.org/10.1016/j.comppsych.2016.09.011
Acknowledgements
The authors are thankful to the participants for their participation in the current study.
Funding
No funding source was used in the current paper.
Author information
Authors and Affiliations
Contributions
Conception and design of the study were done by NS, DE, and MH. Acquisition of data was done by RM and MH, analysis and/or interpretation of data was done by NS and DE, drafting the manuscript was done by MH, revising the manuscript critically for important intellectual content was done by NS and DE, and approval of the version of the manuscript to be published was done by NS. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shaker, N.M., Serafi, D.e., Mahfouz, R.H.E.LD. et al. Exploring the role of serum uric acid as a biomarker in patients with schizophrenia, bipolar affective disorder, and major depressive disorder. Middle East Curr Psychiatry 30, 31 (2023). https://doi.org/10.1186/s43045-023-00307-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00307-3