Abstract
Background
Male infertility is a major health problem with multi-factorial etiology. Intracytoplasmic sperm injection (ICSI) has revolutionized the treatment of men with severely compromised semen parameters and improved their chances of achieving pregnancy. However, many concerns have been raised about ICSI safety; in part owing to utilizing aneuploid sperms from infertile men, which may be associated with an increased incidence of chromosomal aneuploidies in ICSI pregnancies. The aim of the study was to determine the incidence of sperm aneuploidies for chromosomes 13, 18, 21, X, and Y in semen of infertile males with failed ICSI. This will assist infertile couples and enable them to make informed decisions. For this purpose, sperm aneuploidy frequency for chromosomes 13, 18, 21, X, and Y was evaluated by multicolor fluorescence in-situ hybridization (FISH) in 35 patients with abnormal semen parameters, and 10 normozoospermic healthy men who served as controls.
Results
Sperm aneuploidies for chromosomes 13, 18, 21, X, and Y in semen from infertile men with failed ICSI were detected at higher frequencies than controls. Patients had significantly higher disomy, nullisomy, diploidy, and polyploidy frequencies compared to controls.
Conclusions
Infertile men with failed ICSI have a significantly increased frequency of sperm chromosome abnormalities compared to controls. Fluorescence in situ hybridization facilitated the study of numerical chromosomal abnormalities in human sperm nuclei (sperm FISH). Sperm FISH, prior to the application of assisted reproductive techniques, saves a considerable amount of time and resources.
Similar content being viewed by others
Background
Infertility is a major health problem with multi-factorial etiology that affects approximately 14–22% of couples in reproductive age worldwide [1, 2]. In Egypt, the total infertility prevalence rate is 12% [1], with male factor infertility ranging between 13 and 46% of infertile couples presenting to assisted reproduction technology (ART) clinics, where the male factor was the sole cause of infertility in 13% of cases, and in 46% of cases male factor was involved [3].
Male factor infertility refers to a male's inability to induce pregnancy in a fertile female. Male infertility is heterogeneous, commonly due to deficiencies in the semen, and/or sperm parameters. Abnormal sperm parameters can be manifested by either aspermia (complete lack of semen with ejaculation) or hypospermia (decreased semen volume). Deficiencies of sperm parameters involve either sperm morphology (< 4% morphologically normal sperms in teratozoospermia), sperm concentration (< 15 million/ml in oligozoospermia, and total absence in azoospermia), or sperm motility (< 40% sperm motility or less than 32% with progressive motility is considered asthenozoospermia) [4, 5]. For all abnormal semen profiles, there is an increase in sperm aneuploidy, with the highest aneuploidy rate found in infertile men with severe sperm morphologic abnormalities as in severe oligoasthenoteratozoospermia (OAT) and sperms retrieved from testicular biopsies in non-obstructive azoospermia patients (NOA) [6,7,8].
Intracytoplasmic sperm injection (ICSI) has been used to overcome the problem of severe male factor infertility [9]. It allows the use of spermatozoa from men with severely compromised semen, and greatly reduces the requirements for semen quality, motility, and fertilization ability [8]. Since the advent of ICSI, it was rapidly adopted in invitro fertilization (IVF) clinics worldwide, and it revolutionized infertility treatment and improved the chances of achieving pregnancy in couples with severe male factor infertility [10, 11].
Although ICSI has demonstrated its safety in many large programs worldwide, many concerns have been raised about its safety, especially in regards to the genetic consequences of utilizing sperms from infertile men [12]. Prenatal diagnosis of ICSI pregnancies indicate an increased incidence of chromosomal aneuploidies particularly sex chromosomal aneuploidies (approximately 1–2%) that were shown to be of paternal origin [13]. Fluorescence in situ hybridization (FISH) facilitated the study of numerical chromosomal abnormalities in human sperm nuclei (sperm FISH) from both infertile and fertile men [14]. Testing is advisable for men with chromosome translocations, for couples with unexplained recurrent pregnancy loss or in couples undergoing IVF with or without ICSI failures [11, 15].
The aim of the study was to determine the incidence of sperm aneuploidies for chromosomes 13, 18, 21, X, and Y in semen ejaculates from infertile men with failed intracytoplasmic sperm injection (ICSI). This will ultimately assist infertile couples and enable them to make informed decisions on whether to proceed with ICSI or to combine it with further testing such as preimplantation genetic diagnosis.
Materials and methods
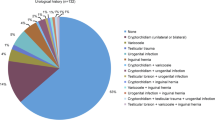
This was a prospective study conducted on thirty-five infertile men with normal karyotypes, with history of at least one ICSI failure, whose female partners were fertile and clinically free with normal karyotypes as well, referred to Cytogenetic Laboratory, Human Genetics Department, Medical Research Institute. Ten normal fertile males with normal semen served as controls. Patients with obstructive azoospermia, history of cancer, chemotherapy, or radiotherapy treatment, positive Y-chromosome microdeletions testing, chronic illnesses such as thyroid dysfunction, diabetes mellitus, or autoimmune disorders, addiction, and smokers were excluded from the study. Informed consent for participation in the study was obtained from all patients, according to the Ethical Guidelines of the Medical Research Institute, Alexandria University.
All patients were subjected to full history taking, hormonal profile including follicle stimulating hormone (FSH), luteinizing hormone (LH), testosterone, and thyroid stimulating hormone (TSH), and computerized semen analysis (CASA) [16].
FISH assay [17]
The semen samples were obtained 2–3 days after sexual abstinence, by masturbation. Fluorescence in situ hybridization technique was applied to semen sample using Prenatal Enumeration Probe kit, REF (LPA 001), which was supplied by Cytocell (Cytocell, Cambridge, UK). The kit contains two probe sets for two separate hybridizations. The 1st probe set for chromosome X centromere, Xp11.1–q11.1 (DXZ1) Green, Y centromere, Yp11.1–q11.1 (DYZ3) Orange and 18 centromere, 18p11.1–q11.1 (D18Z1) Blue, and the 2nd probe set for chromosome 13 unique sequence, 13q14.2 Green and 21 unique sequence, 21q22.13 Orange. Probes and slides preparations as well as hybridization and washing techniques were performed according to manufacturing protocols as follows:
The semen samples obtained for FISH testing were centrifuged for 5 min at 1000 revolutions per minute (rpm) to separate seminal fluid from cells. The supernatants were gently removed. Hypotonic solution (KCl) (Sigma-Aldrich, product of Germany) pre-heated at 37 °C was added to the samples, drop by drop, while mixing on a vortex to obtain a final volume of 10 ml. Then the tubes were placed in a water bath at 37 °C for 30 min. Next, the tubes were centrifuged at 1000 × g for 5 min, and then the supernatant was carefully discarded from each tube. The pellets were resuspended by adding freshly prepared Carnoy’s fixative (3:1 methanol: acetic acid) drop by drop while mixing on a vortex to obtain a final volume of 8 ml. The last step was repeated until obtaining white pellets. Approximately 5 ml from each sample was fixed on a slide. The slides were stored at − 20 °C before processing for FISH. Upon using the slide, it was defrosted by resting at room temperature, and then placed in two consecutive coplin jars with 2xSCC by Vysis (Abbott Laboratories, USA) solution for 3 min each. Next, it was transferred through a series of ethanol washes for 2 min in each coplin jar, starting with 70% ethanol, followed by 90% and finally with 100%. The slide was dried out by leaving it at room temperature. After that, the slide was incubated in dithiothreitol solution (1,4-dithiothreitol 5 mM) at 37 °C in the water bath to decondense the chromatin. The incubation time of the slides in dithiothreitol solution (DTT) (Sigma, product of Canada) was adjusted to be 8 min, after serial trials at our laboratory to avoid disperse FISH signals resulting from excessive exposure to DTT or lack of some FISH signals from short exposure. The slide was immediately transferred into two consecutive coplin jars with 2xSSC for 3 min in each. Next the slide was placed through a series of ethanol washes (70%, 90%, and 100% ethanol), 2 min for each jar. After that it was left to dry out at room temperature. Afterward, the slide denatured for 5 min at 74 ºC and hybridized with 10 µl of probe mixture at 37 ºC overnight using the Thermobrite Slide Processing System (Leica ThermoBrite System, USA). Finally, the slide was counterstained with 4,6-diamidino2-phenylindole (DAPI-II/Antifade; Cytocell, Cambridge, UK). The slides were scanned under fluorescent microscope (Olympus/BX53) equipped with single band-pass filter (DAPI/Green, Red and Blue) which is designated to excite and transmit spectrum DAPI counterstain, spectrum green, spectrum red, and spectrum aqua. Image capture was done using digital high-resolution camera (JENOPTIK: D-007739Jena) (Olympus, Japan) and the software auto image analysis for FISH and karyotyping “LUCIA”. The results of hybridization were assessed by the number of signals from sperm nuclei.
Statistical analysis of the data
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp.). Qualitative data were described using number and percentage. Kolmogorov–Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, and median. Significance of the obtained results was judged at the 5% level. Student’s t test was used for normally distributed quantitative variables, to compare between two studied groups. Mann–Whitney test was used for abnormally distributed quantitative variables, to compare between two studied groups. Kruskal–Wallis test was used for abnormally distributed quantitative variables, to compare between more than two studied groups, and post hoc (Dunn’s multiple comparisons test) for pairwise comparisons. Spearman coefficient was used to correlate between two distributed abnormally quantitative variables.
Results
The age of the studied patients ranged from 26 to 49 years (mean = 33.66 ± 4.65), representing non-statistically significant difference (p = 0.054) compared to the age of controls, ranging from 27 to 39 years (mean = 30.50 ± 3.50). The number of failed ICSI experienced by the couples ranged from 1 to 9 (mean = 4.23 ± 2.14). Only one of our couples achieved pregnancy through ICSI; however, early abortion occurred.
Statistically significant differences were observed between patients and controls regarding sperm concentration, motility, and abnormal morphology (p = 0.001, p < 0.001, p < 0.001 respectively), while no statistically significant difference was detected between the two groups (p = 0.443) regarding semen volume (Table 1). All infertile males included in the study had undergone semen analysis, with the results summarized in Table 2.
Interpretation of FISH results was performed by evaluation of sperm nuclei chromosomal constitution as regards abnormalities in chromosomes 13, 18, 21, X, and Y. The number of nuclei scored per slide was 1000 and 2000 sperms were counted for each patient. The total number of sperms scored in the patients was 70,000, in addition to 20,000 scored sperms in the control group.
Nullisomy (no signal for the given probe and one signal for the other control probe), disomy ( two signals for the given probe and one signal for the other control probe) and diploidy (two signals for both the given probe and the other control probe) of the 5 examined chromosomes were observed in the 35 patients, while aneuploidies other than disomy, nullisomy were observed in 15 patients and polyploidies other than diploidy (triploidy (three signals for both the given probe and the other control probe), tetraploidy (four signals for both the given probe and the other control probe)), were found only in 6 patients.
Disomy 13 was observed 3 times more frequently in patients compared to controls (p < 0.001). Nullisomy 13 was the single most common sperm chromosomal anomaly recorded in patients, detected 12 times more frequently in patients compared to controls (p < 0.001) (Table 4, Fig. 1). In the control group, disomy 21 was 3 times higher in patients compared to controls (p < 0.001). The frequency of nullisomy 21 was 11 times more in patients than in controls (p < 0.001) (Fig. 1). Aneuploidies (13, 21) were observed in patients 8 time more frequently compared to controls (p < 0.001) (Table 3).
Sperm FISH images using dual color probes for chromosomes 13 and 21 showing a Normal spermatozoa with one green signal for chromosome 13 and one red signal for chromosome 21. b Abnormal spermatozoa with one red signal for chromosome 21 and no green signal for chromosome 13 (nullisomy 13). c Abnormal spermatozoa with one green signal for chromosome13 and no red signal for chromosome 21 (nullisomy 21). d Abnormal spermatozoa with no green or red signals for both chromosome13 and chromosome 21 respectively (nullisomy13 and 21)
Diploidy (13, 21) frequency was observed 3 times higher in patients compared to controls (p = 0.003). The frequency of total aberrations (13, 21) was detected 7 times more frequently in patients compared to controls (p < 0.001) (Fig. 2, Table 3).
Sperm FISH images using dual color probes for chromosomes 13 and 21 showing a Normal spermatozoa with one green signal for chromosome 13 and one red signal for chromosome 21. b Abnormal spermatozoa with one red signal for chromosome 21 and no green signal for chromosome 13 (nullisomy 13). c Abnormal spermatozoa with three green signals for chromosome 13(trisomy 13) and two red signals for chromosome 21 (disomy 21). d Abnormal spermatozoa with four green signals for chromosome 13 (tetrasomy 13) and two red signals for chromosome 21 (disomy 21)
The sperms with sex chromosomes disomy showed either XX, or YY, or XY. A statistically significant difference was found between patients and controls as regards XX and YY (p = 0.001, p = 0.014 respectively), while no statistically significant difference existed between the 2 groups as regards the frequency of XY (p = 0.198) (Table 4, Fig. 3).
Sperm FISH image with probes for chromosomes X, Y, and 18 showing a normal spermatozoa with one red signal for Y chromosome and one blue signal for chromosome 18. b Normal spermatozoa with one green signal for X chromosome and one blue signal for chromosome 18. c Abnormal spermatozoa with one green signal X chromosome and no blue signal for chromosome 18 (nullisomy 18). d Abnormal spermatozoa with one blue signal for chromosome 18 and no green or red signals for sex chromosomes (nullisomy sex chromosome). e A diploid spermatozoa with one green signal for X chromosome, one red signal for Y chromosome and two blue signals for chromosome 18 (XY1818). f A diploid spermatozoa with two green signals for X chromosome and two blue signals for chromosome 18 (XX1818). g A diploid spermatozoa with two red signals for Y chromosome and two blue signals for chromosome 18 (YY1818)
In patients, the frequency of sex chromosome disomy was 3 times higher than controls (p < 0.001). Sex chromosome nullisomy was the second most common sperm chromosomal aberration detected in the patients’ group, 16 times more frequent in patients compared to controls (p < 0.001). Sex chromosome aneuploidies were 6.5 times more frequent in patients than in controls (p < 0.001) (Table 4).
The frequency of disomy 18 was 10 times more common in patients compared to controls (p < 0.001). Nullisomy 18 was 15 times more frequent in patients than controls (p < 0.001). The frequency of aneuploidies X, Y, 18 was 8 times higher in patients compared to controls (p < 0.001). Diploidy 18/sex chromosomes was 4 times more frequently detected in patients compared to controls (p = 0.028). In patients, the frequency of total aberrations 18, X, Y was 8 times more frequent compared to controls (p < 0.001) (Table 4).
In the present study, chromosome 13 showed the highest observed anomalies frequency (15.7%), while chromosome 18 had the least observed single chromosome anomalies (12.8%). The frequencies of total aberrations, total aneuploidies and total diploidies for the 5 chromosomes (13, 18, 21, X, Y) were respectively 8, 10, and 3.5 times more common in patients compared to controls (p < 0.001for each).
Spearman correlation test showed a statistically significant inverse correlation between sperm concentration and polyploidy other than diploidy (r = − 0.737, p = 0.010) regarding aberrations 13, 21 (Fig. 4). Similarly, a statistically significant inverse correlation was detected between sperm concentration and sex chromosomes nullisomy (r = − 0.368, p = 0.030), aneuploidy XY18 (r = − 0.402, p = 0.017), polyploidy other than diploidy (r = 0.882, p = 0.012), and total aberrations XY18 (r = − 0.339, p = 0.047). A statistically significant correlation was observed between semen volume and sex chromosome disomy YY (r = 0.334, p = 0.050) and polyploidy other than diploidy (r = 0.882, p = 0.004), as well as between abnormal sperm morphology and aneuploidy other than disomy or nullisomy (r = − 0.717, p = 0.045).
No statistically significant correlation was detected between different semen parameters and total aneuploidy, total diploidy, and total aberrations, while a statistically significant correlation existed between abnormal morphology and autosomal aneuploidy (13, 18, 21) (r = 0.331, p = 0.048) (Fig. 5).
Discussion
Infertility affects about 12% of the population at reproductive age, and about 50% of cases [18] are due to a male factor [19,20,21,22]. Reproductive difficulties are associated not only with somatic chromosomal abnormalities, but also with cytogenetic abnormalities in the germ cells of infertile individuals [23, 24]. There have been concerns regarding the risk of ICSI embryos with chromosomal abnormalities due to oocyte fertilization by aneuploid spermatozoa that might result in an aneuploid blastocyst [25, 26]. Sperm FISH is an effective cytogenetic screening tool for infertile patients that can be used to study sperm chromosomal aberrations [11].
In the current study, patients had statistically significant higher frequencies of 13/21 and XY18 sperm chromosomal aberrations compared to controls, in agreement with Ramasamy, Scovell [27], Vegetti, Van Assche [28], Brahem, Letaief [29], and Levron, Aviram-Goldring [30]. On the other hand, Younan, Sorour [23] reported a non-statistically significant difference.
During meiosis, two mechanisms can result in chromosomal segregation errors: non-disjunction and anaphase lag. Non-disjunction is the predominant mechanism inducing sperm aneuploidy, producing nullisomic and disomic gametes. On the contrary, anaphase lag induces only nullisomic sperm [31]. Meiotic processes first associated with non-disjunction in infertile males were synapsis and recombination [32]. The leading recombination error inducing non-disjunction in meiosis I is the presence of two separated univalents at meiosis I, corresponding to homologous chromosomes which did not recombine. Indirect studies related lack of recombination to the genesis of trisomic conceptuses [33, 34]. Pachytene studies in infertile men also showed a positive correlation between achiasmate bivalents and increased levels of aneuploid spermatozoa [35, 36].
In the current study, the frequencies of disomy13, disomy 21, disomy 18, disomy sex chromosomes (total), XX and YY were significantly higher in patients compared to controls, which goes in agreement with Ramasamy, Scovell [27], Kirkpatrick, Ferguson [37] and Vegetti, Van Assche [28]. In contrast, Younan, Sorour [23], and Tang, Gao [38] reported non-statistically significant difference. Increased aneuploidy frequency may be attributed to mutations of one or more genes involved in the control of common aspects of chromosomal segregation or in cell-cycle checkpoints [39,40,41,42], or involved in DNA repair mechanisms [43].
In the present study, there was statistically significant higher frequency of the total sex chromosomes disomy, XX and YY disomy between patients and controls, while no statistically significant difference between patients and controls for disomy XY was observed although the frequency was higher in the patient group, which is in agreement with Vegetti, Van Assche [28]. In contrast, Ohashi, Miharu [44] and Nishikawa, Murakami [45] found a statistically significant higher frequency of XY disomy in patients compared with normozoospermic controls. This may be attributed to different inclusion criteria, the efficiency of the utilized technique and inter-individual variations in sperm aneuploidy. Disomic sperms with X and Y chromosomes originate from meiosis I due to chromosomal non-separation but may undergo meiotic II chromatid separation plus nuclear cleavage. In contrast, disomic cells with sex-identical chromosome set can originate only from a defective meiosis II [46].
Statistically significant higher frequencies of nullisomy13, nullisomy 21, nullisomy 18 and sex chromosome nullisomy were encountered in the patients group compared to controls in the present study, coinciding with Vegetti, Van Assche [28] but are in disagreement with Tang, Gao [38]. Nullisomy originates from non-disjunction and anaphase lag during meiosis [31, 47]. The frequency of nullisomy can be equal or surpass that of disomy, highlighting the importance of checking for nullisomy and not only disomy when examining for sperm aneuploidies at the clinical level. Sperm nullisomy gives rise to embryo monosomy, which is more detrimental for embryo development than trisomies, manifesting as spontaneous abortions, infertility, or sterility [48].
In the current study, the frequency of total aneuploidies was 10 times higher in patients compared to controls, in agreement with Perrin, Morel [49], Perrin, Louanjli [50] and Brahem, Elghezal [51]. In contrast, Gole, Wong [52] and Sarrate, Vidal [53] reported a 2- to threefold increase of sperm aneuploidies in patients. Constitutive biochemical mechanism is a prevailing mechanism that may induce higher frequencies of somatic and germinal aneuploidies by augmenting both mitotic and meiotic segregation errors [54].
There was a statistically significant higher frequency of diploidy 13/21 in patients compared to controls in the present study. These results are consistent with Younan, Sorour [23], unlike Vegetti, Van Assche [28]. Moreover, a statistically significant higher frequency of diploidy XY18 in patients compared to the control group was observed in the current study; in agreement with Brahem, Letaief [29], in contrast with Miharu, Best [55]. The greater part of polyploid cells are diploids [56]. A delay in synapsis or existence of heterosynapses involving unpaired regions of some chromosomes may result in an incorrect alignment on the metaphase plate, with chromosomes losing ability to migrate to the poles at anaphase I [43]. Lack in the anaphase I checkpoint, that arrests the meiotic process, results in cellular non-division, producing a single diploid secondary spermatocyte, giving rise to two diploid spermatozoa after meiosis II [21, 43, 57].
The current study observed the presence of triploidies, tetraploidies, and pentaploidies in addition to diploidies; a finding in agreement with Brahem, Elghezal [51] and Benzacken, Gavelle [58]. Tetraploid cells could emanate from cell fusion, chromosomal endoreplication in a single cell, or cytokinesis failure [59]. A possible explanation for triploidy is extrusion of one nucleus in a tetraploid sperm. Polyploidies may arise throughout mitotic divisions due to higher levels of sperm centrioles’ defects [58].
The total sperm aberrations frequency for the five studied chromosomes was 55.96% among patients, in agreement with Petousis, Prapas [60], and Ramasamy, Scovell [27]. Also, the total sperm chromosomal aberrations frequency was significantly higher in patients compared to controls, which goes in agreement with previous reports by Petousis, Prapas [60], Tang, Gao [38], and Vegetti, Van Assche [28].
In the present study, total sex chromosome aberrations were more common than total autosomal aberrations in the patients group. These results are consistent with Ghedir, Mehri [61], Harton and Tempest [62], and Baccetti, Collodel [63], in contrast with Rives, Mazurier [64]. Sex chromosomes are particularly susceptible to meiotic non-disjunction, which is the mechanism of sperm aneuploidy, owing to their unique structures, providing only sparse locations of recombination [65]. Under normal conditions, abnormal cells exhibiting non-disjunction of sex chromosomes during meiosis I or II undergo partial or complete meiotic arrest via the pachytene checkpoint mechanism [43].
The most common sperm chromosomal anomaly was nullisomy 13 followed by sex chromosome nullisomy, nullisomy 18 and sex chromosome disomy. Chromosome 13 showed the highest observed frequency for single chromosome anomalies, while chromosome 18 had the least observed single chromosome anomalies. These results are consistent with Tang, Gao [38], but disagree with Petousis, Prapas [60], Tang, Gao [38], Rives, Mazurier [64] Rives, Mazurier [66], and Sanchez-Castro, Jimenez-Macedo [67].
All chromosomes are susceptible to non-disjunction, with certain chromosomes more liable for a higher frequency of non-disjunction. The processes postulated for the occurrence of certain aneuploidies comprise the presence and/or variants of nucleolar organizer regions (NORs), presence and/or variants of heterochromatin, altered frequencies of recombination, differences in size, and non-homologous pairing of sex chromosomes in males [68].
In the current study, there was statistically significant inverse correlation between sperm concentration and sperm chromosomal aberrations including aneuploidy XY18 and total aberrations XY18, in agreement with the study of Vegetti, Van Assche [28], but disagree with Younan, Sorour [23], Collodel, Capitani [69], and Ohashi, Miharu [44]. Oligozoospermia was strongly related with high sperm aneuploidy, whereas significantly increased aneuploidy have been documented in the testicular sperm of patients with non-obstructive azoospermia due to a marked increase in the incidence of meiotic errors in such patients [35, 70,71,72,73,74].
Teratozoospermia is one of the most critical parameters associated with sperm aneuploidy and it is usually associated with a significant increase in the aneuploidy frequency [75]. The current study showed the presence of a statistically significant positive correlation between sperm morphology and chromosomal aberrations. These findings are in agreement with Levron, Aviram-Goldring [65], Brahem, Letaief [29], and Perrin, Morel [49]. In contrast, Younan, Sorour [23] and Vegetti, Van Assche [28] failed to encounter any correlation between sperm chromosomal aberrations and sperm morphology in the patients group.
Finally, the major point of strength of the current study is the fact that, to the best of our knowledge, this was the first study involving sperm FISH examination for infertile males after failed ICSI. On the other hand, our study was conducted on a relatively small sample size, which could be attributed to our selective inclusion criteria. Future larger-scale studies, with the utilization of more diagnostic probes, is recommended, together with aneuploidy screening on embryos by means of PGD.
Conclusion
Sperm FISH examination revealed that normal karyotype infertile males with failed ICSI had significantly higher frequency of sperm chromosomal aberrations (disomy, nullisomy, and diploidy) compared to normal fertile controls. Sperm FISH analysis provides a simple and effective method to assess the male gamete. It defines the proportion of aneuploidy present in the ejaculates of infertile men. Diagnosis of an elevated frequency of sperm chromosome aneuploidy may help to reduce the high financial and emotional expense of repeated ICSI failure. Sperm-FISH can be used to direct reproductive counselling, clinical management, and to allow the couple to make an informed reproductive decision; either to perform PGD or to choose adoption. Couples with abnormal sperm-FISH should always be referred to a genetic counsellor to further understand the risks, benefits, and their alternatives in family planning.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. (https://docs.google.com/spreadsheets/d/16FyhIoc_6IR-255E2YiueAFTHUKWAD1k/edit?usp=sharing&ouid=111278995170865109972&rtpof=true&sd=true).
Abbreviations
- ART:
-
Assisted reproduction technology
- CASA:
-
Computer-aided sperm analysis
- FISH:
-
Fluorescence in situ hybridization
- FSH:
-
Follicle-stimulating hormone
- ICSI:
-
Intracytoplasmic sperm injection
- IVF:
-
Invitro fertilization
- LH:
-
Luteinizing hormone
- NOA:
-
Non-obstructive azoospermia patients
- OAT:
-
Oligoasthenoteratozoospermia
- PGD:
-
Preimplantation genetic diagnosis
- TSH:
-
Thyroid stimulating hormone
References
Inhorn MC (2004) Middle Eastern masculinities in the age of new reproductive technologies: male infertility and stigma in Egypt and Lebanon. Med Anthropol Q 18(2):162–182
Esteves SC (2013) A clinical appraisal of the genetic basis in unexplained male infertility. J Hum Reprod Sci 6(3):176–182
Agarwal A et al (2015) A unique view on male infertility around the globe. Reprod Biol Endocrinol 13:37
Cooper TG et al (2010) World Health Organization reference values for human semen characteristics. Hum Reprod Update 16(3):231–245
Aston K (2014) Genetic susceptibility to male infertility: news from genome-wide association studies. Andrology 2(3):315–321
McAuliffe ME et al (2012) The association between sperm sex chromosome disomy and semen concentration, motility and morphology. Hum Reprod 27(10):2918–2926
Faure AK et al (2007) Predictive factors for an increased risk of sperm aneuploidies in oligo-astheno-teratozoospermic males. Int J Androl 30(3):153–162
Martin RH et al (2003) Analysis of aneuploidy in spermatozoa from testicular biopsies from men with nonobstructive azoospermia. J Androl 24(1):100–103
Kahraman S et al (2006) Preliminary FISH studies on spermatozoa and embryos in patients with variable degrees of teratozoospermia and a history of poor prognosis. Reprod Biomed Online 12(6):752–761
Ushijima C et al (2000) Analysis of chromosomal abnormalities in human spermatozoa using multi-colour fluorescence in-situ hybridization. Hum Reprod 15(5):1107–1111
Hwang K, Weedin JW, Lamb DJ (2010) The use of fluorescent in situ hybridization in male infertility. Ther Adv Urol 2(4):157–169
Palermo G et al (1992) Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 340(8810):17–18
Aittomaki K et al (2004) Safety issues in assisted reproduction technology: should ICSI patients have genetic testing before treatment? A practical proposition to help patient information. Hum Reprod 19(3):472–476
Martin RH, Rademaker A (1995) Reliability of aneuploidy estimates in human sperm: results of fluorescence in situ hybridization studies using two different scoring criteria. Mol Reprod Dev 42(1):89–93
Carrell DT (2008) The clinical implementation of sperm chromosome aneuploidy testing: pitfalls and promises. J Androl 29(2):124–133
Raziel A et al (2002) Increased frequency of female partner chromosomal abnormalities in patients with high-order implantation failure after in vitro fertilization. Fertil Steril 78(3):515–519
Sarrate Z, Anton E (2009) Fluorescence in situ hybridization (FISH) protocol in human sperm. J Vis Exp 31:1405
Chandra A et al (2005) Fertility, family planning, and reproductive health of US women; data from the 2002 National Survey of Family Growth. Centers for disease control and prevention 25:2006–1977
van Echten-Arends J et al (2011) Chromosomal mosaicism in human preimplantation embryos: a systematic review. Hum Reprod Update 17(5):620–627
Taylor TH et al (2014) The origin, mechanisms, incidence and clinical consequences of chromosomal mosaicism in humans. Hum Reprod Update 20(4):571–581
Egozcue S et al (2000) Human male infertility: chromosome anomalies, meiotic disorders, abnormal spermatozoa and recurrent abortion. Hum Reprod Update 6(1):93–105
Fragouli E et al (2017) Analysis of implantation and ongoing pregnancy rates following the transfer of mosaic diploid–aneuploid blastocysts. Hum Genet 136(7):805–819
Younan D, Sorour A, Genedy R (2015) Aneuploidy frequency in spermatozoa of Egyptian men with normal and abnormal semen parameters using fluorescence in situ hybridisation. Andrologia 47(2):228–235
Lissitsina J, Mikelsaar R, Punab M (2006) Cytogenetic analyses in infertile men. Arch Androl 52(2):91–95
Hassold T, Hunt PA, Sherman S (1993) Trisomy in humans: incidence, origin and etiology. Curr Opin Genet Dev 3(3):398–403
Vialard F et al (2008) Gamete cytogenetic study in couples with implantation failure: aneuploidy rate is increased in both couple members. J Assist Reprod Genet 25(11–12):539–545
Ramasamy R et al (2015) Fluorescence in situ hybridization detects increased sperm aneuploidy in men with recurrent pregnancy loss. Fertil Steril 103(4):906-909.e1
Vegetti W et al (2000) Correlation between semen parameters and sperm aneuploidy rates investigated by fluorescence in-situ hybridization in infertile men. Hum Reprod 15(2):351–365
Brahem S et al (2013) Efficacy of the density gradient centrifugation method in eliminating sperm with aneuploidy. Andrologia 45(3):158–162
Levron J et al (2001) Sperm chromosome abnormalities in men with severe male factor infertility who are undergoing in vitro fertilization with intracytoplasmic sperm injection. Fertil Steril 76(3):479–484
Templado C, Uroz L, Estop A (2013) New insights on the origin and relevance of aneuploidy in human spermatozoa. Mol Hum Reprod 19(10):634–643
Templado C et al (1981) A new meiotic mutation: desynapsis of individual bivalents. Hum Genet 59:345–348
Oliver TR et al (2009) Investigation of factors associated with paternal nondisjunction of chromosome 21. Am J Med Genet A 149(8):1685–1690
Thomas NS et al (2000) A reinvestigation of non-disjunction resulting in 47, XXY males of paternal origin. Eur J Hum Genet 8(10):805–808
Sun F et al (2008) Reduced meiotic recombination on the XY bivalent is correlated with an increased incidence of sex chromosome aneuploidy in men with non-obstructive azoospermia. Mol Hum Reprod 14(7):399–404
Ferguson KA et al (2007) Abnormal meiotic recombination in infertile men and its association with sperm aneuploidy. Hum Mol Genet 16(23):2870–2879
Kirkpatrick G et al (2008) A comparison of sperm aneuploidy rates between infertile men with normal and abnormal karyotypes. Hum Reprod 23(7):1679–1683
Tang SS et al (2010) Aneuploidy and DNA fragmentation in morphologically abnormal sperm. Int J Androl 33(1):e163–e179
Tolmie JL et al (1988) Siblings with chromosome mosaicism, microcephaly, and growth retardation: the phenotypic expression of a human mitotic mutant? Hum Genet 80(2):197–200
Papi L et al (1989) Evidence for a human mitotic mutant with pleiotropic effect. Ann Hum Genet 53(3):243–248
Nash RN (1997) Recurrent multiple aneuploidies: a family with autosomal recessive failure of mitotic control. Am J Hum Genet 61:A136
Gazvani MR et al (2000) Evaluation of the role of mitotic instability in karyotypically normal men with oligozoospermia. Fertil Steril 73(1):51–55
Wong EC et al (2008) Sperm aneuploidy and meiotic sex chromosome configurations in an infertile XYY male. Hum Reprod 23(2):374–378
Ohashi Y et al (2001) High frequency of XY disomy in spermatozoa of severe oligozoospermic men. Hum Reprod 16(4):703–708
Nishikawa N et al (2000) Sex chromosomal analysis of spermatozoa from infertile men using fluorescence in situ hybridization. J Assist Reprod Genet 17(2):97–102
Pison-Rousseaux S (2003) Origin of sperm with extra chromosome set. Hum Reprod 18(2):459–460
Sarrate Z, Vidal F, Blanco J (2014) Meiotic abnormalities in metaphase I human spermatocytes from infertile males: frequencies, chromosomes involved, and relationship with polymorphic karyotype and seminal parameters. Asian J Androl 16(6):838
Munné S et al (2004) Differences in chromosome susceptibility to aneuploidy and survival to first trimester. Reprod Biomed Online 8(1):81–90
Perrin A et al (2008) Study of aneuploidy in large-headed, multiple-tailed spermatozoa: case report and review of the literature. Fertil Steril 90(4):1201.e13–7
Perrin A et al (2011) Study of aneuploidy and DNA fragmentation in gametes of patients with severe teratozoospermia. Reprod Biomed Online 22(2):148–154
Brahem S et al (2011) Cytogenetic and molecular aspects of absolute teratozoospermia: comparison between polymorphic and monomorphic forms. Urology 78(6):1313–1319
Gole LA et al (2001) Does sperm morphology play a significant role in increased sex chromosomal disomy? A comparison between patients with teratozoospermia and OAT by FISH. J Androl 22(5):759–763
Sarrate Z, Vidal F, Blanco J (2010) Role of sperm fluorescent in situ hybridization studies in infertile patients: indications, study approach, and clinical relevance. Fertil Steril 93(6):1892–1902
Gazvani MR et al (2000) Role of mitotic control in spermatogenesis. Fertil Steril 74(2):251–256
Miharu N, Best RG, Young SR (1994) Numerical chromosome abnormalities in spermatozoa of fertile and infertile men detected by fluorescence in situ hybridization. Hum Genet 93(5):502–506
Jakab A et al (2003) Origin of sperm with extra chromosome set. Hum Reprod 18(2):459–459
Blanco J, Egozcue J, Vidal F (2001) Meiotic behaviour of the sex chromosomes in three patients with sex chromosome anomalies (47, XXY, mosaic 46, XY/47, XXY and 47, XYY) assessed by fluorescence in-situ hybridization. Hum Reprod 16(5):887–892
Benzacken B et al (2001) Familial sperm polyploidy induced by genetic spermatogenesis failure: case report. Hum Reprod 16(12):2646–2651
In’t Veld PA et al (1997) Intracytoplasmic sperm injection (ICSI) and chromosomally abnormal spermatozoa. Hum Reprod (Oxford, England) 12(4):752–754
Petousis S, et al., Fluorescence in situ hybridisation sperm examination is significantly impaired in all categories of male infertility. Andrologia, 2018;50(2).
Ghedir H et al (2014) Meiotic segregation and sperm DNA fragmentation in Tunisian men with dysplasia of the fibrous sheath (DFS) associated with head abnormalities. J Assist Reprod Genet 31(9):1167–1174
Harton GL, Tempest HG (2012) Chromosomal disorders and male infertility. Asian J Androl 14(1):32–39
Baccetti B et al (2005) Fluorescence in situ hybridization and molecular studies in infertile men with dysplasia of the fibrous sheath. Fertil Steril 84(1):123–129
Rives N et al (1998) Assessment of autosome and gonosome disomy in human sperm nuclei by chromosome painting. Hum Genet 102(6):616–623
Levron J et al (2013) Aneuploidy rates for chromosomes X/Y and 18 among preselected spermatozoa in men with severe teratospermia. Reprod Biomed Online 27(3):280–285
Rives N, Mazurier S, Sibert L (1998) Incidence of aneuploidy in sperm nuclei of infertile men. Hum Reprod 245(Suppl 13):126–127
Sanchez-Castro M et al (2009) Prognostic value of sperm fluorescence in situ hybridization analysis over PGD. Hum Reprod 24(6):1516–1521
Spriggs E, Rademaker A, Martin R (1996) Aneuploidy in human sperm: the use of multicolor FISH to test various theories of nondisjunction. Am J Hum Genet 58(2):356
Collodel G et al (2007) Sperm aneuploidies and low progressive motility. Hum Reprod 22(7):1893–1898
Mougou-Zerelli S et al (2011) Detection of aneuploidy rate for chromosomes X, Y and 8 by fluorescence in-situ hybridization in spermatozoa from patients with severe non-obstructive oligozoospermia. J Assist Reprod Genet 28(10):971–977
Durak Aras B et al (2012) Exploring the relationship between the severity of oligozoospermia and the frequencies of sperm chromosome aneuploidies. Andrologia 44(6):416–422
Rodrigo L et al (2011) Testicular sperm from patients with obstructive and nonobstructive azoospermia: aneuploidy risk and reproductive prognosis using testicular sperm from fertile donors as control samples. Fertil Steril 95(3):1005–1012
Vozdova M et al (2012) Testicular sperm aneuploidy in non-obstructive azoospermic patients. Hum Reprod 27(7):2233–2239
Gonsalves J et al (2004) Defective recombination in infertile men. Hum Mol Genet 13(22):2875–2883
Calogero AE et al (2001) Aneuploidy rate in spermatozoa of selected men with abnormal semen parameters. Hum Reprod 16(6):1172–1179
Acknowledgements
Not applicable.
Code availability
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
RE: data acquisition, data analysis, and drafting the work. AB and SK: design of the work, interpretation of data, and revision. YO: clinal assessment of cases. GE: design of the work, interpretation of data, and revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was reviewed and approved by the Ethics Committee (IORG#: IORG0008812), Medical Research Institute, Alexandria University. Informed written consent to participate was obtained from all participants/their guardians.
Consent for publication
Informed written consent for publication was obtained from all participants/their guardians.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elnahas, R.F., Behery, A.K., Kholeif, S. et al. Sperm chromosomal abnormalities in infertile men with failed intracytoplasmic sperm injection (ICSI). Middle East Fertil Soc J 28, 18 (2023). https://doi.org/10.1186/s43043-023-00144-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-023-00144-8