Abstract
Background
Polycystic ovary syndrome (PCOS) is the most typical endocrine disorder affecting women worldwide. Although the etiology of PCOS is not fully understood, genetic factors are believed to play an essential role in its pathogenesis. Hence, this paper presents a review of the outcome of functional enrichment analysis of pathways associated with PCOS phenotypes for the identification of potential molecular targets as area of further research for therapeutic development for PCOS.
Method
It is the implementation of comprehensive literature search in database including PubMed and Google Scholar and functional analysis of genes including the HSD3B2, PPARG, PPP1R3A, LMNA, and AMH and their roles in the metabolic pathways associated with PCOS.
Findings
The genes including HSD3B2, PPARG, and LMNA emerged as the most important genes in relation to PCOS, suggesting that they could play key roles in regulating different aspects of PCOS pathogenesis. These findings provide valuable insights into the molecular mechanisms that underlie the complex condition of PCOS and highlight the potential of targeting these genes and their specific pathways as a promising approach to developing effective treatments for PCOS.
Conclusion
It was concluded that these exploring pathways associated with these genes could provide new insights into the genetic factors contributing to PCOS, and the study recommended further research on these targets for improving the health and quality of life women battling with PCOS worldwide.
Similar content being viewed by others
Background
Polycystic ovarian syndrome (PCOS) is a complex reproductive disorder and a significant cause of infertility [1]. While its underlying genetic factors contribute to this endocrine condition, PCOS does not follow a clear pattern of Mendelian inheritance [2]. Globally, anovulatory infertility cases are often associated with PCOS, posing challenges to the field of reproductive science [3]. In Africa, women bear the brunt of infertility stigma, leading to isolation and abandonment due to childlessness, as well as social, economic, and cultural burdens [4,5,6].
PCOS is not only a leading cause of infertility but also associated with various clinical conditions, including irregular menstrual cycles, hormone dysregulation, diabetes mellitus, endometrial cancer, and cardiovascular diseases [7]. This makes PCOS a significant challenge to family well-being and society worldwide. Although PCOS is strongly linked to genetics, it does not adhere to Mendelian inheritance principles. Environmental exposures to xenobiotics have been suggested as potential causes, highlighting the need to understand the gene-phenotype relationships related to PCOS [8, 9].
Polycystic ovary syndrome (PCOS) is also relevant to the United Nations’ Sustainable Development Goals (SDGs). Specifically, it relates to SDG 3 (Good Health and Well-being), as it is a hormonal disorder that profoundly affects the health and well-being of individuals. Women with PCOS face an increased risk of several adverse health outcomes, such as type 2 diabetes, cardiovascular disease, and various types of cancer [11,12,13]. Understanding PCOS and developing more effective treatments can significantly improve the health and well-being of affected individuals, thus contributing to the achievement of the SDGs.
Additionally, PCOS has implications for SDG 5 (Gender Equality) as it primarily affects women and has a significant impact on their reproductive health and overall well-being, particularly in Africa, where childlessness stigmatizes women. Understanding PCOS and its effects on women’s health can promote gender equality and support women’s right to access quality healthcare. Furthermore, PCOS can be associated with SDG 11 due to environmental and lifestyle factors prevalent in urban areas, such as the risk of exposure to endocrine-disrupting chemicals (EDCs) and sedentary behavior, which are reported to contribute to the incidence of PCOS [14, 15]. Studying PCOS can lead to the development of more accurate diagnostic tools and effective treatments for women with the condition. A better understanding of PCOS and its impact on reproductive health can contribute to improved family planning, thus controlling the global population growth rate and supporting sustainable development. Therefore, by addressing the underlying causes and impacts of PCOS, it is possible to promote a more sustainable and equitable world.
Etiology of PCOS with a focus on genetic and environmental factors contributing to the development of the syndrome
PCOS is a common case of infertility across the world, and between 5 and 10% cases of infertility diagnosis have been reportedly linked with its occurrence in different parts of the world including the developing countries [1]. In Nigeria, about 20% cases of infertility has been linked with PCOS, while about 75% cases of the anovulatory infertilities have been linked with it. These are indications that PCOS could be referred to as the chief executive being one of the most common forms of infertility in the country [2, 3]. Unfortunately, the pathophysiology of PCOS is not clear, although genetic factors have been verified through genome-wide association studies. Hence, there is a need to investigate possible functional roles of these genetic complications in different population ancestries to move toward developing effective therapeutic measures [4]. PCOS is also a metabolic disorder reportedly linked with oxidative stress which could relate to the activities of mitochondria genomic regulations and maintenance [5]. Clinical trial registration numbers and information regarding ethical approval should be included if applicable.
Polycystic ovary syndrome (PCOS) is a complex and heterogeneous endocrine disorder affecting 5–15% of reproductive-aged women which the exact cause is not fully understood, but it is believed to result from a combination of genetic and environmental factors [5]. There are research studies which indicate that there is a genetic component to PCOS as some studies have found that there is an increased risk of developing it among first-degree relatives of women with the condition [6,7,8]. Additionally, genome-wide association studies (GWAS) have identified several genetic variants that are associated with PCOS, including variants in genes involved in insulin resistance, inflammation, and androgen production [9]. Although the specific genetic factors contributing to PCOS are not yet fully understood, there are several genes identified for playing a possible role in the occurrence of the disease. Mutations in genes involved in insulin resistance have been linked to an increased risk of PCOS, as insulin resistance is a common feature of the condition [10].
However, while genetics may increase the risk of developing PCOS, it is not the only factor; there are other factors including environmental-linked factors, such as diet, exercise, and stress, which may also play a role in the development and severity of the condition [11]. Therefore, while there could be a genetic dimension to PCOS, it is important to consider both genetic and environmental factors when assessing and managing the condition. This made PCOS a complex endocrine disorder affecting many women of reproductive age to study since the exact cause of PCOS is not yet fully understood, and a multifactorial condition could be influenced by both genetic and environmental factors.
Genome-wide association studies (GWAS) are a type of study that examines the entire genome of individuals to identify genetic variants that may be associated with a particular disease or trait. In the case of PCOS, the application of GWAS has identified several genetic variants that are associated with the condition, and one of the most consistent among them is the association between PCOS and genes involved in insulin resistance, which occurs when the body’s cells become less responsive to the hormone insulin causing high levels of insulin in the blood [4]. This contributes to the development of PCOS because insulin can stimulate the ovaries to produce more androgens, which can disrupt the menstrual cycle and lead to the anovulation which is a symptom of PCOS.
Meanwhile, there are other several genes and genetic factor that could get involved in insulin signaling and glucose metabolism, and through this pathway, there could be increasing development of PCOS, such as the expression of gene for insulin receptor substrate 1 (IRS1). In addition to insulin resistance, inflammation is another metabolic activity believed to be playing a role in the development of PCOS. There are also studies which have found that women with PCOS have higher levels of inflammatory markers in their blood compared to women without the condition. Some of the genetic variants that have been associated with PCOS are also involved in immune function and inflammation, including the genes for tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 [12].
However, the production of male reproductive hormone, androgen, is a hallmark feature of PCOS, and this has been confirmed through GWAS which identified genetic variants in genes involved in androgen synthesis and metabolism, such as the gene for the luteinizing hormone receptor (LHCGR) and the gene for 17-hydroxysteroid dehydrogenase type 4 [13]. These genetic variants may influence the production and metabolism of androgens in the ovaries, which can contribute to the development of PCOS symptoms. These valuable insights into the genetic basis of PCOS have contributed to identification of the potential biological pathways that could be targeted for the treatment of the condition. However, it is important to note that the genetic variants identified in GWAS only explain a small proportion of the overall heritability of PCOS, and that other factors, such as epigenetics and environmental factors, are also likely to play a role in the development of the condition, which is why functionally some of the pathways have to be elucidated. While GWAS studies are valuable for identifying genetic variants associated with PCOS, complementary functional genomics and transcriptomics approaches are necessary to gain a deeper understanding of the functional genetic differences underlying the condition which is why this paper focus on identifying molecular targets that could be exploited for better understanding of the PCOS.
As parts of the etiology of PCOS, environmental factors such as diet, physical activity, and exposure to endocrine-disrupting chemicals (EDCs) have been implicated in the development of PCOS [14]. The consumption of high-calorie diets rich in carbohydrates have been reported to contribute to insulin resistance and hyperinsulinemia, which are often common in women diagnosed with PCOS. Also, exposure to EDCs such as bisphenol A (BPA) and phthalates, because of their potential capacity of causing endocrine disruption, can contribute to the development of PCOS through hormonal dysregulation which is a hallmark feature of PCOS [15]. This is often accompanied with elevated levels of androgens, such as testosterone, hirsutism (excess hair growth), and acne which is a skin condition in adolescent characterized by red pimples on the skin, especially on the face, due to inflamed or infected sebaceous glands in women. These group of young women may also be experiencing some irregularities in their menstrual cycles or anovulation (lack of ovulation) due to disruptions in the hypothalamic-pituitary-ovarian axis. This has also been reportedly linked with insulin resistance and hyperinsulinemia which are common in women with PCOS and can contribute to the hormonal dysregulation those women. Metabolic dysregulation, including insulin resistance and hyperinsulinemia, is common in women with PCOS, and insulin resistance can contribute to the elevated androgen levels in PCOS and can also lead to metabolic complications, such as type 2 diabetes and cardiovascular disease. The PCOS is a complex disorder resulting from a combination of genetic and environmental factors sandwich by hormonal and metabolic dysregulation as hallmark features of the disorder. Hence, the understanding of the underlying mechanisms of PCOS is essential for developing effective treatments and improving outcomes for women with the disorder.
Mendelian genetics and inheritance of PCOS
Mendelian genetics is based on the laws of inheritance proposed by Gregor Mendel, which describe the way in which traits are passed down from one generation to another. According to the principles of Mendelian genetics, a gene inherited from either parent segregates at an equal frequency, meaning that there is a 50–50 chance that an individual will inherit the gene from either the mother or the father [16]. However, in some cases, genes may not follow Mendelian genetics, and whenever this happen, the genes may be inherited in a non-Mendelian fashion, such as those that are linked with or those that are controlled by multiple genes [17]. In such cases, the frequency of inheritance may deviate from the expected 50:50 ratio, and the expression of the trait may be more complex than predicted by simple Mendelian genetics.
Additionally, there are some genetic disorders that could result from mutations in the DNA that affect the way in which genes are inherited [18]. For example, some genetic disorders are caused by dominant genes, which means that an affected individual only needs to inherit one copy of the mutated gene to develop the disorder [19]. Also, there are other genetic disorders not following the Mendelian inheritance that could be caused by recessive genes, which means that an affected individual must inherit two copies of the mutated gene (one from each parent) to develop the disorder [19, 20]. In essence, while Mendelian genetics provides a useful framework for the understanding of inheritance of many traits, not all genes and genetic disorders follow the simple Mendelian patterns of inheritance [21]. An example of such traits is the PCOS which does not follow the simple Mendelian patterns of inheritance and to understand the underlying mechanisms of the PCOS inheritance. Hence, it would be necessary to apply some other genetic approaches including linkage analysis, GWAS, epigenetic, and functional analyses for better understanding of the condition from the genetic perspective.
Linkage analysis is a technique used in identification of genes that are physically located close together on a chromosome and tend to be inherited together; this technique can be used to study complex traits that are influenced by multiple genes and can contribute to the identification of candidate genes that may be involved in a trait of interest [22]. There is another approach known as GWAS which as to with study that involves comparing the DNA of people with a particular trait or disorder to the DNA of people without the trait or disorder. By looking for the differences in the DNA sequences between these two groups of people, researchers can identify genetic variations that are associated with the trait or disorder.
Epigenetic changes on the other hands are modifications to the DNA molecule that can influence gene expression and function, without changing the underlying DNA sequence, and it has been largely associated with environmental influences [23, 24]. The approach of studying epigenetic changes can help researchers understand how environmental and other nongenetic factors can influence the expression of genes and contribute to the development of complex traits. Functional genetic analysis involves studying the effects of specific genes or genetic variations on the function of cells and organisms. This can involve techniques such as gene editing or gene silencing, which can be used to modify or block the expression of specific genes to study their effects [25, 26]. The application of these and other approaches could contribute to gaining a better understanding of the complex inheritance patterns associated with the underlying genetic and epigenetic mechanisms involved in the development of PCOS.
Metabolic pathways in PCOS: focus on metabolic pathways of insulin resistance, dyslipidemia, and inflammation and their associated genes
Metabolic dysregulation is a common feature of polycystic ovarian syndrome (PCOS), involving a hormonal disorder that affects reproductive-age women [27]. Women with PCOS often exhibit insulin resistance characterized by difficulty using insulin to regulate blood sugar levels which can lead to high levels of insulin expression in the bloodstream which could consequently result to other range of metabolic and hormonal disturbances [28]. Hence, studying these metabolic dysregulations pathways in PCOS could be very important because it can facilitate better understanding of the underlying mechanisms of the disorder which is still poorly understood. The studying of these metabolic dysregulation could also lead to identifying of the specific metabolic pathways that are disrupted due to PCOS which could also lead to the development of targeted and effective treatments for the disorder. Furthermore, studying these metabolic disturbances could facilitate gaining insights into the long-term health risks associated with the PCOS and could contribute to the development of strategies for prevention and or managing these complications [29, 30]. Finally, research into metabolic dysregulation in PCOS has the potential to improve the understanding of all the combined factors including genetic, environmental, and lifestyle factors associated with the disease.
Polycystic ovary syndrome (PCOS) is a complex condition that is characterized by a range of clinical, hormonal, and metabolic features; although PCOS is typically classified as a single entity, recent research has suggested that there may be distinct subtypes of PCOS based on different underlying metabolic and hormonal profiles47. The first proposed PCOS subtypes include the insulin-resistant PCOS which is the subtype characterized by insulin resistance, leading to hyperinsulinemia and compensatory hyperandrogenemia. Typically, women with this subtype of PCOS, there are high levels of insulin and testosterone, and they are at increased risk for type 2 diabetes and cardiovascular disease [31]. There is also post-pill PCOS which is the subtype believed to be caused using hormonal contraceptives, such as the combined oral pills, which can disrupt the normal hormonal balance in the body. While this has been reported, it has also been contested that what happened is not post-pill PCOS but rather just a myth that birth control pills cause PCOS due to a condition called post-birth control syndrome which was reported as a collection of symptoms that can occur in some people when they stop taking hormonal birth control pill [32]. Meanwhile, the proponents of the concept associated the habits of experiencing of irregular periods, skin inflammation, and excessive growth of dark or coarse hair in a male-like pattern such as excessive growth of hair on face, chest, and back even after discontinuing taking of the hormonal contraceptives as PCOS. There is also what has been described as inflammatory PCOS which is a subtype reported to be associated with chronic low-grade inflammation as well as insulin resistance and hyperandrogenemia [33]. It was reported that women with inflammatory PCOS may have elevated levels of inflammatory markers, such as C-reactive protein (CRP), but may benefit from anti-inflammatory therapies [34]. The C-reactive protein (CRP) is a protein that is produced by the liver in response to inflammation in the body; its levels can rise rapidly in response to tissue injury, infection, or other inflammatory processes and can be measured in the blood as a marker of inflammation. The CRP could serve as an important biomarker in a range of health conditions, including cardiovascular disease, autoimmune disorders, and infections, and within the context of polycystic ovary syndrome (PCOS), elevated levels of CRP have been observed in some women with the inflammatory subtype of PCOS, which is characterized by chronic low-grade inflammation [35]. Therefore, measuring CRP levels can help to identify the presence and severity of inflammation-induced PCOS and can be used to monitor the response to anti-inflammatory therapies.
There is also adrenal PCOS which is a subtype that is characterized by increased adrenal androgen production, which can lead to high levels of dehydroepiandrosterone sulfate DHEA-S and androstenedione. According to reports, women with adrenal PCOS may have fewer ovarian cysts and may not meet the diagnostic criteria for PCOS based on ultrasound findings but may still have elevated androgen levels and other symptoms including insulin resistance, body weight changes, and hyperlipidemia. The DHEA-S is a hormone produced by the adrenal glands, which are small glands located on top of the kidneys. DHEA-S is a sulfated form of the hormone DHEA and is the most abundant circulating steroid hormone in the body. DHEA-S levels are typically highest in young adulthood and decline with age, but it is involved in the production of other hormones, such as testosterone and estrogen, and plays a role in a range of physiological processes, including bone health, immune function, and cognitive function [36]. In the context of polycystic ovary syndrome (PCOS), elevated levels of DHEA-S are often observed in women with the adrenal subtype of PCOS, which is characterized by increased adrenal androgen production in addition to DHEA-S; there could be other adrenal androgens elevation such as androstenedione which may also be elevated. Hence, measuring the DHEA-S levels could also serve as a lead in the identification of the presence of adrenal androgen excess which may be used to differentiate the adrenal subtype of PCOS from other subtypes.
Finally, one of key genes associated with insulin resistance in PCOS is the insulin receptor substrate 1 (IRS1) gene which plays a crucial role in insulin signaling; it is essential for maintaining normal glucose metabolism in the body [37]. Dysregulation of insulin signaling pathways can lead to insulin resistance, a key metabolic abnormality associated with PCOS [38]. Insulin resistance refers to a diminished response of target tissues, such as skeletal muscle, adipose tissue, and the liver, to the actions of insulin. This impaired response can result in elevated levels of circulating insulin, known as hyperinsulinemia, as the body tries to compensate for the reduced effectiveness of insulin.
Insulin resistance is closely linked to metabolic disturbances observed in PCOS, including dyslipidemia and inflammation. This is connected to dyslipidemia which is the abnormal lipid profiles characterized by increased levels of triglycerides, low-density lipoprotein cholesterol (LDL-C), and decreased levels of high-density lipoprotein cholesterol (HDL-C). Insulin resistance contributes to dyslipidemia by impairing the clearance of triglyceride-rich particles and promoting lipolysis in adipose tissue, leading to elevated levels of circulating free fatty acids. These alterations in lipid metabolism contribute to the development of atherogenic dyslipidemia, increasing the risk of cardiovascular disease in women with PCOS [39].
Furthermore, insulin resistance can also induce a state of chronic low-grade inflammation in PCOS. Adipose tissue, particularly visceral adipose tissue, produces various pro-inflammatory cytokines and adipokines, such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and leptin. These inflammatory molecules contribute to a state of systemic inflammation, which further impairs insulin signaling and exacerbates insulin resistance [40]. In turn, insulin resistance can promote adipose tissue dysfunction, leading to a perpetuating cycle of inflammation and metabolic dysfunction in PCOS. The role of IRS1 in insulin signaling is crucial in this context. Variations in the IRS1 gene can affect the efficiency of insulin signaling pathways, leading to reduced downstream signaling cascades and impaired glucose uptake in target tissues. This diminished insulin sensitivity contributes to insulin resistance and the subsequent metabolic disturbances observed in PCOS.
Therefore, an understanding of the intricate interplay between IRS1, insulin signaling, and metabolic pathways related to insulin resistance, dyslipidemia, and inflammation is essential for unraveling the complex pathophysiology of PCOS. Targeting these pathways through precision medicine approaches may offer potential therapeutic strategies for managing PCOS, such as the development of novel insulin sensitizers or targeted interventions aimed at improving dyslipidemia and reducing chronic inflammation. Further research is needed to elucidate the precise mechanisms underlying the role of IRS1 in PCOS and to explore the therapeutic potential of targeting this pathway for personalized treatments in the future.
Functional enrichment analysis of pathways associated with PCOS phenotypes
Polycystic ovary syndrome (PCOS) is a common endocrine disorder affecting reproductive-aged women worldwide; it is characterized by a wide range of symptoms, including irregular menstrual cycles, ovarian cysts, hyperandrogenism, and insulin resistance. However, the molecular mechanisms underlying the pathophysiology of PCOS are not fully understood; because of this, functional enrichment analysis is a powerful tool that can be used to identify pathways and gene having differential regulation in PCOS patients which could also be playing roles in its management. By analyzing the enrichment of specific functional categories within sets of genes associated with different PCOS phenotypes, researchers could gain insight into the underlying molecular mechanisms and selection of potential therapeutic targets for this complex disorder. In this context, functional enrichment analysis of pathways associated with PCOS phenotypes is being carried out and reported in this study.
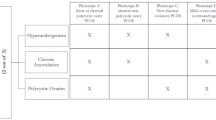
Polycystic ovary syndrome (PCOS) is a complex endocrine disorder with a complex genetic basis, but genetic studies have identified several genes and genomic regions associated with PCOS, many of which remain poorly characterized. Some of these genes are listed in the Online Mendelian Inheritance in Man (OMIM), which is a database that provides information on genes and genetic disorders, including those associated with PCOS. In this study, a PCOS phenotype table was generated from the OMIM database (Table 1). The table provides a comprehensive summary of the known genetic factors involved in PCOS which can serve as a valuable resource for researchers interested in understanding the genetic underpinnings of this disorder. In this article, we will discuss the implications of these findings for our understanding of PCOS pathogenesis and potential diagnostic and therapeutic strategies. The genes generated through the PCOS phenotype were also functionally enriched to elucidate pathways that can serve as target for the PCOS understanding and treatment.
The autosomal recessive inheritance is a pattern in which an individual must inherit two copies of a defective gene, one from each parent, to develop a particular genetic disorder [41]. This means that both parents must carry one copy of the defective gene but do not show any symptoms of the disorder because they have one normal copy of the gene that can produce the necessary protein. However, when both parents pass on their defective gene to their offspring, the child inherits two defective copies, which results in the manifestation of the disorder. Autosomal recessive disorders are relatively rare, and many are caused by mutations in a single gene; examples of autosomal recessive disorders include sickle cell anemia, cystic fibrosis, Tay-Sachs disease, and phenylketonuria. In general, individuals with autosomal recessive disorders have a 25% chance of having an affected child with each pregnancy, a 50% chance of having a carrier child, and a 25% chance of having an unaffected, noncarrier child. Therefore, genetic counseling can help individuals who are carriers of autosomal recessive disorders to understand the risks associated with having children and make informed decisions about marriage, number of children, and on termination of affected pregnancies. Testing can also be done to determine whether individuals are carriers of certain autosomal recessive disorders.
The contiguous gene duplication or deletion syndrome (CGDS) is a type of genetic disorder in which multiple genes are involved; in CGDS, a segment of DNA containing multiple genes is either duplicated or deleted, leading to a range of clinical features [42]. The affected genes are located next to each other on the chromosome and are inherited together as a unit; the CGDS could also result from a variety of genetic mechanisms, including nonallelic homologous recombination, microdeletions or microduplications, and chromosomal translocations. The exact mechanism and location of the duplication or deletion will determine which genes are affected and the severity of the symptoms. The clinical presentation of CGDS can vary widely depending on the specific genes involved and the extent of the duplication or deletion. Some common features of CGDS can include intellectual disability, developmental delay, congenital abnormalities, growth and feeding problems, seizures, and behavioral issues. There are examples of CGDS including Williams syndrome, which is caused by a deletion of 26–28 genes on chromosome 7, and Potocki-Lupski syndrome, which is caused by a duplication of a segment of chromosome 17 that includes about 20 genes. Other examples include Smith-Magenis syndrome, caused by a deletion on chromosome 17 that affects several genes, and 16p11.2 deletion and duplication syndromes, which involve the loss or gain of several genes on chromosome 16. The diagnosis of CGDS typically involves genetic testing, such as chromosomal microarray analysis or next-generation sequencing, to identify the location and extent of the duplication or deletion. Management of CGDS involves addressing the specific symptoms and providing supportive care which may include therapies such as speech and occupational therapy, behavioral interventions, and medical treatments for seizures, gastrointestinal problems, or other medical issues that may arise.
The cytogenetic location of the PCOS-associated genes (Table 1) showed that most of the genes are located on chromosomes 1 (1p12 and 1q22) and 19 (19p13.2 and 19p13.3), respectively. These cytogenetic locations contain a different set of genes, genetic variations, and regulatory elements that can have unique effects on cellular function and health outcomes. For example, the genes located in 1p12 have been associated with various medical conditions such as cancer, while the genes in 19p13.2 and 19p13.3 have been linked to developmental disorders and neurological conditions. The clinical relevance of each the cytogenetic location can vary depending on the genes and genetic variations present in that region. Although some genetic variations may be benign or have no known clinical significance, others can have significant effects on an individual’s health and disease risk. In this study, the interactive effects of the genes in the cytogenetic locations 1p12, 1q22, 19p13.2, and 19q13.3 were functionally enriched in reactome pathway and WikiPathway for better understanding of the pathways associated with PCOS (Table 2).
To identify the most important genes associated with PCOS with respect to their roles in the metabolic pathways associated with it, the STRING database was used to analyze the genes in Table 2 above, since they are known to be associated with PCOS. Specifically, there was an examination of the number, degree, and centrality of interactions among these genes, as well as the strength of the interactions. The information was then plotted bubble charts, to allow for easy visualization of the relative importance of each gene with respect to PCOS. Based on this analysis, there was identification of the top genes with the highest number of interactions (Fig. 1) and the three most important genes associated with PCOS (Fig. 2), which could serve as potential molecular targets for better understanding and therapeutic development for the condition.
Bubble chart depicting the degree of centrality of selected genes associated with PCOS phenotypes. The size of each bubble represents the relative count of network interactions for the corresponding gene, while the color indicates the significance level of the gene’s association with PCOS. The chart shows that HSD3B2 has the highest degree of centrality, followed by PPARG and LMNA, indicating that these genes have the most connections within the PCOS-associated gene network. Other genes, such as AMH, PPP1R3A, and PLIN1, also show significant associations with PCOS, albeit with lower degrees of centrality. The bubble chart provides an overview of the relative counts network connections of the selected genes in the PCOS-associated gene network, highlighting potential targets for further investigation
Bubble chart showing the degree of centrality and relative strength of network interactions for selected genes associated with PCOS phenotypes. The chart highlights the top three genes with the strongest connections as HSD3B2, PPARG, and LMNA, in descending order of strength. The size of each bubble represents the degree of centrality of the gene network, with larger bubbles indicating higher centrality. The chart provides an overview of the most important genes and their relationships in the context of PCOS
Polycystic ovary syndrome (PCOS) is a complex endocrine disorder affecting reproductive-age women worldwide. It is characterized by hormonal imbalances, ovarian dysfunction, and various metabolic disturbances. While the exact etiology of PCOS remains elusive, recent research has implicated several genes in its development and progression. Understanding the molecular pathways associated with PCOS and identifying potential therapeutic targets are crucial for the development of effective treatment strategies. In this study, part of efforts is to shed light on the intricate molecular mechanisms underlying PCOS by exploring the role of specific genes in the manifestation of PCOS phenotypic traits. The findings focus on the genes including HSD3B2, PPARG, PPP1R3A, LMNA, and AMH, which have emerged as potential candidates associated with PCOS pathogenesis (Figs. 1 and 2).
HSD3B2 (3β-hydroxysteroid dehydrogenase 2) is involved in the biosynthesis of androgens and plays a crucial role in steroid hormone metabolism. Studies have shown that mutations or dysregulation of HSD3B2 may lead to adrenal hyperplasia, resulting in the excessive production of androgens, a hallmark characteristic of PCOS. The gene has to with androgens and primarily testosterone, which is an essential sex steroid hormone produced in testicular Leydig cells in men and in adrenal cortex and ovaries in women. The gene could act through the androgen receptor to regulate gene transcription and exert rapid effects through interaction with membrane proteins or signaling molecules [43]. It has also been reported that the HSD3B1 gene encodes for 3βHSD1 protein affects DHEA metabolism and androgen synthesis, with the HSD3B1(1245C) allele resulting in greater androgen production and HSD3B1 (1245A) limiting it, leading to divergent outcomes in androgen-sensitive diseases [44]. It has also been reported that lower levels of HSD3B2 in adrenal reticularis facilitate DHEAS synthesis, contributing to increased androgen production during adrenarche and demonstrated by premature adrenarche in subject with a loss in HSD3B2 activity [45].
PPARG (peroxisome proliferator-activated receptor gamma) is a transcription factor that regulates lipid and glucose metabolism. Dysregulation of PPARG has been associated with severe insulin resistance, a common metabolic consequence observed in PCOS patients. Understanding the role of PPARG in PCOS may provide insights into the underlying mechanisms of insulin resistance and offer potential therapeutic avenues [46]. PPP1R3A (protein phosphatase 1 regulatory subunit 3A) is involved in glycogen metabolism and glucose homeostasis. Perturbations in PPP1R3A expression have been linked to abnormal glycogen storage and impaired glucose metabolism, which are prevalent in PCOS patients [47, 48]. Hence, exploring the role of PPP1R3A in PCOS could provide valuable insights into the metabolic dysregulation observed in affected individuals.
LMNA is a nuclear protein involved in maintaining nuclear structure and function, and mutations in the gene have been reported to be associated with various cardiomyopathies, including those seen in PCOS patients; hence, investigating the impact of LMNA mutations on cardiac function in PCOS may help elucidate the connection between PCOS and cardiovascular abnormalities [49, 50]. AMH (anti-Müllerian hormone) is a hormone secreted by the ovaries and has a crucial role in follicular development. Elevated AMH levels are frequently observed in PCOS, contributing to the characteristic follicular abnormalities and impaired ovulation. This situation necessitates an understanding of the molecular mechanisms underlying AMH dysregulation in PCOS and may provide insights into the disrupted ovarian function observed in affected individuals [51,52,53]. Therefore, by exploring the metabolic consequences associated with these genes, including adrenal hyperplasia, severe insulin resistance, carotid intimal-medial thickness, cardiomyopathy, and persistent type 1 Müllerian duct syndrome, it is possible to gain a comprehensive understanding of the molecular pathways implicated in PCOS. Furthermore, these findings could lead to identification of potential molecular targets for therapeutic development that could pave the way for more effective treatments for PCOS patients.
The identification of HSD3B2, PPARG, and LMNA as key genes associated with PCOS in this research holds significant implications for therapeutic intervention and the development of effective treatments. Understanding the molecular mechanisms regulated by these genes provides valuable insights into the underlying pathogenesis of PCOS and offers promising avenues for targeted therapeutic approaches. In this study, this exploration holds value for therapeutic intervention in dealing with genetic findings and their potential implications for PCOS management. HSD3B2, a crucial enzyme involved in androgen biosynthesis, emerged as a prominent gene in PCOS. Dysregulation of HSD3B2 can lead to adrenal hyperplasia and excessive androgen production, contributing to the characteristic symptoms of PCOS. Targeting HSD3B2 through pharmacological interventions or gene therapy holds promise for modulating androgen levels and mitigating PCOS-related symptoms. Inhibitors or modulators of HSD3B2 activity could help restore hormonal balance and alleviate hyperandrogenism, thereby improving reproductive outcomes and ameliorating associated metabolic disturbances.
Similarly, PPARG as a therapeutic target has potential roles because of its involvement in insulin resistance which is a hallmark feature of PCOS. Targeting PPARG and its downstream pathways may represent a viable therapeutic strategy for managing insulin resistance in PCOS patients. This could also facilitate identification of pharmacological agents which modulate PPARG activity, such as selective agonists or antagonists that can help in restoring insulin sensitivity, improve glucose metabolism, and address the metabolic consequences associated with PCOS. Furthermore, lifestyle interventions, including exercise and dietary modifications, can influence PPARG expression and activity, providing additional non-pharmacological approaches for therapeutic intervention.
Furthermore, LMNA as a therapeutic target could be contributing to treatment of cardiomyopathy, a significant metabolic consequence observed in PCOS which has been linked to mutations in the LMNA gene. Targeting LMNA and its associated pathways could have profound implications for managing cardiac abnormalities in PCOS patients. These strategies aimed at restoring normal LMNA function or modulating downstream signaling cascades could potentially ameliorate cardiomyopathy and reduce the risk of cardiovascular complications. Cardiac-specific interventions, including medications targeting specific pathways involved in LMNA-related cardiomyopathy, may prove beneficial in preserving cardiac function and improving the overall cardiovascular health of PCOS patients.
Collectively, targeting these identified genes and their specific pathways offers a multifaceted approach to therapeutic intervention in PCOS. This approach can also promote personalized medicine approaches, considering individual variations in genetic profiles and the specific molecular abnormalities present in each patient. Tailoring treatments based on the underlying genetic and molecular characteristics of PCOS holds promise for enhancing treatment efficacy and improving patient outcomes. However, it is important to note that therapeutic interventions based on these genetic findings are still in the early stages of development which required further research.
Findings in this study is relevant in the context of the guidelines of the International Federation of Gynaecology and Obstetrics (FIGO) whose focus is promotion and facilitation of education, clinical care, design, and interpretation of basic, translational, clinical, and epidemiological research for improvement of sexual and reproductive health of women [54]. The guideline identified that polycystic ovary syndrome (PCOS) is being experienced by up to 20% of reproductive-aged women worldwide, and ovulatory disorders are common causes of amenorrhea, abnormal uterine bleeding, and infertility. FIGO classified PCOS based on anatomical model focusing on hypothalamus, pituitary, and ovary (HyPO-P) into types 1, 2, 3, and 4 categories [55]. The classifications suggested that PCOS is of different cause and phenotypes which could include genetic, autoimmune, latrogenic, and neoplasm (type 1); functional, infectious, or inflammatory, trauma, and vascular (type 2); physiological, idiopathic and endocrine (type 3); and anovulation, clinical or biochemical hyperandrogenism, and polycystic ovaries on ultrasound (type 4) [55]. The categorization of PCOS into different types by the International Federation of Gynaecology and Obstetrics (FIGO) provides a comprehensive framework for understanding the diverse etiological factors and phenotypes associated with the complex syndrome (Fig. 3). Meanwhile, findings from this study highlight the significance of genes HSD3B2, PPARG, PPP1R3A, and AMH in the context of metabolic pathways and the identification of HSD3B2, PPARG, and LMNA as key genes in PCOS pathogenesis.
Graphical depiction of the proposed FIGO Ovulatory Disorders Classification System. The types 1, 2, or 3 disorders according to their primary source are hypothalamus, pituitary gland, or ovary, respectively. The PCOS type 4 category is the criteria including clinical, biochemical, hormones, and ultrasound findings [56]
The relationship between these findings and FIGO classification, focusing on their potential contributions to therapy for each PCOS category, is discussed as follows:
-
Type 1: This encompasses PCOS cases associated with genetic, autoimmune, iatrogenic, or neoplasmic causes. The identification of genes such as HSD3B2, PPARG, and LMNA is an important player in PCOS pathogenesis which aligns with the genetic component of type 1 PCOS. These genes have been implicated in various molecular pathways related to androgen biosynthesis, insulin resistance, and cardiomyopathy. Therapeutic strategies targeting these genes could potentially be beneficial in managing the underlying genetic abnormalities and associated clinical manifestations seen in this category of PCOS.
-
Type 2: This is characterized by factors such as functional issues, infectious or inflammatory processes, trauma, and vascular disturbances. While this present study does not specifically investigate the factors mentioned in type 2 PCOS, the molecular pathways regulated by genes like PPARG and PPP1R3A are associated with inflammation, glucose metabolism, and vascular health. Modulating the activity of these genes and downstream pathways of the genes could potentially contribute to addressing the underlying mechanisms contributing to functional, infectious/inflammatory, trauma, or vascular aspects of PCOS in type 2 cases.
-
Type 3: This encompasses cases where the etiology of PCOS is primarily physiological, idiopathic, or related to endocrine dysregulation. Although your research did not focus on these specific factors, the genes identified in your study, such as HSD3B2 and PPARG, play crucial roles in endocrine regulation, and their dysregulation may contribute to the development of PCOS. Therefore, therapeutic interventions targeting these genes and associated pathways could potentially address the physiological, idiopathic, or endocrine aspects of PCOS observed in type 3 cases.
-
Type 4: This is the PCOS cases characterized by anovulation, clinical/biochemical hyperandrogenism, and the presence of polycystic ovaries on ultrasound. The genes, HSD3B2, PPARG, and AMH, identified as central to the molecular pathways involved in PCOS in this present study are particularly relevant in this category. HSD3B2 and AMH have direct implications for androgen synthesis and follicular development, respectively, while PPARG affects insulin sensitivity and lipid metabolism. Therapies targeting these genes and associated pathways could potentially address the specific features of type 4 PCOS, including anovulation, hyperandrogenism, and ovarian morphology.
In summary, findings in this present study with respect to importance of genes including HSD3B2, PPARG, PPP1R3A, and AMH in PCOS pathogenesis align with the FIGO classification’s categorization of PCOS into different types. This is because these genes contribute to various molecular pathways associated with PCOS and could have potential roles in the targeted therapeutic approaches tailored toward addressing the underlying genetic and phenotypic characteristics of each PCOS category and could also lead to improved management and personalized treatment strategies for PCOS patients.
Conclusions
Polycystic ovary syndrome (PCOS) is a complex condition that affects many women worldwide. Although the exact causes of PCOS are not fully understood, research has shown that genetic factors play an important role. In this study, comprehensive analysis of metabolic pathways that are associated with PCOS was carried out to identify potential molecular targets for further research and therapeutic development. The analysis implemented revealed that HSD3B2, PPARG, PPP1R3A, and AMH had the highest number of interactions in relation to metabolic pathways reported with PCOS, indicating that these genes may be central to the molecular pathways involved in the development of PCOS. Furthermore, HSD3B2, PPARG, and LMNA emerged as the most important genes, suggesting that they could be playing key roles in regulating different aspects of PCOS pathogenesis. These findings suggest having important implications for future research into PCOS. By identifying these key genes and their associated pathways, this present study has provided valuable insights into the molecular mechanisms that underlie the complex condition PCOS.
Furthermore, these findings could serve as a basis for the development of novel therapeutic approaches that target these genes and their associated pathways. For example, future research could focus on developing drugs that target HSD3B2, PPARG, and LMNA, with the goal of regulating the metabolic and hormonal imbalances that contribute to PCOS. Alternatively, these genes could be targeted using gene therapy or other approaches that modify their expression or activity. In overall, this study provides important new insights into the genetic factors that contribute to PCOS and highlights the potential of targeting specific genes and pathways as a promising approach to developing effective treatments for this condition. Further research into these targets could lead to the development of novel and more effective therapies for PCOS, with the potential to improve the health and quality of life of millions of women around the world.
Availability of data and materials
Not applicable.
Abbreviations
- GWAS:
-
Genome-wide association studies
- EDCs:
-
Endocrine-disrupting chemicals
- CRP:
-
C-reactive protein
- DHEA-S:
-
Dehydroepiandrosterone sulfate
- CGDS:
-
Contiguous gene duplication or deletion syndrome
- PCOS:
-
Polycystic ovary syndrome
- OMIM:
-
Online Mendelian Inheritance in Man
- FPLD:
-
Familial partial lipodystrophy
- SDGs:
-
Sustainable development goals
References
Huttler A, Murugappan G, Stentz NC, Cedars MI (2023) Reproduction as a window to future health in women. Fertil Steril. https://doi.org/10.1016/j.fertnstert.2023.01.005
Omokanye LO, Ibiwoye-Jaiyeola A, Olatinwo OA, Abdul IF, Durowade KA, Biliaminu SA (2015) Polycystic ovarian syndrome: analysis of management outcomes among infertile women at a public health institution in Nigeria, Nigerian Journal of. Gen Pract 13:44–48
Seli E, Duleba AJ (2002) Optimizing ovulation induction in women with polycystic ovary syndrome. Curr Opin Obstet Gynecol 14:245–254. https://doi.org/10.1097/00001703-200206000-00002
Hiam M-A (2019) Teede, Laven, Stepto, Moran, Gibson-Helm, The genetics of polycystic ovary syndrome: an overview of candidate gene systematic reviews and genome-wide association studies, J. Clin Med 8:1606. https://doi.org/10.3390/jcm8101606
Dabravolski SA, Nikiforov NG, Eid AH, Nedosugova LV, Starodubova AV, Popkova TV, Bezsonov EE, Orekhov AN (2021) Mitochondrial dysfunction and chronic inflammation in polycystic ovary syndrome. Int J Mol Sci 22:3923. https://doi.org/10.3390/ijms22083923
van der Ham K, Louwers YV, Laven JSE (2022) Cardiometabolic biomarkers in women with polycystic ovary syndrome. Fertil Steril 117:887–896. https://doi.org/10.1016/j.fertnstert.2022.03.008
Dapas M, Dunaif A (2022) Deconstructing a syndrome: genomic insights into PCOS causal mechanisms and classification. Endocr Rev 43:927–965. https://doi.org/10.1210/endrev/bnac001
Pradhan J, Mishra I, Rattan R, Choudhury AK, Baliarsinha AK (2022) Correlation of markers of inflammation with hormonal, metabolic parameters, insulin resistance and adiposity indices in first-degree relatives of patient with polycystic ovary syndrome, Journal of Human Reproduction. Science 15:250–258
Barber TM (2022) Why are women with polycystic ovary syndrome obese? Br Med Bull 143:4–15. https://doi.org/10.1093/bmb/ldac007
Xu Y, Qiao J (2022) Association of insulin resistance and elevated androgen levels with polycystic ovarian syndrome (PCOS): a review of literature. J Healthc Eng 2022:1–13. https://doi.org/10.1155/2022/9240569
Kshetrimayum C, Sharma A, Mishra VV, Kumar S (2019) Polycystic ovarian syndrome: environmental/occupational, lifestyle factors; an overview. J Turk Ger Gynecol Assoc 20:255–263. https://doi.org/10.4274/jtgga.galenos.2019.2018.0142
Nasri F, Zare M, Hesampour F, Ahmadi M, Ali-Hassanzadeh M, Mostafaei S, Gharesi-Fard B (2022) Are genetic variations in IL-1β and IL-6 cytokines associated with the risk of pre-eclampsia? Evidence from a systematic review and meta-analysis. J Matern Fetal Neonatal Med 35:6600–6609. https://doi.org/10.1080/14767058.2021.1918092
Rani S, Chandna P (2023) Multiomics analysis–based biomarkers in diagnosis of polycystic ovary syndrome. Reprod Sci 30:1–27. https://doi.org/10.1007/s43032-022-00863-9
Jozkowiak M, Piotrowska-Kempisty H, Kobylarek D, Gorska N, Mozdziak P, Kempisty B, Rachon D, Spaczynski RZ (2022) Endocrine disrupting chemicals in polycystic ovary syndrome: the relevant role of the theca and granulosa cells in the pathogenesis of the ovarian dysfunction. Cells 12:174. https://doi.org/10.3390/cells12010174
Ananthasubramanian P, Ananth S, Kumaraguru S, Barathi S, Santosh W, Vasantharekha R (2021) Associated effects of endocrine disrupting chemicals (EDCs) on neuroendocrine axes and neurotransmitter profile in polycystic ovarian syndrome condition. Proc Zool Soc 74:378–386. https://doi.org/10.1007/s12595-021-00411-4
Panoutsopoulou K, Wheeler E (2018) Key concepts in genetic epidemiology, in: Genet Epidemiol:7–24. https://doi.org/10.1007/978-1-4939-7868-7_2
Li L, Petsch K, Shimizu R, Liu S, Xu WW, Ying K, Yu J, Scanlon MJ, Schnable PS, Timmermans MCP, Springer NM, Muehlbauer GJ (2013) Mendelian and non-Mendelian regulation of gene expression in Maize. PLoS Genet 9:e1003202. https://doi.org/10.1371/journal.pgen.1003202
Yu-Wai-Man P (2016) Genetic manipulation for inherited neurodegenerative diseases: myth or reality? Br J Ophthalmol 100:1322–1331. https://doi.org/10.1136/bjophthalmol-2015-308329
Cooper DN, Krawczak M, Polychronakos C, Tyler-Smith C, Kehrer-Sawatzki H (2013) Where genotype is not predictive of phenotype: towards an understanding of the molecular basis of reduced penetrance in human inherited disease. Hum Genet 132:1077–1130. https://doi.org/10.1007/s00439-013-1331-2
Alliance G (2010) Understanding genetics: a district of Columbia guide for patients and health professionals. Genetic Alliance; District of Columbia Department of Health, Washington, D.C.
Duncan RG, Castro-Faix M, Choi J (2016) Informing a learning progression in genetics: which should be taught first, Mendelian inheritance or the central dogma of molecular biology. Int J Sci Math Educ 14:445–472. https://doi.org/10.1007/s10763-014-9568-3
Bailey-Wilson JE, Wilson AF (2011) Linkage analysis in the next-generation sequencing era. Hum Hered 72:228–236. https://doi.org/10.1159/000334381
El Khoury D, Fayjaloun S, Nassar M, Sahakian J, Aad PY (2019) Updates on the effect of mycotoxins on male reproductive efficiency in mammals. Toxins (Basel) 11:515. https://doi.org/10.3390/toxins11090515
Fleming A, Abdalla EA, Maltecca C, Baes CF (2018) Invited review: reproductive and genomic technologies to optimize breeding strategies for genetic progress in dairy cattle. Arch Anim Breed 61:43–57. https://doi.org/10.5194/aab-61-43-2018
Huang M-T, Zhai P-M (2021) Achieving Paris Agreement temperature goals requires carbon neutrality by middle century with far-reaching transitions in the whole society. Adv Clim Chang Res 12:281–286. https://doi.org/10.1016/j.accre.2021.03.004
Li H, Yang Y, Hong W, Huang M, Wu M, Zhao X (2020) Applications of genome editing technology in the targeted therapy of human diseases: mechanisms, advances and prospects. Signal Transduct Target Ther 5:1. https://doi.org/10.1038/s41392-019-0089-y
Azziz R (2018) Polycystic ovary syndrome. Obstet Gynecol 132:321–336. https://doi.org/10.1097/AOG.0000000000002698
Amisi CA (2022) Markers of insulin resistance in polycystic ovary syndrome women: an update., World. J Diabetes 13:129–149. https://doi.org/10.4239/wjd.v13.i3.129
Hanson B, Johnstone E, Dorais J, Silver B, Peterson CM, Hotaling J (2017) Female infertility, infertility-associated diagnoses, and comorbidities: a review. J Assist Reprod Genet 34:167–177. https://doi.org/10.1007/s10815-016-0836-8
Barber TM, Hanson P, Weickert MO, Franks S (2019) Obesity and polycystic ovary syndrome: implications for pathogenesis and novel management strategies. Clin Med Insights Reprod Health 13:117955811987404. https://doi.org/10.1177/1179558119874042
Armanini D, Boscaro M, Bordin L, Sabbadin C (2022) Controversies in the pathogenesis, diagnosis and treatment of PCOS: focus on insulin resistance, inflammation, and hyperandrogenism. Int J Mol Sci 23:4110. https://doi.org/10.3390/ijms23084110
Olopaade J (2021) Can the pill cause polycystic ovary syndrome (PCOS)?, Healthline Media
Rudnicka E, Suchta K, Grymowicz M, Calik-Ksepka A, Smolarczyk K, Duszewska AM, Smolarczyk R, Meczekalski B (2021) Chronic low grade inflammation in pathogenesis of PCOS. Int J Mol Sci 22:3789. https://doi.org/10.3390/ijms22073789
Mohammadi S, KarimzadehBardei L, Hojati V, Ghorbani AG, Nabiuni M (2017) Anti-inflammatory effects of curcumin on insulin resistance index, levels of interleukin-6, C-reactive protein, and liver histology in polycystic ovary syndrome-induced rats. Cell J 19:425–433. https://doi.org/10.22074/cellj.2017.4415
Ostadmohammadi V, Jamilian M, Bahmani F, Asemi Z (2019) Vitamin D and probiotic co-supplementation affects mental health, hormonal, inflammatory and oxidative stress parameters in women with polycystic ovary syndrome. J Ovarian Res 12:5. https://doi.org/10.1186/s13048-019-0480-x
Whitham JC, Bryant JL, Miller LJ (2020) Beyond glucocorticoids: integrating dehydroepiandrosterone (DHEA) into animal welfare research. Animals 10:1381. https://doi.org/10.3390/ani10081381
Sam S, Dunaif A (2003) Polycystic ovary syndrome: syndrome XX? Trends Endocrinol Metab 14:365–370. https://doi.org/10.1016/j.tem.2003.08.002
Sesti G, Federici M, Hribal ML, Lauro D, Sbraccia P, Lauro R (2001) Defects of the insulin receptor substrate (IRS) system in human metabolic disorders. FASEB J 15:2099–2111. https://doi.org/10.1096/fj.01-0009rev
Li M, Chi X, Wang Y, Setrerrahmane S, Xie W, Xu H (2022) Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Signal Transduct Target Ther 7:216. https://doi.org/10.1038/s41392-022-01073-0
Jung U, Choi M-S (2014) Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci 15:6184–6223. https://doi.org/10.3390/ijms15046184
Kövesdi A, Patócs A (2019) Brief description of inheritance patterns. pp 21–27. https://doi.org/10.1007/978-3-030-25905-1_2
Cui H, Dhroso A, Johnson N, Korkin D (2015) The variation game: cracking complex genetic disorders with NGS and omics data. Methods 79–80:18–31. https://doi.org/10.1016/j.ymeth.2015.04.018
NaamnehElzenaty R, du Toit T, Flück CE (2022) Basics of androgen synthesis and action. Best Pract Res Clin Endocrinol Metab 36:101665
Naelitz BD, Sharifi N (2020) Through the looking-glass: reevaluating DHEA metabolism through HSD3B1 genetics. Trends Endocrinol Metab 31:680–690. https://doi.org/10.1016/j.tem.2020.05.006
Turcu A, Smith JM, Auchus R, Rainey WE (2014) Adrenal androgens and androgen precursors—definition, synthesis, regulation and physiologic actions. Compr Physiol, Wiley. pp. 1369–1381. https://doi.org/10.1002/cphy.c140006
Astarci E, Banerjee S (2009) PPARG (peroxisome proliferator-activated receptor gamma). Atl Genet Cytogenet Oncol Haematol 13:417–421
Shi H, SPD Senthil Kumar (2012) Sex differences in obesity-related glucose intolerance and insulin resistance, in: Glucose Tolerance, InTech. https://doi.org/10.5772/52972
Broekema MF, Savage DB, Monajemi H, Kalkhoven E (1864) Gene-gene and gene-environment interactions in lipodystrophy: lessons learned from natural PPARγ mutants. Biochim Biophys Acta Mol Cell Biol Lipids 2019:715–732. https://doi.org/10.1016/j.bbalip.2019.02.002
Varlet A-A, Desgrouas C, Jebane C, Bonello-Palot N, Bourgeois P, Levy N, Helfer E, Dubois N, Valero R, Badens C, Beliard S (2021) A rare mutation in LMNB2 associated with lipodystrophy drives premature cell senescence. Cells 11:50. https://doi.org/10.3390/cells11010050
Bagias C, Xiarchou A, Bargiota A, Tigas S (2020) Familial partial lipodystrophy (FPLD): recent insights. Diabetes Metab Syndr Obes 13:1531–1544. https://doi.org/10.2147/DMSO.S206053
Franks S, Hardy K (2020) What causes anovulation in polycystic ovary syndrome? Curr Opin Endocr Metab Res 12:59–65. https://doi.org/10.1016/j.coemr.2020.03.001
Broekmans FJ, Visser JA, Laven JSE, Broer SL, Themmen APN, Fauser BC (2008) anti-Müllerian hormone and ovarian dysfunction. Trends Endocrinol Metab 19:340–347. https://doi.org/10.1016/j.tem.2008.08.002
Dumont A, Robin G, Catteau-Jonard S, Dewailly D (2015) Role of anti-Müllerian hormone in pathophysiology, diagnosis and treatment of polycystic ovary syndrome: a review. Reprod Biol Endocrinol 13:137. https://doi.org/10.1186/s12958-015-0134-9
Aude L (2022) FIGO publishes a new ovulatory disorders classification system, Addressing the Global Challenge of Ovulatory Disorders
Munro MG, Balen AH, Cho S, Critchley HOD, Díaz I, Ferriani R, Henry L, Mocanu E, van der Spuy ZM (2022) The FIGO Ovulatory Disorders Classification System. Int J Gynecol Obstet 159:1–20. https://doi.org/10.1002/ijgo.14331
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ, Andersen M, Azziz R, Balen A, Baye E, Boyle J, Brennan L, Broekmans F, Dabadghao P, Devoto L, Dewailly D, Downes L, Fauser B, Franks S, Garad RM, Gibson-Helm M, Harrison C, Hart R, Hawkes R, Hirschberg A, Hoeger K, Hohmann F, Hutchison S, Joham A, Johnson L, Jordan C, Kulkarni J, Legro RS, Li R, Lujan M, Malhotra J, Mansfield D, Marsh K, McAllister V, Mocanu E, Mol BW, Ng E, Oberfield S, Ottey S, Peña A, Qiao J, Redman L, Rodgers R, Rombauts L, Romualdi D, Shah D, Speight J, Spritzer PM, Stener-Victorin E, Stepto N, Tapanainen JS, Tassone EC, Thangaratinam S, Thondan M, Tzeng C-R, van der Spuy Z, Vanky E, Vogiatzi M, Wan A, Wijeyaratne C, Witchel S, Woolcock J, Yildiz BO (2018) Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome†‡. Hum Reprod 33:1602–1618. https://doi.org/10.1093/humrep/dey256
Acknowledgements
Not applicable.
Funding
There is no funding support for this work.
Author information
Authors and Affiliations
Contributions
AS, MA, KA, HB, and GK contributed to this manuscript in the following ways. AS conceived the study, designed the experiments, and analyzed the data. MA critically revised the manuscript and provided intellectual input. KA performed literature search and contributed to writing. HB contributed to writing. GK contributed to the writing and data analysis. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sikiru, A.B., Adeniran, M.A., Akinola, K. et al. Unraveling the complexity of the molecular pathways associated with polycystic ovary syndrome (PCOS) and identifying molecular targets for therapeutic development: a review of literature. Middle East Fertil Soc J 28, 16 (2023). https://doi.org/10.1186/s43043-023-00142-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-023-00142-w