Abstract
Aim
To evaluate whether dietary pattern changes, antioxidant supplementation or 5–10% weight loss could improve disease activity (skin and joint) in patients with psoriatic arthritis (PsA).
Methods
A total of 97 PsA patients were enrolled in this 12-week randomized, double-blinded, placebo-controlled trial. Patients were randomized into three groups: Diet-placebo (hypocaloric diet + placebo supplementation); Diet-fish (hypocaloric diet + 3 g/day of omega-3 supplementation; and Placebo. Food intake (3-day registry, Healthy Eating Index (HEI), and the Dietary Inflammatory Index (DII)), body composition (whole-body dual-energy X-ray absorptiometry (DXA), weight and waist circumference) and disease activity (PASI, BSA, BASDAI, DAS28-ESR, DAS28-CRP and MDA) were evaluated at baseline and after the 12-week intervention. Statistical analysis used the intention-to-treat approach. The P value was considered to indicate significance when below 0.05.
Results
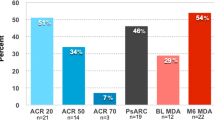
After 12 weeks, DAS28-CRP and BASDAI scores improved, especially in the Diet-placebo group (− 0.6 ± 0.9; p = 0.004 and − 1.39 ± 1.97; p = 0.001, respectively). In addition, a higher proportion of patients achieved minimal disease activity (MDA) in all groups. The Diet-fish group showed significant weight loss (− 1.79 ± 2.4; p = 0.004), as well as waist circumference (− 3.28 ± 3.5, p < 0.001) and body fat (− 1.2 ± 2.2, p = 0.006) reductions. There was no significant correlation between weight loss and disease activity improvement. Each 1-unit increase in the HEI value reduced the likelihood of achieving remission by 4%. Additionally, each 100-cal daily intake increase caused a 3.4-fold DAS28-ESR impairment.
Conclusion
A 12-week hypocaloric intervention provided suitable control of joint disease activity in patients with PsA, regardless of weight loss. Adding omega-3 supplementation caused relevant body composition changes but not disease activity improvement.
Trial Registration: The study was recorded on Clinicaltrials.gov (NCT03142503).
Similar content being viewed by others
Introduction
Psoriatic arthritis (PsA) is a chronic inflammatory disease that affects 20–33% of patients with psoriasis (Ps) [1]. The joint and skin outcomes are associated with multiple comorbidities, particularly metabolic syndrome (MetS), obesity, hypertension and diabetes [2]. These findings suggest a potential link between adiposity and Ps/PsA, highlighting a possible fat-joint-skin axis mediated by cells and proinflammatory cytokines, oxidative stress, dysbiosis and nutritional inadequacy [3].
More recently, it was demonstrated that an increased body mass index (BMI) caused a 50-fold greater likelihood of having PsA [4], as well as a lower chance of achieving disease remission [2] and worse response to pharmacological treatment, including a higher switching rate [2]. In addition, a significant association between disease activity and body composition measurements, such as a positive correlation with fat mass and a negative correlation with lean mass, has been reported [5]. Some studies have also shown weight gain after using tumor necrosis factor (TNF-α) blockers [6], suggesting that adjustments of these agents based on body weight are necessary to achieve a better drug response and lower toxicity [7].
Several nonpharmacological strategies, including weight loss and antioxidant supplementation, have had beneficial effects on obesity [8, 9], dyslipidemia [10, 11], nonalcoholic fatty liver disease [10] and diabetes [11]. However, only two controlled clinical trials evaluated the impact of weight loss on the disease activity of patients with PsA [7, 12]. Di Mino et al. [7] demonstrated that a 5 to 10% reduction in body weight increased the chance of disease remission, and Abou-Raya et al. [12] reported that the combination of a hypocaloric diet and exercise was a suitable intervention to improve PsA disease activity, depression and fatigue.
Based on the potential adjuvant effect of weight loss on the improvement of the clinical response of PsA patients, the aim of this study was to evaluate whether a dietary pattern change added to antioxidant supplementation or a 5–10% weight loss could improve the disease activity in patients with PsA, including skin and joint outcomes and inflammatory markers.
Methods
Study design and sampling
A sample of 85 patients was calculated based on an α error of 5% and β of 20% and was increased by 15% to minimize potential losses during follow-up. Thus, 97 patients aged 18 years or older with PsA, according to the Classification Criteria of Psoriatic Arthritis (CASPAR) [13], were enrolled in this 12-week randomized, double-blinded, placebo-controlled clinical trial (Fig. 1).
Patient disposition. Intent to treat analysis. CASPAR: ClASsification of Psoriatic Arthritis [13]
Patients with PsA were recruited from Sao Paulo’s Hospital (Sao Paulo, Brazil) and other rheumatology facilities (Heliopolis Hospital and Public State Hospital, Sao Paulo, Brazil) from September 2012 to May 2014.
Patients with gastrointestinal, endocrine, pulmonary, kidney, hepatic, and neuromuscular diseases; with an HIV-positive diagnosis; who were pregnant or breast-feeding, or who had a history of cancer were excluded. Patients taking anabolic steroids, protein supplements, vitamins, multivitamins, or antioxidants or who were allergic to fish and shellfish products were also excluded. Specific medications for PsA and physical activity were required to be stable for the 3 months prior to enrollment.
The study was approved by the Ethics Committee of Research at the Federal University of Sao Paulo (CAAE: 00591412.5.0000.5505) and was recorded on Clinicaltrials.gov (NCT03142503). Subjects were included in the study after signing an informed consent form, in accordance with the Declaration of Helsinki.
Randomization
Patients were equally randomized using randomizer.org into three different groups: Diet-Placebo—a hypocaloric diet plus placebo supplementation (1 g of soybean oil, 3 times a day); Diet-Fish—a hypocaloric diet plus omega 3 supplementation (362 mg of EPA and 242 mg of DHA, 3 times a day); and Placebo: 1 g of soybean oil 3 times a day and no dietary intervention. After 12 weeks, 91 patients completed the study, corresponding to 93.8% of the original sample (dropout rate = 6.2%) (Fig. 1). All tools and measurements, including food intake records, physical activity, disease activity, body composition, and lab tests, were analyzed before and after the 12-week intervention.
Dietary intervention
The patient diet was tailored, supervised and calculated by a well-trained nutritionist according to the nutritional needs, dietary habits, culture, socioeconomic level and routine of each individual patient. The diet for overweight and obese patients considered their basal metabolic rate [14] and included a 500-kcal restriction, as proposed by the Institute of Medicine [15, 16]. For eutrophic patients, the diet was calculated without a calorie restriction, aiming at maintaining their weight [15]. In both cases, macronutrients were divided into 45–65% carbohydrates, 10–35% proteins and 20–35% lipids [16], with reduced saturated fat (< 7% of daily caloric intake—DCI) and increased monounsaturated (20% of DCI) and polyunsaturated (6–10% of DCI) fats [17]. The omega-6:omega-3 ratio was 5:1, and cholesterol intake was lower than 300 mg a day [17]. Daily fiber consumption was 20–30 g [18].
All patients were instructed to make 3 main meals (breakfast, lunch and dinner), have 2 or 3 snacks between meals, and increase their intake of water, fruits and vegetables, avoiding processed foods.
In monthly meetings, the dietitian checked the patient’s diet adherence with a 24-h diet record and performed weight and waist circumference measurements. A brief anamnesis concerning concomitant drug use, current physical activity, sleep pattern, gut changes and side effects during the intervention was performed. Supplement exchange and pill count were also evaluated.
To ensure compliance with the nutritional intervention, patients were contacted monthly by e-mail or telephone. In addition, the nutritionist was available online throughout the intervention to clarify any doubts or complaints.
Patients who were not allocated to a diet group (Diet-Placebo or Diet-Fish) were counseled to maintain their habitual diet. After the 12-week intervention, a healthy diet was prescribed to these patients (placebo group).
Outcome measurements
To evaluate the activity and severity of PsA skin involvement, the psoriasis area severity index (PASI) [19] and body surface area (BSA) [20] were used. Joint assessment was performed using tools such as the disease activity score (DAS28-ESR and DAS28-CRP) [21]. Axial complaints were evaluated using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [22]. Functional capacity was evaluated using the health assessment questionnaire (HAQ) [23]. Minimal disease activity (MDA) was also used to identify patients in remission and assess the response to this particular intervention [24].
Three-day food records (3-DFR) were used to evaluate food intake. All subjects were asked to record their food and beverage intake for 3 days: 2 weekdays (alternate days) and one weekend day (Saturday or Sunday). Nutrient data were calculated using The Food Processor SQL – Professional Nutrition. Energy was adjusted using the residual method described by Willett and Stamper [25] in Analysis Software and Databases – ESHA Research, USA, 2010. To enhance the accuracy of nutritional data, the Diet Quality Index (DQI) [26] and Dietary Inflammatory Index (DII) [27] were also calculated.
Metabolic syndrome (MetS) was defined according to the Harmonization criteria [28], which assess the presence of dyslipidemia, hypertension, insulin resistance and central obesity as risk factors.
To analyze physical activity status, the International Physical Activity Questionnaire (IPAQ-short form) [29] and metabolic equivalents (METs) [29] were used. Patients were placed into the following categories: inactivity, minimal activity or health-enhancing physical activity, a high activity category.
Body composition measurements were assessed using dual-energy X-ray absorptiometry (DXA, GE-Lunar Radiation Corporation, DPX MD+, Madison, WI, USA) according to the standard protocol for acquisition and analysis suggested by the International Society Clinical Densitometry (ISCD). Measurements included total lean mass (kg), skeletal lean mass (kg), total and regional adipose tissue (kg e %), total bone mineral density (g/cm2), and bone mineral content (g). The coefficients of variation were 1.14%, 1.64%, 1.53%, 1.62%, 0.67%, and 1.72%, respectively [30]. To identify low appendicular lean mass (ALM), Baumgartner’s method was used for patients older than 50 years, and Rosetta’s method was used for those under 50 years old, according to sex [31]. The fat mass index (FMI) was calculated using the equation proposed by NHANES III, with reference values of 5–9 kg/m2 for females and 3–6 kg/m2 for males [32].
Statistical analysis
Descriptive statistics are expressed as the mean, standard deviation, and frequency (%).
The association between two categorical variables was verified using the chi-square test or, in cases of small samples, Fisher's exact test. The linear associations between two variables of numerical nature were evaluated by Pearson's correlation.
For the evaluation of the behavior of the means of the clinical variables at two time points per treatment group, analysis of variance (ANOVA) with repeated measures was used, with group as a fixed factor. ANOVA was used to analyze data with a normal distribution, which was verified using the Kolmogorov–Smirnov test. For nonnormally distributed data, the means of the groups at each time point were compared using the Kruskal–Wallis nonparametric test. The means of each group between time points were compared using the nonparametric Wilcoxon test.
The McNemar test was used to determine whether there were differences in a dichotomous dependent variable between two related groups with a continuous dependent variable.
The comparison of two means was performed using Student's t test. For nonnormally distributed data, the nonparametric Mann–Whitney test was used.
An intention-to-treat analysis was performed for all outcomes. To evaluate the simultaneous effects of sex, age, joint and cutaneous disease time, group (nutritional intervention) and capsule count, multiple linear regression was used. Logistic regression was used for dependent variables of a dichotomous nature (DAS28-VHS, DAS28-PCR and MDA classes). Linear regression presents normality as one of the assumptions. In all regression models, due to the large number of explanatory variables versus sample size, the variables whose associations with the dependent variable were significant at 10% in the univariate analysis were selected for the model. Initially, all the selected explanatory variables were included in the model, and then the variables that were nonsignificant at 5% were excluded one by one in order of significance (backward method). P values below 5% were considered indicative of significance. All data were analyzed using SPSS version 20.0.
Results
Age, sex, disease duration, body composition measurements, comorbidities, disease activity (joint and skin) and concomitant medications were similar between the groups at baseline (Table 1). There was a high prevalence of hypertension, diabetes, and overweight/obesity among the patients, regardless of intervention group. Normal BMI was observed in 12.1% of the placebo group, 19.4% of the diet-fish group and 15.6% of the diet-placebo group.
Most patients were physically inactive or minimally active, according to the IPAQ. Approximately 60% were postmenopausal women, and nearly 20% were taking hormone replacement therapy (data not shown).
After the 12-week nutrition intervention, all groups had a reduction in DAS28-CRP values (p = 0.004), although the Diet-placebo group showed a disease activity improvement nearly three times higher than that of the Placebo group. Considering only the skin outcome, there was no significant change. An MDA outcome was achieved for all groups (p = 0.006) (Table 2). Although not significant, the Diet-placebo group had a fourfold greater likelihood of improving the DAS28-ESR value than the Placebo group (exp B = 4.049).
There was no significant change regarding physical activity or therapy with disease-modifying antirheumatic drugs (DMARDs), including conventional synthetic and biologic agents, and medications related to metabolism, such as insulin, statins, and other antidiabetic drugs, after the 12-week intervention (Table 1). Although all groups had significant weight loss, only the Diet-fish group had body composition changes, including body fat, fat mass index and waist circumference reduction during the follow-up time. However, no relevant lean mass changes were observed. Surprisingly, only the Diet-placebo group showed a significant food intake improvement, as shown by a reduced DII value and decreased calorie (kcal/kg) and fat consumption (Table 3). In addition, there was no difference between the prescribed (1687.7 ± 339.6 kcal) and consumed (1737.8 ± 840.2 kcal) diets (p = 0.63) of patients in the diet intervention groups.
Interestingly, a dietary inflammatory pattern improvement was associated with higher micronutrient intake but not macronutrient consumption, except in the Diet-placebo group, which had a significant fat intake reduction. After the intervention, there was a significant increase in fiber, omega 3, vitamin B1, B2, B3, B6, B12 and vitamin D consumption. In addition, there was a significant reduction in the omega-6:omega-3 ratio. These changes directly impacted the decreased values of DII in all groups.
Although the greatest decreases in DII and DAS28-CRP scores were observed in the Diet-placebo group, there was no correlation between dietary changes and disease activity improvement. Nonetheless, each 100-cal increase led to a 3.4-fold increase in DAS28-ESR values (OR = 0.34; 95% CI 0.002–0.67; p = 0.039).
Regarding other outcomes, such as the DAS28-ESR score, it was found that the chance of continuing (from remission to remission) or achieving (from active disease to remission) joint remission was 5.5 times more likely for men (OR = 5.46; 95% CI 2.03–14.7; p = 0.001) than for women. Furthermore, each 1-unit increase in the HEI score decreased the likelihood of maintaining or achieving remission by 4% (OR = 0.96; 95% CI 0.92–1.0; p = 0.03).
Considering the disease activity outcomes, according to weight loss magnitude, there were no significant changes among the 3 groups after the 12-week diet intervention (Table 4 and Table 5). Additionally, no significant differences were observed in the following parameters: PASI, BSA, enthesitis and dactylitis count, and the number of swollen and painful joints (data not shown). Similarly, when the weight changes were equal to or greater than 5–10%, no disease activity improvement was observed (Table 5).
Importantly, at monthly meetings, the dietitian checked the patient’s diet and supplement adherence with a 24-h diet record and pill count, respectively. Intolerance and/or adverse events were monitored in all groups during the intervention. The adhesion of supplement intake (60–100%) was 69.7% in the Placebo group, 71.00% in the Diet-fish group and 69.7% in the Diet-placebo group. No adverse events were related to the dietary changes. Appetite reduction and eructation were the most commonly reported, especially in the Diet-fish group, but none of the adverse events were considered significant or caused discontinuation or dropout.
Discussion
The DIETA trial showed that a 12-week supervised nutritional intervention, including a 500-cal restriction, dietetic counseling and omega-3 supplementation, was effective in improving the disease activity and modifying the body composition measurements of patients with PsA. It is worth emphasizing that a hypocaloric diet plus omega-3 supplementation was more effective than a hypocaloric diet alone in promoting weight loss and fat mass and waist circumference reduction but had no extra beneficial effects on disease activity. In addition, our data suggested that increased energy intake and worse diet quality may negatively affect joint activity and reduce the likelihood of achieving disease remission, regardless of weight loss or body composition changes.
Our group previously reported a close relationship between body composition and disease activity in PsA patients. While fat mass was positively correlated with joint disease activity, lean mass was negatively associated with it, suggesting a possible harmful link between fat and joint disease activity. It was also observed that patients with severe joint disease activity had more bodily fat than patients in remission or with low disease activity [5].
Interestingly, all three groups had some clinical joint improvement, particularly the Diet-placebo group, with a 0.66 reduction in their DAS28-CRP scores, highlighting an early (12 weeks) moderate EULAR response [33], instead of the 24 weeks that would be expected in pharmacologic clinical trials [34]. Nonetheless, no significant skin changes were observed after three months of follow-up. The lack of a cutaneous response could be explained by low PASI and BSA values at baseline or chronicity of disease. Although we did have sufficient data regarding 68/66 joint counts to perform the DAPSA (Disease Activity in Psoriatic Arthritis), we obtained significant results using other instruments, including a nonspecific (DAS28-CRP) assessment and another more specific and more complete assessment of skin and articular outcomes (MDA) for PsA.
A recent meta-analysis demonstrated that obesity or overweight may decrease the chance of achieving remission or a low level of disease activity [35] in patients with rheumatic diseases, such as rheumatoid arthritis or PsA. According to Mok et al. [36], inflammation and oxidative stress can be a possible link between obesity and rheumatic diseases. This possibility has been previously described by the presence of multiple biomarkers of inflammation (C-reactive protein, sulfhydryl and hydroperoxide), such as those observed in obese individuals [37, 38] and PsA patients [39]. Thus, weight loss should be considered an important approach for managing patients with PsA, although we did not observe a relationship between weight loss and disease activity, as previously reported [2, 7]. According to Di Minno et al. [7], a weight loss of more than 5 or 10% would be sufficient to increase the probability of achieving MDA. In our study, we observed that few patients (10%) met this target, and improvements were more closely related to quality of diet than weight loss itself.
A recent study regarding bariatric surgery and other procedures to lose weight showed a significant incidence of PsA reduction after bypass but not after the gastric band, regardless of weight loss level [40]. The authors proposed that these findings may be related to changes in insulinotropic hormones, including glucagon-like pepitide-1 (GLP-1). GLP-1 contributes to weight loss and inflammatory marker reduction, such as tumor necrosis factor, which is essential for minimizing systemic inflammation and controlling PsA disease activity [40]. In addition, some studies have demonstrated that GLP-1 release and the regulation of energy homeostasis may be enhanced by nutrient intake (protein [41], omega3 [42], monounsaturated fatty acid [42] and fiber [42]) and reduced by higher carbohydrate consumption [43]. Although we did not observe any protein or carbohydrate intake changes, we hypothesized that the improved disease activity observed in the present study could have been influenced by GLP-1 release after DII reduction and increased fiber and omega-3 consumption, regardless of weight loss.
In addition to the reduced DII score, we showed that restricting energy consumption contributed to changes in relevant targets for decreasing one of the major triggers of MetS [44], which is closely related to PsA [45]. Recently, Leite et al. [5] reported that inadequate food consumption, including high total calorie intake, low antioxidant vitamin intake, a poor quality diet and a proinflammatory pattern, was common among patients with PsA and that there were associations between joint disease activity and fat intake and between skin activity and higher intake of trans fat and sodium. Our results confirm the ability of a hypocaloric diet to significantly improve the quality of nutrients and modulate articular activity, as demonstrated for each 1-unit increase in HEI values, which was related to a reduced likelihood of achieving remission in 4% of patients. Additionally, each 100-cal daily intake increase caused a 3.4-fold DAS28-ESR score impairment. Interestingly, the benefits observed in the Diet-placebo group were not improved by the addition of omega-3 present in fish oil.
Although omega-3 supplementation has not been shown to provide any extra benefits to disease activity, this fatty acid combined with hypocaloric diet counseling improved the adiposity of patients with excess visceral fat. Considering our best knowledge and a lack of information about omega-3 supplementation in PsA, our study was the first to evaluate the role of a dietetic approach, including this fatty acid, on disease activity in patients with PsA. Furthermore, omega-3 supplementation was associated with improved MetS parameters, such as dyslipidemia, hypertension and insulin resistance, as well as reduced waist circumference, body weight, obesity, pain and rates of nonalcoholic fatty liver disease [46]. We believe that these findings could be more relevant in longer clinical trials, as reported by Flachs et al., who noted some improvement in mitochondrial oxidation capacity, lipid metabolism and inflammation [47].
Importantly, it is already well established that nonpharmacologic interventions have a low rate of adherence. Therefore, a limitation of our results is not evaluating levels of omega-3 and its metabolites in plasma or cell membranes to avoid the information bias that has been amply described in food records [48], as well as a lack of information regarding DAPSA (Disease Activity in Psoriatic Arthritis). It is also very difficult to measure real food behavior and dietary changes because the provided information is subjective. Moreover, dietary patterns are closely linked to culture, habits, emotions and economic status, which makes it difficult to promote relevant and longer modifications [49]. Nevertheless, the adherence level was monitored at the dietitian’s monthly appointments, aiming to identify low adherence, complaints, and doubts about supplementation (adverse effects). Another limitation in the relatively short follow-up period for a chronic disease and reduced long-term compliance with the diet and supplements. Regardless of these points, this randomized clinical trial (RCT) has important relevance because it is the first RCT designed to assess the effectiveness of a supervised dietary intervention plus omega-3 fatty acid supplementation on disease activity in patients with PsA. In addition, no change in PsA, concomitant medications or physical activity was made during the 12-week intervention, reinforcing the role of diet in the context of immunometabolism.
Therefore, dietary counseling aimed at losing or controlling weight could be part of the global protocol for PsA patients. In addition, supervised exercises could contribute to weight loss, lean mass gain and better disease activity control.
Conclusion
A 12-week supervised nutritional intervention, including a 500-cal restriction, dietetic counseling, and omega-3 supplementation, was effective in improving the disease activity and body composition of patients with PsA, regardless of weight loss, but was related to food pattern and diet quality improvement. The DIETA trial, a nonpharmacologic approach, is an inexpensive, suitable, and efficient approach that could be combined with standardized drug therapy. The addition of omega-3 supplementation did not improve disease activity or inflammatory parameters but promoted relevant body composition changes that can be modulated by indirect pathways of disease activity.
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Change history
05 May 2022
In the online version of this article, there was a typo in the article title. The article has been updated.
References
Ranza R, Carneiro S, Qureshi AA, Martins G, Rodrigues JJ, Romiti R, Barros TB, Carneiro J, Sampaio AL, Grynszpan R, et al. Prevalence of psoriatic arthritis in a large cohort of Brazilian patients with psoriasis. J Rheumatol. 2015;42:829–34.
Gisondi P, Del Giglio M, Di Francesco V, Zamboni M, Girolomoni G. Weight loss improves the response of obese patients with moderate-to-severe chronic plaque psoriasis to low-dose cyclosporine therapy: a randomized, controlled, investigator-blinded clinical trial. Am J Clin Nutr. 2008;88:1242–7.
Davidovici BB, Sattar N, Prinz J, Puig L, Emery P, Barker JN, van de Kerkhof P, Stahle M, Nestle FO, Girolomoni G, Krueger JG. Psoriasis and systemic inflammatory diseases: potential mechanistic links between skin disease and co-morbid conditions. J Invest Dermatol. 2010;130:1785–96.
Love TJ, Zhu Y, Zhang Y, Wall-Burns L, Ogdie A, Gelfand JM, Choi HK. Obesity and the risk of psoriatic arthritis: a population-based study. Ann Rheum Dis. 2012;71:1273–7.
Leite BF, Morimoto M, Pinheiro MM, Genaro PS, Damasceno NRT. Food intake, metabolic profile and oxidative stress in pacients with Psoriatic Arthritis. Ann Nutr Metab. 2015;67(suppl 1):1–601.
Renzo LD, Saraceno R, Schipani C, Rizzo M, Bianchi A, Noce A, Esposito M, Tiberti S, Chimenti S. A DEL: Prospective assessment of body weight and body composition changes in patients with psoriasis receiving anti-TNF-alpha treatment. Dermatol Ther. 2011;24:446–51.
Di Minno MN, Peluso R, Iervolino S, Russolillo A, Lupoli R, Scarpa R, CaRRDs Study Group. Weight loss and achievement of minimal disease activity in patients with psoriatic arthritis starting treatment with tumour necrosis factor α blockers. Ann Rheum Dis. 2014;73(6):1157–62. https://doi.org/10.1136/annrheumdis-2012-202812.
Van Gemert WA, May AM, Schuit AJ, Oosterhof BY, Peeters PH, Monninkhof EM. Effect of weight loss with or without exercise on inflammatory markers and adipokines in postmenopausal women: the SHAPE-2 trial, a randomized controlled trial. Cancer Epidemiol Biomarkers Prev. 2016;25:799–806.
Polus A, Zapala B, Razny U, Gielicz A, Kiec-Wilk B, Malczewska-Malec M, Sanak M, Childs CE, Calder PC, Dembinska-Kiec A. Omega-3 fatty acid supplementation influences the whole blood transcriptome in women with obesity, associated with pro-resolving lipid mediator production. Biochim Biophys Acta. 2016;1861:1746–55.
He XX, Wu XL, Chen RP, Chen C, Liu XG, Wu BJ, Huang ZM. Effectiveness of omega-3 polyunsaturated fatty acids in non-alcoholic fatty liver disease: a meta-analysis of randomized controlled trials. PLoS ONE. 2016;11:e0162368.
Chen C, Yu X, Shao S. Effects of omega-3 fatty acid supplementation on glucose control and lipid levels in type 2 diabetes: a meta-analysis. PLoS ONE. 2015;10:e0139565.
Abou-Raya A, Abou-Raya S, Helmii M. OP0076 effect of exercise and dietary weight loss on symptoms and systemic inflammation in obese adults with psoriatic arthritis: randomized controlled trial. Ann Rheum Dis. 2014;73:89–90.
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum. 2006;54:2665–73.
World Health Organization. Human energy requirements. Rome: Food and Agriculture Organization; 2004.
Institute of Medicine. Dietary reference intakes: applications in dietary planning. Washington: National Academies Press; 2002.
Padovani RM, Amaya-Farfán J, Colugnati FAB, Domene SMÁ. Dietary reference intakes: aplicabilidade das tabelas em estudos nutricionais. Rev Nutr. 2006;19:741–60.
Santos RD, Gagliardi ACM, Xavier HT, Magnoni CD, Cassani R, Lottenberg AMP, Casella Filho A, Araújo DB, Cesena FY, Alves RJ, et al. I Diretriz sobre o consumo de gorduras e saúde cardiovascular. Arq Bras Cardiol. 2013;100:1–40.
Sposito AC, Caramelli B, Fonseca FAH, Bertolami MC, Afiune Neto A, Souza AD, Lottenberg AMP, Chacra AP, Faludi AA, Loures-Vale AA, et al. IV Diretriz Brasileira sobre Dislipidemias e Prevenção da Aterosclerose: Departamento de Aterosclerose da Sociedade Brasileira de Cardiologia. Arq Bras Cardiol. 2007;88:2–19.
Fredriksson T, Pettersson U. Severe psoriasis–oral therapy with a new retinoid. Dermatologica. 1978;157:238–44.
Henseler T, Schmitt-Rau K. A comparison between BSA, PASI, PLASI and SAPASI as measures of disease severity and improvement by therapy in patients with psoriasis. Int J Dermatol. 2008;47:1019–23.
Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–8.
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21:2286–91.
Ferraz MB, Oliveira LM, Araujo PM, Atra E, Tugwell P. Crosscultural reliability of the physical ability dimension of the health assessment questionnaire. J Rheumatol. 1990;17:813–7.
Coates LC, Helliwell PS. Validation of minimal disease activity criteria for psoriatic arthritis using interventional trial data. Arthritis Care Res (Hoboken). 2010;62:965–9.
Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124:17–27.
Bowman SA, Lino M, Gerrior SA, Basiotis PP. The Healthy Eating Index: 1994–96. US Department of Agriculture ed. Center for Nutrition Policy and Promotion;1998.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hebert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17:1689–96.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Fan M, Lyu J, He P. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ). 2005. http://www.IPAQ.ki.se.
Sousa M, Pinheiro MM, Szejnfeld VL, Castro CH. Body composition parameters in healthy Brazilian women differ from white, black, and Hispanic American women reference range. J Clin Densitom. 2013;16:360–7.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Kelly TL, Wilson KE, Heymsfield SB. Dual energy X-ray absorptiometry body composition reference values from NHANES. PLoS ONE. 2009;4:e77038.
van Gestel AM, Prevoo ML, van’t Hof MA, van Rijswijk MH, van de Putte LB, van Riel PL. Development and validation of the European League Against Rheumatism response criteria for rheumatoid arthritis. Comparison with the preliminary American College of Rheumatology and the World Health Organization/International League Against Rheumatism Criteria. Arthritis Rheum. 1996;39:34–40.
Helliwell PS, Kavanaugh A. Comparison of composite measures of disease activity in psoriatic arthritis using data from an interventional study with golimumab. Arthritis Care Res (Hoboken). 2014;66:749–56.
Lupoli R, Pizzicato P, Scalera A, Ambrosino P, Amato M, Peluso R, Di Minno MND. Impact of body weight on the achievement of minimal disease activity in patients with rheumatic diseases: a systematic review and meta-analysis. Arthritis Res Ther. 2016;18:297.
Mok CC, Ko GT, Ho LY, Yu KL, Chan PT, To CH. Prevalence of atherosclerotic risk factors and the metabolic syndrome in patients with chronic inflammatory arthritis. Arthritis Care Res (Hoboken). 2011;63:195–202.
Aronson D, Bartha P, Zinder O, Kerner A, Markiewicz W, Avizohar O, Brook GJ, Levy Y. Obesity is the major determinant of elevated C-reactive protein in subjects with the metabolic syndrome. Int J Obes Relat Metab Disord. 2004;28:674–9.
Aslan M, Horoz M, Sabuncu T, Celik H, Selek S. Serum paraoxonase enzyme activity and oxidative stress in obese subjects. Pol Arch Med Wewn. 2011;121:181–6.
Firuzi O, Fuksa L, Spadaro C, Bousova I, Riccieri V, Spadaro A, Petrucci R, Marrosu G, Saso L. Oxidative stress parameters in different systemic rheumatic diseases. J Pharm Pharmacol. 2006;58:951–7.
Egeberg A, Sorensen JA, Gislason GH, Knop FK, Skov L. Incidence and prognosis of psoriasis and psoriatic arthritis in patients undergoing bariatric surgery. JAMA Surg. 2017;152:344–9.
Caron J, Cudennec B, Domenger D, Belguesmia Y, Flahaut C, Kouach M, Lesage J, Goossens J-F, Dhulster P, Ravallec R. Simulated GI digestion of dietary protein: release of new bioactive peptides involved in gut hormone secretion. Food Res Int. 2016;89(Part 1):382–90.
Bodnaruc AM, Prud’homme D, Blanchet R, Giroux I. Nutritional modulation of endogenous glucagon-like peptide-1 secretion: a review. Nutr Metab. 2016;13:92.
Ingves S, Vilhelmsson N, Strom E, Fredrikson M, Guldbrand H, Nystrom FH. A randomized cross-over study of the effects of macronutrient composition and meal frequency on GLP-1, ghrelin and energy expenditure in humans. Peptides. 2017;93:20–6.
Mozaffarian D. Foods, obesity, and diabetes-are all calories created equal? Nutr Rev. 2017;75:19–31.
Wolk K, Sabat R. Adipokines in psoriasis: an important link between skin inflammation and metabolic alterations. Rev Endocr Metab Disord. 2016;17:305–17.
Leite BF, Jamar G, Caranti D. Effects of fatty acids on the metabolic syndrome: a literature review. Nutrire Rev Soc Bras Alim Nutr. 2014;39:112–29.
Flachs P, Ruhl R, Hensler M, Janovska P, Zouhar P, Kus V, Macek Jilkova Z, Papp E, Kuda O, Svobodova M, et al. Synergistic induction of lipid catabolism and anti-inflammatory lipids in white fat of dietary obese mice in response to calorie restriction and n-3 fatty acids. Diabetologia. 2011;54:2626–38.
Ortega RM, Perez-Rodrigo C, Lopez-Sobaler AM. Dietary assessment methods: dietary records. Nutr Hosp. 2015;31(Suppl 3):38–45.
Eertmans A, Baeyens F, Van den Bergh O. Food likes and their relative importance in human eating behavior: review and preliminary suggestions for health promotion. Health Educ Res. 2001;16:443–56.
Acknowledgements
Not applicable.
Funding
This study was supported by FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo) (Grants 2012/18701-2 and 2012/18789-7) and by CAPES.
Author information
Authors and Affiliations
Contributions
All authors equally contributed to this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Research at the Federal University of Sao Paulo (CAAE: 00591412.5.0000.5505) and was recorded on Clinicaltrials.gov (NCT03142503). Subjects were included in the study after signing an informed consent form, in accordance with resolution 466 from CONEP (Comissão Nacional de Ética em Pesquisa/National Committee of Ethics in Research; CNS/466) in 2012.
Consent for publication
We confirm that the data presented here have not been published elsewhere and that the article has not been submitted to any other journal. We give our consent for the publication of the article Dietetic IntervEntion in psoriaTic Arthritis: The DIETA trial.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leite, B.F., Morimoto, M.A., Gomes, C.M.F. et al. Dietetic intervention in psoriatic arthritis: the DIETA trial. Adv Rheumatol 62, 12 (2022). https://doi.org/10.1186/s42358-022-00243-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-022-00243-6