Abstract
Background
Although transcatheter arterial embolization for pseudoaneurysms is already well-established, ureteral artery pseudoaneurysm embolization is extremely rare. The present case shows a successful transcatheter arterial embolization for pseudoaneurysms in the ureteral branch of the renal artery due to ureteral invasion from gastric cancer.
Case presentation
A 57-year-old female presented with gross hematuria after treatments for poorly differentiated gastric adenocarcinoma. A contrast-enhanced computed tomography revealed pseudoaneurysms around the right ureter with a massive hematoma in the right ureter and bladder. The diagnosis was ureteral branch pseudoaneurysms resulting from possible retroperitoneal invasion due to pelvic lymph node metastasis of gastric cancer. Transcatheter arterial embolization was performed using gelatin particles, successfully controlling her hematuria without complications.
Conclusions
Ureteral branch artery embolization, although extremely rare, may be an effective and safe treatment option.
Similar content being viewed by others
Background
Urinary tract obstruction is an occasional complication in patients with gastric cancer [1]. Undifferentiated gastric cancer tends to spread and infiltrate along the vessels, nerves, and lymphatic without forming a mass [2]. Infiltration of the ureteral wall weakens the ureteral branch arterial wall, leading to pseudoaneurysm formation. Here, we present a case of ureteral branch pseudoaneurysm caused by possible ureteral invasion from gastric cancer without clear mass formation that was successfully treated by transcatheter arterial embolization (TAE). TAE is a common treatment for pseudoaneurysms, using various embolic materials such as coils, gelatin sponge, cyanoacrylate glue, ethanol sclerosant, and detachable balloons [3]. However, ureteral branch artery embolization has been reported in only one case [4].
Case presentation
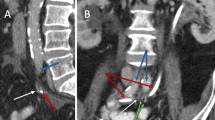
A 57-year-old female presented with gross hematuria. She underwent distal gastrectomy and ovarian resection for gastric cancer and bilateral ovarian metastases 11 years ago, with a pathological diagnosis of poorly differentiated adenocarcinoma. Adjuvant therapy with an oral fluoropyrimidine (S-1) was followed for about 1 year, but sigmoid colon metastasis was subsequently found. Five years prior to the embolization, she underwent sigmoid colon resection and received adjuvant S-1 therapy for one year. Three years after that, due to right extraperitoneal recurrence in the right pelvic wall, she underwent ileocecal resection with concomitant right ureter resection, right urethra-bladder anastomosis, partial rectal resection, and hysterectomy. Adjuvant therapy with S-1 plus docetaxel has been ongoing for 10 months. However, a recent computed tomography (CT) revealed a narrowed sigmoid colon due to peritoneal dissemination. As a result, a colostomy was created, and the patient's hematuria worsened after the operation. Subsequent CT imaging showed a massive hematoma in the right ureter and bladder, along with right hydronephrosis in the noncontrast phase (Fig. 1A and B). Pseudoaneurysms were detected around the right ureter in the arterial dominant phase (Fig. 2A and B) and in the volume-rendered image (Fig. 3).
Right femoral artery catheterization was performed under local anesthesia using the Seldinger technique. A 3-Fr diagnostic catheter (Hook type; Medikit; Tokyo, Japan; 65 cm) was inserted through a 3-Fr sheath and placed at the right renal artery. Renal arteriography showed the ureteral branch (Fig. 4A), and a 2.2/2.4-Fr microcatheter (Carnelian Marvel; Tokai Medical; Aichi, Japan; 135 cm) was advanced in the branch. The arteriography demonstrated multiple tiny pseudoaneurysms (Fig. 4B). Gelatin sponge particles were made by pumping it back and forth about 20 times using two syringes attached on a three-way stopcock [5]. The particles with size distribution of mainly < 1 mm [6] were used for the embolization. Postprocedural angiography revealed the disappearance of the pseudoaneurysms. Subsequently, right internal iliac arteriography was performed. Although aneurysms or extravasation were not clearly seen, the iliolumbar artery ran near the abovementioned aneurysms and was embolized using the gelatin sponge particles as well. The patient was discharged without any complications 10 days after the embolization. One month after the embolization, follow-up contrast-enhanced CT indicated no aneurysms or hematoma in the ureter and the bladder. However, her bone metastases and peritoneal dissemination were exacerbated, and her disease condition was uncontrollable. She died 5 weeks after the embolization.
Discussion
Gastric cancer can spread to the paraaortic area or pelvis, causing ureteral obstruction [7]. Ureteric involvement by metastatic diseases can occur through three different ways: direct invasion of the ureter by a tumor in a neighboring organ, metastasis to lymph nodes around the ureter resulting in retroperitoneal invasion, or distant metastasis [2, 7]. This case was considered to be close to the second scenario as the pseudoaneurysms were found adjacent to a soft-tissue shadow from the right common iliac lymph node metastasis. The retroperitoneal invasion could occur in terms of the trait that the undifferentiated gastric cancer would infiltrate without forming a mass; however, confirming it from the CT images was difficult [2]. However, there are no reports addressing ureteral branch aneurysm due to retroperitoneal invasion, and TAE for the ureteral branch is extremely rare. To the best of our knowledge, there is only one study by Kase et al. [4], who successfully performed embolization using coils and Abiten® for the ureteral branch from the renal artery without complications after an injury caused by cystoscopic removal of a Double-J stent.
The ureteral branches derive from multiple arteries [8]. The upper part receives its blood supply from a branch of the renal artery, while the middle part is supplied by branches from the common iliac arteries, the abdominal aorta, and the gonadal arteries. The most distal part receives blood from branches of the superior and inferior vesicular arteries. The blood supply of the ureter is segmental through these branches, which anastomose on the adventitia covering its wall [9]. Gelatin sponge particles could be safer than others, considering that the distance between the tip of the microcatheter and the pseudoaneurysm was a bit far. Highly diluted N-butyl-2- cyanoacrylate (NBCA) is required due to the long distance in NBCA cases. However, highly diluted NBCA would impede the collaterals due to distant traveling, thereby causing ischemia. Conversely, coil placement would be too near. It has the possibility of recanalization through the anastomose.
Conclusions
Ureteral branch artery embolization is rare but may be an effective and safe procedure.
Availability of data and materials
Not applicable.
Abbreviations
- TAE:
-
Transcatheter arterial embolization
- CT:
-
Computed tomography
References
Boubaker K, Alkadi M, Fitouri O, Ali Rahil AI, Al Malki H. An unusual case of acute kidney injury caused by obstructive uropathy revealing gastric cancer. Qatar Med J. 2022;2022:15.
Saida Y, Tsunoda HS, Matsueda K, Kurosaki Y, Kuramoto K. Gastric cancer and obstructive uropathy. Nihon Igaku Hoshasen Gakkai Zasshi. 1990;50:390–7. [in Japanese].
Lee JH, Hwang DW, Lee SY, Hwang JW, Song DK, Gwon DI, et al. Clinical features and management of pseudoaneurysmal bleeding after pancreatoduodenectomy. Am Surg. 2012;78:309–17.
Kase DJ, Crystal KS, Naidich JB, Badillo FL, Waldbaum RS. Embolization to control iatrogenic ureteral hemorrhage: a case report. J Urol. 1994;151:420–1.
Saiga A, Yokota H, Higashide T, Takishima H, Omoto A, Kubota Y, et al. The relationship between gelatin sponge preparation methods and the incidence of intrauterine synechia following uterine artery embolization for postpartum hemorrhage. Cardiovasc Intervent Radiol. 2019;42:195–204.
Katsumori T, Kasahara T. The size of gelatin sponge particles: differences with preparation method. Cardiovasc Intervent Radiol. 2006;29:1077–83.
Liaw CC, Chuang CK, Chen JS, Chang HK. Gastric cancer with obstructive uropathy: clinical experience with 17 cases. Changgeng Yi Xue Za Zhi. 1997;20:286–92.
Chaudhry SR, Liman MN, Peterson DC. Anatomy, abdomen and pelvis, stomach. In: StatPearls. Treasure Island: StatPearls Publishing; 2022.
Jacob S. Chapter 4 - Abdomen. In: Jacob S, editor. Human Anatomy: Churchill Livingstone; 2008. p. 71–123.
Acknowledgements
Not applicable.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
AS, TA, RS, and KA contributed to the design and implementation of the research, to the analysis of the results. HG created the volume-rendered image. AS was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Consent for publication was obtained for the individual person’s data included in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saiga, A., Aramaki, T., Sato, R. et al. Embolization of pseudoaneurysms in the ureteral branch of the renal artery. CVIR Endovasc 6, 51 (2023). https://doi.org/10.1186/s42155-023-00400-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42155-023-00400-y







