Abstract
Background
Fine-needle aspiration cytology (FNAC) of the breast is a well-established technique that aids in the preoperative identification and differentiation between nonneoplastic and neoplastic breast lesions. Breast lesions can be efficiently categorized into different cytological groups using the International Academy of Cytology (IAC) Yokohama System. The aim of this study was to classify breast lesions based on the proposed Yokohama system of reporting breast cytology and identify the need for a unified system of reporting breast lesions.
Materials and methods
This retrospective descriptive study was performed in the Department of Pathology, Government Medical College, Datia, M.P. from January 2019 to June 2023. A total of 762 FNAC slides reported during this period were retrieved, re-examined and reclassified according to the IAC Yokohama System. Histopathological diagnoses were also retrieved and correlated with the cytological findings wherever available.
Results
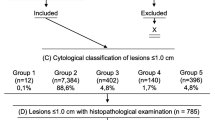
In the present study, a total of 762 smears of breast fine needle aspirations were included and categorized using the IAC Yokohama System. There were 3.8% cases (29/762) in the C1 category (insufficient), 71.6% cases (545/762) in the C2 category (benign), 6.3% cases (48/762) in the C3 category (atypical), 3.1% cases (24/762) in the C4 category (suspicious for malignancy) and 15.2% (116/762) cases in the C5 category (malignant).
Conclusion
FNAC is a reliable diagnostic technique for the evaluation and management of breast lesions prior to surgery. Implementing the IAC Yokohama System for reporting breast cytopathology enhances the accuracy of diagnosing breast lesions, reduces missed diagnoses, and offers reliable estimates of risk of malignancy. Adopting the Yokohama system is a crucial first step in boosting the overall effectiveness of breast cytology reporting among clinicians and pathologists, which will ultimately lead to improved communication and patient care.
Similar content being viewed by others
Introduction
Breast carcinoma is the most common cancer in females worldwide. As per the Globocan data 2020, in India, breast carcinoma accounted for 13.5% of all cancer cases and 10.6% of all deaths with a cumulative risk of 2.81 (Mehrotra and Yadav 2022). The three primary methods used for diagnosing breast masses are clinical examination, radiographic imaging, and breast cytopathology with or without core needle biopsy (CNB). These techniques seek to increase the preoperative detection of cancer so that the patient can receive early, conclusive, one-stage surgery or other suitable treatment (Field 2017; Singh and Wells 2001). When used with ultrasound guidance for both palpable and impalpable lesions, fine needle aspiration cytology (FNAC) is a rapid, minimally invasive, trustworthy, and economical breast biopsy method with a long history of success (Field and Zarka 2016; Dong et al. 2016; Farras Roca et al. 2017). The FNAC direct smear rates of insufficient samples and anomalous or suspicious samples are decreased by rapid on-site evaluation (ROSE). Additionally, ROSE enables immediate triage of lesions depending on the findings of FNA. The International Academy of Cytology (IAC) Breast Group was established in 2016 at the Yokohama International Congress of Cytology with the intention of creating a globally acknowledged and standardized reporting system that would define best practice guidelines for the use of FNAC in more consistently and accurately diagnosing breast lesions (Field et al. 2017). Five distinct categories for breast FNAC have been defined by the system and stratified based on the associated risk of malignancy (ROM) and provided recommendations for further management for each category (Field et al. 2017; Ahuja and Malviya 2021). The categories defined under the Yokohama system include the following:
C1- Insufficient
C2- Benign
C3- Atypical
C4- Suspicious for malignancy
C5- Malignant.
The present study aims to classify breast FNAs according to the IAC Yokohama system and evaluate the risk of malignancy (ROM), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy of different categories.
Materials and methods
The present study was a retrospective observational study performed in the Department of Pathology, Government Medical College, Datia, M.P. Ethical clearance was obtained from the Institutional Ethical Committee. All FNACs performed for breast lumps between January 2019 and June 2023 were included in the study, which accounted for a total of 762 patients. Breast lumps in lactating females or patients presenting with only nipple discharge without breast lumps were excluded from the study. FNAC of the breast lump was performed by a trained pathologist after taking written informed consent of the patient using a 22–23 gauge needle with 20 ml disposable syringe under aseptic conditions. Ultrasound-guided FNAC was performed in small or deeper inaccessible breast lumps, or breast lumps with cystic and necrotic components. The smears prepared on glass slides were air-dried or fixed in 95% ethyl-alcohol and stained in Giemsa stain and Pap stain. Slides thus prepared were examined by three cytopathologists and reported following the standard criteria in the IAC Yokohama Reporting System for Breast Cytology.
The corresponding histopathological diagnosis, which was considered the gold standard, was available in 321 cases. The cases with both cytological and histological diagnoses were divided into 3 groups, namely group A, group B and C, for proper statistical analysis. Group A included the scenario in which only the “malignant” cases on cytology were considered as positive, group B included the scenario in which “malignant” and “suspicious of malignancy” category on cytology were regarded as positive, whereas group C presented a scenario in which cases in the “malignant,” “suspicious of malignancy,” and “atypical” categories on cytology were regarded as positive as shown in Table 1.
The ROM for each category was calculated as the percentage of confirmed malignant cases in each category to the total number of cases in that category. For each of the three groups (A, B, C), the sensitivity, specificity, PPV, NPV and diagnostic accuracy of FNAC for the diagnosis of breast lesions were evaluated using the standard formulae.
The cyto-histological concordance (CHC) was also calculated in the present study to study the concordance and discordance of the interpretation and to evaluate errors in the cytological screening. Pairs with an exact agreement were designated as an agreement (Raju et al. 2019).
Results
A total of 762 breast FNAC smears were included in the study. The age group of patients ranged from 18 years to 74 years, with the majority of cases belonging to the age group between 25 and 45 years (67.2%). The smears were categorized under 5 categories from C1 to C5. There were 3.8% cases (29/762) in the C1 category (insufficient), 71.6% cases (545/762) in the C2 category (benign), 6.3% cases (48/762) in the C3 category (atypical), 3.1% cases (24/762) in the C4 category (suspicious for malignancy) and 15.2% (116/762) cases in the C5 category (malignant).
Histopathological correlation was performed in 321 cases (42.12%), which were further categorized as benign and malignant breast lesions. Out of the 321 cases, 70.4% (226/321) of the cases were benign on histopathological examination, whereas 29.6% (95/321) were malignant (Table 2). The most common benign lesion on histopathology was fibroadenoma in 81.4% of cases (184/226), whereas the most common malignant lesion was infiltrating breast carcinoma of no special type in 82.1% of cases (78/95) as shown in Fig. 1.
Cytological and histopathological photomicrographs of common breast lesions with cyto-histological concordance: (A) May Grunwald-Giemsa stained smear shows cohesive clusters of benign ductal epithelial cells with few bipolar nuclei- Category 2 [400x magnification] (B) Hematoxylin and Eosin stained section- Intracanalicular Fibroadenoma [400x magnification] (C) May Grunwald-Giemsa stained smear shows loose clusters of atypical ductal epithelial cells with nuclear enlargement and absence of myoepithelial cells- Category 5 [400x magnification] (D) Hematoxylin and Eosin stained section- Invasive carcinoma breast [400x magnification]
Risk of malignancy was calculated for each cytological category, which was maximum for C5 (100%), followed by C4 (75%), and C3 (19.04%). ROM was only 1.02% in C2 category whereas it was 16.6% in C1, which could be explained by the fact that high-grade malignant lesions can present with vast areas of necrosis and hemorrhage accounting for the unsatisfactory smears. The ROM for various categories is represented in Table 2.
87.9% of the cases (282/321) showed total concordance with the cytological and histological diagnosis, whereas 12.1% cases showed disagreement between the cytological and histological diagnosis (Table 2).
Statistical analysis was performed in each of the three groups to estimate the efficacy of the IAC Yokohama system. Sensitivity and specificity in group A was 82.10% and 100% respectively, which was 91.5% and 98.67% in group B and 95.78% and 90.29% in group C respectively. The sensitivity increased as the cases of suspicious for malignancy and atypical breast lesions were also considered as positive whereas the specificity decreased. Maximum sensitivity for the diagnosis of malignant lesions was achieved in Group C; however, the specificity decreased. Similarly, the PPV also increases if only confirmed cases, i.e. category C5 were included as positive results, as in group A (100%), followed by group B (96.67%) and group C (81.98%). Additionally, the diagnostic accuracy was maximum in Group B. (Table 3).
Discussion
One of the most commonly performed FNAs worldwide is breast FNAC and is a highly investigation for both palpable and impalpable lesions (Wong et al. 2019). The technique is minimally invasive, rapid, and cost-effective and can be used efficiently in the outpatient and limited-resource settings. The Yokohama system provides a five-tiered system with uniform terminology for better communication between clinicians and pathologists, better reproducibility of reports between different institutions and stratification of patients according to the risk of malignancy to improve the overall management of the patients (Smith et al. 2012).
The present study observed high efficacy of FNAC for the diagnosis of breast lumps even with limited resources, without the application of expensive and invasive methods. FNAC also proved to be a good test for rapid onsite evaluation of breast lumps which reduces the turn-around time for the diagnosis. Also, FNAC can provide enough material for the application of ancillary tests such as immunochemical analysis and molecular testing.
In the present study, 762 breast FNAC smears were studied, and the results were interpreted based on the IAC Yokohama system for reporting of breast cytopathology. In the present study, most of the cases fell under the benign category (C2-71.6%) on cytological examination and there were 15.2% cases in the malignant category (C5). Similar results were obsereved by studies done by Kamatar P et al. (Kamatar et al. 2019), Apuroopa M et al. (Apuroopa et al. 2020), Shankar M et al. (Shankar et al. 2023), and Guru A et al. (Guru et al. 2023). In the present study there were 6.3% cases in the atypical category (C3), which was much lower when compared to the studies done by Apuroopa M et al. (Apuroopa et al. 2020) and Shankar M et al. (Shankar et al. 2023). This difference could be due to observer variability or due to over-reporting of few cases of benign breast disease as atypical or technical fault during the processing of the smears (Table 4).
The risk of malignancy (ROM) for each category in the present study was 16.6%, 1.02%, 19.04%, 75% and 100% in categories C1, C2, C3, C4 and C5, respectively. The ROM was comparable to the studies by Wong S et al. (Wong et al. 2019), Apuroopa M et al. (Smith et al. 2012) and Ahuja S et al. (Ahuja and Malviya 2021). However, Agarwal A et al. (Agarwal et al. 2021) estimated ROM as 60.9% in category C1, which is discordant with the present study. This may be due to improper sampling resulting in higher number of cases falling under the unsatisfactory or non-diagnostic category (C1). This error can be avoided by instilling a proper technique of sampling by a trained personnel or using ultrasound guidance to aid the FNAC procedure. This result is higher than that in the present study, which could be due to sampling errors or technical errors leading to errors in interpretation (Table 5).
Raju K et al. (Raju et al. 2019) conducted a study to estimate the CHC of gynaecological and non-gynaecological samples in their institute and the concordance rate in their study was 86.97% cases, which was 87.9% in the present study. However, organ-wise discordant cases for breast in the mentioned study was 28%, which is much higher than the present study (12.1%), which could be accounted for the very small sample size in comparison to the present study.
In the present study, the sensitivity in group A was 82.1% when only malignant cases were included in positive test results, which increased further in group C (95.7%) when atypical, suspicious, and malignant cases were considered positive test results. Similar results were achieved by Wong S et al. (Wong et al. 2019), Montezuma D et al. (Montezuma et al. 2019) and Ahuja S et al. (Raju et al. 2019). However, specificity, which is the ability of a test to identify people who don’t have the disease, was higher in group A, which included only malignant cases (100%), and decreased further in group C when atypical and suspicious for malignancy were also considered positive results. This decrease in the specificity is observed since some cases diagnosed as atypical or suspicious on cytology were found to be benign on histology (Table 6; Fig. 2).
Cytological and histopathological photomicrographs of breast lesion with cyto-histological discordance: (A) May Grunwald-Giemsa stained smear shows loosely cohesive clusters of ductal epithelial cells showing mild nuclear pleomorphism and atypia- Category 3 [400x magnification] (B) Hematoxylin and Eosin stained section- showing benign looking breast lobules along with well-formed granulomas composed of multinucleated giant cells, lymphovytes and plasma cells- suggestive of Benign breast disease: Granulomatous Mastitis [400x magnification]
The specificity and PPV in the third scenario (group C) was found to be quite in disagreement with the previous studies. The present study observed a high specificity (90.2%) in group C when compared with the studies done by Wong S et al. (Wong et al. 2019) (62.1%), Montezuma D et al. (Montezuma et al. 2019) (54.8%) and De Rosa F et al. (Rosa et al. 2020) (56.3%), which may be due the fact that they reported a higher proportion of cases in the atypical and suspicious for malignant category on cytology that turned out to benign on histopathological examination. The PPV of the present study (81.9%) was also discordant with the results of Montezuma D et al. (Montezuma et al. 2019) (49.2%) and De Rosa F et al. (Rosa et al. 2020) (30.5%). PPV represents the proportion of true positives amongst the total positive cases on FNAC. Higher PPV indicates that the proportion of false positives detected by the screening test is low, which is true in our study and the studies done by Wong S et al. (Wong et al. 2019) (71.7%) and Ahuja S et al. (Ahuja and Malviya 2021) (77%) (Table 6).
The diagnostic accuracy in the present study was maximum in group B (96.5%) when malignant and suspicious cases were included in positive results. These results were comparable to the studies performed by Wong S et al. (Wong et al. 2019), Montezuma D et al. (Montezuma et al. 2019), De Rosa F et al. (Rosa et al. 2020) and Ahuja S et al. (Ahuja and Malviya 2021), as shown in Table 6.
Conclusion
Breast FNAC is a reliable test for diagnosing breast lesions, especially malignant breast lesions. Sensitivity, specificity, negative predictive value, positive predictive value, and diagnostic accuracy were all statistically significant in this investigation. Utilizing the IAC Yokohama breast cytology reporting system then aids in standardizing reporting across numerous institutes and stratifying cases according to the risk of malignancy to guide clinicians for appropriate follow-up management.
Data availability
All the data used in the present study is available in the departmental records in Government Medical College, Datia, M.P. All data generated or analysed during this study are included in this published article [and its supplementary information files]. The datasets generated during and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Agarwal A, Singh D, Mehan A, Paul P, Puri N, Gupta P, et al. Accuracy of the International academy of cytology Yokohama system of breast cytology reporting for fine needle aspiration biopsy of the breast in a dedicated breast care setting. Diagn Cytopathol. 2021;49:195–202.
Ahuja S, Malviya A. Categorization of breast fine needle aspirates using the International Academy of Cytology Yokohama System along with Assessment of Risk of Malignancy and Diagnostic Accuracy in a Tertiary Care Centre. J Cytol. 2021;38(3):158–63.
Apuroopa M, Chakravarthy VK, Rao DR. Application of Yokohama system for reporting breast fine needle aspiration cytology in correlation with histopathological and radiological findings. Annals Pathol Lab Med. 2020;7:A210–5.
De Rosa F, Migliatico I, Vigliar E, Salatiello M, Pisapia P, Iaccarino A, et al. The continuing role of breast fine-needle aspiration biopsy after the introduction of the IAC Yokohama system for reporting breast fine needle aspiration biopsy cytopathology. Diagn Cytopathol. 2020;48:1244–53.
Dong J, Ly A, Arpin R, Ahmed Q, Brachtel E. Breast fine needle aspiration continues to be relevant in a large academic medical center: experience from Massachusetts General Hospital. Breast Cancer Res Treat. 2016;158(2):297–305.
Farras Roca JA, Tardivon A, Thibault F, El Khoury C, Alran S, Fourchotte V, et al. Diagnostic performance of ultrasound-guided fine-needle aspiration of nonpalpable breast lesions in a multidisciplinary setting: the institut curie’s experience. Am J Clin Pathol. 2017;147(6):571–9.
Field AS. Breast FNA biopsy cytology: current problems and the International Academy of Cytology Yokohama standardized reporting system. Cancer Cytopathol. 2017;125(4):229–30.
Field AS, Zarka MA. Practical cytopathology: a Diagnostic Approach E-Book: a volume in the Pattern Recognition Series. Elsevier Health Sciences; 2016.
Field AS, Vielh P, Schmitt F. IAC standardized reporting of breast FNA biopsy cytology. Acta Cytol. 2017;61:3–6.
Guru A, Sutrakar SK, Jatav J, Tripathi L, Singh UR, Gupta R, et al. Validation of the IAC Yokohama system for reporting breast fine-needle aspiration cytology categorization of breast lesions in Vindhya region population. Asian J Med Sci. 2023;14(5):161–6.
Kamatar P, Athanikar V, Dinesh US. Breast fine needle aspiration biopsy cytology peporting using international academy of cytology Yokohama system-two year retrospective study in tertiary care center in Southern India. Natl J Lab Med. 2019;8:PO01–3.
Mehrotra R, Yadav K. Breast cancer in India: Present scenario and the challenges ahead. World J Clin Oncol. 2022;13(3):209–18.
Montezuma D, Malheiros D, Schmitt FC. Breast fine needle aspiration biopsy cytology using the newly proposed IAC Yokohama system for reporting breast cytopathology: the experience of a single institution. Acta Cytol. 2019;63:274–9.
Raju K, Sunanda M, S., Shree Rajanna V. Cytology-histology correlation of gynecologic and non-gynecologic samples at a tertiary health care center: a two-year study. Biomedical Res Therapy. 2019;6(4):3096–106.
Shankar M, Singh M, Sugandha S. Evaluation of applicability of Yokohama system for reporting of breast fine needle aspiration cytology: a retrospective study in a tertiary care center. Int J Adv Res. 2023;11(1):732–7.
Singh N, Wells CA. Assessment of accuracy in breast cytology. Cytopathology. 2001;12(4):211–8.
Smith MJ, Heffron CC, Rothwell JR, Loftus BM, Jeffers M, Geraghty JG. Fine needle aspiration cytology in symptomatic breast lesions: still an important diagnostic modality? Breast J. 2012;18(2):103–10.
Wong S, Rickard M, Earls P, Arnold L, Bako B, Field A. The IAC Yokohama System for reporting breast FNAB cytology: a single institutional retrospective study of the application of the system and the impact of ROSE. Acta Cytol. 2019;63:280–91.
Acknowledgements
The Authors would like to thank all the technical and non-technical staff in Department of Pathology and Surgery, Government Medical College Datia, MP for their co-operation and co-ordination throughout the study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
RY: data collection and preparation of manuscript. NS: Conceputalisation and Preparation of manuscript. MB: Statistical analysis, interpretation and preparation of manuscript. AB: Statistical analysis, interpretation and preparation of manuscript. AS:Preparation and Revision of manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Ethical Committee at Government Medical College, Datia, MP before commencing the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yadav, R., Singh, N., Bakna, M. et al. Cytomorphological spectrum of breast fine needle aspiration cytology using the International Academy of Cytology Yokohama System and evaluation of associated risk of malignancy–A retrospective study in a tertiary care cente. Surg Exp Pathol 7, 6 (2024). https://doi.org/10.1186/s42047-024-00148-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42047-024-00148-2