Abstract
Background
Effective therapy for acute ischemic stroke relies on timely intervention. We aimed to evaluate the factors associated with the onset-to-arrival time and delayed hospital presentation in acute ischemic stroke patients. Subjects with acute ischemic stroke in Bethesda Hospital Yogyakarta, Indonesia from March to June, 2023 were prospectively recruited. A questionnaire was used to collect the information by direct interviews. Prespecified variables were included in univariate and multivariable analyses to identify the predictors of delayed hospital presentation of more than 4.5 h.
Results
Among a total of 175 patients, 64.6% of the patients arrived at the hospital more than 4.5 h after the stroke onset. Only 3 (1.7%) patients were eligible and received intravenous thrombolysis. In multivariable analysis, monthly income of more than IDR 550,000 (OR, 4.22; 95% CI 1.47–12.17; p = 0.007), wake-up stroke or unknown stroke onset (OR vs. known onset, 0.17; 95% CI 0.05–0.56; p = 0.004), distance from location of stroke onset more than 9.45 km (OR, 3.13; 95% CI 1.41–6.92; p = 0.005) and no history of coronary artery disease or heart failure (OR vs. present history, 0.12; 95% CI 0.04–0.37; p = 0.000) were related to delayed hospital presentation. The most frequently mentioned reasons for the delay were waiting for spontaneous improvement at home and unawareness of the stroke symptoms.
Conclusions
There is an enormous disparity in stroke services between developed and developing countries. This study highlighted the need to increase public stroke symptoms awareness.
Similar content being viewed by others
Introduction
Stroke is one of the leading causes of death in the world. It is estimated that there are 12.2 million people in the world who suffer from stroke each year. Ischemic stroke is the most common type, accounting for 62.4–87% of all stroke events [1,2,3]. Early diagnosis and prompt treatment are crucial in optimizing the benefits of stroke intervention. Intravenous thrombolysis is still the mainstay of therapy in patients with acute ischemic stroke, followed by the development of endovascular thrombectomy as a therapy that is beneficial up to 24 h after stroke onset in patients with proximal large vessel occlusion [4].
Effective thrombolytic therapy relies on timely intervention, and guidelines for recombinant tissue plasminogen activator (rtPA) recommend therapy within 3–4.5 h after the onset of stroke symptoms [5]. The time between the onset of symptoms and admission to the emergency department (ED) is the most fundamental factor in meeting eligibility requirements for intravenous thrombolysis [6]. Until recently, studies that have been conducted in Indonesia have not covered socioeconomic and literacy aspects regarding acute ischemic stroke [7, 8]. This study aims to evaluate the onset-to-arrival time of acute ischemic stroke patients and the factors that are attributed to it.
Methods
Study design and subject
This cross-sectional survey in a prospective cohort of acute ischemic stroke inpatients from the ED was conducted at Bethesda Hospital Yogyakarta, Indonesia in a 4-month period between March and June 2023. The study aims to analyze the factors influencing delayed presentation of acute ischemic stroke patients. The dependent outcome variable was onset-to-arrival time, divided into within 4.5 h and after 4.5 h from the stroke onset. Study subjects were approached to participate with consent before recruitment. No public campaigns regarding stroke awareness and no educational stroke programs for the personnel of the Emergency Medical Services (EMS) were taking place before or during the study.
Method of data collection
The diagnosis of acute ischemic stroke was established by the neurologist on duty based on clinical signs and brain computed tomography (CT). The diagnosis criteria were based on the classification of the acute ischemic cerebrovascular syndrome, including the definite and probable acute ischemic cerebrovascular syndrome. Definite category was defined as an acute onset of neurologic dysfunction of any severity consistent with focal brain ischemia and imaging/laboratory confirmation of an acute vascular ischemic pathology, while probable category was defined as an acute onset of neurologic dysfunction of any severity suggestive of focal brain ischemic syndrome but without imaging/laboratory confirmation of acute ischemic pathology and imaging, laboratory, and clinical data studies do not suggest nonischemic etiology (possible alternative etiologies are ruled out). Stroke onset was defined by the time sign and symptoms of stroke occurred [9]. Transient ischemic attack (TIA) was also included in the study. In the case of wake-up stroke and/or unknown onset of stroke, stroke onset was defined as the time when the patient went to sleep or the last time the patient was known to be awake without symptoms. Patients referred from other hospitals, those with in-hospital strokes, and those with stroke mimics were excluded.
For patients without cognitive impairment, aphasia, or confusion, the information was obtained directly from the patient. If the patient had aphasia, confusion, or cognitive impairment, details were obtained from family, caregivers, relatives, and/or stroke witnesses. Hospital arrival time was recorded by the time the patient registered in the ED triage office. A questionnaire was used to collect the information by direct interview within 48 h of hospital admission. A direct interview was done after disposition from the ER and did not postpone any stroke services. We developed a questionnaire with 34 questions adapted from existing studies to develop questionnaire items [10, 11]. Validation was carried out through testing questionnaires to the four lay members of the public. From March to June 2023, a face-to-face interview was conducted with the participants. The questionnaire was only administered once patient informed consent had been obtained. Patients with low data quality as incapacity to answer the structured questionnaire in the prehospital phase during the interview were not included in the analysis. The dependent outcome variable was onset-to-arrival time, divided into within 4.5 h and after 4.5 h from the stroke onset. The study was approved by the Health Research Ethic Committee of Bethesda Hospital Yogyakarta (reference number: 18/KEPK-RS/II/2023).
Key independent variables
The key independent variables included various parameters that were obtained from the existing study database and the interview. Socio-demographic information included age, sex, marital status, educational status, living arrangement, monthly and yearly incomes, location of stroke onset, EMS contact, mode of transportation to the hospital, history of cardiovascular risk factors (hypertension, diabetes mellitus, atrial fibrillation, smoking, history of concomitant cardiovascular disease [previous ischemic stroke, coronary artery disease, and heart failure]), and awareness of stroke symptoms and risk factors. Youden’s index cut score was used to classify age (≤ 76 and > 76 years), monthly income (IDR ≤ 550,000 and > 550,000), and distance from onset location (≤ 9.45 and > 9.45 km). The distance from the onset location to our hospital was calculated using Google Maps Directions Application Programming Interface (API) in kilometers.
Hypertension, diabetes mellitus, atrial fibrillation, and concomitant cardiovascular disease were defined as self-reported relevant history or diagnosed during hospitalization. Patients were classified as smokers (current and past smokers) and non-smokers. Anthropometric parameters (body weight and height) and blood pressure were also measured at admission. The body mass index (BMI) was calculated and classified based on the Asia–Pacific BMI classification. The severity of stroke was assessed at admission with the National Institutes of Health Stroke Scale (NIHSS). Stroke was categorized as minor (1–4) and moderate-to-severe (> 4) based on the NIHSS. The patient’s degree of disability was classified using the modified Rankin Scale (mRS) at admission. Awareness of risk factors and signs and/or symptoms of stroke was assessed by asking open-ended questions. A possible valid answer for signs and/or symptoms of stroke was according to the BE FAST mnemonic (Balance, Eye, Face, Arm, Speech, and Time) [12] and for the risk factors was based on the study by Boehme et al. [13].
Statistical analyses
The continuous data are presented as median and standard deviation. Explanatory variables were either continuous or categorical. Univariable and multivariable logistic regression analyses were used to calculate the crude and adjusted odds ratio (OR) and confidence intervals (CI), which describe the association between explanatory variables and the dependent variables. The selection of variables that were included in the models was based on the clinical experience, literature review, and available data. The selection of variables entered in the multivariate analysis was based on a significance level of 20% (p < 0.2) in the univariate model, considering the rule of thumb. For multivariate analysis, the level of significance used was 5% (p < 0.05). Statistical analysis was performed using STATA version 16 (Stata Corp).
Result
Subject characteristics
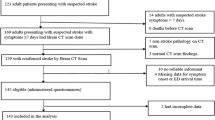
One hundred and eighty-one patients were included between March and June, 2023, 4 were excluded due to stroke mimics, and 2 others were not included in the analysis due to the low quality of the data. Finally, 175 patients were enrolled with characteristics of all subjects summarized in Table 1. One-hundred and thirteen (64.6%) of the patients arrived at the hospital more than 4.5 h after the stroke onset. The median age of the patient was 63 years (SD ± 11.47) and 66 (37.7%) were women. Thirty-three (18.9%) of the patients had a wake-up stroke or unknown stroke onset. Most patients had stroke onset location within 9.45 km from our hospital (106; 60.6%) and only 22 (12.6%) patients contacted the EMS before hospital arrival. The majority of patients (146; 83.4%) had multiple comorbid conditions. One hundred and twenty two (69.1%) of the patients came by private car, 22 (12.6%) came using online taxis, while only 20 (11.4%) patients used ambulances. Hemiparesis was the most common neurologic deficit, found in 131 (74.9%) patients, with the severity of NIHSS > 4 and mRS 4–5 in 73 (41.7%) and 46 (26.3%) of all patients, respectively. In univariate analysis, variables that predicted onset-to-arrival at the ED of more than 4.5 h from the stroke onset were onset condition, distance from location of onset, history of coronary artery disease and/or heart failure, and the ability to mention risk factor and signs and/or symptoms of stroke (Table 2).
Factors attributing to delayed presentation
The median onset-to-arrival time was 9.8 ± 22.8 h. Of all patients arriving at the hospital within 4.5 h, only 3 (1.7%) patients were eligible and received intravenous thrombolysis. Table 3 shows the multivariable analysis of the factors that may influence the onset-to-arrival time. In multivariable analysis, independent predictors of onset-to-arrival time of more than 4.5 h were the monthly income of more than IDR 550000 (OR 4.22, 95% CI 1.47–12.17, p = 0.007), wake-up stroke or unknown stroke onset (OR vs. known onset 0.17, 95% CI 0.05–0.56, p = 0.004) and distance from location of stroke onset more than 9.45 km (OR 3.13, 95% CI 1.41–6.92, p = 0.005). Patients with a history of coronary artery disease or heart failure had a significantly reduced risk of experiencing onset-to-arrival time delay of more than 4.5 h (OR 0.12, 95% CI 0.04–0.37, p = 0.000).
Reasons of delay
Sixty-two patients were brought timely to the hospital. Within the patients who experienced a delay in hospital admission, 28 (24.8%) of them were waiting for spontaneous improvement at home, while another 28 (24.8%) were not aware of the stroke symptoms (Table 4).
Literacy of stroke
Only 9 out of 175 patients and/or patients’ relatives were not able to mention any signs and/or symptoms of stroke and stroke risk factors. The most commonly mentioned stroke sign and/or symptom was one-sided limb weakness (153, 92.2%), while the most commonly mentioned risk factor of stroke was hypertension (148, 89.2%).
Discussion
This study highlights the proportion of onset-to-arrival time delay of acute ischemic stroke patients and the factors attributed to it. Several similar studies have assessed the time intervals between stroke onset and hospital arrival. The proportion of the patients arriving at the hospital within 4.5 h is slightly higher compared to the delayed group [11, 14,15,16]. Another study in Romania revealed that only 31.6% of the patients arrived within the intravenous thrombolysis time window [17]. The number is close to this study, in which only 35.4% of the patients presented within 4.5 h of stroke onset.
It is widely recognized that the earlier the intravenous thrombolysis is administered, the better the outcome is [18]. While intravenous thrombolysis remains underutilized globally, the rate of intravenous thrombolysis in Indonesia is still very low, ranging between 0.5% and 6.9% compared to a study in Italy that showed a much higher intravenous thrombolysis rate of 24.4% [7, 19,20,21]. Other than the delayed presentation, several factors also contributed to the rate of intravenous thrombolysis, including spontaneous clinical improvement, minor stroke, patient/family refusal, extensive infarction, seizures at onset, and history of gastrointestinal bleeding and/or acute bleeding diathesis [20, 22, 23].
Consistent with prior studies, this study found that sex, age, marital status, and payer type did not significantly affect arrival time [24, 25]. Several studies found an association between delayed presentation and older age or female sex group [11, 19, 21]. This study showed that having higher income was associated with a longer delay of presentation, although it was incongruous with other studies [26]. Most of our patients have national health insurance that covers stroke-related medical expenses including intravenous thrombolysis, this probably contributes to none of our patients mentioning cost consideration as a delay reason. Living in an elderly household or living alone was found to be significantly associated with delayed presentation of stroke patients [27], while in this study, only a small proportion of patients lived alone. Wake-up stroke and unknown stroke onset play a significant role in presentation delay, as shown in other studies [19, 28].
History of previous illness may contribute to hospital presentation time. Previous studies showed that patients with a history of prior stroke did not prove to be more aware of the stroke symptoms or arrive earlier than first-ever stroke patients [29]. It is important to make sure that patients of high-risk groups and their relatives receive proper information during hospitalization regarding stroke risk factors, symptoms, and the need for urgent evaluation for new cerebrovascular events. Patients with a history of coronary artery disease or heart failure may have better emergency awareness as a result of their previous contacts with medical providers. In a comparable study, atrial fibrillation was also associated with earlier hospital presentation [17]. Prehospital delay is longer for stroke rather than coronary artery disease, although there is an overlapping pathophysiology between the two conditions. This may reflect greater awareness of heart disease than stroke [30].
Geographical location has been established as one of the main factors related to later onset-to-arrival time [31]. Our hospital is the only thrombectomy-capable stroke center in our region that has more than 400,000 population within a land area of 3186 km2 [32]. To our knowledge, there are only four other hospitals that provide stroke services as primary stroke centers. We do not have any specific stroke referral system. In this study, the location of stroke onset more than 9.45 km was found to delay patient presentation significantly. The use of ambulance or EMS services is associated with earlier arrival care. Patients who used EMS had 2.61 higher odds of arriving at the ED within 4.5 h of onset, and 6.24 higher odds of arriving within 3 h [16]. Ambulance usage was as high as 60% in one of the French stroke units. However, one study showed that nearly all EMS staff would dispatch stroke patients to the nearest hospital irrespective of the availability of stroke intervention capability [31, 33]. In this study, even the use of online taxis exceeds the use of EMS. Similar results from Kenya, where most patients in the ED came by public means, including taxi [34]. This could be due to the familiarity and simplicity of using online taxi platforms.
An alarming lack of knowledge about stroke signs, symptoms, and risk factors needs to be targeted. Nearly, all of our respondents correctly mentioned one-sided limb weakness as the symptom of stroke. A similar study also showed that one-sided limb weakness was mentioned correctly by most subjects. Although psychosocial stress was not listed as one of the direct risk factors of stroke, it was mentioned frequently by the subjects [35]. Albeit with costly campaigns, better awareness of stroke does not automatically improve onset-to-arrival time nor increase intravenous thrombolysis rate, and stroke information from the internet was negatively correlated with early arrival [35, 36].
Several top priorities of improvement include establishing stroke units, increasing public awareness, and training health care providers and collaboration [29]. The use of EMS must be promoted to improve the timely presentation of acute ischemic stroke patients to the ED. Although this study was carefully designed and performed, this was a single-centered study in urban areas, therefore the result of this study may not be applicable nationally. This study also had potential sampling and measurement errors for the time of stroke onset due to the recall bias from the patients and/or family and relatives, especially for patients presenting with wake-up stroke.
Conclusion
This study showed that having a monthly income of more than IDR 550,000, wake-up stroke or unknown stroke onset, and distance from the location of onset more than 9.45 km were factors associated with later onset-to-arrival time. Patients with a history of coronary artery disease or heart failure tend to arrive earlier to the hospital. Delayed presentation is a major obstacle to implement thrombolytic and endovascular therapies. Health promotion strategies to increase stroke symptoms awareness, maximize the use of EMS, and the transfer of patients directly to intravenous thrombolysis-capable hospitals are promising methods to improve the onset-to-arrival time of acute ischemic stroke patients in Yogyakarta, Indonesia. To generalize the study findings, a larger and multicentered study is required to better assess the factors that contributed to the delayed hospital presentation in acute ischemic stroke patients.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- rtPA:
-
Recombinant tissue plasminogen activator
- ED:
-
Emergency department
- EMS:
-
Emergency medical services
- CT:
-
Computed tomography
- API:
-
Application programming interface
- BMI:
-
Body mass index
- NIHSS:
-
National Institutes of Health Stroke Scale
- mRS:
-
Modified Rankin Scale
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17:18–29. https://doi.org/10.1177/17474930211065917.
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart Disease and Stroke Statistics-2023 Update: a Report From the American Heart Association. Circulation. 2023;147:e93-621. https://doi.org/10.1161/CIR.0000000000001123.
Avan A, Digaleh H, Di Napoli M, Stranges S, Behrouz R, Shojaeianbabaei G, et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019;17:191. https://doi.org/10.1186/s12916-019-1397-3.
Xiong Y, Wakhloo AK, Fisher M. Advances in acute ischemic stroke therapy. Circ Res. 2022;130:1230–51. https://doi.org/10.1161/CIRCRESAHA.121.319948.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344-418. https://doi.org/10.1161/STR.0000000000000211.
Evenson KR, Foraker RE, Morris DL, Rosamond WD. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke. 2009;4:187–99. https://doi.org/10.1111/j.1747-4949.2009.00276.x.
Tangkudung G, Pertiwi JM, Girsang R, Tongku AS, Ate A. Characteristic of factors associated with admission time of stroke patients in hospital. Jurnal Sinaps. 2019;2:5–8.
Ningsih DK, Andarini S, Rachmawati D. Incident location distance and transportation to hospital delayed arrival patients post-acute ischemic stroke attack in emergency department east java-Indonesia. Ind J Publ Health Rese Dev. 2020;11:244–9. https://doi.org/10.37506/ijphrd.v11i12.13244.
Kidwell CS, Warach S. Acute ischemic cerebrovascular syndrome: diagnostic criteria. Stroke. 2003;34:2995–8. https://doi.org/10.1161/01.STR.0000098902.69855.A9.
Ihle-Hansen H, Thommessen B, Wyller TB, Engedal K, Fure B. Risk factors for and incidence of subtypes of ischemic stroke. Funct Neurol. 2012;27:35–40.
Fladt J, Meier N, Thilemann S, Polymeris A, Traenka C, Seiffge DJ, et al. Reasons for prehospital delay in acute ischemic stroke. J Am Heart Assoc. 2019;8: e013101. https://doi.org/10.1161/JAHA.119.013101.
Aroor S, Singh R, Goldstein LB. BE-FAST (Balance, Eyes, Face, Arm, Speech, Time): reducing the proportion of strokes missed using the FAST Mnemonic. Stroke. 2017;48:479–81. https://doi.org/10.1161/STROKEAHA.116.015169.
Boehme AK, Esenwa C, Elkind MSV. Stroke risk factors, genetics, and prevention. Circ Res. 2017;120:472–95. https://doi.org/10.1161/CIRCRESAHA.116.308398.
Al Khathaami AM, Mohammad YO, Alibrahim FS, Jradi HA. Factors associated with late arrival of acute stroke patients to emergency department in Saudi Arabia. SAGE Open Med. 2018;6:2050312118776719. https://doi.org/10.1177/2050312118776719.
Bhaskar S, Thomas P, Cheng Q, Clement N, McDougall A, Hodgkinson S, et al. Trends in acute stroke presentations to an emergency department: implications for specific communities in accessing acute stroke care services. Postgrad Med J. 2019;95:258–64. https://doi.org/10.1136/postgradmedj-2019-136413.
Dimitriou P, Tziomalos K, Christou K, Kostaki S, Angelopoulou S-M, Papagianni M, et al. Factors associated with delayed presentation at the emergency department in patients with acute ischemic stroke. Brain Inj. 2019;33:1257–61. https://doi.org/10.1080/02699052.2019.1641226.
Terecoasă EO, Radu RA, Negrilă A, Enache I, Cășaru B, Tiu C. Pre-hospital delay in acute ischemic stroke care: current findings and future perspectives in a tertiary stroke center from romania-a cross-sectional study. Medicina (Kaunas). 2022. https://doi.org/10.3390/medicina58081003.
Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695–703. https://doi.org/10.1016/S0140-6736(10)60491-6.
Minalloh RH, Machin A, Mardiana W, Suansanae T, Chulavatnatol S, Nathisuwan S. Pre-hospital and in-hospital delay in acute ischemic stroke patients in Indonesia: a multi-center study. Indonesian Journal of Pharmacy. 2022;33:299–306.
Situmeang RFV, Pangestu A, Stevano R, Tannu Y, Herlambang J, Putri C. Reasons withholding intravenous thrombolysis for acute ischemic stroke in an Indonesian Tertiary Center. Egypt J Neurol Psychiatry Neurosurg. 2023;59:11. https://doi.org/10.1186/s41983-023-00613-x.
Bandettini di Poggio M, Finocchi C, Brizzo F, Altomonte F, Bovis F, Mavilio N, et al. Management of acute ischemic stroke, thrombolysis rate, and predictors of clinical outcome. Neurol Sci. 2019;40:319–26. https://doi.org/10.1007/s10072-018-3644-3.
Eissa A, Krass I, Levi C, Sturm J, Ibrahim R, Bajorek B. Understanding the reasons behind the low utilisation of thrombolysis in stroke. Australas Med J. 2013;6:152–67. https://doi.org/10.4066/AMJ.2013.1607.
Reiff T, Michel P. Reasons and evolution of non-thrombolysis in acute ischaemic stroke. Emerg Med J. 2017;34:219–26. https://doi.org/10.1136/emermed-2015-205140.
Lacy CR, Suh DC, Bueno M, Kostis JB. Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (STROKE). Stroke. 2001;32:63–9. https://doi.org/10.1161/01.str.32.1.63.
Jin H, Zhu S, Wei JW, Wang J, Liu M, Wu Y, et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. 2012;43:362–70. https://doi.org/10.1161/STROKEAHA.111.623512.
Nepal G, Yadav JK, Basnet B, Shrestha TM, Kharel G, Ojha R. Status of prehospital delay and intravenous thrombolysis in the management of acute ischemic stroke in Nepal. BMC Neurol. 2019;19:155. https://doi.org/10.1186/s12883-019-1378-3.
Hagiwara Y, Imai T, Yamada K, Sakurai K, Atsumi C, Tsuruoka A, et al. Impact of life and family background on delayed presentation to hospital in acute stroke. J Stroke Cerebrovasc Dis. 2014;23:625–9. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.05.034.
Arulprakash N, Umaiorubahan M. Causes of delayed arrival with acute ischemic stroke beyond the window period of thrombolysis. J Family Med Prim Care. 2018;7:1248–52. https://doi.org/10.4103/jfmpc.jfmpc_122_18.
Al Khathaami AM, Algahtani H, Alwabel A, Alosherey N, Kojan S, Aljumah M. The status of acute stroke care in Saudi Arabia: an urgent call for action! Int J Stroke. 2011;6:75–6. https://doi.org/10.1111/j.1747-4949.2010.00542.x.
Herlitz J, Wireklintsundström B, Bång A, Berglund A, Svensson L, Blomstrand C. Early identification and delay to treatment in myocardial infarction and stroke: differences and similarities. Scand J Trauma Resusc Emerg Med. 2010;18:48. https://doi.org/10.1186/1757-7241-18-48.
Derex L, Adeleine P, Nighoghossian N, Honnorat J, Trouillas P. Factors influencing early admission in a French stroke unit. Stroke. 2002;33:153–9. https://doi.org/10.1161/hs0102.100533.
Wikipedia contributors. Special Region of Yogyakarta. Wikipedia 2024. https://en.wikipedia.org/wiki/Special_Region_of_Yogyakarta#:~:text=As%20a%20first%2Dlevel%20division,entity%20of%20Indonesia%20after%20Jakarta. (accessed February 18, 2024).
Althubaity E, Yunus F, Al Khathaami AM. Assessment of the experience of Saudi emergency medical services personnel with acute stroke. On-scene stroke identification, triaging, and dispatch of acute stroke patients. Neurosciences (Riyadh). 2013;18:40–5.
Wachira B, Martin IBK. The state of emergency care in the Republic of Kenya. Afr J Emerg Med. 2011;1:160–5. https://doi.org/10.1016/j.afjem.2011.10.008.
Mithi C, Shah J, Mativo P, Sokhi DS. Infrastructural and knowledge barriers to accessing acute stroke care at a regional tertiary facility in kenya. J Stroke Med. 2021;4:50–7. https://doi.org/10.1177/25166085211018046.
Lecouturier J, Rodgers H, Murtagh MJ, White M, Ford GA, Thomson RG. Systematic review of mass media interventions designed to improve public recognition of stroke symptoms, emergency response and early treatment. BMC Public Health. 2010;10:784. https://doi.org/10.1186/1471-2458-10-784.
Acknowledgements
We would like to thank all the subjects participated in the current work, to the neurologist at Bethesda Hospital Yogyakarta and the medical staffs in the neurology wards.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YH: idea of the research, writing of the paper, supervising of data collection, proofreading. NY: collection of data, making the study design. All authors were involved in drafting the article or revising it critically for important intellectual content. All authors have read and approved the final manuscript to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Health Research Ethic Committee of Bethesda Hospital Yogyakarta (reference number: 18/KEPK-RS/II/2023). The study was explained to the participants and a written informed consent was given by each participant.
Consent for publication
A written informed consent was given by each participant regarding the publication of their information.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, N., Hartanto, Y.B. Characteristics and reasons for delayed presentation in acute ischemic stroke: single-centered study in Indonesia. Egypt J Neurol Psychiatry Neurosurg 60, 67 (2024). https://doi.org/10.1186/s41983-024-00838-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-024-00838-4