Abstract
Background
Osteoporosis (OP) is the fourth leading cause of disability in the elderly. The challenges presented by OP fractures are complex. Vertebral body fractures (VCF) are frequently encountered in osteoporotic patients. Due to the predominant age group of osteoporotic VCF along with co-morbidities, restoring the vertebral body height and the correction of kyphosis via minimally invasive methods are preferred. Vertebroplasty continues to be the most commonly employed method in this selection. The purpose of this study is to provide evidence for the combined employment of vertebroplasty with other minimally invasive techniques in the treatment of osteoporotic VCF. A retrospective analysis of patients treated for multilevel thoracolumbar osteoporotic VCF was performed. The patients were treated with percutaneous vertebroplasty (PVP), transforaminal lumbar interbody fusion supplemented by vertebroplasty (TLIF-VP) and minimally invasive transpedicular screw fixation supplemented by vertebroplasty (TP-VP). They were followed up for at least a year and VAS and ODI scores along with the degree of kyphotic correction and restoration of vertebral body height have been evaluated.
Results
Sixty patients with 132 levels of VCF treated were evaluated. PVP was superior in terms of shortened operative period, decreased blood loss, earlier ambulation and not requiring general anesthesia. Both TLIF-VP and TP-VP required general anesthesia, with longer operative period and increased blood loss, however it provided greater kyphotic correction. Restoration of vertebral body height was the highest in the PVP and TP-VP group. All patients benefited clinically from the interventions in regard to VAS pain and ODI scores.
Conclusions
VP continues to be the choice for minimally invasive correction of osteoporotic VCF. VP can be employed with other techniques as seen in this study in selected patients with sufficient symptomology. TLIF implantation allowed for discectomy and sufficient root decompression while transpedicular screw fixation allowed for greater correction especially in the chronic fractures.
Highlights
-
Osteoporosis primarily affects the elderly with the fourth leading cause of disability
-
Osteoporotic vertebral compression fractures are commonly encountered, but require special attention given the age and co-morbidities of the patients
-
Minimally invasive spinal surgery should be the first choice of the treatment of osteoporotic vertebral compression fractures
-
Vertebroplasty remains the quickest and safest minimally invasive method in the treatment of compression fractures
-
Vertebroplasty can be safely employed with other minimally invasive approaches, such as TLIF and transpedicular screw system in selected patients
Similar content being viewed by others
Background
Defined as a bone mineral density (BMD) value below the average value by 2.5 standard deviations, osteoporosis (OP) is on the rise parallel to life expectancy and longevity. This in turn has increased the rate of osteoporotic fractures. Although the cranium is exempt, fractures usually occur in the vertebrae, distal arm and hip [1]. OP is the fourth leading cause of disability in the elderly [2]. Its unique characteristics make the approach to treatment of OP fractures unique as well.
OP complicated with a fracture creates a complex situation for the patient, the treating physician and accompanied by socio-economic support. OP fractures in the US has an incidence of 1.5 million/year with almost half of the fractures localized in the vertebral column [3]. To appreciate this amount, we can say that a fracture of the vertebrae is recorded every 2 min. This is expected to rise by 20% in 2035 [4].
The manifestation of an osteoporotic vertebral compression fracture (VCF) is often mistaken for back pain, characterized by acute onset. Most patients complain of stubborn pain at the affected level, deteriorating postural change, loss of body height and kyphotic inclination. Patients note a sharp deterioration in the quality of life, activity is reduced or eliminated, the psyche and emotional status becomes unstable and depression may ensue [3]. The onset of osteoporosis forces a person to adjust their lifestyle, deviate from their usual schedule, which makes it more difficult to overcome exacerbations of chronic diseases and higher mortality risks [5].
Morbidity caused by VCF can be exhausting due to pain and limitation of mobility thus indirectly affecting mortality [6]. Although conservative treatment may be employed in selected cases, WFNS Spine Committee concluded that both vertebroplasty (VP) and kyphoplasty are equally superior to conservative treatment [7]. First described in 1984 to fill the void left following an excision of a vertebral malignancy, percutaneous vertebroplasty (PVP) has become a standard surgical approach [8]. It allows for the radiological and functional correction of the VCF under local anesthesia with minimal invasive methods allowing for earlier mobilization of the patient. These factors are especially important in the more frequently encountered elderly population [9].
The aim of this study was to evaluate the treatment in terms of effectiveness, three different modalities employing VP in patients with multilevel osteoporotic VCF. The outcomes are assessed clinically and radiologically in detail.
Methods
A retrospective analysis of patients admitted to the traumatology ward from January 2020 to January 2021 was performed. WMA Declaration of Helsinki—ethical principles for medical research involving human subjects was strictly followed: Informed consent to participate in the study was obtained from all the participants. Ethics approval was obtained from the Ethics Committee of the Petrovsky National Research Centre of Surgery (Petrovsky NRCS) in Moscow (Ref: ESN/6_1222, Date: 10.12.21).
Patients aged 60 years or more with a multilevel VCF of the thoracolumbar spine treated by VP were included in the study. Patients with concomitant pathologies such as malignancy, infection and type C and complicated fractures according to the Magerl AO/ASIF classification [10] were excluded. Patients with spinal canal stenosis and/or disc herniation were included. Demographic data, clinical and radiological (JIKEI Index) evaluation, BMD score, levels of intervention, surgical approach and details, complications, visual analog scale (VAS) for lower back pain and Oswestry Disability Index (ODI) scores for functional recovery were collected.
Patients were followed up at 3-month intervals for at least a year. Post-operative radiological assessment consisted of the correction of the vertebral body height and kyphosis. These parameters were evaluated in the long-term follow-up as well to note any losses.
The surgical approach was based on the patient, co-morbidities, morphology of the fracture and concomitant spinal pathologies. Three different surgical protocols were employed: (1) PVP, (2) minimally invasive transforaminal lumbar interbody fusion supplemented by vertebroplasty (TLIF-VP) and (3) minimally invasive transpedicular screw fixation supplemented by vertebroplasty (TP-VP).
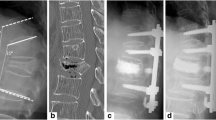
All patients were operated in the prone position. PVP was performed under local anesthesia and IV sedation. No deviations from the standard technique were made. Jamshidi needle was bilaterally, transpedicularly inserted, and cement [poly-methyl methacrylate (PMMA)] injection was controlled in the lateral and A–P fluoroscopic views (Fig. 1). Both TLIF-VP and TP-VP were performed under general anesthesia in the same position. TLIF-VP patients underwent minimally invasive laminotomies with discectomy followed by the placement of a TLIF cage. This was followed by the standard vertebroplasty technique described above. The TP-VP patients underwent above described steps followed by the placement minimally invasive transpedicular cannulated screws through a guide wire. The vertebral body was augmented with cement through the screws and after correct positioning of the patient rods were tightened.
Results
Radiological and clinical data of 60 patients comprising 18 men and 42 women were collected. With a range of 60–100 years of age, the mean age was 70.2 ± 9.17 years. 68.30% of the patients were between the ages of 70–80 and 40% had two or more chronic diseases. 58% of the patients had post-menopausal OP, 23% due to prolonged steroid use and 8% due to post-gynecological surgery-related causes. No patient had any pre- or post-operative neurological deficit.
VCF in 132 levels were treated in total (Fig. 2). The most common site was the thoracolumbar junction (T11–L1) fractures with 46 levels. The most common type of fracture was type A with 107 levels (81%) and the remainder 25 levels were type B.
Patients with a loss of height no more than 50% in the affected level and less than 20° of kyphosis (Type A) were treated with PVP alone (n = 38). Regardless of the type of fracture, patients with a loss of height greater than 50%, kyphosis less than 20° and concomitant disc pathology, were treated with TLIF-VP (n = 6). Patients with a kyphosis greater than 20° were treated with TP-VP (n = 16). PVP patients were mobile 6 h after surgery, whereas the other group was mobile after 12–24 h.
The shortest duration of surgery and minimum blood loss was in the PVP group (Fig. 3). Indicators of restoring the height of the vertebral body and correction of kyphotic deformity were assessed in the first three days after surgery using radiography. The results obtained were subjected to statistical processing using the MS Excel software package. The distribution of populations other than normal was carried out on the basis of methods of non-parametric analysis of the sample using the Mann–Whitney test. Differences were considered statistically significant at p < 0.05.
The restoration of the vertebral body height was notably highest in the TLIF-VP group whereas the kyphotic deformity correction angle was greatest in the TP-VP group (Table 1). Although statistically insignificant, fractures younger than 1 month were more prone to restored body height and kyphotic correction.
For the follow-up examinations, the operated patients were invited for examinations at 3, 6, 12 months from the date of the intervention, and some were also interviewed by phone. On average, each patient was observed for 14.8 ± 6.2 months. Forty-five patients stated they benefited from the intervention in alleviating their back pain, whereas 15 patients stated minimal improvement. VAS pain score changes at the 3rd month control on average indicated a reduction by 4.3 points (range: 1–8) (p < 0.05).
The functional recovery and satisfaction of the patients at the 12-month control were evaluated in reference to ODI and VAS score changes. A VAS score of 0–3, ODI < 20% and the correction of kyphosis to be not less than 5° were considered good in 45 patients. A satisfactory result of a VAS score of 4–5, ODI < 40% and the correction of kyphosis to be not less than 10° was observed in 10 patients. Unsatisfactory result of VAS 6 ≥, ODI 41–100%, significant loss of correction in kyphosis, neighboring VCF and sagittal imbalance was observed in five patients.
Discussion
This study has presented its results of PVP, TLIF-VP and TP-VP in the treatment of VCF of the thoracolumbar spine in osteoporotic patients. As expected, the patient population mostly comprised women (70%) with an average age of 70.2 years since OP is frequently encountered in post-menopausal women aged 50 and over. Most of the fractures were localized between T11 and L1, which is of no surprise since the thoracolumbar junction is one of the most common sites of vertebral fractures. In reference to ODI and VAS scores, along with radiological evaluation, 92% of the patients had good or satisfactory results. Only five patients had unsatisfactory results after one year. The results obtained from the Oswestry questionnaire were not compared according to the technique employed for VP since different techniques were decided on a patient basis. The difference in the intervention was mainly based on sagittal balance and the primary aim of the study was to evaluate the use of VP along with concomitant pathologies requiring concomitant interventions. Thus the emphasis of the study is not to evaluate the differences in interventions superiority-wise but rather on the effectiveness of VP and VP augmented surgeries in the treatment of multilevel OP compression fractures. Regardless of the technique employed, all VP modalities proved to be mostly efficient in treating the patients’ symptoms, improving their disability index and kyphotic deformity. All patients benefited from the interventions with an average reduction of 4.3 in the VAS score at the 1-year follow-up. 75% of the patients had a VAS score decrease in the range of 3–5, which is a significant relief.
PVP provided for quick and efficient method of restoring vertebral body height by 26.6% (p < 0.01). It has an easier learning curve and is applicable under local anesthesia. The patient is able to recover swiftly from the intervention with an earlier ambulation period. It can be safely employed in the elderly population who have co-morbidities with intact spinal canals and a kyphotic deformity less than 20°. PVP on average corrected the kyphosis by 7.2° (p < 0.05). This technique also allowed the patient to “feel better” quicker, with an increased confidence of self-sufficiency along with satisfaction. This technique is known to increase the patient’s ability to perform daily activities, move from a chair to the bed and sufficiently climb stairs [11]. Although there is confounding results on the ability of PVP to reduce pain, our results in line with previous studies [12, 13] resulted in an immediate pain relief and continued to decrease for a year. PVP remains to be the most cost effective treatment modality of VCF making it a vital tool in underdeveloped and developing parts of the world. Understandably, it has a shorter operative time period with minimum hemorrhage. While performing PVP, the most difficult moment was the correct manipulation of the inserted Jamshidi needles, fluoroscopy was repeated many times in order to control the position.
Vertebroplasty can be combined with other techniques as seen in our cases. Patients who had concomitant disc pathology received minimally invasive TLIF implantation and the neighboring VCF were treated with VP. This was also the chosen modality with increased loss of vertebral body height. It allowed for a correction of kyphotic deformity on average by 9.5° while restoring the body height on average by 42.7% (p < 0.05). The minimally invasive TLIF-VP allowed for the adequate discectomy allowing for the relief of radiculopathy symptoms while treating the VCF in selected patients. However, it did require about 50 min of more operative time under general anesthesia and on average 92 ml of blood loss. The increased duration of operative period was observed in the TP-VP group with an average of 112.7 min and 101 ml blood loss. The minimally invasive transpedicular screw fixation allowed for the correction of greater kyphotic deformity thus preserving this technique for patients with a pre-operative kyphotic deformity of 20° and with chronic fractures. Appropriate intraoperative manipulation of the vertebral column before fixing the system allows for an increased body height restoral and lordotic angle. The TP-VP group had the highest rate of kyphotic deformity correction with an average of 16.3°. However, the average restoration of vertebral body height in the TP-VP was lower than the TLIF-VP. This may have been due to the chronic nature of the patients in the TP-VP group.
Conclusions
The age and the BMD score of a patient with a multilevel VCF require special attention. As osteoporotic VCF are seen mostly in the elderly population with concomitant disorders, minimally invasive interventions should be the first choice if conservative treatment fails. The restoration of the vertebral body height and the correction or arrest of kyphotic deformity increase the quality of life while decreasing pain and disability. Mobility is of vital importance in the elderly population as it dramatically decreases the rate of morbidity and mortality. Vertebroplasty, as evidenced in this paper is still a safe, quick and efficient treatment modality for osteoporotic VCF. This study also has put forth the results of combined surgeries that could be employed with VP. Since additional techniques require general anesthesia with prolonged operation time and increased blood loss, this decision should be made on patient basis keeping the symptoms and nature of the fractures along with the desired goal.
We consider PVP as a priority in the choice of treatment because it requires less trauma to the patient, the operation is performed quickly and there is a decreased amount of hemorrhage and local anesthesia is sufficient. Stand-alone PVP and combined with TLIF placement have a high rate of vertebral body height restoration.
Availability of data and materials
All data related to this study can be requested from the corresponding author via e-mail.
Abbreviations
- BMD:
-
Bone mineral density
- OP:
-
Osteoporosis
- VCF:
-
Vertebral compression fracture
- VP:
-
Vertebroplasty
- PVP:
-
Percutaneous vertebroplasty
- VAS:
-
Visual analog scale
- ODI:
-
Oswestry Disability Index
- TLIF:
-
Transforaminal lumbar interbody fusion
- TLIF-VP:
-
TLIF supplemented by vertebroplasty
- TP-VP:
-
Pedicle screw supplemented by vertebroplasty
- PMMA:
-
Poly-methyl methacrylate
References
Salari N, Ghasemi H, Mohammadi L, Behzadi MH, Rabieenia E, Shohaimi S, et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):609.
Wilson DJ. Vertebroplasty for vertebral fracture. BMJ. 2011;343: d3470.
Langner S, Henker C. Vertebroplastie und Kyphoplastie: Eine kritische Stellungnahme [Vertebroplasty and kyphoplasty: a critical statement]. Radiologe. 2020;60(2):138–43.
Chen WC, Tsai SHL, Goyal A, Fu TS, Lin TY, Bydon M. Comparison between vertebroplasty with high or low viscosity cement augmentation or kyphoplasty in cement leakage rate for patients with vertebral compression fracture: a systematic review and network meta-analysis. Eur Spine J. 2021;30(9):2680–90.
Savage JW, Schroeder GD, Anderson PA. Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Am Acad Orthop Surg. 2014;22(10):653–64.
Barrocas AM, Eskey CJ, Hirsch JA. Vertebral augmentation in osteoporotic fractures. Injury. 2007;38(3):88–96.
Sharif S, Ali MY, Costa F, Zileli M, Parthiban J. Vertebral augmentation in osteoporotic spine fractures: WFNS Spine Committee recommendations. J Neurosurg Sci. 2022;66(4):311–26.
Mathis JM, Belkoff SM, Deramond H. History and early development of kyphoplasty. In: Mathis JM, Deramond H, Belkoff SM, editors. Percutaneous vertebroplasty and kyphoplasty. 2nd ed. New York: Springer Science+Business Media; 2006. p. 3–5.
Huang Y, Zhao T, Reidler JS, Chen X, Zhang H, Shao H, et al. The top 100 most-cited articles on kyphoplasty and vertebroplasty. World Neurosurg. 2020;135:e435–46.
Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201.
Su WC, Wu WT, Peng CH, Yu TC, Lee RP, Wang JH, et al. The short-term changes of the sagittal spinal alignments after acute vertebral compression fracture receiving vertebroplasty and their relationship with the change of bathel index in the elderly. Geriatr Orthop Surg Rehabil. 2022;13:21514593221100240.
Karmakar A, Acharya S, Biswas D, Sau A. Evaluation of percutaneous vertebroplasty for management of symptomatic osteoporotic compression fracture. J Clin Diagn Res. 2017;11(8):RC07-RC10.
Santiago FR, Abela AP, Alvarez LG, Osuna RM, García MM. Pain and functional outcome after vertebroplasty and kyphoplasty. A comparative study. Eur J Radiol. 2010;75(2):e108–13.
Acknowledgements
The authors would like to acknowledge all the patients giving consent to have their results published.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. No corporate, government or institutional funding has been received.
Author information
Authors and Affiliations
Contributions
DES: conceptualization, methodology, software, surgery. RN, AV: investigation, data curation, surgery. IB: writing—original draft, writing—review and editing, formal analysis. MD, BC: supervision, visualization, validation.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Ethics Committee of the Petrovsky National Research Centre of Surgery (Petrovsky NRCS) in Moscow (Ref: ESN/6_1222, Date: 10.12.21) was obtained prior to the study. The study was carried out according to the latest revision of the Helsinki Declaration regarding medical research involving human subjects. Consent for participation was obtained from all patients.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Encarnacion-Santos, D., Nurmukhametov, R., Bozkurt, I. et al. Restoring vertebral height in the treatment of multilevel vertebral compression fractures with vertebroplasty. Egypt J Neurol Psychiatry Neurosurg 59, 135 (2023). https://doi.org/10.1186/s41983-023-00737-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00737-0