Abstract
Background
The prevalence of cervical canal stenosis alone is estimated to be present in 4.9% of the adult population. Co-existence of dual pathology may complicate clinical presentation and necessitates a wise and individually based decision process.
Objectives
To estimate the co-existence of cervical canal stenosis in surgical lumbar canal stenosis patients and its reflection on decision-making regarding surgery.
Methods
It is a prospective study that was conducted on 70 cases with symptomatic lumbar canal stenosis by investigating them for cervical canal stenosis clinically and radiologically.
Results
The co-existence of cervical and lumbar canal stenoses was seen in 62 cases (88.57%); cases with relative cervical stenosis were 25 (35.714%) and absolute cervical stenosis was 37 (52.857%). Cases with no cervical stenosis were 8 (11.428%) and cases with relative lumbar stenosis were 22 (31.428%), while cases with absolute lumbar stenosis were 48 (68.571%). Cases with symptomatic cervical canal stenosis were 30 (42.857%). Cases with asymptomtic cervical canal stenosis were 32 (45.71%).
Conclusion
Tandem spinal stenosis (TSS) is not uncommon and MRI cervical spine should be done for every lumbar canal stenosis patient especially if indicated by history or clinical examination.
Similar content being viewed by others
Introduction
Cervical stenosis can occur concomitantly with lumbar stenosis. However, the spectrum of symptomatology varied from patient to patient [1]. Whether symptomatic or asymptomatic cervical stenosis, the decision should be weighed wisely in the presence of disabling symptomatic lumbar stenosis [2]. Symptomatic cervical stenosis is easily diagnosed; however, the asymptomatic one is difficult to catch due to its “hidden” nature [3]. On the other hand, severe cervical stenosis can be completely asymptomatic and called “silent stenosis” [4, 5]. This should be known well, as reports of complete paralysis and post-operative non-relevant neurological disorder of cervical origin were published previously [6, 7].
The aim of the study was to identify the incidence of concomitant cervical and lumbar canal stenosis and the influence of cervical canal stenosis on the surgical decision made for lumbar canal stenosis and hence the outcome of the patient’s condition.
Methods
This was a prospective cross-sectional study held from February 2018 to September 2018. Seventy patients with lumbar canal stenosis indicated for surgery were admitted to the outpatient clinic for investigating cervical spine pathology by both clinical and radiological examination through performing cervical spine magnetic resonance (MR) imaging. The study was ethically approved prior to enrollment of participants and patient consent was provided before recruitment.
Degenerative lumbar canal stenosis indicated for surgery and age over 40 years was the only inclusion criteria for the study. Conservative lumbar canal stenosis, history of trauma, genetic disease, and anomalies of lumbar spine are the main exclusion criteria for this study.
All patients underwent complete history taking and clinical examination. Japanese Orthopedic Association (JOA) score for back pain syndrome was used for assessment in addition to clinical and radiological assessment. Indication for lumbar spine surgery was validated by two senior certified neurosurgeons prior to pre-operative preparation and patient consent.
MRI cervical spine was done to all these patients. MRI was performed using 1.5 T Siemens Magnetom Symphony Maestro Class, Syngo MR 2002B (Siemens Medical System Inc., Erlangen, Germany). Cervical canal stenosis was assessed according to cord indentation according to anterior and posterior subarachnoid space around the cord; stenosis was diagnosed by measuring the antero-posterior and lateral diameters in axial and sagittal views in T2-weighted images at the level of C3 to assess the stenosis according to these diameters’ measurements (normal AP diameter is 13–17 mm, relative stenosis 11–13 mm, and absolute stenosis < 10 mm).
Patients were assessed post-operatively for satisfaction by finding any improvement in pain, spasticity, sensory and motor functions, and improvement in daily activities and lifestyle.
The primary outcomes of this study were investigating the prevalence of concomitant cervical and lumbar canal stenosis and estimation of number of patients whose plan of management changed from doing lumbar surgery only to doing both cervical and lumbar surgeries and cervical decompression only.
The secondary outcome of the study was the rate of symptomatic and asymptomatic concomitant lumbar and cervical canal stenosis and the incidence of different degrees of cervical stenosis by MRI either relative or absolute.
Statistical tests were 2-sided and included Student t test for continuous data and either Fisher exact or c2 test for continuous or categorical data, respectively, with statistical significance defined using a threshold P below 0.05. Data was analyzed using the IBM Statistical Package of Social Science (SPSS) advanced statistics version 25 (SPSS Inc., 2019, Chicago, IL, USA).
Results
The patients’ criteria are illustrated in Table 1. The mean and standard deviation of age was 55.7 ± 9.8 years. The most frequent age sector was those ranging from 60 to 70 years. Male patients constitute 65.7% of our study. Diabetes mellitus was found to be the most prevalent comorbidity in our study (37.14%).
According to Fig. 1, the actual difference between the number of cases with symptomatic cervical stenosis and non-symptomatic cervical stenosis was discovered to be statistically significant (p = 0.001).
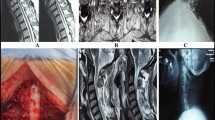
Frequency of symptoms is illustrated in Table 2. Back pain was the main complaint in 65 cases; 62 patients showed improvement of the back pain after either cervical decompression or lumbar decompression or both combined. Neck pain was a presenting symptom in 8 cases which improved later after cervical decompression. Lower limb pain was a complaint in (58 cases) whether sciatica (12 cases) or claudication (46 cases) and improved after lumbar decompression except in 4 cases of claudication which did not show any improvement. As well, 4 cases presented with brachialgia which improved in only 3 cases. Spasticity was seen in 26 cases. All cases with spasticity improved after cervical decompression gradually but was more evident in cases operated by posterior cervical decompression than anterior cervical discectomy and fusion (ACDF) except one case. Weakness was seen in 12 cases presented with foot drop (partial or complete) and 2 cases were quadriparetic with the weakness more in upper limbs due to absolute cervical canal stenosis; weakness improved after decompression, while one case of foot drop showed no improvement. Gait disturbances occurred only in cases with absolute canal stenosis which was improved post-operatively after canal decompression especially the spastic gait in cervical canal stenosis and high steppage gait in foot drop to a less extent that got better after intense physiotherapy. Five patients presented with associated urinary manifestations, and three cases presented with precipitancy that improved post-operative.
The affected lumbar and cervical spinal stenosis are illustrated in Figs. 2 and 3. There was statistically significant elevated percentage of both L4-5 and C3-4 more than any other level (p = 0.0084, 0.005), respectively, assessed according to mid sagittal T2 MRI. Cervical stenosis cases were found to be relative cervical stenosis in 25 cases (35.714%) and absolute in 37 (52.857%). Figure 1 illustrates the subdivisions of each category within symptomatic and asymptomatic cervical stenosis. It has been found that relative lumbar spinal stenosis was detected in 22 cases (31.42%) and absolute in 48 cases (68.57%).
The surgical decision was changed according to the cervical findings in 33 cases (47.142%). Once the patients knew their total clinical and spinal status, they shared with their physicians the surgical decision either in the priority of surgery or the type of surgery taken as follows: cervical only in 14 cases (20%), lumbar only in 35 cases (50%), and both cervical and lumbar in 21 cases (30%) in the form of one-staged combined surgery in 8 cases (11.4%), lumbar first in 2 cases (2.857%), and cervical first in 11 cases (15.714%)
The surgical approach was ACDF in 19 cases (27.14%), posterior cervical laminectomy in 16 cases (22.85%), lumbar laminectomy in 40 cases, and lumbar fixation in 10 cases.
Improvement has been estimated in our study and found to be in 56 cases (80%); non-improved cases were seen in 6 cases (8.5%), while complications were emergent in 8 cases (11.4%).
Wound infection was seen in the follow-up of 2 patients in the outpatient clinic who were known to be diabetic and both needed wound debridement and followed by intense course of IV antibiotics and they were improved in the follow-up. Non-intentional durotomy occurred in 4 cases after lumbar decompression in patients with absolute lumbar stenosis and were managed by primary suturing and only one case was complicated with CSF leak which was managed conservatively using medical treatment. Cord edema manifested with quadriplegia and respiratory muscle paralysis as the patient could not be weaned from endotracheal tube post-operative, that was seen in only (one case), for which the patient received intense dehydrating measures and corticosteroid followed by improvement of quadriplegia and underwent tracheostomy.
Discussion
The co-existence of cervical and lumbar canal stenosis was seen in 62 cases (88.57%) out of our 70 cases. Although literature stated the exact percentage is ranging from 5 to 25% [3, 5, 8], our results agreed with Matsumoto et al. [9] who discovered that positive degenerative MRI findings in both the lumbar and cervical spine was observed in 78.7% of the patients; Kikuike et al. [10] stated that the incidence of this pathologic condition has been reported to range from 0.12 to 19%. Dagi et al. [11] concluded that the calculated prevalence of degenerative spine disease, including tandem spinal stenosis (TSS), is higher in the radiological than in the surgical literature. Radiographic signs of degenerative cervical and lumbar spondylotic changes can be seen in 50% of the population over the age of 50 years and 75% over the age of 64 years. Aydogan et al. [12] thought that the overall proportion of patients with combined complaints of cervical and lumbar spine stenosis was 3.4% among 230 patients.
In a series of 12 patients with cervical spondylosis reported by Teng and Papatheodorou [13], seven had TSS. Four of the 12 patients were asymptomatic, but seven underwent decompression at both levels. Epstein et al. [14] reported that 5% of patients with spondylotic disease presented with symptoms referable to both the lumbar and the cervical portions of the spine.
Dagi et al. [11] stated that 19 of 100 patients admitted with a diagnosis of cervical or lumbar stenosis were found to have TSS. This variation in incidence may be a function of patient selection or of the small number in each series.
Cases with symptomatic cervical canal stenosis were 30 (42.857%), cases with asymptomatic cervical canal stenosis were 32 (45.71%), and cases with no cervical symptoms were 8 (11.4%). Epstein et al. and Dagi et al. [11, 14] concluded that four out of the 30 patients admitted for symptomatic lumbar canal stenosis had clinical signs of cervical myelopathy. And 9 out of the 30 patients admitted for lumbar canal stenosis had radiological cervical canal stenosis. Matsumoto et al. [9] concluded that MR images from asymptomatic subjects frequently showed degenerative changes in the lumbar spine, and these changes were significantly associated with degeneration in the cervical spine, suggesting that disk degeneration occurs in tandem in the lumbar and cervical spine.
As regards concomitant diseases, we had two cases known to be rheumatic (2.8%). Dagi et al. [11] also noted the presence of osteoarthritis in 16% and one patient had mild rheumatoid arthritis, but the limited records of patients with rheumatic disease hinders finding the actual association of these group of diseases in canal stenosis patient because they usually present with bony and joint pains that mimic degenerative canal stenosis symptoms.
As concluded by Felbaum et al. [15] when they stated that cervical decompression alone only may provide clinically significant relief of these lumbar symptoms and Epstein et al. [14] performed cervical decompression only in 12 patients with both cervical and lumbar canal stenosis. Post-operatively, they all showed improvement of both symptoms.
Also Aydogan et al. [12] stated that the treatment plan should be designed according to the chief complaints and symptoms of the patient. The operation should also be staged as it eliminates the risks of same-day surgery in patients which typically have an advanced age and comorbidities prior to surgery.
Two patients only underwent lumbar decompressive surgery before cervical decompression and they showed modest improvement because they were associated with absolute cervical canal stenosis, with the need for another surgery for cervical decompression [16].
Epstein et al. [14] performed lumbar decompression to 9 cases with both cervical and lumbar symptoms; post-operatively, the patient showed improvement of lumbar stenosis symptoms and worsening of cervical symptoms, and Yamada et al. [17] stated that radiographic coexisting cervical stenosis did not affect surgical outcomes for lumbar stenosis, although symptomatic cervical lesion affected the neurological score after lumbar surgery. An additional surgery for cervical lesion significantly improved neurological findings in tandem spinal stenosis (TSS) patients.
Krishnan et al. [18] recommend one-stage surgery for patients below the age of 60 while staged surgery is recommended in patients above the age of 60 years. Naderi and Mertol [19] concluded that simultaneous surgery for different segments of the spine is an alternative approach in patients with combined symptomatic pathologies, whose general or social condition is risky for two long-lasting procedures. This fact is also agreed with Epstein et al.’s [14] conclusion; they stated that the clinical outcomes of 1-staged combined cervical and lumbar decompression (CCLD), measured by JOA score for cervical myelopathy and low back pain and by activities of daily life (ADL), improved significantly at 6 months post-operatively. These effects were maintained for an average of 69 months in 10 patients suggesting that CCLD may be indicated for elderly patients, because of its potential benefits of minimum hospital stay and reduced costs [3]. Although other authors such as Kikuike et al. [10] have reached opposite conclusion, still there are no enough evidence about the pros and cons of the one-staged combined surgery because larger numbers of patients are necessary to provide sufficient data.
Aydogan et al. [12] concluded that the treatment plan should be designed according to the chief complaints and symptoms of the patient. The operation should also be staged. Staged surgery eliminates the risks of same-day surgery in patient who typically have an advanced age and comorbidities prior to surgery.
In our study, we discovered that the number of patients having both cervical and lumbar canal stenosis is much higher than proven in the literature. Out of 70 patients, we had 62 patients (88%) with concomitant cervical and lumbar canal stenosis, and 33 patients whose plan of management has been changed from doing lumbar decompressive surgery to cervical decompressive surgeries either alone, preceding lumbar decompression, or together in a single-staged surgery.
Dagi et al. [11] stated that the calculated prevalence of degenerative spine disease including TSS is higher in the radiological than in the surgical literature. Radiographic signs of degenerative cervical and lumbar spondylotic changes can be seen in 50% of the population over the age of 50 years and 75% over the age of 64 years.
Caron and Bell [20] stated that the exact frequency of symptomatic tandem stenosis is unknown, since only a small percentage of patients presenting with either cervical or lumbar stenosis have imaging studies of both the lumbar and the cervical spine. Furthermore, asymptomatic radiographic cervical or lumbar neural compression can be seen in a large percentage of the population.
Matsumoto et al. [9] concluded that MR images of asymptomatic patients with degenerative changes in the lumbar spine, and these changes were significantly associated with degeneration in the cervical spine, suggesting that disk degeneration occurs in tandem in the lumbar and cervical spine.
Krishnan et al. [18] stated that though TSS occurs relatively infrequently, the unrecognized occurrence in the general population may be higher. Detailed examination for even subtle signs followed by whole spine MRI (T2 sagittal) screening should be done. Lebl et al. [21] also stated that tandem stenosis should be considered when evaluating a patient with mixed claudication and myeloradiculopathy symptoms.
Problems may arise when the associated cervical stenosis is asymptomatic as it may lead to deficits or paraplegia after non-cervical spine surgery because it is asymptomatic stenosis; there is no clinical reason to obtain radiographic studies. And one can have severe radiographic stenosis without any symptoms. Krishnan et al. [18] stated that failure to detect cervical stenosis in a patient presenting predominantly with lumbar stenosis may carry significant risk of injury to the cervical cord during positioning for lumbar decompression surgery.
There are reports of missed compressive lesions of the spinal cord at the cervical region in lumbar degenerative disease [1, 3, 19].
According to the site of stenosis, the narrowing of the spinal canal may cause spinal cord and/or nerve root compression. The problem of missing a cervical lesion arises from dynamic mechanical factors of the cervical spine because as the neck extends, ligamentum flavum buckles inwards which results in the greatest decrease in the cross sectional area in the cervical canal as well as the spinal cord shortens and its cross sectional area increases which in turn increases the risk of cervical spondylotic myelopathy (CSM) [1, 5].
Aydogan et al. [12] stated that the treatment plan should be designed according to the chief complaints and symptoms of the patient. Yamada et al. [17] concluded that a clearly defined surgical algorithm does not exist and it remains unknown which procedure is more effective for achieving post-operative neurologic improvement in TSS patients with myelopathy.
Conclusion
Patients who present with lumbar canal stenosis indicated for surgery should have a thorough clinical and neurological examination and MRI cervical spine to exclude TSS.
Availability of data and materials
The dataset used and/or analyzed during the study are available from the corresponding author upon reasonable request.
Abbreviations
- TSS:
-
Tandem spinal stenosis
- JOA:
-
Japanese Orthopedic Association
- AP:
-
Antero-posterior
- ACDF:
-
Anterior cervical discectomy and fusion
- IV:
-
Intravenous
- CSF:
-
Cerebrospinal fluid
- CCLD:
-
Combined cervical and lumbar decompression
- ADL:
-
Activities of daily life
- CSM:
-
Cervical spondylotic myelopathy
References
Overley SC, Kim JS, Gogel BA, Merrill RK, Hecht AC. Tandem spinal stenosis: a systematic review. Jbjs Rev. 2017;5(9):e2.
Luo CA, Kaliya-Perumal AK, Lu ML, Chen LH, Chen WJ, Niu CC. Staged surgery for tandem cervical and lumbar spinal stenosis: which should be treated first? Eur Spine J. 2019;28(1):61–8.
Molinari RW, Flanigan R, Yaseen Z. Tandem spinal stenosis (TSS): literature review and report of patients treated with simultaneous decompression. Curr Orthop Pract. 2012;23(4):356–63.
Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yabe Y, Shiga H. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80(1):19–24.
Park MS, Moon SH, Kim TH, Oh JK, Lyu HD, Lee JH, Riew KD. Asymptomatic stenosis in the cervical and thoracic spines of patients with symptomatic lumbar stenosis. Global Spine J. 2015;5(5):366–71.
Young IA, Burns SP, Little JW. Sudden onset of cervical spondylotic myelopathy during sleep: a case report. Arch Phys Med Rehabil. 2002;83(3):427–9.
Kudo T, Sato Y, Kowatari K, Nitobe T, Hirota K. Postoperative transient tetraplegia in two patients caused by cervical spondylotic myelopathy. Anaesthesia. 2011;66(3):213–6.
Cheng F, You J, Rampersaud YR. Relationship between spinal magnetic resonance imaging findings and candidacy for spinal surgery. Can Fam Physician. 2010;56(9):e323–30.
Matsumoto M, Okada E, Toyama Y, Fujiwara H, Momoshima S, Takahata T. Tandem age-related lumbar and cervical intervertebral disc changes in asymptomatic subjects. Eur Spine J. 2013;22(4):708–13.
Kikuike K, Miyamoto K, Hosoe H, Shimizu K. One-staged combined cervical and lumbar decompression for patients with tandem spinal stenosis on cervical and lumbar spine: analyses of clinical outcomes with minimum 3 years follow-up. Clin Spine Surg. 2009;22(8):593–601.
Dagi TF, Tarkington MA, Leech JJ. Tandem lumbar and cervical spinal stenosis: natural history, prognostic indices, and results after surgical decompression. J Neurosurg spine. 1987;66(6):842–9.
Aydogan M, Ozturk C, Mirzanli C, Karatoprak O, Tezer M, Hamzaoglu A. Treatment approach in tandem (concurrent) cervical and lumbar spinal stenosis. Acta Orthop Belg. 2007;73(2):234.
Teng P, Papatheodorou C. Combined cervical and lumbar spondylosis. Arch Neurol. 1964 Mar 1;10(3):298–307.
Epstein NE, Epstein JA, Carras R, Murthy VS, Hyman RA. Coexisting cervical and lumbar spinal stenosis: diagnosis and management. Neurosurgery. 1984;15(4):489–96.
Felbaum DR, Fayed I, Stewart JJ, Sandhu FA. Relief of lumbar symptoms after cervical decompression in patients with tandem spinal stenosis presenting with primarily lumbar pain. Cureus. 2016;8(12):294–9.
Eskander MS, Aubin ME, Drew JM, Eskander JP, Balsis SM, Eck J, Lapinsky AS, Connolly PJ. Is there a difference between simultaneous or staged decompressions for combined cervical and lumbar stenosis? Clin Spine Surg. 2011;24(6):409–13.
Yamada T, Yoshii T, Yamamoto N, Hirai T, Inose H, Kato T, Kawabata S, Okawa A. Clinical outcomes of cervical spinal surgery for cervical myelopathic patients with coexisting lumbar spinal canal stenosis (tandem spinal stenosis): a retrospective analysis of 297 cases. Spine. 2018;43(4):E234–41.
Krishnan A, Dave BR, Kambar AK, Ram H. Coexisting lumbar and cervical stenosis (tandem spinal stenosis): an infrequent presentation. Retrospective analysis of single-stage surgery (53 cases). Eur Spine J. 2014;23(1):64–73.
Naderi S, Mertol T. Simultaneous cervical and lumbar surgery for combined symptomatic cervical and lumbar spinal stenoses. Clin Spine Surg. 2002;15(3):229–32.
Caron TH, Bell GR. Combined (tandem) lumbar and cervical stenosis. Semin Spine Surg. 2007;19(1):44–6 WB Saunders.
Lebl DR, Hughes A, Cammisa FP, O’Leary PF. Cervical spondylotic myelopathy: pathophysiology, clinical presentation, and treatment. HSS J. 2011;7(2):170–8.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public or commercial sector.
Author information
Authors and Affiliations
Contributions
OYA: contributed in design, revision of intellectual content, and follow-up. AAE: contributed in data collection and drafting manuscript. HM: contributed in data collection and data analysis. HAS: contributed in draft writing. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Department of Neurosurgery, Kasr Aliny Faculty of Medicine, Cairo University, on the 3rd of January 2018 (reference number, not applicable). All participants provided informed written consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdalla, O.Y., Al-Shami, H., Maghraby, H.M. et al. The value of cervical MRI in surgical lumbar canal stenosis patients. Egypt J Neurol Psychiatry Neurosurg 57, 10 (2021). https://doi.org/10.1186/s41983-020-00249-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-020-00249-1