Abstract
Background
Patients with acute ischemic stroke are at a higher risk of developing cognitive impairment which could be often attributed to cytokine activation.
Objectives
To explore the relationship between the cognitive performance and the inflammatory markers in the ischemic stroke patients at the early stage.
Patients and methods
A cross-sectional case-control study was performed on 44 ischemic stroke patients. The patients underwent the following battery of evaluation: (A) assessment of stroke disability by modified Rankin Scale (mRS) and National Institute of Health Stroke Scale (NIHSS). (B) neuropsychological evaluation using Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA) scale, trail making test (TMT), and Controlled Oral Word Association Test (COWAT). (C) Assessment of depression was done by using Beck Depression Inventory (BDI). Measurement of the serum levels of ESR, C-reactive protein, and IL-8 was done. This study included 44 ages, sex, and educational level matched controls for comparison of neuropsychological tests and serum level of IL-8.
Results
The patients showed worse performance in neuropsychological tests (MMSE, MoCA, COWAT, TMT) than the controls. There was a significant negative correlation between the serum level of IL-8 and (MoCA) (r = − 0.43, p = 0.004), verbal fluency (r = − 0.56, p < 0.001), and positive significant correlation between IL8 and executive functions (r = 0.61, p < 0.001).
Conclusion
The cognitive impairment in early acute ischemic stroke is highly correlated to the serum level of IL-8.
Similar content being viewed by others
Introduction
Cerebrovascular stroke was considered to be the third cause of death and morbidity worldwide. Although different mechanisms are involved in the pathogenesis of stroke, there is increasing evidence showing that inflammation could play a role in stroke progression, at least in acute phase [1], several inflammatory mediators may be involved in pathogenesis of acute stroke including CRP (C-reactive protein), interleukin-1b (IL-1b), IL-6, IL-8, IL-12, and IL-10 and may have prognostic role after the acute ischemic stroke [2].
The cognitive impairment observed in post-stroke patients was variable. It could be global cognitive deficits or domain-specific impairments including executive dysfunction, short-term memory problems and language, and visuospatial disabilities [3]. Cognitive impairment is often associated with cytokine activation [4].
The identification of clinical determinants and laboratory markers of post-stroke cognitive deficits may help to detect the patients at increased risk of cognitive deterioration and to prevent or delay the occurrence of post-stroke cognitive impairments. Although the inflammatory processes have been implicated in the pathogenesis of stroke, their role in the complex pathophysiological mechanism of post-stroke cognitive impairment is not completely understood [5]. This study aimed to explore the relationship between the cognitive impairment to the inflammatory markers in the ischemic stroke patients (within the first 48 h).
Patients and methods
This study is a case-control cross-sectional study included 44 patients presented with acute ischemic stroke in the first 48 h with age ranged from 21 to71 years old. The patients were collected from the emergency department, Neurology Outpatient Clinic, Fayoum University from October 2015 to September 2016. The patients and the control groups had written informed consent to participate in the study.
Forty-four age, sex, and educational level matched healthy individuals were included as a control group for comparison of the psychometric tests. They had no neurological disorders, cognitive dysfunction, or any vascular risk factors.
The sample size was calculated using EpiCalc 2000. The least required sample size based on a previous study [6] assuming power of study 90% and significance level 5%, thus least size required to be 10 per group.
The patients were excluded from the study if they presented with disturbed conscious level, aphasia, severe dysarthria or patients who had a history of psychiatric troubles or were receiving psychotropic drugs that could interfere with their ability to complete the psychometric assessments. The patients presented with neurological deficits that could be attributed to other causes such as acute infection, vasculitis and other inflammatory disorders such as neurosarcoidosis or Behçet’s syndrome were excluded particularly in patients’ age younger than 45 years. The patients presented with hemorrhagic stroke as it could be due to different etiology and clinical course or patients presented with metabolic disorders such as renal, hepatic, and autoimmune diseases with elevated ESR or interleukins levels were also excluded from the study.
All the ischemic stroke patients underwent an assessment of severity of disability using modified Rankin Scale (mRS) and National Institute of Health Stroke Scale (NIHSS). Moreover, the patients subjected to the following neuropsychological battery of evaluation within the first 48 h including screening neuropsychological tests using Folstein’s Mini-Mental State Examination (MMSE) [7] and Montreal Cognitive Assessment (MoCA) [8] with Arabic edition [9]. It was postulated that MoCA is an increasingly popular cognitive screening tool that it has been shown to have better sensitivity in detecting post-stroke impairments compared with the MMSE [10]. The national guidelines of the UK (2013) [11] recommended that all patients should be assessed for cognitive impairment within 6 weeks post-stroke using a validated tool, particularly the MoCA. It is thought to be containing more items assessing important domains such as executive functions and attention that are frequently affected in post-stroke patients than MMSE [9].
The Trail Making Test (TMT) was used for assessment of executive functions, the original trail making test was a paper a pencil test with two parts. In part A, the individual was asked to draw lines between 25 consecutively numbered circles spread randomly across a sheet of paper. Part B is more difficult; the participant is asked to draw lines alternating between numbers and letters in sequence. They are asked to complete the task as quickly as possible without lifting the pencil from the paper. The test takes a maximum of 5 min to complete [12] with Arabic edition [13]. Controlled Oral Word Association Test (COWAT) [14] was used for assessment of verbal fluency with Arabic edition [15]. Assessment of depression was done by Beck Depression Inventory-II (BDI-II), normative data: below10 and 11–16 corresponding to mild mood disturbance) [16].
Laboratory tests including CBC, kidney functions, liver functions, and serum glucose level were performed to exclude patients with metabolic disorders. Lipid profile including total cholesterol, triglycerides, separated using autoanalyzer by colorimetric method, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) levels were withdrawn after at least 10 h of fasting from the patients and controls.
Serum level of interleukin 8 (IL-8) was withdrawn within the first 48 h of the ischemic stroke. Serum suspension was centrifuged at 1500×g for 10 min within 30 min and directly frozen and stored at − 80 °C until analysis. The level of IL-8 was measured using enzyme-linked immunoabsorbent assay (ELISA) method.serum CRP level was measured using enzyme-linked immunosorbent assay (ELISA) with normal value below 6 mg/dl.
The patient underwent brain neuroimaging using magnetic resonance imaging (MRI) on TITAN TOSHIBA 1.5 Tesla (diffusion weighted image) or computed tomography (CT) on TOSHIBA multislice detector, Japan, in the Radiology Department, Fayoum University Hospital, in order to evaluate the localization and size of the ischemic infarction.
Statistical analysis
Statistical Package for Social Science IBM (SPSS) version 18 (2010) was used for data analysis. Qualitative data were presented as percentages, quantitative data were presented as arithmetic means and standard deviations. The Mann-Whitney test was used for comparison of quantitative variables. Spearman’s test was used for correlations. The level p < 0.05 was considered the cut-off value for significance.
Results
The demographic data of the patients and controls were illustrated in Table 1. There was no significant difference in age, sex, or educational level between them. The distribution of the vascular risk factors among the patients was shown in Fig. 1. It was shown that 36 patients (81.8%) presented with manifestation of anterior circulation ischemia, and 8 patients (18.2%) presented with manifestation of posterior circulation ischemia. The mean National Institutes of Health Stroke Scale (NIHSS) score was 4.3 ± 2.1. The mean modified Rankin Scale (mRS) score was 1.8 ± 0.86. As regards the neuroimaging of the brain, it was found that 37 patients (84.1%) presented with supra-tentorial lesions, and 7 patients (15.9%) presented with infra-tentorial lesions. Nineteen patients (43.2%) presented with left side infarction and 25 (56.8%) presented with right side infarction.
The patients showed significantly worse performance in the neuropsychological tests than the controls as shown in Table 2. There was a significant difference as regards Beck depression inventory (BDI) between the patients (10.3 ± 4.5) and the controls (7.7 ± 3.4) (p < 0.001). There was a statistically significant negative correlation between BDI-II score and MMSE score (r = − 0.33, p value = 0.03). On the other hand, there was no statistically significant correlation found between depression and MOCA (r = − 0.21, p = 0.2), TMT-B (r = 0.23,p = 0.1), COWAT-semantic (r = − 0.17,p = 0.3), and COWAT-phonemic (r = − 0.27, p = 0.08) tests.
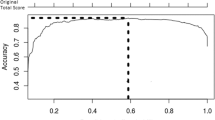
The patients showed significantly higher serum level of IL8 (47.6 ± 8.3) than the controls (14.6 ± 5.9) (p < 0.001). There was a statistically significant negative correlation between the serum level of IL-8 and MOCA (r = − 0.43, p = 0.004) as shown in Fig. 2, COWAT-semantic (r = − 0.56, p < 0.001), and COWAT phonemic (r = − 0.61, p < 0.001) tests. Moreover, there was a significant positive correlation with TMT-B (r = 0.61, p < 0.001), and serum IL8. On the other hand, there was no statistically significant correlation between MMSE score (r = − 0.27, p = 0.08) and the serum level of IL-8.
In respect to the hemispheric dominance, the patients with dominant hemisphere infarction showed significant worse MoCA performance (p = 0.03) as shown in Table 3. There was no significant difference in cognitive performance or serum IL-8 level between the patients in respect to localization of infarction as shown in Table 4.
There was no significant correlation between the ESR and MMSE (r = − 0.06, p = 0.7), MoC (r = − 0.09,p = 0.6), TMT-B (r = 0.01, p = 0.9), COWAT–semantic(r = − 0.03, p = 0.8), and COWAT–phonemic (r = − 0.02, p = 0.9). As regards ESR, there was no significant difference in neuropsychological tests between the patients with positive and negative ESR as shown in Table 5. As regards the CRP, there was no significant difference in neuropsychological tests between the patients with positive and negative CRP as shown in Table 6.
Discussion
Patients with stroke are considered to be at a higher risk of developing cognitive impairment. The incidence of cognitive deficit increases threefold after stroke and about 25% of the stroke patients may develop dementia. Cognitive dysfunctions may result in worsening stroke prognosis and outcome [5].
Accurate screening of cognitive impairment at the early stages of stroke is very important [17]. In this study, the patients were found to have worse cognitive performances in the first 48 h post stroke in both screening tests (MMSE and MoCA) compared to the control group. These results were in agreement with these studies [18, 19] (Figs. 3 and 4).
Moreover, it was found that patients with acute ischemic stroke showed significantly worse performance than the controls in the executive functions and verbal fluency in agreement with [18, 19]. Some research had postulated that various cognitive domains are affected depending on the area of the cortex damaged and the time after the stroke. At the acute stage (< 1 month), about 72% of patients with stroke presented with executive function affection particularly speed and attention [20]. The post-stroke cognitive impairment was not stable in severity or expression. The patients with acute stroke showed significant improvement across executive functions till 3 months especially within: speed and attention, numerical ability, and perception. Transient cognitive impairment was most prevalent in the first week post-stroke (39%) compared with after this week (19%) [21].
It was found that the serum level of IL-8 was significantly elevated in the plasma of the patients in the first 48 h post stroke in comparison to control group in this study which was in concordance with [6, 22]. This could be attributed to the fact that astrocytes induce IL-8 expression in the area of brain damage. IL-8 is a potent neutrophil chemoattractant and activator leading to neutrophil accumulation, IL-8 gives rise to mechanical obstruction in the collateral microcirculation in the capillaries. Hence, IL-8 and neutrophils take part in the augmentation of ischemic damage and extent of lesions, and the elevation of IL-8 is correlated with CNS injury [23].
Several researches had studied the association between cognitive functioning and inflammation in different neurological disorders, and few studies have evaluated the effect of inflammation on cognitive function in the acute stroke stage. In this study, the serum level of IL-8 was significantly correlated with screening MOCA test, executive functions, and verbal fluency. It was suggested that interleukin 8 has been shown to have proangiogenic properties independent of inflammatory cells that are upregulated in both tumor angiogenesis and in oxidative stress. It was hypothesized that the association between IL-8 and baseline cognitive function that we observed in these post-stroke patients may be indicative of the level of cortical damage during the initial ischemia [24].
However, we could not find a significant correlation between the IL-8 level and MMSE scores. This result was in agreement with Baune and colleagues (2008) [25] that postulated that cognitive performance among the elderly was not correlated with MMSE. These results could be attributed to that the sensitivity of MMSE is slightly lower than MoCA as screening test for detection the cognitive impairment particularly processing speed and executive function. MMSE is less capable of testing for complex cognitive impairments in domains such as visuospatial, executive function, and abstract reasoning that are commonly affected in stroke patients [26].
In this study, it was found that patients with dominant hemispheric infarction exhibited poor performance with MoCA test. This finding agreed with Chan and colleagues (2017) [27] that hypothesized the poor performance of dominant hemisphere stroke patients on the MoCA most probably reflected the dependence of the MoCA constitutes on both receptive and expressive language skills as well as verbal working memory abilities, which are commonly involved following a dominant hemisphere stroke.
There was no significant difference found in neuropsychological evaluation between the patients’ groups as regards the localization of infarction. It was observed that the prevalence of high-level cognitive impairments following stroke were somewhat independent of neuroanatomical location [28]. Alexander and Stuss [29] noticed the discrepancy between the studies’ results of executive functions using neuroimaging in healthy volunteers which exhibited frontal activation during executive tasks versus patients with brain injury, they noted the limitations of conventional tests of executive functions to be correlated with location of the brain damage assuming that these tests were not actually constructed to interpret structure/function relationships.
In respect to the other inflammatory markers, it was observed that there was no association between CRP level and cognitive performance as the patients showed almost the same cognitive performance whether they had positive or negative CRP. It could be attributed to measurement of low-sensitivity CRP in this study rather than high-sensitivity CRP (hs-CRP) assay, and this could not be adequately sensitive to estimate the blood levels of CRP within the normal range (< 10 mg/L); though, the development of high-sensitivity assays for CRP (hs-CRP) had permitted detection of even minor increase of CRP [30].
Erythrocyte sedimentation rate (ESR) is another marker of inflammation. ESR is a measure of the aggregation of erythrocytes, and their rate of sedimentation is determined by the increase in proteins, such as fibrinogen and globulins. As a consequence, ESR is subjected to less rapid change than other inflammatory markers such as CRP and accordingly is likely to be a more stable indicator of systemic inflammation [31].
In the present study, it was found that there was no significant correlation between ESR with cognitive performance of the patients. However, the patients with positive ESR showed poor cognitive performance than those patients with negative ESR but did not reach to a significant level in agreement with [32]. Kliper and colleagues (2013) [33] postulated that higher ESR values are associated with worse performance in cognitive tests that likely represent chronic systemic inflammatory processes, rather than a consequence of the acute event.
In this study, the patients presented with acute ischemic stroke were more depressed than the control group in concordance with [34, 35]. It could be attributed to either ischemic insults affecting neural circuits especially frontal-subcortical circuits, the pallidum, and caudate which are involved in mood regulation or a psychosocial hypothesis due to social and psychosocial stressors associated with stroke resulting in reactive depression [36].
Several studies had documented the association between post-stroke depression and cognitive functioning [37, 38]. We found a significant negative correlation between depression and cognitive impairment using MMSE. On the other hand, this study could not find a significant correlation between depression and MOCA or detailed cognitive assessment using TMT-B, COWAT-semantic, or COWAT-phonemic tests. This could be explained by the depression assessment that was performed so early within 48 h of acute ischemic stroke. However, the peak of post-stroke depression is 3 to 6 months following stroke [39].
This study had some limitations including the inability to use high-sensitivity CRP measurement as well as lack of evaluation of other domain-specific cognitive functions such as verbal, visuospatial memory, and information processing speed in the early stage of acute ischemic stroke. Finally, the application of the transcranial duplex would be beneficial if it had been used to detect the degree of the atherosclerotic changes and correlate with the serum level of IL-8.
Conclusion and recommendation
It was concluded that the executive function and verbal fluency were negatively correlated to IL8. So, regular assessment of serum level of IL 8 in patients with acute ischemic stroke especially those presented with cognitive impairment is recommended. Effectiveness of screening and monitoring procedures to detect inflammation and to prevent cognitive decline across acute and long-term settings were highly recommended.
Conflict of interest
The authors have no conflicts of interest to declare in relation to this study. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Availability of data and materials
The dataset cannot be publicly available due to institutional rules.
Abbreviations
- BDI:
-
Beck Depression Inventory
- CNS:
-
Central nervous system
- COWAT:
-
Controlled Oral Word Association Test
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- ELIZA:
-
Enzyme-linked immunoabsorbent assay
- ESR:
-
Erythrocyte sedimentation rate
- HDL:
-
High-density lipoprotein cholesterol
- IL:
-
Interleukin
- LDL:
-
Low-density lipoprotein cholesterol
- MMSE:
-
Mini-Mental State Examination
- MoCA:
-
Montreal Cognitive Assessment
- MRI:
-
Magnetic resonance imaging
- mRS:
-
Modified Rankin Scale
- NIHSS:
-
National Institute of Health Stroke Scale
- SPSS:
-
Statistical package for social science
- TMT:
-
Trail making test
- TNF:
-
Tumor necrosis factor
References
Chamorro A, Hallenbeck J. The harms and benefits of inflammatory and immune responses in vascular disease. Stroke. 2006;37(2):291–3.
Whiteley W, Chong WL, Sengupta A, Sandercock P. Blood markers for the prognosis of ischemic stroke: a systematic review. Stroke. 2009;40(5):e380–9.
Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network Vascular Cognitive Impairment Harmonization Standards. Stroke. 2006;37(9):2220–41.
Angelopoulos P, Agouridaki H, Vaiopoulos H, Siskou E, Doutsou K, Costa V, et al. Cytokines in Alzheimer’s disease and vascular dementia. Int J Neurosci. 2008;118(12):1659–72.
Danovska M, Peychinska D. Post-stroke cognitive impairment—phenomenology and prognostic factors. j imab - Annu Proceeding (Scientific Pap 2012;18, 3 290–297.
Kostulas N, Kivisäkk P, Huang Y, Matusevicius D, Kostulas V, Link H. Ischemic stroke is associated with a systemic increase of blood mononuclear cells expressing interleukin-8 mRNA. Stroke. 1998;29(2):462–6.
Folstein MF, Folstein SE, McHugh PR. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Rahman TTA, El Gaafary MM. Montreal Cognitive Assessment Arabic version: reliability and validity prevalence of mild cognitive impairment among elderly attending geriatric clubs in Cairo. Geriatr Gerontol Int. 2009;9(1):54–61. https://doi.org/10.1111/j.1447-0594.2008.00509.x.
Blackburn DJ, Bafadhel L, Randall M, Harkness KA. Cognitive screening in the acute stroke setting. Age Ageing. 2013;42(1):113–6.
National Institute for Health and Clinical Excellence. Stroke rehabilitation: long term rehabilitation after stroke. London: NICE; 2013. www.guidance.nice.org.uk/CG162
Corrigan JD, Hinkeldey NS. Relationships between parts A and B of the Trail Making Test. J Clin Psychol. 1987;43(4):402–9.
Stanczak DE, Stanczak EM, Awadalla AW. Development and initial validation of an Arabic version of the Expanded Trail Making Test: implications for cross-cultural assessment. Arch Clin Neuropsychol. 2001;16(2):141–9.
Ruff RM, Light RH, Parker SB, Levin HS. Benton Controlled Oral Word Association Test: reliability and updated norms. Arch Clin Neuropsychol. 1996;11(4):329–38.
Abdel Aziz K, Khater MS, Emara T, Tawfik HM, Rasheedy D, Mohammedin AS, et al. Effects of age, education, and gender on verbal fluency in healthy adult Arabic-speakers in Egypt. Appl Neuropsychol Adult. 2017;24(4):331–41.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Shen X, Li A, Zhang Y, Min Dong X, Shan T, Wu Y, et al. The effect of different intensities of treadmill exercise on cognitive function deficit following a severe controlled cortical impact in rats. Int J Mol Sci. 2013;14(11):21598–612.
Koyama A, O’Brien J, Weuve J, Blacker D, Metti AL, Yaffe K. The role of peripheral inflammatory markers in dementia and Alzheimer’s disease: a meta-analysis. J Gerontol A Biol Sci Med Sci. 2013;68(4):433–40.
Schaapsmeerders P, Maaijwee NAM, van Dijk EJ, Rutten-Jacobs LC, Arntz RM, Schoonderwaldt HC, et al. Long-term cognitive impairment after first-ever ischemic stroke in young adults. Stroke. 2013;44(6):1621–8.
Hurford R, Charidimou A, Fox Z, Cipolotti L, Werring DJ. Domain-specific trends in cognitive impairment after acute ischaemic stroke. J Neurol. 2013;260(1):237–41.
Mulder T, van Limbeek J, Donders R, Schoonderwaldt H, Hochstenbach J. Cognitive decline following stroke: a comprehensive study of cognitive decline following stroke*. J Clin Exp Neuropsychol (Neuropsychology, Dev Cogn Sect A). 1998;20(4):503–17.
Zhu Y, Chai YL, Hilal S, Ikram MK, Venketasubramanian N, Wong BS, et al. Serum IL-8 is a marker of white-matter hyperintensities in patients with Alzheimer’s disease. Alzheimers Dement. 2017;7:41–7.
Domac FM, Misirli H. The role of neutrophils and interleukin-8 in acute ischemic stroke. Neurosciences (Riyadh). 2008;13(2):136–41.
Narasimhalu K, Ang S, De Silva DA, Wong MC, Chang HM, Chia KS, et al. The prognostic effects of poststroke cognitive impairment no dementia and domain-specific cognitive impairments in nondisabled ischemic stroke patients. Stroke. 2011;42(4):883–8.
Baune BT, Ponath G, Golledge J, Varga G, Arolt V, Rothermundt M, et al. Association between IL-8 cytokine and cognitive performance in an elderly general population—the MEMO-study. Neurobiol Aging. 2008;29(6):937–44.
Shen Y-J, Wang W-A, Huang F-D, Chen J, Liu HY, Xia YL, et al. The use of MMSE and MoCA in patients with acute ischemic stroke in clinical. Int J Neurosci. 2016;126(5):442–7.
Chan E, Altendorff S, Healy C, Werring DJ, Cipolotti L. The test accuracy of the Montreal cognitive assessment (MoCA) by stroke lateralisation. J Neurol Sci. 2017;373:100–4.
Hom J, Reitan RM. Generalized cognitive function after stroke. J Clin Exp Neuropsychol. 1990;12(5):644–54.
Alexander M, Stuss DT. Frontal injury: impairments of fundamental processes lead to functional consequences. J Int Neuropsychol Soc. 2006;12(2):192–3.
Roberts WL, Sedrick R, Moulton L, Spencer A, Rifai N. Evaluation of four automated high-sensitivity C-reactive protein methods: implications for clinical and epidemiological applications. Clin Chem. 2000;46(4):461–8.
van Leeuwen MA, van Rijswijk MH. Acute phase proteins in the monitoring of inflammatory disorders. Baillieres Clin Rheumatol. 1994;8(3):531–52.
Kliper E, Bashat DB, Bornstein NM, Shenhar-Tsarfaty S, Hallevi H, Auriel E, et al. Cognitive decline after stroke: relation to inflammatory biomarkers and hippocampal volume. Stroke. 2013;44(5):1433–5.
Helmy AA, Naseer MMA, El SS, Nada MAF. Role of interleukin 6 and alpha-globulins in differentiating Alzheimer and vascular dementias. Neurodegener Dis. 2012;9(2):81–6.
Paolucci S, Gandolfo C, Provinciali L, Torta R, Toso V, DESTRO Study Group. The Italian multicenter observational study on post–stroke depression (DESTRO). J Neurol. 2006;253(5):556–62.
Townend BS, Whyte S, Desborough T, Crimmins D, Markus R, Levi C, et al. Longitudinal prevalence and determinants of early mood disorder post-stroke. J Clin Neurosci. 2007;14(5):429–34.
Whyte EM, Mulsant BH. Post stroke depression: epidemiology, pathophysiology, and biological treatment. Biol Psychiatry. 2002;52(3):253–64.
Leeds L, Meara RJ, Woods R, Hobson JP. A comparison of the new executive functioning domains of the CAMCOG-R with existing tests of executive function in elderly stroke survivors. Age Ageing. 2001;30(3):251–4.
Hackett ML, Anderson CS. Predictors of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(10):2296–301.
Alajbegovic A, Djelilovic-Vranic J, Nakicevic A, Todorovic L, Tiric-Campara M, Tiric-Campara M. Post stroke depression. Med Arch (Sarajevo, Bosnia Herzegovina). 2014;68(1):47–50.
Acknowledgements
The departments of clinical pathology and radiology should be acknowledged as they save no time and effort to bring this study to reality.
Funding
No funding resources were declared for this research.
Author information
Authors and Affiliations
Contributions
HAS was responsible for the conception of the work, analyzed and interpreted the data, and approved the final reversion of the work. LID was responsible for drafting the work, analyzed and interpreted the data, and communicated with the journal during the manuscript submission, peer review, and publication process. MMS was responsible for laboratory analysis of the collected data. AAA was responsible for data collection, interviewed the patients, and wrote the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Faculty of Medicine, Fayoum University Ethical Committee had approved the study and written informed consent was obtained from all the patients and control volunteers before study initiation. The research has been approved in the ethical committee, Faculty of Medicine, Fayoum University, on 8 July 2015 with reference number (16) and code (M-110).
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of financial interest to declare in relation to this study. We confirm that we have read the journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shaheen, H.A., Daker, L.I., Abbass, M.M. et al. Post-stroke executive dysfunction and verbal fluency negatively correlated to IL8. Egypt J Neurol Psychiatry Neurosurg 55, 45 (2019). https://doi.org/10.1186/s41983-019-0090-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-019-0090-y