Abstract
Background
Pneumococcal community-acquired pneumonia (P-CAP) is a major cause of morbidity and hospitalization. Several host genetics factors influencing risk of pneumococcal disease have been identified, with less information about its association with P-CAP. The aim of the study was to assess the influence of single nucleotide polymorphisms (SNP) within key genes involved in the innate immune response on the susceptibility to P-CAP and to study whether these polymorphic variants were associated with the severity and outcome of the episodes in a cohort of adult Caucasian patients.
Methods
Seventeen SNPs from 7 genes (IL-R1, IL-4, IL-10, IL-12B, NFKBIA, NFKBIE, NFKBIZ) were analyzed. For susceptibility, a case-control study including a cohort of 57 adult with P-CAP, and 280 ethnically matched controls was performed. Genetic influence on clinical severity and outcome was evaluated in a prospective observational study including all consecutive adult P-CAP patients from November 2015 to May 2017.
Results
The NFKBIA polymorphism rs696 and a haplotype combination were associated with susceptibility to P-CAP (OR = 0.62, p = 0.005 and OR = 0.63, p = 0.008, respectively). The SNP IL4 rs2227284 was associated with severe P-CAP (OR = 2.17, p = 0.04). IL-R1 (rs3917267) and IL-10 (rs3024509) variants were related with respiratory failure (OR = 3.31, p = 0.001 and OR = 0.18, p = 0.003, respectively) as well as several haplotype combinations in NFKBIA, NFKBIZ, IL-R1 and IL-10 (p = 0,02, p = 0,01, p = 0,001, p = 0,03, respectively). CURB-65 values were associated with the IL-10 rs3024509 variant (beta = − 0.4, p = 0.04), and with haplotype combinations of NFKBIZ and IL-10 (p = 0.05, p = 0.04, respectively). Genetic variants in IL-10 (rs3024509) and in IL-12B (rs730691) were associated with PSI values (beta = − 0.54, p = 0.01, and beta = − 0.28, p = 0.04, respectively), as were allelic combinations in IL-R1 (p = 0.02) and IL-10 (p = 0.01). Finally, several polymorphisms in the IL-R1 gene (rs13020778, rs2160227, & rs3917267) were associated with the time elapsed until clinical stability (beta = − 0.83, p = 0.03; beta = − 1, p = 0.02 and beta = 1.07, p = 0.008, respectively).
Conclusions
A genetic variant in NFKBIA was associated with susceptibility to P-CAP in adult Caucasian patients and genetic variants from key cytokines of the innate immune response (Il-4, IL-10, IL-R1 and IL-12B) and NF-κB inhibitors were associated with different phenotypes of severe P-CAP. If validated, these SNPs may help to identify people at risk of P-CAP or severe P-CAP on which preventive measures could be applied.
Similar content being viewed by others
Introduction
Community-acquired pneumonia (CAP) is a leading cause of hospitalization and mortality worldwide [1, 2]. Before SARS-Cov-2 pandemics, Streptococcus pneumoniae was the major CAP etiological agent and was responsible for a significant proportion of CAP mortality [3,4,5] The COVID-19 pandemic and subsequent lockdown measures have been associated with a large decline in invasive pneumococcal disease (IPD) [6, 7]. Nevertheless, IPD seems to be reaching values similar to the pre-pandemic period during the last year [8].
The risk of developing pneumococcal pneumonia (P-CAP) and the severity of the episodes are conditioned by the interplay between the host susceptibility, the virulence of the pathogen and the appropriateness of antimicrobial treatment, which will determine the characteristics and the magnitude of the inflammatory response [9,10,11]. Regarding host susceptibility, it is well known that age, comorbidities and vaccination status are related with the development and evolution of P-CAP [12,13,14,15]. Recently, it has also been suggested that the lung microbiota could play a role in P-CAP susceptibility and the intensity of the inflammatory response [9, 16]. However, it is still unknown why only a minority of the patients with nasopharyngeal pneumococcal colonization develop P-CAP, as the pathogenesis of pneumococcal pneumonia and its severity is not fully explained by these elements.
Genetic variability affecting the host immune response may also influence the susceptibility, the severity and outcome of P-CAP. At the end of the twentieth century, genetic factors were found to be a major determinant of susceptibility to infectious diseases, according to studies carried out in twins and adoptees [17, 18]. Genetic susceptibility to pneumococcal disease was first identified in extreme-phenotype studies in patients with recurrent invasive pneumococcal disease (IPD) [19]. During the last 20 years single nucleotide polymorphisms (SNP) of several genes encoding for key molecules in pathways of the innate and adaptive host immunity that potentially influence the susceptibility, the severity and outcome of pneumococcal disease have been identified.
Genetic variants of different cytokines of the innate immune response, such as IL-1b, IL1-R1, IL-4, IL-10 or IL-12B, have been associated with susceptibility to IPD in children of different ethnic groups [20]. Given the relevance of the nuclear factor κB (NF-κB), its potential association with susceptibility to IPD has been evaluated, reporting associations with an increased risk of IPD [17]. In a previous study published by our group evaluating the genetic susceptibility to IPD in as cohort of Caucasian adults, genetic variants in NFKBIA, NFKBIE and the genomic distribution of NFKBIZ and IL1-R1 were associated with IPD [21]. A recent meta-analysis showed that variants in CD14 and MBL2 genes were associated with susceptibility to pneumococcal disease, and there were no associations with the severity or outcome [22]. It should be noted that most of the studies performed with genetic variants in CD14 and those that found an association with the MBL2 SNPs were conducted in children and adults with IPD.
Regarding P-CAP, there is less evidence on the association of host genetic variants with the susceptibility and outcome of the episodes. Several polymorphisms in the genes encoding for MBL2, MASP2, SFTPA1, SFTPA2, SFTPD, FCGR2A and FCGR3A have been evaluated [23,24,25,26,27,28,29], finding that polymorphisms in SFTPA1, SFTPA2 and SFTPD were associated with susceptibility to P-CAP [26] and gnetic variants in FCGR2 were associated with bacteremic P-CAP. The association between the severity and outcome of P-CAP and the host polymorphisms in TLR2, TLR4, MBL2, MASP2, FCGR2A y FCGR3A, IL-10, TNF-α and IL-6 genes has also been evaluated [23,24,25,26, 28,29,30,31,32,33,34]. Allelic variants of MBL2 have been associated with mortality in a cohort of patients with sepsis and CAP [31] and with bacteremia [32]. A polymorphism in FCGR2 has been associated with the presence of bacteremia, acute renal failure, severe sepsis and adult respiratory distress syndrome (ARDS) [28]. In relation to cytokines, SNPs of IL-10 have been associated with septic shock [34] and IL-6 genetic variants have been associated with longer survival and lower risk of ARDS, multiorgan dysfunction and bacterial dissemination [30, 33]. However, it remains to be determined the potential association of the genetic variants of NF-κB and of other relevant cytokines in the innate immune response (pro-inflammatory and anti-inflammatory) in relation to susceptibility, severity, and outcome of P-CAP in adults.
The aims of the present study were: (1) to investigate the influence of genetic polymorphisms of seven candidate genes (IL-R1, IL-4, IL-10, IL-12B, NFKBIA, NFKBIE, NFKBIZ) involved in the innate immune response on the susceptibility to pneumococcal CAP (P-CAP) in a cohort of adult Caucasian patients with CAP and (2) to assess whether polymorphic variants of these genes were associated with the severity and outcome of the episodes.
Methods
Study design, setting and patients
Two different studies were conducted in Hospital Universitari Mútua Terrassa (HUMT), a 400-bed teaching hospital in Barcelona, Spain; the first to determine the influence of genetic polymorphisms on the susceptibility to P-CAP, and the second to assess their association with the severity and outcome of the episodes.
For susceptibility prediction, a case-control study was performed. Cases were 57 adults with P-CAP from a cohort of 124 patients with CAP prospectively included. Controls were 280 ethnically matched healthy adult blood donors from the same geographic area retrospectively collected from an historic database of our study group [14]. The demographic characteristics of the cases and controls population are summarized in Table 1. Comparisons including P-CAP cases (N = 57) and controls (N = 280) have ≥85% statistical power to detect genetic associations with moderate effect (d = 0.05, α = 0.95, two-sided)(calculated with G*Power v3.1.9.4).
Genetic influence on clinical severity and outcome was evaluated in a prospective observational study including all consecutive adult P-CAP patients attending the Emergency Department (ED) from November 2015 to May 2017. The adult P-CAP patients included in this prospective study were also the cases of the case-control study.
CAP was defined as an acute illness (symptoms lasting for ≤7 days) with the presence of a new infiltrate on a chest radiography associated with two or more of the following signs and symptoms: fever or hypothermia, dyspnoea, cough, sputum production, pleuritic chest pain, altered breath sounds on auscultation [3]. The exclusion criteria were: age < 18 years, nosocomial or bronchoaspiratory pneumonia, antibiotic treatment started at the ED > 4 h before the potential inclusion in the study, hospital admission during the previous 14 days or previous inclusion in the study. Only Caucasian subjects were analyzed to reduce genetic heterogeneity.
The study was conducted in accordance with the latest version of the Declaration of Helsinki and was approved by the hospital Ethics and Research Committee (record 11/15). Written informed consent obtained within 72 hours after admission was required for data collection [35].
Definitions
Pneumococcal CAP (P-CAP) was defined as described in a recently published article by the group [36] (Supplementary Material S1). Invasive pneumococcal disease (IPD) was defined as the presence of S. pneumoniae in blood cultures, pleural fluid or cerebrospinal fluid. The pneumonia severity index (PSI) [37] and the CURB score [38] were used to grade the severity of the CAP. The presence of respiratory failure was described as the presence of a PaO2/FiO2 ratio ≤ 300 or a pulse oximetric saturation (SpO2)/FiO2 ratio ≤ 315 [2]. Severe CAP was defined as the presence of septic shock, need of mechanical ventilation (MV) or Intensive Care Unit (ICU) admission.
Clinical evaluation at admission and follow up
Demographic and clinical variables were prospectively collected as described in reported in the supplementary material section (Supplementary Material S1). The time from symptoms onset to the ED visit (hours) and the time needed to reach clinical stability (days) were reported.
Before starting antibiotic therapy, conventional and molecular microbiological studies, chemistry and haematological tests, arterial blood gas sampling and chest radiography were performed (Supplementary Material S1).
Genetic characterisation of the sample
Whole blood samples were obtained from each study participant. DNA was extracted using a commercial kit (SQ Blood DNA Kit II, Omega Bio-Tek, USA) and following the manufacturer’s instructions. Samples were stored at -80C until required for study. Seventeen Tag SNPs (r2 = 0.8, minimum allele frequency ≥ 0.05) from 7 genes coding for proteins involved in the innate immunological response (ILR1, IL4, IL10, IL12B, NFKBIA, NFKBIE, NFKBIZ) were investigated. Genotypic characterisation of the samples was conducted using high-throughput techniques (Sequenom MassARRAY platform and iPLEX Gold reaction assays, CEGEN, Santiago de Compostela, Spain). Quality control analyses revealed ≥99% genotyping success rates for all SNPs and samples. All SNPs except ILR1 rs391726 were found in Hardy-Weinberg equilibrium. As a result, the ILR1 rs391726 was excluded from subsequent analyses.
Statistical analysis
Regression analyses comparing patients versus controls considering the genotypes, age and gender as predictor variables were performed for each individual SNP and for haplotype combinations within a gene to identify possible susceptibility risk genotypes. Further regression analyses considering response phenotypes (severe CAP, respiratory failure, PSI and CURB-65 scores, time to clinical stability) as dependent variables, and genotype, age, gender and Charlson score as predictor variables were conducted to elucidate associations with severity within the patient sample. All comparisons were conducted using the Plink statistical package (version 1.07-dos, Purcell et al. 2007).
Continuous variables are presented as means and standard deviation (SD) or medians and interquartile range (IQR) and categorical variables using counts and percentages. Univariate analyses were performed with t test or Mann-Whitney test for continuous variables and the Chi-square test or Fisher exact test for categorical variables, as appropriate.
Differences were considered statistically significant at the two-sided p < 0.05 level. Statistical analyses were performed using the STATA RELEASE 17 software (StataCorp LP, College Station, TX, USA). Multiple analyses corrections (Bonferroni) were calculated considering the number of polymorphisms investigated (17) and comparisons performed (7) to minimise false positives.
Results
Clinical and microbiological features of the study population
A total of 124 patients of Caucasian ethnicity with episodes of CAP and genetic data available were included in the study. An aetiological diagnosis was established in 84 episodes (67.7%). Fifty-seven patients had P-CAP (46%), 11 had another bacterial CAP (8.9%) and 16 had viral CAP (12.9%). Co-infection was present in 39 individuals (31.5%); of these, 29 were P-CAP patients with viral co-infection in 27 cases (16 rhinovirus, 3 influenza, 3 coronavirus, 2 respiratory syncytial virus and 1 metapneumovirus, parainfluenza and adenovirus) and bacterial co-infection in two cases (Haemophilus influenzae and Moraxella catarrhalis). Patient characteristics and comparison between P-CAP and non- P-CAP episodes are shown in Table 2.
The genetic studies were performed with the 57 P-CAP episodes. All of them received appropriate antimicrobial treatment, based on beta-lactam monotherapy in 12 episodes (21.1%), quinolones monotherapy in 9 (15.8%), beta-lactam + quinolones in 11 (19.3%) and beta-lactam + macrolide in 25 (43.8%). At admission, severe CAP was present in 12 patients (21.1%) and 32 (56.1%) presented respiratory failure. Thirty-one patients (54.4%) had a high-risk PSI (≥4) and 8 (14%) a high-risk CURB65 (≥3). No patient died during the study.
Host genetic variants and susceptibility to pneumococcal CAP
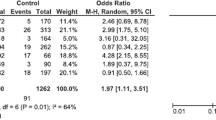
The results of the comparisons of the genetic distribution between cases and controls are summarized in Table 3.
A NFKB1A polymorphism, rs696, was significantly associated with susceptibility to CAP (p = 0.005) with the rs696-A variant more frequently observed in controls (0.43) than in patients (0.34). Haplotype analyses also revealed a similar association between a NFKB1A allele combination and susceptibility to pneumococcal CAP (p = 0.008). No other statistically significant association with susceptibility was observed.
Host genetic variants and severity of pneumococcal CAP
The results of the statistical analyses on severity data are summarized in Table 4.
A single nominal association was observed between an IL-4 rs2227284 variant and severe CAP (p = 0.04). No other significant single marker or haplotype association with severe CAP was detected. Two polymorphic variants in IL-R1 (rs3917267) and IL-10 (rs3024509) genes were associated with respiratory failure (p = 0.001, & p = 0.003, respectively) whereas several associations with haplotype combinations in NFKBIA (p = 0.02), NFKBIZ (p = 0.01), IL-R1 (p = 0.001) and IL-10 (p = 0.003) genes were also observed. CURB-65 values were marginally associated with the IL-10 rs3024509 variant (p = 0.04), and with haplotype combinations of NFKBIZ (p = 0.05), and IL-10 (p = 0.04). Single markers in IL-10 (rs3024509) and in IL-12B (rs730691) were associated with PSI values (p = 0.01& p = 0.04, respectively). Haplotype analyses also revealed significant associations between PSI and allelic combinations in IL-R1 (p = 0.002) and IL-10 (p = 0.01) genes. Finally, several polymorphisms in the IL-R1 gene (rs13020778, rs2160227, & rs3917267) were associated with the time elapsed until clinical stability (p = 0.03, 0.02, & 0.008, respectively). Additionally, a single marker in NFKBIE (rs730775) was also associated with time to stability (p = 0.02). Marginal associations were also observed between the time to clinical stability and haplotype combinations of IL-R1 (p = 0.04) and NFKBIE (p = 0.01) variants. It is important to note that none of the reported associations would survive multiple analyses corrections, except for the association between rs3917267 and respiratory failure (p = 0.02 after Bonferroni correction, Table 4).
Discussion
We investigated the influence of 17 SNPs within 7 immunological genes (IL-R1, IL-4, IL-10, IL-12B, NFKBIA, NFKBIE and NFKBIZ) on the susceptibility, severity, and prognosis of P-CAP, in a prospective cohort of adult Caucasian patients with P-CAP and controls matched by ethnicity.
The allele distribution of the NFKBIA polymorphism rs696 and its allele distribution were associated with susceptibility to P-CAP in the case-control study and several associations between SNPs in the IL-4, IL-10, IL-R1, IL-12B and NF-κB inhibitors genes and the different phenotypes of severity and outcome of P-CAP were found.
Regarding P-CAP susceptibility, the NFKBIA polymorphism, rs696, as well as one haplotype combination of the polymorphisms investigated within the gene, were associated with protection for the development of P-CAP. The rs696-A variant was more frequently observed in controls than in patients. No other statistically significant association with susceptibility was observed. In our study, the haplotype combination of the polymorphisms in different NF-κB inhibitors genes (NFKBIA,NFKBIE and NFKBIZ) have been associated with respiratory failure, time to clinical stability and higher punctuations in the CURB-65 score. Previous studies have found relation between NFKBIA polymorphisms and IPD susceptibility, but to our knowledge, the risk of P-CAP in relation to NFKB1A has nit been assessed. In a case-control study conducted in adult Caucasian patients [21] the allelic distribution of a variant (rs1050851) in the NFKBIA gene was associated with IPD susceptibility. Additionally, genetic variants in NFKBIA (rs3138053 and rs2233406) have been associated with protection from IPD in Caucasian patients [39]. Previous population-based case-control studies have also identified associations between susceptibility to IPD in Caucasian and African patients of all ages and common polymorphisms in the genes NFKBIE, NFKBIZ and NFKBIL2, each of which encodes an inhibitor of NF-κB [21, 40, 41]. Although the individual effect sizes are small, the risk variants are common in Europeans, suggesting that these polymorphisms may have a contribution to the burden of IPD in this population [42]. The nuclear factor NF-κB inflammatory pathway plays a key role in the host immune response to pneumococcal infection, and very rare genetic mutations in an NF-κB inhibitor cause immunodeficiency with severe bacterial infection [13, 39]. The genetic control of this major inflammatory pathway is extremely complex and incompletely understood. On one hand, impaired NF-κB activation is associated with immunodeficiency, but there is also evidence that increased levels of NF-κB activation are associated with a worse outcome from sepsis [13, 39].
In the present cohort, the IL-4 polymorphism rs2227284 was associated with the presence of severe CAP. The genotype distribution of the same SNP was found to be associated with IPD susceptibility [21], as well as other genetic variants of the Il-4 gen [22], but there is no previously published evidence on its relationship with severity, neither in patients with IPD nor with P-CAP. IL-4 is a major factor in B cell activation and differentiation and it plays an important role in the pathogenesis of sepsis and inflammation [21]. IL-4 and other cytokines were found associated with sepsis severity, organ failure and death in a cohort of patients with septic shock [43]. However, their exact role in the course of infection is still unknown.
A variant in the IL-10 gene, rs3024509, was associated with protection for respiratory failure and for higher CURB-65 and PSI values in this study. Haplotype combinations in the IL-10 gene were also protective for respiratory failure and highest punctuations in PSI score. Our results are in line with a previous study performed in a cohort of patients with IPD and pneumonia [34], in which an IL-10 polymorphism was also associated with severity, with the development of septic shock due to an enhanced IL-10 release. IL-10 is an anti-inflammatory cytokine that plays an important role in the innate immune response. It is able to counterbalance the potentially harmful effects of the proinflammatory response, playing a central role in tissue resilience and contributing to lung homeostasis [9]. However, the IL-10 excess may induce immunosuppression in bacterial sepsis and increases mortality in P-CAP due to bacterial clearance impairment [34, 44]. IL-10 serum levels have been correlated with the severity and the clinical outcome in sepsis, septic shock and CAP [34] and with a fulminant course of S. pneumoniae infection in a murine model of P-CAP [45].
A polymorphic variant in the IL-R1 gene, rs3917267, was associated with respiratory failure and time to clinical stability. Moreover, haplotype combinations in this gene were associated with risk of respiratory failure, time to clinical stability and higher CURB-65 and PSI values. Although previous studies have reported an association between genetic variants of the IL-R1 gene and IPD risk [21, 46], there is no published evidence about their relation with the severity or the prognosis of P-CAP. IL-1 plays a critical role in the host response to pneumococcal infections. Its effects are controlled by two inhibitors, the IL-R1 antagonist is one of them The IL-R1 has anti-inflammatory properties and its deficiency in mice has been related with pneumococcal meningitis, higher mortality and enhanced growth of S. pneumoniae [47]. The regulation of IL-1 and IL-R1 is complex with a delicate balance between the beneficial effects of modulating bacterial clearance and the detrimental effects of exacerbating the inflammatory response [46].
In addition, a single polymorphism in IL-12B gene, rs730691, was associated with PSI values in this cohort. No previous associations have been described between the IL-12B gene and the severity of P-CAP episodes. IL-12 is a proinflammatory cytokine that promotes the activation of the cellular immunity by activating T lymphocytes. More studies are needed on the role of the inflammatory pathway of these cytokines to understand the impact of genetic polymorphisms in the severity of P-CAP.
The main limitations of the present study are: (a) The sample size is moderate-low for candidate-gene association studies, although it is a well-characterized cohort of P-CAP patients. (b) The proportion of patients with severe CAP was relatively small and mortality was extremely low, perhaps due to a selection bias. (c) The statistically significant associations found were marginal and did not withstand Bonferroni corrections for multiple analyses (p > 0.05) except for one finding. However, Bonferroni corrections are too conservative and consider genetic variants in the same genes as independent events and may lead to false negatives. (d) The functional expression of the genetic associations is not described. Finally, our study was conducted in an specific geographical area including only Caucasian patients, and the results cannot be extrapolated to other settings or ethnicities.
In conclusion, in the present study we describe a novel association between a genetic polymorphism in the NFKBIA gene and susceptibility to P-CAP in adult Caucasian patients and we find evidence that genetic variants from key cytokines of the innate immune response (Il-4, IL-10, IL-R1 and IL-12B) and NF-κB inhibitors are associated with the presence of severe CAP, respiratory failure or higher punctuations in CURB-65 or PSI scores in patients with P-CAP. These findings, if validated, may help to identify people at risk of P-CAP and patients at risk of severe forms of P-CAP on which preventive measures could be applied.
Availability of data and materials
All data generated or analysed during the current study are available from the corresponding author on reasonable request.
References
Garau J, Calbo E. Community-acquired pneumonia. Lancet. 2008;371:455–8. https://doi.org/10.1016/S0140-6736(08)60216-0.
Mandell LA. Community-acquired pneumonia: An overview. Postgrad Med. 2015;127:607–15. https://doi.org/10.1080/00325481.2015.1074030.
Musher DM, Mandell LA, Niederman MS, File TM, Dowell SF, Torres A, et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clin Infect Dis. 2007;44:S27–72. https://doi.org/10.1086/511159.
Rozenbaum MH, Pechlivanoglou P, Van Der Werf TS, Lo-Ten-Foe JR, Postma MJ, Hak E. The role of Streptococcus pneumoniae in community-acquired pneumonia among adults in Europe: A meta-analysis. Eur J Clin Microbiol Infect Dis. 2013;32:305–16. https://doi.org/10.1007/s10096-012-1778-4.
Shoar S, Musher DM. Etiology of community-acquired pneumonia in adults: a systematic review. Pneumonia. 2020;12 https://doi.org/10.1186/s41479-020-00074-3.
Shaw D, Abad R, Amin-Chowdhury Z, Bautista A, Bennett D, Broughton K, et al. Trends in invasive bacterial diseases during the first 2 years of the COVID-19 pandemic: analyses of prospective surveillance data from 30 countries and territories in the IRIS Consortium. Lancet Digit Heal. 2023;5:e582–93. https://doi.org/10.1016/S2589-7500(23)00108-5.
Amin-Chowdhury Z, Alano F, Mensah A, Sheppard CL, Litt D, Fry NK, et al. Impact of the COVID-19 Pandemic on Invasive Pneumococcal Disease and Risk of Pneumococcal Coinfection with SARS-CoV-2: prospective national cohort study, England. Clin Infect Dis. 2021;72(5):e65–75.
Perniciaro S, Van Der Linden M, Weinberger DM. Reemergence of Invasive Pneumococcal Disease in Germany During the Spring and Summer of 2021. Clin Infect Dis. 2022;75:1149–53. https://doi.org/10.1093/cid/ciac100.
Torres A, Cilloniz C, Niederman MS, Menéndez R, Chalmers JD, Wunderink RG, et al. Pneumonia. Nat Rev Dis Prim. 2021;7 https://doi.org/10.1038/s41572-021-00259-0.
Aspa J, Rajas O, de Castro FR, Huertas MC, Borderías L, Cabello FJ, et al. Impact of initial antibiotic choice on mortality from pneumococcal pneumonia. Eur Respir J. 2006;27:1010–9. https://doi.org/10.1183/09031936.06.00126004.
Weinberger DM, Simonsen L, Jordan R, Steiner C, Miller M, Viboud C. Impact of the 2009 influenza pandemic on pneumococcal pneumonia hospitalizations in the United States. J Infect Dis. 2012;205:458–65. https://doi.org/10.1093/infdis/jir749.
Naucler P, Darenberg J, Morfeldt E, Örtqvist Å, Normark BH. Contribution of host, bacterial factors and antibiotic treatment to mortality in adult patients with bacteraemic pneumococcal pneumonia. Thorax. 2013;68:571–9. https://doi.org/10.1136/thoraxjnl-2012-203106.
Calbo E, Garau J. Of mice and men: innate immunity in pneumococcal pneumonia. Int J Antimicrob Agents. 2010;35:107–13. https://doi.org/10.1016/j.ijantimicag.2009.10.002.
Sangil A, Xercavins M, Rodríguez-Carballeira M, Andrés M, Riera M, Espejo E, et al. Impact of vaccination on invasive pneumococcal disease in adults with focus on the immunosuppressed. J Infect. 2015;71:422–7. https://doi.org/10.1016/j.jinf.2015.07.004.
Pelton SI, Shea KM, Farkouh RA, Strutton DR, Braun S, Jacob C, et al. Rates of pneumonia among children and adults with chronic medical conditions in Germany. BMC Infect Dis. 2015;15:1–8. https://doi.org/10.1186/s12879-015-1162-y.
Dietl B, Henares D, Boix-Palop L, Muñoz-Almagro C, Garau J, Calbo E. Related Factors to Streptococcus pneumoniae Invasive Infection and Clinical Manifestations: The Potential Role of Nasopharyngeal Microbiome. Front Med. 2021;8:1–10. https://doi.org/10.3389/fmed.2021.650271.
Chapman SJ, Hill AVS. Human genetic susceptibility to infectious disease. Nat Rev Genet. 2012;13:175–88. https://doi.org/10.1038/nrg3114.
Classen DC, Evans RS, et al. The New England Journal of Medicine Downloaded from www.nejm.org at UNIVERSITY OF MICHIGAN on December 9, 2010. For personal use only. No other uses without permission. Copyright © 1992 Massachusetts Medical Society. All rights reserved. N Engl J Med. 1992;326:653–7.
Brouwer MC, de Gans J, Heckenberg SG, Zwinderman AH, van der Poll T, van de Beek D. Host genetic susceptibility to pneumococcal and meningococcal disease: a systematic review and meta-analysis. Lancet Infect Dis. 2009;9:31–44. https://doi.org/10.1016/S1473-3099(08)70261-5.
Lingappa JR, Dumitrescu L, Zimmer SM, Lynfield R, McNicholl JM, Messonnier NE, et al. Identifying host genetic risk factors in the context of public health surveillance for invasive pneumococcal disease. PLoS One. 2011;6 https://doi.org/10.1371/journal.pone.0023413.
Betriu AS, Arranz MJ, Güerri-Fernández R, Pérez M, Monzón H, Payeras A, et al. Genetic susceptibility to invasive pneumococcal disease. Infect Genet Evol. 2018;59:126–31. https://doi.org/10.1016/j.meegid.2018.01.024.
Kloek AT, Brouwer MC, van de Beek D. Host genetic variability and pneumococcal disease: a systematic review and meta-analysis. BMC Med Genom. 2019;12:130. https://doi.org/10.1186/s12920-019-0572-x.
Endeman H, Herpers BL, De Jong BAW, Voorn GP, Grutters JC, Van Velzen-Blad H, et al. Mannose-binding lectin genotypes in susceptibility to community-acquired pneumonia. Chest. 2008;134:1135–40. https://doi.org/10.1378/chest.08-0642.
Garcia-Laorden MI, Sole-Violan J, de Castro FR, Aspa J, Briones ML, Garcia-Saavedra A, et al. Mannose-binding lectin and mannose-binding lectin-associated serine protease 2 in susceptibility, severity, and outcome of pneumonia in adults. J Allergy Clin Immunol. 2008:122. https://doi.org/10.1016/j.jaci.2008.05.037.
Mills TC, Chapman S, Hutton P, Gordon AC, Bion J, Chiche JD, et al. Variants in the mannose-binding lectin gene MBL2 do not associatewith sepsis susceptibility or survival in a large european cohort. Clin Infect Dis. 2015;61:695–703. https://doi.org/10.1093/cid/civ378.
García-Laorden MI, Rodríguez de Castro F, Solé-Violán J, Rajas O, Blanquer J, Borderías L, et al. Influence of genetic variability at the surfactant proteins A and D in community-acquired pneumonia : a prospective , observational , genetic study. Crit Care. 2011;15:R57. https://doi.org/10.1186/cc10030.
Endeman H, Cornips MCA, Grutters JC, Van Den Bosch JM, Ruven HJT, Van Velzen-Blad H, et al. The Fcγ receptor IIA-R/R131 genotype is associated with severe sepsis in community-acquired pneumonia. Clin Vaccine Immunol. 2009;16:1087–90. https://doi.org/10.1128/CVI.00037-09.
Solé-Violán J, García-Laorden MI, Marcos-Ramos JA, Rodríguez De Castro F, Rajas O, Borderías L, et al. The Fcγ receptor IIA-H/H131 genotype is associated with bacteremia in pneumococcal community-acquired pneumonia. Crit Care Med. 2011;39:1388–93. https://doi.org/10.1097/CCM.0b013e31820eda74.
García-Loarden MI, Rodríguez de Castro F, Solé-Violán J, Payeras A, Briones ML, Borderías L, et al. The role of mannose-binding lectin in pneumococcal infection. Eur Respir J. 2013;41:131–9. https://doi.org/10.1183/09031936.00174111.
Martín-Loeches I, Solé-Violán J, Rodríguez de Castro F, García-Loarden MI, Borderías L, Blanquer J, et al. Variants at the promoter of the interleukin-6 gene are associated with severity and outcome of pneumococcal community-acquired pneumonia. Intrensive Care Med. 2012:256–62. https://doi.org/10.1007/s00134-011-2406-y.
Garnacho-Montero J, García-Cabrera E, Jiménez-Álvarez R, Díaz-Martín A, Revuelto-Rey J, Aznar-Martín J, et al. Genetic variants of the MBL2 gene are associated with mortality in pneumococcal sepsis. Diagn Microbiol Infect Dis. 2012;73:39–44. https://doi.org/10.1016/j.diagmicrobio.2012.02.002.
Pérez-Castellano M, Peñaranda M, Payeras A, Milà J, Riera M, Vidal J, et al. Mannose-binding lectin does not act as an acute-phase reactant in adults with community-acquired pneumococcal pneumonia. Clin Exp Immunol. 2006:228–34. https://doi.org/10.1111/j.1365-2249.2006.03140.x.
Schaaf B, Rupp J, Mu M, Kruse J, Boehmke F, Maass M, et al. The interleukin-6 ÿ 174 promoter polymorphism is associated with extrapulmonary bacterial dissemination in Streptococcus pneumoniae infection. Cytokine. 2005;31:324–8. https://doi.org/10.1016/j.cyto.2005.05.008.
Schaaf BM, Boehmke F, Esnaashari H, Seitzer U, Kothe H, Maass M, et al. Pneumococcal Septic Shock Is Associated with the Interleukin-10 – 1082 Gene Promoter Polymorphism. Am J Respir Crit Care Med. 2003;168:476–80. https://doi.org/10.1164/rccm.200210-1164OC.
Postma DF, van Werkhoven CH, van Elden LJR, Thijsen SFT, Hoepelman AIM, Kluytmans JAJW, et al. Antibiotic Treatment Strategies for Community-Acquired Pneumonia in Adults. N Engl J Med. 2015;372:1312–23. https://doi.org/10.1056/NEJMoa1406330.
Boix-Palop L, Obradors M, Xercavins M, Picó-Plana E, Canales L, Dietl B, et al. Improvement of pneumococcal pneumonia diagnosis using quantitative real-time PCR targeting lytA in adult patients: a prospective cohort study. Clin Microbiol Infect. 2022;28:138.e1–7. https://doi.org/10.1016/j.cmi.2021.05.049.
Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–50.
Lim WS, Van Der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: An international derivation and validation study. Thorax. 2003;58:377–82. https://doi.org/10.1136/thorax.58.5.377.
Chapman SJ, Khor CC, Vannberg FO, Frodsham A, Walley A, Maskell NA, et al. IkappaB Genetic Polymorphisms and Invasive Pneumococcal Disease. Am J Respir Crit Care Med. 2007;176(2):18–7. https://doi.org/10.1164/rccm.200702-169OC.
Lundbo LF, Harboe ZB, Clausen LN, Hollegaard MV, Sørensen HT, Hougaard DM, et al. Genetic Variation in NFKBIE Is Associated With Increased Risk of Pneumococcal Meningitis in Children. EBioMedicine. 2016;3:93–9. https://doi.org/10.1016/j.ebiom.2015.11.048.
Chapman SJ, Khor CC, Vannberg FO, Rautanen A, Walley A, Segal S, et al. Common NFKBIL2 polymorphisms and susceptibility to pneumococcal disease : a genetic association study. Crit Care. 2010;14:R227. https://doi.org/10.1186/cc9377.
Chapman SJ. Can your genes make you more prone to pneumococcal disease ? Expert Rev Anti Infect Ther. 2010;8:967–72.
Bozza FA, Gomes RN, Japiassú AM, Soares M, Castro-Faria-Neto HC, Bozza PT, et al. Macrophage migration inhibitory factor levels correlate with fatal outcome in sepsis. Shock. 2004;22:309–13. https://doi.org/10.1097/01.shk.0000140305.01641.c8.
Van Der Poll T, Marchant A, Keogh CV, Goldman M, Lowry SF. Interleukin-10 impairs host defense in murine pneumococcal pneumonia. J Infect Dis. 1996;174:994–1000. https://doi.org/10.1093/infdis/174.5.994.
Temple SEL, Lim E, Cheong KY, Almeida CAM, Price P, Ardlie KG, et al. Alleles carried at positions −819 and −592 of the IL10 promoter affect transcription following stimulation of peripheral blood cells with Streptococcus pneumoniae. Immunogenetics. 2003;55:629–32. https://doi.org/10.1007/s00251-003-0621-6.
Carrol ED, Payton A, Payne D, Miyajima F, Chaponda M, Mankhambo LA, et al. The IL1RN Promoter rs4251961 Correlates with IL-1 Receptor Antagonist Concentrations in Human Infection and Is Differentially Regulated by GATA-1. J Immunol. 2011;186:2329–35. https://doi.org/10.4049/jimmunol.1002402.
Zwijnenburg PJG, van der Poll T, Florquin S, Roord JJ, van Furth AM. IL-1 Receptor Type 1 Gene-Deficient Mice Demonstrate an Impaired Host Defense Against Pneumococcal Meningitis. J Immunol. 2003;170:4724–30. https://doi.org/10.4049/jimmunol.170.9.4724.
Acknowledgements
The authors would like to thank the collaboration of the healthcare workers in the Emergency Department of the Hospital Universitari Mútua Terrassa for their important and continuous hardwork.
Funding
This study was supported by the Fondo de Investigación en Salud of the Instituto de Salud Carlos III, with the grant n° PI 14/01898 from the Ministerio de Ciencia, Innovación y Universidades of Spain. This study has been funded by a 2023 CAREer Grant from the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) to LBP.
Author information
Authors and Affiliations
Contributions
Conceptualization, E.C., M.J.A and L.B.P; data curation, L.B.P, B.D, A.S; formal analysis, L.B.P.; funding acquisition, E.C; investigation, L.B.P., M. L. A, B.D, A. S, M.X.; methodology, E.C., M.J.A and L.B.P.; project administration, L.B.P, M.J.A.; resources, M.J.A, M.X, J.P.; supervision, E.C., M.J.A.; writing—original draft, L.B. P., M.J.A; writing—review and editing, L.B.P, M.J.A, E.C. All authors have read and agreed to the published.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the latest version of the Declaration of Helsinki and was approved by the hospital Ethics and Research Committee (record 11/15). Written informed consent obtained within 72 hours after admission was required for data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boix-Palop, L., Arranz, M.J., Sangil, A. et al. Host genetic variants associated with susceptibility and severity of pneumococcal pneumonia in adult patients. Pneumonia 15, 18 (2023). https://doi.org/10.1186/s41479-023-00120-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41479-023-00120-w