Abstract
Streptococcus pneumoniae (Spn) is a major public health problem, as it is a main cause of otitis media, community-acquired pneumonia, bacteremia, sepsis, and meningitis. Acute episodes of pneumococcal disease have been demonstrated to cause organ damage with lingering negative consequences. Cytotoxic products released by the bacterium, biomechanical and physiological stress resulting from infection, and the corresponding inflammatory response together contribute to organ damage accrued during infection. The collective result of this damage can be acutely life-threatening, but among survivors, it also contributes to the long-lasting sequelae of pneumococcal disease. These include the development of new morbidities or exacerbation of pre-existing conditions such as COPD, heart disease, and neurological impairments. Currently, pneumonia is ranked as the 9th leading cause of death, but this estimate only considers short-term mortality and likely underestimates the true long-term impact of disease. Herein, we review the data that indicates damage incurred during acute pneumococcal infection can result in long-term sequelae which reduces quality of life and life expectancy among pneumococcal disease survivors.
Similar content being viewed by others
Introduction
Streptococcus pneumoniae (Spn) is the most common etiological agent of community-acquired pneumonia (CAP), bacteremia, and sepsis; in low or low-middle-income countries with no immunization schedule it is also the leading cause of meningitis [1,2,3]. Accordingly, the pneumococcus is the leading cause of infectious death in both children and older adults [4,5,6,7,8]. Spn is also a common cause of non-life-threatening infections including sinusitis, otitis media, and bronchitis which are associated with major personal and socio-economic costs [9,10,11,12,13]. This opportunistic, Gram-positive bacterium most often resides asymptomatically in the nasopharynx but can be aspirated into the lungs to cause pneumonia [8]. From the airway, the pneumococcus can gain access to the bloodstream and spread to other sites, where it can cause disseminated organ damage [14,15,16]. Young children with underdeveloped immune systems, those with immunodeficiencies, adults over the age of 65 with multiple comorbidities, and individuals experiencing or who have recently experienced a respiratory viral infection have increased susceptibility to both becoming infected with and dying from pneumococcal disease [5, 16,17,18].
It is worth noting that in most pneumococcal pneumonia cases, i.e., those that do not require hospitalization, there is typically no long-term negative effect. Among those with severe pneumonia, and despite the dense consolidation that can occur, the lungs radiologically return to normal by 2–4 months and most patients recover fully from all residual symptoms within 6 to 18 months [19, 20]. Yet, pneumococcal infections can exacerbate underlying pulmonary diseases, such as COPD. They can also cause a tremendous amount of system-wide damage. This damage is attributable to cytotoxic factors released by the bacterium, physiological stress put on the body during the infection, and an overzealous inflammatory response [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]. Strikingly, individuals previously hospitalized for invasive pneumococcal disease typically die sooner than would be expected based on census data; with nearly a decade of mean years of life lost being [37]. This reduction in life expectancy can be attributed to systemic organ damage during the infection [37, 38].
Sir William Osler was the first to describe the triad of pneumonia, endocarditis, and meningitis, and observed the presence of ‘micrococci’ in the affected tissues and blood in histological specimens at post-mortem examination; these ‘micrococci’ were later classified by Robert Austrian as S. pneumoniae, which is how this triad of disease developed the eponym of Austrian syndrome [39,40,41]. Austrian’s work highlighted the systemic consequences of pneumococcal pneumonia and that severe damage occurred when bacteria gained access to the bloodstream and invaded tissues [39, 41]. In accordance with this, Spn is well documented to cause acute damage to the middle ear, lungs, heart, and kidneys [9, 42,43,44,45,46,47]. Should the bacterium gain access to the central nervous system (CNS), there are especially devastating consequences to the affected individual with a case fatality rate of 30% in developed countries and up to 50% in lower-income countries [1, 7, 21, 22, 48,49,50,51,52]. As is discussed below, the damages incurred during pneumococcal infections persist well after the resolution of the acute infection and increase the risk for morbidity and mortality in convalescence. Many reviews on pathogenesis and the immunological events that take place during pneumococcal infection are available, but few have focused on the long-term consequences of this disease. This review examines the role the pneumococcus plays in tissue and organ damage during infection and the long-term sequelae associated with this damage. Sir William Osler famously called Spn “the Captain of all the men of death”; herein, we state that “the Captain lingers”.
Acute pneumonia and invasive disease are highly inflammatory episode
Pneumococci that are aspirated into the lungs first encounter the mucous layer, which serves as a protective mechanical barrier for the mucosal epithelium, and sentinel alveolar macrophages (AMs). These early defenses serve to prevent the dissemination of pneumococci and initiate innate immune signaling and host cell activation [53, 54]. The mucous layer lining the epithelium traps bacteria in its sticky matrix and contains both microbicidal and microbiostatic products such as defensins, lactoferrin, lysozyme, matrix metalloproteinases (MMPs), antibodies, surfactant, complement proteins, and C-reactive protein (CRP) [54,55,56,57,58,59,60,61]. Upon contact with Spn, secretory IgA and complement proteins, C3 and C5a, aggregate and opsonize Spn, respectively, facilitating physical clearance and phagocytosis of the bacteria [56, 62]. Lysozyme, lactoferrin, b-defensin peptides, and LL-37 are directly bactericidal. However, the death of pneumococci, either by the host or the autolysis of itself, not only results in bacterial clearance but also in the release of inflammatory agents such as the pore-forming toxin, pneumolysin, and bacterial cell wall particles that intensify local inflammation [24,25,26, 54, 61, 63,64,65,66,67,68,69,70].
Pathogen recognition receptors (PRRs), including but not limited to Toll-like receptors (TLRs) and NOD-like receptors (NLRs), on both somatic airway epithelial cells and innate immune cells, particularly AMs, recognize pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) present during infection, triggering an inflammatory response to clear the pneumococcus [64]. TLRs-1, 2, 6, and 9 play a critical role in initiating the innate immune response, and their activation of B and T cells also promotes an adaptive immune response [67,68,69]. TLR-1/2 and TLR2/6 heterodimers expressed on host cells recognize teichoic acids and lipoproteins that are part of Spn’s cell wall [67,68,69, 71]. TLR9 detects DNA with unmethylated CpG motifs present in bacterial but not mammalian DNA [72]. TLR-4 is activated by complement and has been reported to detect Spn’s pneumolysin, but conflicting results have been published [64, 68, 73].
The binding of TLRs to their ligands engages adaptor molecules that transduce signals to activate proinflammatory signaling cascades including mitogen-activated protein kinases (MAPKs) and nuclear factor kappa B (NF-κB) [68, 71, 73, 74]. Upon TLR activation, sentinel AM in the airway rapidly signal to epithelial cells locally with cytokines and recruit neutrophils and monocytes via chemokines including tumor necrosis factor (TNF), interleukin (IL)-1β, IL-6, IL-8, CXCL1, CXCL2, and CCL2 [75,76,77,78,79]. Considerable evidence shows that Spn can invade host cells at low frequency, in which case the PAMPs from internalized Spn can interact with another class of PRRs, NLRs, that are found in the cytoplasm of host cells. NLRs have been shown to recognize peptidoglycan motifs via NOD1 and NOD2 which activate signaling cascades and NLRP3 that serves as a component of the inflammasome [80,81,82,83]. Upon NLRP3 detection of PAMPs or DAMPs, NLRP3 oligomerizes with other components to form inflammasomes, which in turn cleave the pro-forms of IL-1β and IL-18 to be released [83, 84]. IL-1β induces the production of chemoattractants CXCL1, CXCL2, and IL-17A by lung epithelial and Th17 cells that enhance the recruitment of macrophages and neutrophils [32, 85, 86]. Notably, since the pneumococcus is encapsulated and therefore resistant to phagocytosis and intracellular killing, this inflammatory response does not necessarily result in bacterial clearance and can worsen disease [87, 88].
When pneumococci kill host cells there is a release of alarmins and DAMPs including S100A8/9, HSP60, IL-1α, and IL-33, promoting the infiltration and activation of neutrophils and circulating monocytes which further the local immune response [32, 89, 90]. In professional antigen-presenting cells, alarmins have been shown to induce upregulation of surface costimulatory (CD80 and CD86) and MHC (class I and II) molecules, enhancement of antigen presentation to lymphocytes inducing adaptive immune responses, and the release of proinflammatory cytokines and chemokines, triggering a positive feedback loop on pro-inflammatory innate immune responses [90]. Additionally, alarmins can trigger mast cell and basophil activation and the release of histamine, prostaglandins, and leukotrienes thus, increasing vascular permeability and attracting neutrophils [90]. Bactericidal peptides and proteins released into the milieu include matrix metalloproteinases (MMPs); these zinc-dependent enzymes degrade extracellular matrix components, which then serve as alarmins, (e.g. hyaluronan) and thereby further increase the magnitude of the inflammatory response [58, 91,92,93,94].
Polymorphonuclear leukocytes (PMNs) are effectors of bacterial clearance and help to control the infection, even though they may be unable to phagocytize encapsulated pneumococci efficiently without opsonizing antibodies. They do this via the release of DNA and the formation of neutrophil extracellular traps (NETs). NETs trap and kill Spn with antimicrobial proteins associated with the DNA such as MMPs and serine proteases [31, 36, 59, 60]. Neutrophils also release agents that not only elicit inflammation but also cause tissue damage. These include reactive oxygen and nitrogen species, myeloperoxidase (MPO), and granule serine proteases such as cathepsin G, proteinase 3, and neutrophil elastase [32, 36, 57, 60]. The neutrophil influx necessary to fight off airway infection must be scaled appropriately to avoid excessive or prolonged inflammation [31, 94, 95]. Excessive inflammation sets the stage for the loss of alveolar-capillary barrier integrity, infiltration of additional neutrophils and monocytes, and initiation of a positive feed-forward pro-inflammatory loop.
During the early stages of pneumonia, the cytokine response to Spn is largely compartmentalized within the lung [96, 97]. However, as disease develops and becomes more severe, the inflammatory response in the airway becomes systemic with pro-inflammatory cytokines also becoming elevated in the blood of pneumonia patients [97,98,99,100,101]. Notably, a robust early response is vital, and patients who succumb to pneumonia have higher levels of cytokines and acute phase reactants in the serum versus the airway, indicating that failure to generate a robust local immune response at the site of initial infection contributes to systemic inflammation and overall disease severity [38, 96, 98]. TNF is one of the earliest and most important mediators of this local inflammatory response. TNF initiates inflammatory signaling cascades that induce a second wave of pro- and anti-inflammatory cytokines to advance the immune response [102]. TNF can also be damaging by causing increased neutrophil accumulation and activation, vascular dysfunction, and induction of necroptosis, a form of programmed cell death. [102,103,104,105,106]. Accordingly, levels of TNF in serum and the CNS correlate with overall disease severity and mortality [103, 107]. Patients who delayed going to the hospital > 48 h past the onset of symptoms had higher serum TNF levels, lower blood pressure (< 90 mmHg), and lower oxygen saturation levels at the time of admission; all of which are associated with poorer outcomes during infection [98]. Bacteremic patients have higher levels of TNF circulating in the serum compared to pneumonia alone [100, 108, 109]. Nearly all patients admitted to the hospital have a systemic inflammatory response, as measured by detectable IL-6 (98% in a study by Örtqvist et al.) and CRP; moreover, higher levels are associated with poorer outcomes [110, 111]. Compared to survivors, patients who died had higher levels of proinflammatory cytokines TNF, IL-6, IL-8, IL-10, and acute phase reactants (CRP) in serum [38, 96,97,98, 112]. Along such lines, polymorphisms in human genes involved in the inflammatory response to infection such as chemokines/cytokines (TNF, IL-6, IL-1 family, macrophage migration inhibitory factor, and IL-10), pattern recognitional molecules (TLRs and Mannose-binding lectin (MBL)), local host defense of the lung (surfactant protein), and coagulation cascades (plasminogen-activator-inhibitor (PAI)-1 and factor V) have been associated with susceptibility to pneumonia and outcomes including sepsis, IPD, and mortality [113,114,115,116,117,118,119,120,121,122,123,124,125,126,127]. This is due to an impaired ability to respond to the infection, but in other instances a far too exuberant response.
In summation, an inflammatory response is needed to fight off the potentially deadly pneumococcal infection. The immune system creates a highly inflammatory environment at the site of infection characterized by the recruitment of immune cells resulting in lung consolidation [128]. As the infection progresses, epithelial cell death and the subsequent loss of vascular integrity results in the leakage of pro-inflammatory bacterial products and cytokines into the systemic circulation that contributes to disease pathology. Scaling an appropriate immune response to avoid excessive inflammation is important to prevent damage from occurring, as an overzealous inflammatory response results in impaired oxygen exchange in the airway, damage contributing to organ injury, and increases the likelihood of poor outcomes, such as widespread organ failure and mortality [95, 129].
Organ damage occurs during acute infection with lasting consequences
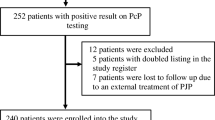
Sites of pneumococcal infection include the middle ear, lower airway, circulation, invaded organs, and the CNS. The consequences of severe infection at these locations can significantly and permanently alter human health (Fig. 1). Notably, work done in animal models shows unequivocally that bacterial-derived factors, as well as a dysregulated immune response, together contribute to this damage.
Consequences of pneumococcal disease during acute infection occur system-wide. Acute pneumococcal pneumonia and invasive disease can be life-threatening. It can also result in organ damage that results in debilitating long-term sequelae. These sequelae, in turn, contribute to loss of physiological resilience and early mortality
Middle ear
Clinical aspects & pathophysiology
Otitis media is a common malady that affects the majority of children, with 80% having at least one episode by 10 years of age [11]. New infections often arise after viral infections or allergic reactions, as congestion obstructs the eustachian tube at its most narrow point, leading to the accumulation of middle ear secretions which create a niche for Spn to multiply within [130]. Children with otitis media often experience ear pain, otorrhea, difficulty hearing, and headache. Furthermore, ~60% of children develop otitis media with effusion (OME) that can persist for weeks to months following the resolution of the initial infection [130]. In the majority of otitis media cases, the tympanic membrane bulges, due to inflammation and fluid accumulation in the middle ear, but remains intact; however, spontaneous membrane perforation occurs in 4–30% of cases [9]. The majority of spontaneous perforations resolve within one month with favorable outcomes; however, 15% of cases become occluded, preventing drainage of pus from the middle ear and requiring medical intervention [9]. Children with perforations are twice as likely to have recurrent infections, which may be associated with permanent hearing loss [9]. Notably, populations with limited access to medical care, such as in indigenous communities or people in developing countries, are prone to developing complications of otitis media including labyrinthitis, mastoiditis, extradural abscess, subdural empyema, lateral sinus thrombosis, and meningitis [2, 10, 47, 130].
Bacterial factors
Swelling and death of inner and outer hair cells have been observed in the cochlea in experimental animal models as well as in human autopsies [23, 42, 131]. This damage was found to be dependent on the production of Spn’s pore-forming toxin, pneumolysin. Guinea pig cochleae perfused with pneumolysin had splayed hair bundle stereocilia and damaged, swollen hair cells that tore away from the supporting cells, ultimately resulting in hearing loss [23, 132]. Notably, chinchilla middle ears inoculated with purified cell wall of Spn exhibited the same histopathologic inflammation seen with live bacteria [123]. Otitis media is characterized as being highly neutrophilic with an abundance of neutrophil elastase, Cathepsin G, and lactoferrin, as well as the presence of NETs in middle ear effusions [133]. Myeloperoxidase generated by neutrophils to kill the bacterium has been shown to contribute to damage to the middle ear during otitis by generating hypohalous acids [30, 134].
Sequelae
Fluid present in the middle ear was shown to cause a hearing loss of 25 decibels (dB), similar to putting in earplugs, and the loss was 10 dB greater with bilateral disease [12]. Persistent effusion of the middle ear is often treated with tympanostomy tubes that provide relief by draining middle ear secretions to remove pressure and restore some hearing [11, 12]. In general, hearing substantially improves after one year although full recovery is a relatively slow process and children with a history of OME had defects in binaural processing 1 to 2 years past hearing recovery [135]. In addition to hearing loss, otitis media causes issues with vestibular balance and motor function that mostly return to normal following tympanostomy tube placement [47, 136, 137]. In children, recurrent episodes of otitis media may result in failure to reach cognitive developmental milestones, delayed or deficient speech development, and poorer school performance particularly in mathematics and reading [12, 13, 130].
Lungs
Clinical aspects & pathophysiology
As pneumonia progresses, PMN infiltration occurs into bronchioles and adjacent alveoli with neutrophilic inflammation expanding into alveolar spaces in a manner that eventually obliterates the alveolar septa [138, 139]. Infection also results in the release of endogenous prostaglandins, which induce hypoxic pulmonary vasoconstriction of pulmonary artery blood flow into the consolidated lung resulting in an intrapulmonary shunt and increased oxygen consumption by the lung contributing to edema and arterial hypoxemia, referred to as acute lung injury. Additionally, carbon dioxide exchange is disrupted, increasing the respiratory rate, the minute ventilation, and the effort needed to breathe. Impaired surfactant activity reduces the dynamic compliance of the lungs, furthering the work needed to breathe effectively [140]. Typically, S. pneumoniae is associated with a lobar pattern that can be observed based on the pattern of opacity on chest radiographs. Lung congestion can be followed by the leakage of red blood cells (RBCs), neutrophils, and fibrin into the alveolar fluid, which changes the color of the lungs to dark red and for this reason is termed red hepatization [141]. Eventually, the RBCs associated with fibrinopurulent exudates break down transforming the lung from red to gray (i.e. gray heparinization) [141]. Resolution of infection is characterized by macrophage infiltration into alveolar space, clearing the exudates by scavenging dying neutrophils and other debris [138, 141].
During severe pneumonia, acute respiratory distress (ARDS) can develop. According to the American-European Consensus Conference, if the concentration of arterial oxygen in the blood divided by the inspired fraction of oxygen (i.e. a PaO2/FiO2) is less than 200 mm Hg a diagnosis of ARDS is made with the Berlin definition stratifying the severity of disease into 3 groups: mild (≤ 300 mm Hg), moderate (≤ 200 mm Hg), and severe (≤ 100 mm Hg) [28, 142, 143]. ARDS during severe pneumonia can be described as occurring in stages associated with direct damage to the lung parenchyma along with indirect damage incurred from systemic inflammation [28, 144]. In the first 1–6 days, there is interstitial and alveolar edema characterized by inflammation, thickening of the alveolar-capillary membrane, and the accumulation of neutrophils, macrophages, and red blood cells in the alveoli with evidence of both endothelial and epithelial injury [28, 144]. There is both denuding of the alveolar epithelium and the appearance of prominent hyaline membranes in the alveoli [144]. During the subacute phase (the next 7–14 days), some of the edema is reabsorbed and attempts at repair by the proliferation of alveolar epithelial type II cells along with infiltration of fibroblasts and increased collagen deposition [28, 144]. After 14 days, (the chronic phase), there is typically resolution of the acute neutrophilic infiltrate, but there are more mononuclear cells in the alveoli and more fibrosis and repair of the alveolar epithelial [28, 144]. The concentration of albumin, lactate dehydrogenase, IL-6, and neutrophil elastase in epithelial lining fluid of small airways is elevated in patients with ARDS [145, 146]. The edema and acute inflammation of ARDS is gradually resolved in many patients without fibrosis occurring [28]. The presence of ARDS increases the likelihood of non-pulmonary organ failure including cardiovascular failure, renal failure, abnormal liver function, and hematologic abnormalities such as anemia and thrombocytopenia [28, 142]. These are discussed in more detail below. In addition to ARDS, other pulmonary complications of pneumococcal pneumonia can occur including pleural effusion, empyema, multilobar infiltration, and abscesses or cavitations; having one or more of these complications is referred to as complicated pneumonia and is associated with higher rates of ICU admission, shock, a longer length of hospital stay, and treatment failure [147, 148].
Bacterial factors
Pneumolysin released from Spn causes lung damage through its cytolytic activity resulting in the impairment of pulmonary microvascular barrier function, damage-mediated influx of neutrophils, and severe pulmonary hypertension [28, 89, 106, 149,150,151,152,153,154,155,156]. Endothelial cells treated with pneumolysin had increased cell retraction and gap formation as well as detachment; pneumolysin-treated human alveolar epithelial cells also exhibited increased cell layer permeability [156]. Pneumolysin has been shown to induce respiratory epithelial cell necroptotic death as a result of ion dysregulation, causing the release of alarmins, and stimulating neutrophil elastase release after neutrophilic cell death, all of which contribute to lung injury [43, 57, 106, 157]. Pneumococci, through the conversion of pyruvate to acetyl phosphate by the metabolic enzyme streptococcus pyruvate oxidase (SpxB), produce profuse amounts of H2O2 [158]. This is known to induce oxidative stress, DNA damage, and apoptotic/necroptotic cell death in the lungs [158, 159]. Pneumolysin and H2O2 are especially potent together and have been implicated in the death of host cells [75, 77]. These molecules also have consequential negative effects even at concentrations below their cytotoxic threshold, for example slowing the beating of the cilia on epithelial cells [24, 25]. Notably, inhibiting macrophage apoptosis has been shown to decrease pneumococcal clearance from the lungs and promotes invasive pneumococcal disease as AM laden with Spn facilitate their own killing by undergoing apoptotic death [75, 77, 160].
Sequelae
In most instances, individuals with pneumonia recover fully. However, during severe cases, the physiological stress put on other organs and bacterial products or live bacteria in the circulation results in systemic organ damage. Patients with preexisting chronic obstructive pulmonary disease (COPD) were 42.3% more likely to experience exacerbations of disease if they experienced CAP [161]. Tachycardia is seen in many patients with pneumonia and can complicate pre-existing conditions to worsen cardiac function [162]. One feature of pneumonia, particularly in the elderly is loss of cognitive function and dementia. This is far more common and distinct from bacterial invasion of the CNS as discussed below. Many of these clinical features mirror those which are seen during sepsis.
Patients hospitalized for community-acquired pneumonia have an increased risk for long-term mortality that is nearly double that of patients hospitalized for all other combined causes [163,164,165,166,167,168]. Pneumococcal pneumonia results in a greater risk of death for at least 10 years following the acute bout of infection with 32.2% of survivors dying within 10 years [169]. Increased pneumococcal disease severity, as measured by the CURB-65 (confusion, urea > 7 mmol/L, respiratory rate ≥ 30/min, low blood pressure, and age ≥ 65 years) and/or the Pneumonia Severity Index (PSI) also known as the Pneumonia Patient Outcomes Research Team (PORT) risk score, is associated with greater long-term mortality [14, 170,171,172,173].
Sepsis
S. pneumoniae is a primary cause of sepsis, and this has well-documented associations with poor outcomes such as mortality and the development of frailty. Sepsis, a life-threatening hyperinflammatory state, occurs due to the host being unable to clear Spn from the airway or bloodstream and the accompanying dysregulated host response to infection and organ failure [174,175,176]. Sepsis is a major contributor to the physiological stress and organ damage that ultimately leads to the sequelae following pneumococcal infection due to septic-associated dysfunction in the respiratory system, cardiovascular system, brain, liver, and kidneys. Notably, many excellent reviews on the pathophysiology of pneumococcal sepsis are available [175,176,177,178,179,180,181]. The features of sepsis overlap with those which occur during IPD, as in many instances these are often concomitant.
Invasive pneumococcal disease
IPD refers to when the pneumococcus gains access to previously sterile sites including the bloodstream and CNS. Pneumococcal bacteremia occurs in roughly half of patients hospitalized with pneumonia and is associated with increased length of stay, the severity of infection, mortality, and risk of developing new morbidities [38, 182,183,184,185]. The mortality rate of patients with bacteremia is around 19% [184, 186]. Importantly once in the bloodstream, pneumococci are not restricted to the vasculature and are captured by / can invade filtering organs such as the liver, spleen, and kidneys. This puts the parenchyma of these organs at direct risk for damage if overwhelmed. The importance of the spleen in eliminating bacteria from the bloodstream is highlighted by the increased occurrence and magnitude of pneumococcal disease in asplenic individuals [187]. Likewise, splenectomized guinea pigs infected with Spn had increased bacterial titers in their blood, delayed clearance, and decreased survival [188]. It is now known that splenic CD169 + macrophages can be overcome by the bacteria and then serve as a “sanctuary” for replication of the bacteria and dissemination back into the bloodstream [189]. Additionally, there have been reported cases of splenic rupture during pneumococcal pneumonia [190]. Bacteria in the bloodstream can also invade the CNS and heart with devastating consequence. This is the result of direct translocation of pneumococci across vascular endothelial cells into organs.
It is worth noting that organ damage incurred during IPD does not occur in isolation but instead accrues throughout multiple sites in the body simultaneously. This is due to the bacteria disseminating throughout the body. Inflammatory responses occurring concurrently in the lungs, vasculature, and within various organs exacerbate systemic inflammation and injury that can ultimately contribute to the development of sepsis. In addition to direct damage caused by the bacterium, biomechanical stress caused by alterations in circulatory volume and vascular resistance, inflammatory stress, increased metabolic demand, and other stressors associated with infection contribute to organ damage amassed during infection [191,192,193]. Collectively, this organ damage contributes to the sequelae of pneumococcal disease and long-term risk for mortality; survivors having increased risk of adverse events such as heart, renal, and neurological disease [49, 51, 194,195,196]. Accordingly, mortality rates among IPD survivors are greater than for individuals hospitalized for pneumonia without bacteremia [169]; one-third of patients who survived past 1-month end up dying within the next 10 years [169]. What is more, one 3-decade-long study from Ajayi et. Al, found that most patients that recovered from IPD died before their anticipated life expectancy with a mean potential life loss of 9.936 years [37]. In other studies the presence of bacteremia nearly doubled long-term mortality compared to blood culture-negative pneumonia [14, 37, 169]. Pneumococcal pneumonia in itself is a risk factor for the development of frailty with similar long-term mortality rates compared to chronic diseases, such as cardiovascular and cerebrovascular disease.
Heart
Clinical aspects & pathophysiology
The correlation between pneumococcal pneumonia and acute heart failure has been recognized for over a century [41, 197, 198]. In the early twentieth century, patients with pneumococcal pneumonia were routinely prescribed Digitalis, a drug used to strengthen heart contractility [198, 199]. Hospitalization for pneumococcal pneumonia has been associated with new or worsened adverse cardiovascular events (CVEs) such as atrial fibrillation, heart failure, or myocardial infarction [162, 191, 192, 200]. In all, studies suggest that between a fifth to a third of patients admitted to the hospital for pneumonia develop cardiac complications [194]. Patients with preexisting cardiac conditions, such as heart failure, have an increased risk of disease exacerbations following pneumonia compared to a pneumonia-free cohort [161]. Over 90% of patients with pneumococcal disease who did experience cardiac complications had their first adverse cardiac event within the first week after admission to the hospital with > 50% occurring on the very same day [200]. Severe pneumonia episodes, in particular those with IPD, are positively correlated with increased short-term and long-term risk for adverse cardiac events. The presence of bacteremia increased the risk of adverse cardiac events. One of the best predictive measures of the severity of disease and in-hospital mortality was having higher troponin levels, a biomarker of cardiac damage, at the time of admission [162]. Supporting this notion, the 30-day mortality is higher in pneumonia patients with CVEs [200]. The increased incidence of CVEs during or following pneumococcal disease suggests that pneumococcal disease may exacerbate CVEs or even play a causal role.
Intense systemic inflammation present during pneumonia places stress on the heart which requires it to work harder due to decreased blood oxygen and lowered blood pressure that accompanies infection [162]. The increased levels of leukocytes, circulating inflammatory cytokines, CRP, coagulation factors, reactive oxygen species, and vasodilating molecules may increase the risk for thrombogenesis, procoagulant activity, and decrease cardiac contractility [201,202,203]. Myeloperoxidase produced from infiltrating neutrophils and monocytes has been implicated in cardiovascular disease as it can cause plaque rupture, damage artery walls, and activate MMPs causing further cardiovascular damage [204]. Infection promotes the development of thrombi by activating platelets, vascular constriction, dysregulation of the coagulation system, endothelial dysfunction, procoagulant changes in blood, inducing demand ischemia, and increases the risk for the instability and rupture of atherosclerotic plaque. Increased concentrations of troponins, BNP, and ANP have been associated with depression of left ventricular function and myocarditis. Increased pulmonary arterial pressure and levels of thrombin-antithrombin complexes, D-dimer, and plasminogen activator inhibitor along with decreased factor IX contributes to increased coagulation activation that is seen in almost 90% of patients hospitalized for pneumonia [200, 205, 206]. Alongside all of this, pneumococci also have a direct cytotoxic effect on cardiomyocytes.
Bacterial factors
Pneumococci-derived products including cell wall, H2O2, and pneumolysin are cardiotoxic and able to kill cardiomyocytes and suppress heart function. Pneumococcal cell wall components have been detected in the hearts of experimentally Spn-infected animals and shown to directly suppress cardiac contractility in a platelet-activating factor receptor-dependent manner [207]. Platelet-activating factor (PAF) activation in cardiac tissue is associated with long-lasting negative and arrhythmogenic effects on cardiomyocyte contractility [207,208,209]. Pneumolysin in the circulation is also able to cause cardiac damage, as pneumolysin-deficient Spn have less circulating troponins, biomarkers of cardiac injury, and cardiac damage when compared to pneumolysin-expressing Spn [210,211,212]. Cardiomyocytes exposed to pneumolysin experience an influx of Ca2+ into the cytoplasm through pneumolysin membrane-bound pores disrupting calcium signaling that is crucial for cardiac contractility in a dose-dependent manner [210]. Finally, work in non-human primates and mice has shown that Spn can translocate into the myocardium from the circulation in platelet-factor receptor and laminin receptor dependent fashion, establish a niche, and replicate to cause foci of infection called microlesions, serving to directly deliver cytotoxic products, including cell wall, pneumolysin, and H2O2 (Fig. 2) [45, 212, 213].
Cardiac microlesion formation and resolution. Microlesions form in the heart as a result of an individual pneumococcus adhering to the vasculature in the bloodstream and invading the myocardium by crossing vascular endothelial cells. Invaded pneumococci are capable of replicating to form a foci of infection (left panel). Infiltrating macrophages die of H2O2 and pneumolysin-mediated necroptosis preventing further infiltration of immune cells. Additionally, cardiomyocytes undergo necroptotic death leaving “holes” within the heart. The resolution of infection is characterized by the remodeling of cardiac tissue (right panel). This includes the infiltration of fibroblasts that deposit collagen to form long-lasting scar tissue. Microlesion morphology based on high-resolution images of cardiac sections from mice infected with Streptococcus pneumoniae strain TIGR4, shown 30 h post-infection, intraperitoneal challenge
Sequelae
The transient risk of cardiovascular events occurring, including myocardial infarction or stroke, is 2–10 times greater following an acute respiratory infection [191,192,193, 200, 214, 215] and this is positively linked to its severity. Notably, admission to an ICU for pneumonia is associated with the greatest risk of new-onset heart failure, myocardial infarction, and cardiac-related death. Beyond acute infection, heightened risk for adverse cardiac events lingers for more than 5 years post-hospitalization [162, 192]. Work with primates and mice, suggests that upon successful antibiotic treatment, former microlesions are the site of extensive cardiac remodeling and collagen deposition [43, 157, 212]. Echocardiography of convalescent mice rescued with antimicrobials from IPD still had impaired ejection fractions and fractional shortening 3 months after successful intervention with antimicrobials [216]. Blocking of pneumolysin-induced cardiomyocyte death in experimentally infected mice rescued with antimicrobials reduced cardiac collagen deposition and reduced the extent of heart dysfunction in convalescence [216].
Kidney
Clinical aspects & pathophysiology
Patients with chronic kidney disease are at increased risk of developing pneumococcal disease and vaccination is highly recommended in this group [217,218,219]. Independently, acute renal injury in the form of nephritis has been anecdotally associated with pneumococcal disease since 1872 [220, 221]. More recently, several studies have reported pneumococcal disease is damaging to the kidneys with consequences ranging from persistent proteinuria to end-stage renal disease [195]. Following hospitalization for pneumococcal pneumonia, one-third of patients experience acute kidney injury (AKI) [46, 222]. Those with AKI have increased hospital mortality, increased risk for adverse events including myocardial infarction and end-stage renal disease, and a nearly threefold greater rate of long-term mortality in those with moderate and severe injury [46, 222]. Among survivors, AKI can progress to chronic kidney disease as nephron loss leads to glomerular hypertrophy in the remaining nephrons [46, 223]. While Spn is not considered a typical agent of urinary tract infections (UTIs), it has been reported that children with chronic kidney disease have had urinary tract abnormalities associated with Spn infection and clinical UTI symptoms consistent with cystitis [224, 225]. Additionally, even in the absence of other disorders, Spn can be the causative agent of UTI, but due to the rarity of these causes more data is needed to evaluate the involvement of the pneumococci in the epidemiology and pathogenesis of UTIs [226].
Postulated mechanisms of renal injury during and following pneumococcal pneumonia include systemic hypotension and hypoxemia that contributes to peritubular hypoxia inducing fibrosis [195, 219, 227, 228]. Post-pneumococcal acute glomerulonephritis biopsy showed neutrophil and mononuclear cell infiltration into capillary loops with deposition of C3c and nephritis-associated plasmin receptors in the mesangial area and capillary loops [33]. Leukocyte-derived myeloperoxidase also contributes to glomerulonephritis [204]. Notably, pneumonia patients who develop acute kidney injury were older, had more comorbidities, and higher levels of inflammatory cytokines in the blood (IL-6, TNF, D-dimer) even in those without severe disease [222].
Bacterial factors
Although, case reports exist of Spn causing pyelonephritis and urosepsis [229, 230], there is overall a paucity of evidence that pneumococcal products or live Spn directly damage kidneys impairing function. Given what is known about the pneumococcus and since pneumococci are isolated from the kidneys of experimentally infected animals, it seems likely that a direct cytotoxic effect also contributes to the damage and therefore more research is warranted in this area. Along these lines, pneumolysin and bacterial neuraminidase have been implicated in damage [231,232,233]. Pneumococcal cell wall increasing levels of inflammation and prothrombotic molecules such as CRP, fibrinogen, and factor VII contribute to deteriorating renal function [195, 234]. Immune-complex-mediated acute glomerulonephritis is a rare complication of pneumococcal infection, and the pathogenic mechanism is hypothesized to involve the deposition of streptococcal antigen and formation of circulating immune complexes [33].
Sequelae.
Spn-associated hemolytic uremic syndrome (HUS) is an uncommon complication of pneumococcal pneumonia that develops 3–13 days after the onset of symptoms and is mostly observed in young children [235,236,237]. Pneumococcal HUS has a poor outlook with a mortality rate of 12.3% during the acute phase and ~ 10% of recovered patients going on to develop end-stage renal failure [236].
Central nervous system
Clinical aspects & pathophysiology
Perhaps the most severe form of pneumococcal infection is meningitis, with case fatality rates varying from 20–37% in high-income countries and up to 51% in low-income countries where patients often face poor access to sufficient medical care. Cerebrovascular complications are very common during pneumococcal meningitis, with arterial stroke occurring in up to 30% of patients, cerebral venous thrombosis in 9%, and intracerebral hemorrhage in up to 9% [1, 238]. Pneumococci most likely gain access to the CNS via multiple sites including the blood-cerebrospinal fluid (CSF) barrier in the subarachnoid space, the blood–brain barrier (BBB) of the cerebral cortex, and the blood-CSF barrier in the choroid plexus [239, 240]; this is also the result of bacterial translocation across vascular endothelial cells and is dependent on pneumococci binding to platelet-activating factor receptor and laminin receptor. Additionally, children can develop meningitis, while having no obvious source of infection, in which bacteria gain access to the CNS directly from either the nasopharynx or middle ear. While CNS involvement most likely is preceded by bacteremia in adults, exceptions to this include those with craniofacial injury and hearing devices.
Much of the damage incurred during pneumococcal meningitis can be attributed to the inflammatory response to bacterial products [241]. CSF levels of inflammasome-associated cytokines, IL-1β and IL-18, correlate with systemic complications and worse clinical outcomes in patients [29, 242]. Blocking IL-1β reduces PM-induced cerebral inflammation and disease pathology [241, 243, 244]. MMPs released by neutrophils, neurons, and glial cells, among others, degrade the extracellular matrix contributing to decreased integrity of the subendothelial basal lamina of BBB, increased leukocyte invasion, inflammation, and neuronal injury [245]. Increased levels of myeloperoxidase produced by infiltrating leukocytes has been indicated in various neurodegenerative processes [204]. In experimental mouse models of pneumococcal meningitis, inhibition of MMP-2 and -9 decreased brain injury, lowered mortality, and prevented cognitive impairment [246, 247]. Remarkably, inflammation and leukocyte recruitment into the CNS occurred during bacteremia prior to pneumococci being detected in the brain [248]. Human histopathological studies from brains recovered from autopsies of pneumococcal meningitis patients have shown parenchymal damage secondary to intracranial pressure, cytotoxic and vasogenic edema, microhemorrhages, local leukocyte infiltration, abscess formation, fibrin thrombi, cortical necrosis, neuronal apoptosis in the hippocampal dentate gyrus, and hippocampal neuronal loss [48, 52]. Brain-diffuse ischemic axonal injury and Wallerian degeneration have been shown in brain autopsy and experimental pneumococcal meningitis [52, 249]. Brain structural damage can result from vasospasms and reduced blood flow eventually causing cortical necrosis and apoptotic cell death in the dentate gyrus [50]. Accordingly, blocking leukocyte invasion either by pharmaceutical inhibition of selectins or antibodies against endothelial intercellular adhesion molecules (ICAM1) or leukocyte integrin (Mac-1), attenuated the increased cerebral blood flow and intracranial pressure seen in early meningitis, inhibited leukocyte accumulation, brain edema, inflammation and BBB damage [29, 250, 251].
Bacterial factors
Pneumolysin, H2O2, and autolysin mediate brain cell mitochondrial damage and apoptosis of neurons through P38 MAPK activation, as well as intrinsic and extrinsic caspase-dependent programmed cell death [21, 22, 252,253,254]. Notably, the symptoms of meningitis can be replicated by injecting components of pneumolysin or Spn’s cell wall into the CNS; this is due to their cytotoxic properties and the inflammatory response generated in the CNS, respectively [255]. Meningeal inflammation significantly increased following antibiotic treatment attributed to bacterial lysis and release of cell wall [255]. However, by reducing the inflammatory response during antibiotic therapy using cyclooxygenase inhibitors some of the damage caused by host cells was mitigated [256]. Further, corticosteroid treatment has been shown to reduce CNS inflammation, severe morbidities, and case fatality rates [257].
Sequelae
Up to 30% of patients that survived meningitis have some type of neurological or neuro-behavioral sequelae [49]. These include seizures, hearing and vision loss, cognitive impairment, neuromotor disability, and memory or behavior changes [51]. In adult survivors of community-acquired pneumococcal meningitis from a Dutch nationwide prospective cohort study, 34% had persistent neurologic sequelae – most commonly hearing loss (27%). Neuro-physical evaluation revealed that patients who recovered from meningitis performed worse than controls with alertness, and cognitive flexibility with cognitive impairment seen in 14% of patients [22, 49, 51, 258]. Cognitive impairment occurred in all domains – most commonly cognitive speed (71%) but attention (60%) and memory (61%) were also affected. Survivors had lower quality of life scores, social functioning, and perceived health than those who had not experienced pneumococcal meningitis [49, 258]. Even healthy children and adults without apparent neurological deficits are at risk for long-term cognitive deficits following pneumococcal meningitis [259, 260]. Early identification and antibiotic/corticosteroid treatment is important to achieve a successful return to society [51].
Frailty
Frailty is a state of vulnerability and loss of resilience to a variety of stressors that increase the risk of a variety of health-related problems that require hospitalization, including pneumonia [261, 262]. There seems to be a bidirectional relationship between pneumonia and cognitive function in which cognitive decline increases the risk for pneumonia while patients with pneumonia are at increased risk of subsequent dementia [260]. In older adults, hospitalization for pneumonia has been associated with a subsequent decline in physical and cognitive abilities along with the development of depressive symptoms [259]. Some patients that survived severe illness, such as ARDS, had persistent reduced physical quality of life 5 years after their illness, despite pulmonary function returning to normal. ICU- acquired weakness, or paresis, is common in survivors of critical illness and associated with worse outcomes, such as increased hospital mortality, long-term function, and quality of life outcomes [263,264,265,266]. Pneumonia is not only life-threatening but life-altering and can trigger a cycle of increased severity of frailty leading to accelerated aging, functional decline, and mortality.
Premature mortality because of pneumococcal disease
While the majority of patients recover from respiratory symptoms within two to three weeks following infection, the general well-being of patients resolves more gradually [19, 267]. Many pneumonia survivors do not recover fully to their pre-infectious state after the cessation of antibiotics and still experience residual symptoms for months [19, 268,269,270,271,272]. Older patients and those with premorbid conditions take longer to recover and had a lower health-related quality of life as measured by physical functioning, and general and perceived health [19, 270]. However, it is important to note that while age is an important predictor of long-term mortality, pneumonia does also appear to cause excess long-term mortality in young populations as well [166, 273]. For example, 10% of patients were hospitalized within 30 days of their pneumonia diagnosis and nearly three-quarters of survivors were hospitalized again within a 5-year period for any cause [173, 192, 272]. The most common cause of death among pneumonia survivors was cardiovascular disease, followed by respiratory diseases and cancer [165,166,167, 173, 206, 274, 275]. Survivors are at increased risk for new-onset heart disease for up to 5 years post-hospitalization and strikingly 20% of survivors developed new or worsening congestive heart failure within 30 days of hospitalization [173, 191, 272].
One of the greatest predictors of long-term mortality following pneumococcal pneumonia is the presence and number of comorbid chronic conditions including cardiovascular disease, respiratory diseases (e.g. COPD), diabetes, kidney disease, liver disease, dementia, seizures, and cancer [19, 163, 185, 206, 273, 274, 276,277,278,279,280,281]. Several studies have found an association between the presence of co-morbidities and long-term mortality, with a larger number of co-morbidities predicting greater long-term mortality [163, 165, 167, 206, 273,274,275,276,277,278,279,280,281,282,283,284,285]. Additionally, a substantial body of evidence supports that advanced age is associated with increased long-term mortality after recovery from pneumonia [164,165,166, 168, 173, 273,274,275,276, 280, 281, 283, 284, 286]. Notably, racial disparity exists with black individuals having higher rates of both short-term and long-term mortality as well as an increased likelihood of developing additional morbidities such as heart failure, gastrointestinal bleeding, frailty, stroke, and myocardial infarction [287]. Potential reasons for these discrepancies in mortality include, genetics, socioeconomic factors, and the presence of additional co-morbidities which are disproportionately higher among African Americans, which together raise the risk for severe infection [279, 288,289,290,291,292,293]. Evidence specific to older adults suggests that older adults exhibit excessive pro-inflammatory cytokine levels after acute pneumonia that are associated with morbidity and mortality [290, 294,295,296]. In accordance with this, higher systemic levels of pro-inflammatory cytokines, such as IL-6 and TNF, at discharge can predict both short and long-term mortality after hospitalization for pneumonia [110, 146, 294, 295, 297, 298]. Male sex appears to accentuate this age-related dysfunction in the resolution of inflammation [298,299,300,301,302]. In addition to inflammatory cytokines, several studies have looked into various biomarkers to attempt to predict short and long-term outcomes, showing that high serum glucose, blood urea nitrogen/albumin ratio, creatinine, pro-atrial natriuretic peptide, pro-endothelin-1,pro-vasopressin, pro-adrenomedullin, CRP, troponins, hemostasis markers (such as D-Dimer, thrombin-antithrombin complexes, factor IX, antithrombin, and plasminogen activator inhibitor-1), and white blood cell count, as well as low serum albumin and alanine aminotransferase all had a high predictive power for short and long term mortality, with pro-adrenomedullin consistently being one of the best indicators of outcomes [110, 167, 182, 205, 206, 273, 284, 303,304,305,306]. The clinical power in utilizing biomarkers, such as pro-adrenomedullin, along with pneumonia severity indexes should be used to identify and guide treatment in patients at high risk for the development of new morbidities or mortality so they can be carefully monitored to attempt to reduce long-term consequences [182].
Treatment and prevention
Currently, the most effective strategy for clinicians to address pneumococcal infections is prompt access to care, accurate diagnosis, rapid antibiotic delivery, and disease prevention by implementing widespread vaccination against the pneumococcus [307]. Many groups have published guidelines for the management of pneumococcal disease, including the American Thoracic Society (ATS), Infectious Diseases Society of America (IDSA), and the British Thoracic Society (BTS) that indicates patients should be treated with an agent that specifically targets pneumococcus, recommending monotherapy with β-lactams for uncomplicated outpatients and a combination of β-lactam and macrolide therapy for severe cases [308,309,310,311,312,313,314,315]. Early administration of antimicrobials is associated with a better prognosis and the failure to use antibiotics concordant with IDSA and ATS guidelines has been associated with an increased risk of in-hospital mortality and more than a five-fold increase in 30-day mortality [316,317,318,319,320,321,322,323,324,325].
The Advisory Committee on Immunization Practices (ACIP) recommended adults ≥ 65 years and adults 19–64 with underlying medical conditions or other risk factors be vaccinated with a polysaccharide-conjugate vaccine, either a combination of PCV15 followed by PPSV23, the pneumococcal polysaccharide vaccine, or PCV20 alone [326]. Annual vaccination against seasonal influenza viruses is recommended in all patients as influenza infection predisposes individuals to pneumococcal infection [326,327,328]. Additionally, individuals with chronic kidney disease are recommended to receive pneumococcal conjugate vaccines as this has been shown to reduce vaccine-type IPD by 75% in these individuals as well as lower overall mortality especially when a pneumococcal vaccine is used in combination with an annual influenza vaccine [217, 218, 329]. This is crucial as patients with end-stage renal disease are between 10 and 16-fold more likely to die from pneumonia than the general population [217, 227, 228, 329]. Vaccination against Spn has also been effective in reducing meningitis however serotype replacement has led to an emergence of non-vaccine serotypes that have reduced the overall effect of vaccination on pneumococcal meningitis incidence in Europe and North America [330, 331]. The Global Vaccine Action Plan has committed to extending the availability of pneumococcal vaccines to low and lower-middle-income countries in an effort to relieve some of the burden of pneumococcal disease [332]. Following the introduction of PCV10 in Brazil, there was a 10% decline in pneumonia mortality in children, and similar large benefits are expected when PCVs are introduced in other low-income settings [333]. Currently, many countries routinely vaccinate adults but there is controversy in policies such as whether the use of PCV and/or PPV is clinically and cost-effective, what age groups should be vaccinated, and whether repeat dosing could prove beneficial [334,335,336,337,338].
There is controversy that exists on the efficacy of pneumococcal vaccination in reducing overall long-term mortality and the consequences of pneumococcal disease. However, research has shown pneumococcal vaccination to be effective at preventing pneumonia and IPD in older adults who are at higher risk [339,340,341,342,343,344,345,346]. With an aging population that is expected to double by the year 2050, it is becoming increasingly important to extend vaccination for the promotion of healthy aging [347, 348]. Considering the drastic long-term effects that pneumonia can have, pneumococcal vaccination should be implemented to reduce pneumococcal disease burden as research has shown that even slight clinical effectiveness is highly cost-effective. Indeed, vaccination in the elderly has been associated with lower hospitalization rates for pneumonia, mortality, and medical cost [349]. PPV is effective at preventing IPD, even in immunocompromised patients [335]. Routine infant immunization with PCV has reduced all-cause pneumonia hospital admissions, cases of acute otitis media, IPD, and mortality in children under 5 [350,351,352,353]. While research investigating the effect of vaccination on the long-term consequences of pneumonia is scarce, considerable evidence does support the beneficial effects of the pneumococcal vaccination, and that wider usage of vaccination should be implemented.
Pneumonia is currently considered the 9th leading cause of death, but this estimate only takes into account short-term mortality of up to 30 days and likely underestimates the overall morbidity and mortality that results from the pneumococcus [354]. Evidence supports that Spn contributes to the new development or worsening life-threatening morbidities and long-term mortality in coming years. Further research is needed to understand the long-term sequelae of pneumococcal disease to come up with better preventatives and treatments, so this Captain of death no longer lingers.
Availability of data and materials
Not applicable.
Abbreviations
- Spn :
-
Streptococcus pneumoniae
- CAP:
-
Community-acquired pneumonia
- CNS:
-
Central nervous system
- AMs:
-
Alveolar macrophages
- MMPs:
-
Matrix metalloproteinases
- CRP:
-
C-reactive protein
- PRRs:
-
Pathogen recognition receptors
- TLRs:
-
Toll-like receptors
- NLRs:
-
NOD-like receptors
- PAMPs:
-
Pathogen-associated molecular patterns
- DAMPs:
-
Damage-associated molecular patterns
- MAPKs:
-
Mitogen-activated protein kinases
- NF-κB:
-
Nuclear factor kappa B
- TNF:
-
Tumor necrosis factor
- IL:
-
Interleukin
- PMNs:
-
Polymorphonuclear leukocytes
- NETs:
-
Neutrophil extracellular traps
- MPO:
-
Myeloperoxidase
- OME:
-
Otitis media with effusion
- dB:
-
Decibels
- ARDS:
-
Acute respiratory distress syndrome
- RBCs:
-
Red blood cells
- COPD:
-
Chronic obstructive pulmonary disease
- IPD:
-
Invasive pneumococcal disease
- CVEs:
-
Cardiovascular events
- AKI:
-
Acute kidney injury
- HUS:
-
Hemolytic uremic syndrome
- UTIs:
-
Urinary tract infections
- CSF:
-
Cerebrospinal fluid
- BBB:
-
Blood–brain barrier
References
Kastenbauer S, Pfister HW. Pneumococcal meningitis in adults: spectrum of complications and prognostic factors in a series of 87 cases. Brain. 2003;126(Pt 5):1015–25.
O’Connor TE, Perry CF, Lannigan FJ. Complications of otitis media in Indigenous and non-Indigenous children. Med J Aust. 2009;191(S9):S60–4.
Bohte R, van Furth R, van den Broek PJ. Aetiology of community-acquired pneumonia: a prospective study among adults requiring admission to hospital. Thorax. 1995;50(5):543–7.
Garcia-Vidal C, et al. Early mortality in patients with community-acquired pneumonia: causes and risk factors. Eur Respir J. 2008;32(3):733–9.
Koivula I, Sten M, Makela PH. Risk factors for pneumonia in the elderly. Am J Med. 1994;96(4):313–20.
Metlay JP, et al. Influence of age on symptoms at presentation in patients with community-acquired pneumonia. Arch Intern Med. 1997;157(13):1453–9.
Black RE, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375(9730):1969–87.
Bogaert D, De Groot R, Hermans PW. Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis. 2004;4(3):144–54.
Berger G. Nature of spontaneous tympanic membrane perforation in acute otitis media in children. J Laryngol Otol. 1989;103(12):1150–3.
Berman S. Otitis media in developing countries. Pediatrics. 1995;96(1 Pt 1):126–31.
Casselbrant ML, et al. Otitis media with effusion in preschool children. Laryngoscope. 1985;95(4):428–36.
Fria TJ, Cantekin EI, Eichler JA. Hearing acuity of children with otitis media with effusion. Arch Otolaryngol. 1985;111(1):10–6.
Williams CJ, Jacobs AM. The impact of otitis media on cognitive and educational outcomes. Med J Aust. 2009;191(S9):S69-72.
Musher DM, et al. Bacteremic and nonbacteremic pneumococcal pneumonia. A prospective study Medicine (Baltimore). 2000;79(4):210–21.
Jover F, et al. A comparative study of bacteremic and non-bacteremic pneumococcal pneumonia. Eur J Intern Med. 2008;19(1):15–21.
Klemets P, et al. Invasive pneumococcal infections among persons with and without underlying medical conditions: implications for prevention strategies. BMC Infect Dis. 2008;8:96.
Ben-Shimol S, et al. Seasonality of Both Bacteremic and Nonbacteremic Pneumonia Coincides With Viral Lower Respiratory Tract Infections in Early Childhood, in Contrast to Nonpneumonia Invasive Pneumococcal Disease, in the Pre-Pneumococcal Conjugate Vaccine Era. Clin Infect Dis. 2015;60(9):1384–7.
van Mens SP, et al. Bacteraemic and non-bacteraemic/urinary antigen-positive pneumococcal community-acquired pneumonia compared. Eur J Clin Microbiol Infect Dis. 2015;34(1):115–22.
El Moussaoui R, et al. Long-term symptom recovery and health-related quality of life in patients with mild-to-moderate-severe community-acquired pneumonia. Chest. 2006;130(4):1165–72.
Jay SJ, Johanson WG Jr, Pierce AK. The radiographic resolution of Streptococcus pneumoniae pneumonia. N Engl J Med. 1975;293(16):798–801.
Braun JS, et al. Pneumolysin causes neuronal cell death through mitochondrial damage. Infect Immun. 2007;75(9):4245–54.
Braun JS, et al. Pneumococcal pneumolysin and H(2)O(2) mediate brain cell apoptosis during meningitis. J Clin Invest. 2002;109(1):19–27.
Comis SD, et al. Cytotoxic effects on hair cells of guinea pig cochlea produced by pneumolysin, the thiol activated toxin of Streptococcus pneumoniae. Acta Otolaryngol. 1993;113(2):152–9.
Feldman C, et al. The effects of pneumolysin and hydrogen peroxide, alone and in combination, on human ciliated epithelium in vitro. Respir Med. 2002;96(8):580–5.
Feldman C, et al. The effect of Streptococcus pneumoniae pneumolysin on human respiratory epithelium in vitro. Microb Pathog. 1990;9(4):275–84.
García-Suárez MdM, et al. The role of pneumolysin in mediating lung damage in a lethal pneumococcal pneumonia murine model. Respir Res. 2007;8(1):3.
Hoegen T, et al. The NLRP3 Inflammasome Contributes to Brain Injury in Pneumococcal Meningitis and Is Activated through ATP-Dependent Lysosomal Cathepsin B Release. J Immunol. 2011;187(10):5440.
Matthay MA, Zemans RL. The acute respiratory distress syndrome: pathogenesis and treatment. Annu Rev Pathol. 2011;6:147–63.
Tuomanen EI, et al. Reduction of inflammation, tissue damage, and mortality in bacterial meningitis in rabbits treated with monoclonal antibodies against adhesion-promoting receptors of leukocytes. J Exp Med. 1989;170(3):959–69.
Xiang Y, et al. The critical role of myeloperoxidase in Streptococcus pneumoniae clearance and tissue damage during mouse acute otitis media. Innate Immun. 2017;23(3):296–306.
Ebrahimi F, et al. Markers of neutrophil extracellular traps predict adverse outcome in community-acquired pneumonia: secondary analysis of a randomised controlled trial. Eur Respir J. 2018;51(4):1701389.
José, R.J., et al., S100 Proteinase-activated receptor 1 signalling contributes to neutrophilic inflammation and alveolar barrier disruption in Streptococcus pneumoniae pneumonia. 2014, BMJ Publishing Group Ltd.
Odaka J, et al. A case of post-pneumococcal acute glomerulonephritis with glomerular depositions of nephritis-associated plasmin receptor. CEN Case Reports. 2015;4(1):112–6.
Ripley-Petzoldt ML, et al. The contribution of pneumococcal cell wall to the pathogenesis of experimental otitis media. J Infect Dis. 1988;157(2):245–55.
van der Sluijs KF, et al. IL-10 Is an Important Mediator of the Enhanced Susceptibility to Pneumococcal Pneumonia after Influenza Infection. J Immunol. 2004;172(12):7603.
Yanagihara K, et al. Effects of specific neutrophil elastase inhibitor, sivelestat sodium hydrate, in murine model of severe pneumococcal pneumonia. Exp Lung Res. 2007;33(2):71–80.
Ajayi OO, et al. Three decades of follow-up of adults after recovery from invasive pneumococcal pneumonia. Am J Med Sci. 2017;353(5):445–51.
Wagenvoort GH, et al. Long-term mortality after IPD and bacteremic versus non-bacteremic pneumococcal pneumonia. Vaccine. 2017;35(14):1749–57.
Austrian R. The syndrome of pneumococcal endocarditis, meningitis and rupture of the aortic valve. Trans Am Clin Climatol Assoc. 1956;68:40–7 discussion 48-50.
Akram A, Kazi A, Haseeb A. The Deathly Hallows of the Austrian Triad. Cureus. 2020;12(1):e6568.
Mandal AK, Mohamad B, Missouris CG. Lessons of the month 3: Gone but not forgotten - Osler - a reminder of the syndrome not bearing his name. Clin Med (Lond). 2019;19(6):523–5.
Cook RD, et al. Cytotoxic changes in hair cells secondary to pneumococcal middle-ear infection. J Otolaryngol. 1999;28(6):325–31.
Reyes LF, et al. Severe Pneumococcal Pneumonia Causes Acute Cardiac Toxicity and Subsequent Cardiac Remodeling. Am J Respir Crit Care Med. 2017;196(5):609–20.
Rubins JB, et al. Dual function of pneumolysin in the early pathogenesis of murine pneumococcal pneumonia. J Clin Invest. 1995;95(1):142–50.
Brown AO, et al. Streptococcus pneumoniae translocates into the myocardium and forms unique microlesions that disrupt cardiac function. PLoS Pathog. 2014;10(9):e1004383.
Coca SG, et al. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;53(6):961–73.
Bluestone, C.D., Clinical course, complications and sequelae of acute otitis media. The Pediatric Infectious Disease Journal, 2000. 19(5).
Nau R, Soto A, Brück W. Apoptosis of Neurons in the Dentate Gyrus in Humans Suffering from Bacterial Meningitis. J Neuropathol Exp Neurol. 1999;58(3):265–74.
Kloek AT, et al. Long-term neurologic and cognitive outcome and quality of life in adults after pneumococcal meningitis. Clin Microbiol Infect. 2020;26(10):1361–7.
Grandgirard D, et al. Pneumococcal Meningitis Induces Apoptosis in Recently Postmitotic Immature Neurons in the Dentate Gyrus of Neonatal Rats. Dev Neurosci. 2007;29(1–2):134–42.
Lucas MJ, Brouwer MC, van de Beek D. Neurological sequelae of bacterial meningitis. J Infect. 2016;73(1):18–27.
Nau R, et al. Axonal injury, a neglected cause of CNS damage in bacterial meningitis. Neurology. 2004;62(3):509–11.
Hiemstra PS, McCray PB Jr, Bals R. The innate immune function of airway epithelial cells in inflammatory lung disease. Eur Respir J. 2015;45(4):1150–62.
Ganz T. Antimicrobial polypeptides in host defense of the respiratory tract. J Clin Invest. 2002;109(6):693–7.
Vissers M, et al. Recognition of Streptococcus pneumoniae and muramyl dipeptide by NOD2 results in potent induction of MMP-9, which can be controlled by lipopolysaccharide stimulation. Infect Immun. 2014;82(12):4952–8.
Verschoor A, et al. Old dogs-new tricks: immunoregulatory properties of C3 and C5 cleavage fragments. Immunol Rev. 2016;274(1):112–26.
Standish AJ, Weiser JN. Human neutrophils kill Streptococcus pneumoniae via serine proteases. J Immunol. 2009;183(4):2602–9.
Greenlee KJ, Werb Z, Kheradmand F. Matrix metalloproteinases in lung: multiple, multifarious, and multifaceted. Physiol Rev. 2007;87(1):69–98.
Opdenakker G, Van den Steen PE, Van Damme J. Gelatinase B: a tuner and amplifier of immune functions. Trends Immunol. 2001;22(10):571–9.
Van Den Steen PE, et al. Gelatinase B/MMP-9 and neutrophil collagenase/MMP-8 process the chemokines human GCP-2/CXCL6, ENA-78/CXCL5 and mouse GCP-2/LIX and modulate their physiological activities. Eur J Biochem. 2003;270(18):3739–49.
Travis SM, et al. Activity of abundant antimicrobials of the human airway. Am J Respir Cell Mol Biol. 1999;20(5):872–9.
Tuomanen EI, et al. Intracellular Trafficking and Killing of<i>Streptococcus pneumoniae</i> by Human Alveolar Macrophages Are Influenced by Opsonins. Infect Immun. 2000;68(4):2286–93.
Houldsworth S, Andrew PW, Mitchell TJ. Pneumolysin stimulates production of tumor necrosis factor alpha and interleukin-1 beta by human mononuclear phagocytes. Infect Immun. 1994;62(4):1501–3.
Malley R, et al. Recognition of pneumolysin by Toll-like receptor 4 confers resistance to pneumococcal infection. Proc Natl Acad Sci U S A. 2003;100(4):1966–71.
Martner A, et al. Pneumolysin released during Streptococcus pneumoniae autolysis is a potent activator of intracellular oxygen radical production in neutrophils. Infect Immun. 2008;76(9):4079–87.
Paton JC, Rowan-Kelly B, Ferrante A. Activation of human complement by the pneumococcal toxin pneumolysin. Infect Immun. 1984;43(3):1085–7.
Knapp S, et al. Toll-like receptor 2 plays a role in the early inflammatory response to murine pneumococcal pneumonia but does not contribute to antibacterial defense. J Immunol. 2004;172(5):3132–8.
Takeuchi O, et al. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity. 1999;11(4):443–51.
Yoshimura A, et al. Cutting edge: recognition of Gram-positive bacterial cell wall components by the innate immune system occurs via Toll-like receptor 2. J Immunol. 1999;163(1):1–5.
Ginsburg I. The role of bacteriolysis in the pathophysiology of inflammation, infection and post-infectious sequelae. APMIS. 2002;110(11):753–70.
Tomlinson G, et al. TLR-mediated inflammatory responses to Streptococcus pneumoniae are highly dependent on surface expression of bacterial lipoproteins. J Immunol. 2014;193(7):3736–45.
Takeda K, Kaisho T, Akira S. Toll-like receptors. Annu Rev Immunol. 2003;21:335–76.
Sanchez-Tarjuelo R, et al. The TLR4-MyD88 Signaling Axis Regulates Lung Monocyte Differentiation Pathways in Response to Streptococcus pneumoniae. Front Immunol. 2020;11:2120.
Sha Q, et al. Activation of airway epithelial cells by toll-like receptor agonists. Am J Respir Cell Mol Biol. 2004;31(3):358–64.
Aberdein JD, et al. Alveolar macrophages in pulmonary host defence the unrecognized role of apoptosis as a mechanism of intracellular bacterial killing. Clin Exp Immunol. 2013;174(2):193–202.
Camberlein E, et al. Importance of bacterial replication and alveolar macrophage-independent clearance mechanisms during early lung infection with Streptococcus pneumoniae. Infect Immun. 2015;83(3):1181–9.
Dockrell DH, et al. Alveolar macrophage apoptosis contributes to pneumococcal clearance in a resolving model of pulmonary infection. J Immunol. 2003;171(10):5380–8.
Guilliams M, et al. Alveolar macrophages develop from fetal monocytes that differentiate into long-lived cells in the first week of life via GM-CSF. J Exp Med. 2013;210(10):1977–92.
Knapp S, et al. Alveolar macrophages have a protective antiinflammatory role during murine pneumococcal pneumonia. Am J Respir Crit Care Med. 2003;167(2):171–9.
Uehara A, et al. Various human epithelial cells express functional Toll-like receptors, NOD1 and NOD2 to produce anti-microbial peptides, but not proinflammatory cytokines. Mol Immunol. 2007;44(12):3100–11.
Chamaillard M, et al. An essential role for NOD1 in host recognition of bacterial peptidoglycan containing diaminopimelic acid. Nat Immunol. 2003;4(7):702–7.
Liu X, et al. NOD2 mediates inflammatory responses of primary murine glia to Streptococcus pneumoniae. Glia. 2010;58(7):839–47.
McNeela EA, et al. Pneumolysin activates the NLRP3 inflammasome and promotes proinflammatory cytokines independently of TLR4. PLoS Pathog. 2010;6(11):e1001191.
Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19(8):477–89.
Way EE, Chen K, Kolls JK. Dysregulation in lung immunity - the protective and pathologic Th17 response in infection. Eur J Immunol. 2013;43(12):3116–24.
Lemon Jamie K, Miller Megan R, Weiser Jeffrey N. Sensing of Interleukin-1 Cytokines during Streptococcus pneumoniae Colonization Contributes to Macrophage Recruitment and Bacterial Clearance. Infect Immun. 2015;83(8):3204–12.
Peppoloni S, et al. The encapsulated strain TIGR4 of Streptococcus pneumoniae is phagocytosed but is resistant to intracellular killing by mouse microglia. Microbes Infect. 2010;12(12):990–1001.
Jonsson S, et al. Phagocytosis and Killing of Common Bacterial Pathogens of the Lung by Human Alveolar Macrophages. J Infect Dis. 1985;152(1):4–13.
Gonzalez-Juarbe N, et al. Bacterial Pore-Forming Toxins Promote the Activation of Caspases in Parallel to Necroptosis to Enhance Alarmin Release and Inflammation During Pneumonia. Sci Rep. 2018;8(1):5846.
Han Z, Yang JJ. Oppenheim, Alarmins and immunity. Immunol Rev. 2017;280(1):41–56.
McQuibban GA, et al. Matrix metalloproteinase processing of monocyte chemoattractant proteins generates CC chemokine receptor antagonists with anti-inflammatory properties in vivo. Blood. 2002;100(4):1160–7.
Hong JS, et al. Dual protective mechanisms of matrix metalloproteinases 2 and 9 in immune defense against Streptococcus pneumoniae. J Immunol. 2011;186(11):6427–36.
Rosendahl A, et al. Lung dendritic cells facilitate extrapulmonary bacterial dissemination during pneumococcal pneumonia. Front Cell Infect Microbiol. 2013;3:21.
Yang S-F, et al. Excessive matrix metalloproteinase-9 in the plasma of community-acquired pneumonia. Clin Chim Acta. 2005;352(1):209–15.
Peñaloza HF, et al. Interleukin-10 plays a key role in the modulation of neutrophils recruitment and lung inflammation during infection by Streptococcus pneumoniae. Immunology. 2015;146(1):100–12.
Dehoux MS, et al. Compartmentalized cytokine production within the human lung in unilateral pneumonia. Am J Respir Crit Care Med. 1994;150(3):710–6.
Kolsuz M, et al. Acute phase reactants and cytokine levels in unilateral community-acquired pneumonia. Respiration. 2003;70(6):615–22.
Calbo E, et al. The impact of time on the systemic inflammatory response in pneumococcal pneumonia. Eur Respir J. 2010;35(3):614–8.
Endeman H, et al. Systemic cytokine response in patients with community-acquired pneumonia. Eur Respir J. 2011;37(6):1431–8.
Fernandez-Serrano S, et al. Molecular inflammatory responses measured in blood of patients with severe community-acquired pneumonia. Clin Diagn Lab Immunol. 2003;10(5):813–20.
Igonin AA, et al. Circulating cytokines as markers of systemic inflammatory response in severe community-acquired pneumonia. Clin Biochem. 2004;37(3):204–9.
Calbo E, Garau J. Of mice and men: innate immunity in pneumococcal pneumonia. Int J Antimicrob Agents. 2010;35(2):107–13.
Barichello T, et al. Tumor necrosis factor alpha (TNF-α) levels in the brain and cerebrospinal fluid after meningitis induced by Streptococcus pneumoniae. Neurosci Lett. 2009;467(3):217–9.
Takashima K, et al. Role of tumor necrosis factor alpha in pathogenesis of pneumococcal pneumonia in mice. Infect Immun. 1997;65(1):257–60.
Bergeron Y, et al. Cytokine Kinetics and Other Host Factors in Response to Pneumococcal Pulmonary Infection in Mice. Infect Immun. 1998;66(3):912–22.
González-Juarbe N, et al. Pore-forming toxin-mediated ion dysregulation leads to death receptor-independent necroptosis of lung epithelial cells during bacterial pneumonia. Cell Death Differ. 2017;24(5):917–28.
Marik P, et al. Hydrocortisone and Tumor Necrosis Factor in Severe Community-Acquired Pneumonia: A Randomized Controlled Study. Chest. 1993;104(2):389–92.
Fernandez-Botran R, et al. Contrasting inflammatory responses in severe and non-severe community-acquired pneumonia. Inflammation. 2014;37(4):1158–66.
Kellum JA, et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med. 2007;167(15):1655–63.
Ortqvist A, et al. Diagnostic and prognostic value of interleukin-6 and C-reactive protein in community-acquired pneumonia. Scand J Infect Dis. 1995;27(5):457–62.
Hedlund J, Hansson LO. Procalcitonin and C-Reactive Protein Levels in Community-Acquired Pneumonia: Correlation with Etiology and Prognosis. Infection. 2000;28(2):68–73.
Lee YL, et al. Systemic and bronchoalveolar cytokines as predictors of in-hospital mortality in severe community-acquired pneumonia. J Crit Care. 2010;25(1):176 e7-213.
Schaaf BM, et al. Pneumococcal septic shock is associated with the interleukin-10–1082 gene promoter polymorphism. Am J Respir Crit Care Med. 2003;168(4):476–80.
Wunderink RG, et al. Tumor Necrosis Factor Gene Polymorphisms and the Variable Presentation and Outcome of Community-Acquired Pneumonia. Chest. 2002;121(3):87S.
Wang D, et al. Functional Polymorphisms of Interferon-gamma Affect Pneumonia-Induced Sepsis. PLoS ONE. 2014;9(1):e87049.
Yende S, et al. The influence of macrophage migration inhibitory factor gene polymorphisms on outcome from community-acquired pneumonia. FASEB J. 2009;23(8):2403–11.
Garred P, et al. Association of Mannose-Binding Lectin Polymorphisms with Sepsis and Fatal Outcome, in Patients with Systemic Inflammatory Response Syndrome. J Infect Dis. 2003;188(9):1394–403.
Smelaya TV, et al. Genetic dissection of host immune response in pneumonia development and progression. Sci Rep. 2016;6(1):35021.
Waterer GW, et al. Septic shock and respiratory failure in community-acquired pneumonia have different TNF polymorphism associations. Am J Respir Crit Care Med. 2001;163(7):1599–604.
Schaaf BM, et al. Pneumococcal septic shock is associated with the interleukin-10-1082 gene promoter polymorphism. Am J Respir Crit Care Med. 2003;168(4):476–80.
Read RC, et al. An interleukin-1 genotype is associated with fatal outcome of meningococcal disease. J Infect Dis. 2000;182(5):1557–60.
Quasney MW, et al. Association between surfactant protein B + 1580 polymorphism and the risk of respiratory failure in adults with community-acquired pneumonia. Crit Care Med. 2004;32(5):1115–9.
Lin Z, et al. Polymorphisms of human SP-A, SP-B, and SP-D genes: association of SP-B Thr131Ile with ARDS. Clin Genet. 2000;58(3):181–91.
Gong MN, et al. Polymorphism in the Surfactant Protein-B Gene, Gender, and the Risk of Direct Pulmonary Injury and ARDS. Chest. 2004;125(1):203–11.
Haralambous E, et al. Role of functional plasminogen-activator-inhibitor-1 4G/5G promoter polymorphism in susceptibility, severity, and outcome of meningococcal disease in Caucasian children. Crit Care Med. 2003;31(12):2788–93.
Hermans PW, et al. 4G/5G promoter polymorphism in the plasminogen-activator-inhibitor-1 gene and outcome of meningococcal disease Meningococcal Research Group. Lancet. 1999;354(9178):556–60.
Yan SB, Nelson DR. Effect of factor V Leiden polymorphism in severe sepsis and on treatment with recombinant human activated protein C. Crit Care Med. 2004;32(5 Suppl):S239–46.
Lisboa T, et al. Radiologic progression of pulmonary infiltrates predicts a worse prognosis in severe community-acquired pneumonia than bacteremia. Chest. 2009;135(1):165–72.
van der Poll T, et al. Interieukin-10 Impairs Host Defense in Murine Pneumococcal Pneumonia. J Infect Dis. 1996;174(5):994–1000.
Klein JO. Otitis media. Clin Infect Dis. 1994;19(5):823–33.
Cureoglu S, et al. Cochlear Changes in Chronic Otitis Media. Laryngoscope. 2004;114(4):622–6.
Winter AJ, et al. A role for pneumolysin but not neuraminidase in the hearing loss and cochlear damage induced by experimental pneumococcal meningitis in guinea pigs. Infect Immun. 1997;65(11):4411–8.
Val S, et al. Proteomic Characterization of Middle Ear Fluid Confirms Neutrophil Extracellular Traps as a Predominant Innate Immune Response in Chronic Otitis Media. PLoS ONE. 2016;11(4):e0152865.
Davies MJ. Myeloperoxidase-derived oxidation: mechanisms of biological damage and its prevention. J Clin Biochem Nutr. 2011;48(1):8–19.
Hall JW 3rd, Grose JH, Pillsbury HC. Long-term Effects of Chronic Otitis Media on Binaural Hearing in Children. Arch Otolaryngol Head Neck Surg. 1995;121(8):847–52.
Schaaf RC. The frequency of vestibular disorders in developmentally delayed preschoolers with otitis media. Am J Occup Ther. 1985;39(4):247–52.
Casselbrant ML, et al. Past history of otitis media and balance in four-year-old children. Laryngoscope. 2000;110(5):773–8.
Corley DE, et al. Reproducibility of the Histologic Diagnosis of Pneumonia Among a Panel of Four Pathologists: Analysis of a Gold Standard. Chest. 1997;112(2):458–65.
Light RB. Pulmonary pathophysiology of pneumococcal pneumonia. Semin Respir Infect. 1999;14(3):218–26.
Günther A, et al. Surfactant alteration and replacement in acute respiratory distress syndrome. Respir Res. 2001;2(6):353–64.
McCullers JA, Tuomanen EI. Molecular pathogenesis of pneumococcal pneumonia. Front Biosci. 2001;6:D877–89.
Gorman EA, O’Kane CM, McAuley DF. Acute respiratory distress syndrome in adults: diagnosis, outcomes, long-term sequelae, and management. The Lancet. 2022;400(10358):1157–70.
Fan E, Brodie D, Slutsky AS. Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment. JAMA. 2018;319(7):698–710.
Shaver CM, Bastarache JA. Clinical and biological heterogeneity in acute respiratory distress syndrome: direct versus indirect lung injury. Clin Chest Med. 2014;35(4):639–53.
Ishizaka A, et al. New bronchoscopic microsample probe to measure the biochemical constituents in epithelial lining fluid of patients with acute respiratory distress syndrome. Crit Care Med. 2001;29(4):896–8.
Bauer TT, et al. Comparison of systemic cytokine levels in patients with acute respiratory distress syndrome, severe pneumonia, and controls. Thorax. 2000;55(1):46–52.
Cillóniz C, et al. Pulmonary complications of pneumococcal community-acquired pneumonia: incidence, predictors, and outcomes. Clin Microbiol Infect. 2012;18(11):1134–42.
Menendez R, et al. Risk factors of treatment failure in community acquired pneumonia: implications for disease outcome. Thorax. 2004;59(11):960–5.
González-Juarbe N, et al. Pore-Forming Toxins Induce Macrophage Necroptosis during Acute Bacterial Pneumonia. PLoS Pathog. 2015;11(12):e1005337.
Rubins JB, et al. Distinct roles for pneumolysin’s cytotoxic and complement activities in the pathogenesis of pneumococcal pneumonia. Am J Respir Crit Care Med. 1996;153(4 Pt 1):1339–46.
Domon H, et al. Streptococcus pneumoniae disrupts pulmonary immune defence via elastase release following pneumolysin-dependent neutrophil lysis. Sci Rep. 2016;6(1):38013.
Letsiou E, et al. Neutrophil-Derived Extracellular Vesicles Activate Platelets after Pneumolysin Exposure. Cells. 2021;10(12):3581.
Witzenrath, M., et al., Role of platelet-activating factor in pneumolysin-induced acute lung injury. Critical Care Medicine, 2007. 35(7).
Lucas R, et al. Protein kinase C-α and arginase I mediate pneumolysin-induced pulmonary endothelial hyperpermeability. Am J Respir Cell Mol Biol. 2012;47(4):445–53.
Czikora, I., et al., Epithelial Sodium Channel-α Mediates the Protective Effect of the TNF-Derived TIP Peptide in Pneumolysin-Induced Endothelial Barrier Dysfunction. Frontiers in Immunology, 2017. 8.
Witzenrath, M., et al., Role of pneumolysin for the development of acute lung injury in pneumococcal pneumonia. Critical Care Medicine, 2006. 34(7).
Reyes LF, et al. A Non-Human Primate Model of Severe Pneumococcal Pneumonia. PLoS ONE. 2016;11(11):e0166092.
Rai P, et al. Streptococcus pneumoniae secretes hydrogen peroxide leading to DNA damage and apoptosis in lung cells. Proc Natl Acad Sci. 2015;112(26):E3421–30.
Mraheil MA, et al. Dual Role of Hydrogen Peroxide as an Oxidant in Pneumococcal Pneumonia. Antioxid Redox Signal. 2021;34(12):962–78.
Steinwede K, et al. TNF-related apoptosis-inducing ligand (TRAIL) exerts therapeutic efficacy for the treatment of pneumococcal pneumonia in mice. J Exp Med. 2012;209(11):1937–52.
Bornheimer R, et al. Risk of exacerbation following pneumonia in adults with heart failure or chronic obstructive pulmonary disease. PLoS ONE. 2017;12(10):e0184877.
Musher DM, et al. The Association between Pneumococcal Pneumonia and Acute Cardiac Events. Clin Infect Dis. 2007;45(2):158–65.
Koivula I, Stén M, Mäkelä PH. Prognosis after community-acquired pneumonia in the elderly: a population-based 12-year follow-up study. Arch Intern Med. 1999;159(14):1550–5.
Sligl WI, et al. Age still matters: prognosticating short- and long-term mortality for critically ill patients with pneumonia. Crit Care Med. 2010;38(11):2126–32.
Bruns AH, et al. Cause-specific long-term mortality rates in patients recovered from community-acquired pneumonia as compared with the general Dutch population. Clin Microbiol Infect. 2011;17(5):763–8.
Eurich DT, et al. Ten-Year Mortality after Community-acquired Pneumonia A Prospective Cohort. Am J Respir Crit Care Med. 2015;192(5):597–604.
Hedlund JU, et al. Factors of importance for the long term prognosis after hospital treated pneumonia. Thorax. 1993;48(8):785–9.
Myles PR, et al. Pneumonia mortality in a UK general practice population cohort. Eur J Public Health. 2009;19(5):521–6.
Sandvall B, Rueda AM, Musher DM. Long-term survival following pneumococcal pneumonia. Clin Infect Dis. 2013;56(8):1145–6.
Lim WS, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–82.
Chalmers JD, et al. Severity assessment tools to guide ICU admission in community-acquired pneumonia: systematic review and meta-analysis. Intensive Care Med. 2011;37(9):1409–20.
Restrepo MI, Faverio P, Anzueto A. Long-term prognosis in community-acquired pneumonia. Curr Opin Infect Dis. 2013;26(2):151–8.
Johnstone J, et al. Long-term morbidity and mortality after hospitalization with community-acquired pneumonia: a population-based cohort study. Medicine (Baltimore). 2008;87(6):329–34.
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Lever A, Mackenzie I. Sepsis: definition, epidemiology, and diagnosis. BMJ. 2007;335(7625):879–83.
Gotts, J.E. and M.A. Matthay, Sepsis: pathophysiology and clinical management. Bmj, 2016. 353.
Leonard AS, et al. The overwhelming postsplenectomy sepsis problem. World J Surg. 1980;4(4):423–7.
Johansen K, Hansen ST. Symmetrical peripheral gangrene (purpura fulminans) complicating pneumococcal sepsis. Am J Surg. 1993;165(5):642–5.
Iannelli F, et al. Pneumococcal Surface Protein C Contributes to Sepsis Caused by Streptococcus pneumoniae in Mice. Infect Immun. 2004;72(5):3077–80.
Manco S, et al. Pneumococcal Neuraminidases A and B Both Have Essential Roles during Infection of the Respiratory Tract and Sepsis. Infect Immun. 2006;74(7):4014–20.
Hosea SW, Brown EJ, Frank MM. The Critical Role of Complement in Experimental Pneumococcal Sepsis. J Infect Dis. 1980;142(6):903–9.
Bello S, et al. Prognostic power of proadrenomedullin in community-acquired pneumonia is independent of aetiology. Eur Respir J. 2012;39(5):1144–55.
Kang CI, et al. Risk factors and pathogenic significance of bacteremic pneumonia in adult patients with community-acquired pneumococcal pneumonia. J Infect. 2013;66(1):34–40.
Bordon JM, et al. Bacteremic pneumococcal pneumonia: clinical outcomes and preliminary results of inflammatory response. Infection. 2015;43(6):729–38.
Ruiz LA, et al. Factors influencing long-term survival after hospitalization with pneumococcal pneumonia. J Infect. 2019;79(6):542–9.
Plouffe JF, Breiman RF, Facklam RR. Bacteremia with Streptococcus pneumoniae. Implications for therapy and prevention. Franklin County Pneumonia Study Group. JAMA. 1996;275(3):194–8.
Altamura M, et al. Splenectomy and sepsis: the role of the spleen in the immune-mediated bacterial clearance. Immunopharmacol Immunotoxicol. 2001;23(2):153–61.
Brown EJ, Hosea SW, Frank MM. The role of the spleen in experimental pneumococcal bacteremia. J Clin Investig. 1981;67(4):975–82.
Ercoli G, et al. Intracellular replication of Streptococcus pneumoniae inside splenic macrophages serves as a reservoir for septicaemia. Nat Microbiol. 2018;3(5):600–10.
Salame J, et al. Atraumatic splenic rupture in the course of a pneumonia with Streptococcus pneumoniae. Case report and literature review. Acta Chir Belg. 1993;93(2):49–53.
Corrales-Medina VF, et al. Intermediate and long-term risk of new-onset heart failure after hospitalization for pneumonia in elderly adults. Am Heart J. 2015;170(2):306–12.
Corrales-Medina VF, et al. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation. 2012;125(6):773–81.
Smeeth L, et al. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351(25):2611–8.
Feldman C, et al. Pathogenesis and prevention of risk of cardiovascular events in patients with pneumococcal community-acquired pneumonia. J Intern Med. 2019;285(6):635–52.
Huang S-T, et al. Pneumococcal pneumonia infection is associated with end-stage renal disease in adult hospitalized patients. Kidney Int. 2014;86(5):1023–30.
Luna CM, et al. The Impact of Age and Comorbidities on the Mortality of Patients of Different Age Groups Admitted with Community-acquired Pneumonia. Ann Am Thorac Soc. 2016;13(9):1519–26.
Osler, S.W., The Principles and Practice of Medicine Academic Medicine, 1944. 19(3).
Cohn AE, Jamieson RA. The action of digitalis in pneumonia. J Exp Med. 1917;25(1):65–81.
Wyckoff J, Dubois EF, Woodruff IO. The therapeutic value of digitalis in pneumonia. J Am Med Assoc. 1930;95(17):1243–9.
Violi F, et al. Cardiovascular complications and short-term mortality risk in community-acquired pneumonia. Clin Infect Dis. 2017;64(11):1486–93.
Danesh J, et al. Association of fibrinogen, c-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279(18):1477–82.
Mendall MA, et al. Relation of serum cytokine concentrations to cardiovascular risk factors and coronary heart disease. Heart. 1997;78(3):273–7.
Kumar A, et al. Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med. 1996;183(3):949–58.
Davies MJ, et al. Mammalian Heme Peroxidases: From Molecular Mechanisms to Health Implications. Antioxid Redox Signal. 2008;10(7):1199–234.
Yende S, et al. Elevated hemostasis markers after pneumonia increases one-year risk of all-cause and cardiovascular deaths. PLoS ONE. 2011;6(8):e22847.
Holter JC, et al. Risk Factors for Long-Term Mortality after Hospitalization for Community-Acquired Pneumonia: A 5-Year Prospective Follow-Up Study. PLoS ONE. 2016;11(2):e0148741.
Fillon S, et al. Platelet-Activating Factor Receptor and Innate Immunity: Uptake of Gram-Positive Bacterial Cell Wall into Host Cells and Cell-Specific Pathophysiology. J Immunol. 2006;177(9):6182.
Alloatti G, et al. Effect of platelet-activating factor (PAF) on human cardiac muscle. Int Arch Allergy Immunol. 1986;79(1):108–12.
Robertson DA, Genovese A, Levi R. Negative inotropic effect of platelet-activating factor on human myocardium: a pharmacological study. J Pharmacol Exp Ther. 1987;243(3):834.
Alhamdi Y, et al. Circulating Pneumolysin Is a Potent Inducer of Cardiac Injury during Pneumococcal Infection. PLoS Pathog. 2015;11(5):e1004836.
Brissac T, et al. Cell Invasion and Pyruvate Oxidase-Derived H2O2 Are Critical for Streptococcus pneumoniae-Mediated Cardiomyocyte Killing. Infect Immun. 2018;86(1).
Brown AO, et al. Cardiotoxicity during invasive pneumococcal disease. Am J Respir Crit Care Med. 2015;191(7):739–45.
Shenoy AT, et al. Streptococcus pneumoniae in the heart subvert the host response through biofilm-mediated resident macrophage killing. PLoS Pathog. 2017;13(8):e1006582.
Davidson JA, et al. Risk of acute respiratory infection and acute cardiovascular events following acute respiratory infection among adults with increased cardiovascular risk in England between 2008 and 2018: a retrospective, population-based cohort study. Lancet Digit Health. 2021;3(12):e773–83.
Meier CR, et al. Acute respiratory-tract infections and risk of first-time acute myocardial infarction. Lancet. 1998;351(9114):1467–71.
Beno SM, et al. Inhibition of Necroptosis to Prevent Long-term Cardiac Damage During Pneumococcal Pneumonia and Invasive Disease. J Infect Dis. 2020;222(11):1882–93.
Vandecasteele SJ, et al. The ABC of pneumococcal infections and vaccination in patients with chronic kidney disease. Clin Kidney J. 2015;8(3):318–24.
Viasus D, et al. Epidemiology, clinical features and outcomes of pneumonia in patients with chronic kidney disease. Nephrol Dial Transplant. 2011;26(9):2899–906.
Su G, et al. Short- and long-term outcomes after incident pneumonia in adults with chronic kidney disease: a time-dependent analysis from the Stockholm CREAtinine Measurement project. Nephrol Dial Transplant. 2020;35(11):1894–900.
Eknoyan G. On the Etymology of Nephritis: A Historical Appraisal of its Origins. J Am Soc Nephrol. 2020;31(6):1170–3.
Ophuls W. Subacute and chronic nephritis as found in one thousand unselected necropsies. Arch Int Med. 1912;IX(2):156–202.
Murugan R, et al. Acute kidney injury in non-severe pneumonia is associated with an increased immune response and lower survival. Kidney Int. 2010;77(6):527–35.
Ingelfinger JR. Disparities in renal endowment: causes and consequences. Adv Chronic Kidney Dis. 2008;15(2):107–14.
Burckhardt I, et al. Streptococcus pneumoniae as an agent of urinary tract infections – a laboratory experience from 2010 to 2014 and further characterization of strains. Diagn Microbiol Infect Dis. 2016;86(1):97–101.
Burckhardt I, Zimmermann S. Streptococcus pneumoniae in urinary tracts of children with chronic kidney disease. Emerg Infect Dis. 2011;17(1):120–2.
Juda, M., I. Korona-Glownik, and A. Prystupa, Streptococcus pneumoniae as an agent of urinary tract infection. Journal of Pre-Clinical and Clinical Research, 2018. 12(3).
Sarnak MJ, Jaber BL. Pulmonary infectious mortality among patients with end-stage renal disease. Chest. 2001;120(6):1883–7.
Guo H, et al. Pneumonia in incident dialysis patients—the United States renal data system. Nephrol Dial Transplant. 2008;23(2):680–6.
Dufke S, Kunze-Kronawitter H, Schubert S. Pyelonephritis and Urosepsis Caused by Streptococcus pneumoniae. J Clin Microbiol. 2004;42(9):4383–5.
Lubarsky D. Streptococcus Pneumoniae Urinary Tract Infection in 3-Year-Old Girl. Translation. 2019;6:32–4.
Wolfmeier H, et al. Active release of pneumolysin prepores and pores by mammalian cells undergoing a Streptococcus pneumoniae attack. Biochimica et biophysica acta (BBA)-general subjects. 2016;1860(11):2498–509.
Coats MT, et al. Exposure of Thomsen-Friedenreich antigen in Streptococcus pneumoniae infection is dependent on pneumococcal neuraminidase A. Microb Pathog. 2011;50(6):343–9.
Kelly R, Greiff D. Toxicity of Pneumococcal Neuraminidase. Infect Immun. 1970;2(1):115–7.
Fried L, et al. Inflammatory and prothrombotic markers and the progression of renal disease in elderly individuals. J Am Soc Nephrol. 2004;15(12):3184–91.
Huang YH, et al. Hemolytic uremic syndrome associated with pneumococcal pneumonia in Taiwan. Eur J Pediatr. 2006;165(5):332–5.
Copelovitch L, Kaplan BS. Streptococcus pneumoniae-associated hemolytic uremic syndrome. Pediatr Nephrol. 2008;23(11):1951–6.
Krysan DJ, Flynn JT. Renal transplantation after Streptococcus pneumoniae-associated hemolytic uremic syndrome. Am J Kidney Dis. 2001;37(2):E15.
Weststrate W, Hijdra A, de Gans J. Brain infarcts in adults with bacterial meningitis. Lancet. 1996;347(8998):399.
Iovino F, Molema G, Bijlsma JJ. Streptococcus pneumoniae Interacts with pIgR expressed by the brain microvascular endothelium but does not co-localize with PAF receptor. PLoS ONE. 2014;9(5):e97914.
Ring A, Weiser JN, Tuomanen EI. Pneumococcal trafficking across the blood-brain barrier. Molecular analysis of a novel bidirectional pathway. J Clin Investig. 1998;102(2):347–60.
Saukkonen K, et al. The role of cytokines in the generation of inflammation and tissue damage in experimental gram-positive meningitis. J Exp Med. 1990;171(2):439–48.
Mustafa MM, et al. Correlation of interleukin-1β and cachectin concentrations in cerebrospinal fluid and outcome from bacterial meningitis. J Pediatr. 1989;115(2):208–13.
Koedel U, et al. Role of Caspase-1 in experimental pneumococcal meningitis: Evidence from pharmacologic Caspase inhibition and Caspase-1-deficient mice. Ann Neurol. 2002;51(3):319–29.
Zwijnenburg PJG, et al. IL-1 Receptor Type 1 Gene-Deficient Mice Demonstrate an Impaired Host Defense Against Pneumococcal Meningitis. J Immunol. 2003;170(9):4724–30.
Leib SL, et al. Matrix metalloproteinases contribute to brain damage in experimental pneumococcal meningitis. Infect Immun. 2000;68(2):615–20.
Liechti FD, et al. Matrix metalloproteinase inhibition lowers mortality and brain injury in experimental pneumococcal meningitis. Infect Immun. 2014;82(4):1710–8.
Barichello T, et al. Inhibition of matrix metalloproteinases-2 and -9 prevents cognitive impairment induced by pneumococcal meningitis in Wistar rats. Exp Biol Med (Maywood). 2014;239(2):225–31.
Iovino F, et al. Interactions between blood-borne Streptococcus pneumoniae and the blood-brain barrier preceding meningitis. PLoS ONE. 2013;8(7):e68408.
Le ND, et al. Evaluation of neurofilament light chain in the cerebrospinal fluid and blood as a biomarker for neuronal damage in experimental pneumococcal meningitis. J Neuroinflammation. 2020;17(1):293.
Angstwurm K, et al. Fucoidin, a polysaccharide inhibiting leukocyte rolling, attenuates inflammatory responses in experimental pneumococcal meningitis in rats. Neurosci Lett. 1995;191(1–2):1–4.
Weber JR, et al. Anti ICAM-1 (CD 54) monoclonal antibody reduces inflammatory changes in experimental bacterial meningitis. J Neuroimmunol. 1995;63(1):63–8.
Zhou A, et al. Apoptosis induced by pneumolysin in human endothelial cells involves mitogen-activated protein kinase phosphorylation. Int J Mol Med. 2012;29(6):1025–30.
Braun JS, et al. Apoptosis-inducing factor mediates microglial and neuronal apoptosis caused by pneumococcus. J Infect Dis. 2001;184(10):1300–9.
Mitchell L, et al. Dual Phases of Apoptosis in Pneumococcal Meningitis. J Infect Dis. 2004;190(11):2039–46.
Tuomanen E, et al. The induction of meningeal inflammation by components of the pneumococcal cell wall. J Infect Dis. 1985;151(5):859–68.
Tuomanen E, et al. Nonsteroidal anti-inflammatory agents in the therapy for experimental pneumococcal meningitis. J Infect Dis. 1987;155(5):985–90.
McIntyre PB, et al. A population based study of the impact of corticosteroid therapy and delayed diagnosis on the outcome of childhood pneumococcal meningitis. Arch Dis Child. 2005;90(4):391.
Weisfelt M, et al. Cognitive outcome in adults with moderate disability after pneumococcal meningitis. J Infect. 2006;52(6):433–9.
Davydow DS, et al. Functional Disability, Cognitive Impairment, and Depression After Hospitalization for Pneumonia. Am J Med. 2013;126(7):615-624.e5.
Shah FA, et al. Bidirectional relationship between cognitive function and pneumonia. Am J Respir Crit Care Med. 2013;188(5):586–92.
Falcone M, et al. Pneumonia in frail older patients: an up to date. Intern Emerg Med. 2012;7(5):415–24.
Iwai-Saito K, et al. Frailty is associated with susceptibility and severity of pneumonia in older adults (A JAGES multilevel cross-sectional study). Sci Rep. 2021;11(1):7966.
Bienvenu OJ, et al. Depressive symptoms and impaired physical function after acute lung injury: a 2-year longitudinal study. Am J Respir Crit Care Med. 2012;185(5):517–24.
Ali NA, et al. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008;178(3):261–8.
Herridge MS, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–304.
De Jonghe B, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002;288(22):2859–67.
Marrie TJ, Beecroft MD, Herman-Gnjidic Z. Resolution of symptoms in patients with community-acquired pneumonia treated on an ambulatory basis. J Infect. 2004;49(4):302–9.
Metlay JP, et al. Time course of symptom resolution in patients with community-acquired pneumonia. Respir Med. 1998;92(9):1137–42.
Metlay JP, et al. Measuring symptomatic and functional recovery in patients with community-acquired pneumonia. J Gen Intern Med. 1997;12(7):423–30.
Marrie TJ, et al. Predictors of Symptom Resolution in Patients with Community-Acquired Pneumonia. Clin Infect Dis. 2000;31(6):1362–7.
Marrie TJ. Normal resolution of community-acquired pneumonia. Semin Respir Infect. 1992;7(4):256–70.
Fine MJ, et al. Processes and Outcomes of Care for Patients With Community-Acquired Pneumonia: Results From the Pneumonia Patient Outcomes Research Team (PORT) Cohort Study. Arch Intern Med. 1999;159(9):970–80.
Waterer GW, Kessler LA, Wunderink RG. Medium-term survival after hospitalization with community-acquired pneumonia. Am J Respir Crit Care Med. 2004;169(8):910–4.
Cecere LM, et al. Long-term survival after hospitalization for community-acquired and healthcare-associated pneumonia. Respiration. 2010;79(2):128–36.
Akiyama Y, et al. Specific pathogens as predictors of poor long-term prognosis after hospital discharge for community-acquired pneumonia. Respir Med. 2021;176:106279.
Kaplan V, et al. Pneumonia: still the old man’s friend? Arch Intern Med. 2003;163(3):317–23.
Lipsky BA, et al. Risk factors for acquiring pneumococcal infections. Arch Intern Med. 1986;146(11):2179–85.
Sibila O, et al. Prior cardiovascular disease increases long-term mortality in COPD patients with pneumonia. Eur Respir J. 2014;43(1):36–42.
Yende S, et al. The influence of pre-existing diabetes mellitus on the host immune response and outcome of pneumonia: analysis of two multicentre cohort studies. Thorax. 2010;65(10):870–7.
Sato K, et al. Improving Physical Activity Ensures the Long-Term Survival of Pneumonia Patients in a Super-Aged Society: A Retrospective Study in an Acute-Care Hospital in Japan. Tohoku J Exp Med. 2016;238(3):237–45.
Bordon J, et al. Decrease in long-term survival for hospitalized patients with community-acquired pneumonia. Chest. 2010;138(2):279–83.
Wesemann T, et al. Pneumonia severity, comorbidity and 1-year mortality in predominantly older adults with community-acquired pneumonia: a cohort study. BMC Infect Dis. 2015;15:2.
Mortensen EM, et al. Assessment of mortality after long-term follow-up of patients with community-acquired pneumonia. Clin Infect Dis. 2003;37(12):1617–24.
Tokgoz Akyil, F., et al., Prognosis of hospitalized patients with community-acquired pneumonia. Pulmonology, 2018.
Hespanhol, V. and C. Bárbara, Pneumonia mortality, comorbidities matter? Pulmonology.
Long PJ, et al. Creative approaches to nurse-midwifery education. III. Meeting specialized problems with creative solutions: an experience with faculty exchange. J Nurse Midwifery. 1975;20(3):22–4.
Polsky D, et al. Short- and long-term mortality after an acute illness for elderly whites and blacks. Health Serv Res. 2008;43(4):1388–402.
Carriere KC, et al. Outcomes and costs among seniors requiring hospitalization for community-acquired pneumonia in alberta. J Am Geriatr Soc. 2004;52(1):31–8.
Nowalk MP, et al. Racial Disparities in Adult Pneumococcal Vaccination Indications and Pneumococcal Hospitalizations in the U.S. J Natl Med Assoc. 2019;111(5):540–5.
Yende S, et al. Influence of comorbid conditions on long-term mortality after pneumonia in older people. J Am Geriatr Soc. 2007;55(4):518–25.
Burton DC, et al. Socioeconomic and racial/ethnic disparities in the incidence of bacteremic pneumonia among US adults. Am J Public Health. 2010;100(10):1904–11.
Moss M. Epidemiology of Sepsis: Race, Sex, and Chronic Alcohol Abuse. Clin Infect Dis. 2005;41(Supplement_7):S490–7.
Yende S, et al. Preinfection systemic inflammatory markers and risk of hospitalization due to pneumonia. Am J Respir Crit Care Med. 2005;172(11):1440–6.
Glynn P, et al. Circulating interleukin 6 and interleukin 10 in community acquired pneumonia. Thorax. 1999;54(1):51–5.
Yende S, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177(11):1242–7.
Hedlund J, Hansson L-O, örtqvist Å. Short- and Long-Term Prognosis for Middle-Aged and Elderly Patients Hospitalized with Community-Acquired Pneumonia: Impact of Nutritional and Inflammatory Factors. Scand J Infect Dis. 1995;27(1):32–7.
Takahashi W, et al. Interleukin-6 Levels Act as a Diagnostic Marker for Infection and a Prognostic Marker in Patients with Organ Dysfunction in Intensive Care Units. Shock. 2016;46(3):254–60.
Guertler C, et al. Inflammatory responses predict long-term mortality risk in community-acquired pneumonia. Eur Respir J. 2011;37(6):1439–46.
Wei J, et al. Increase of plasma IL-6 concentration with age in healthy subjects. Life Sci. 1992;51(25):1953–6.
Harris TB, et al. Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am J Med. 1999;106(5):506–12.
Ferrucci L, et al. The origins of age-related proinflammatory state. Blood. 2005;105(6):2294–9.
Bruunsgaard H, et al. Predicting death from tumour necrosis factor-alpha and interleukin-6 in 80-year-old people. Clin Exp Immunol. 2003;132(1):24–31.
Krüger S, et al. Cardiovascular and inflammatory biomarkers to predict short- and long-term survival in community-acquired pneumonia: Results from the German Competence Network, CAPNETZ. Am J Respir Crit Care Med. 2010;182(11):1426–34.
Gülcher SS, et al. Elevated C-reactive protein levels at ICU discharge as a predictor of ICU outcome: a retrospective cohort study. Ann Intensive Care. 2016;6(1):5.
Griffith DM, et al. Systemic inflammation after critical illness: relationship with physical recovery and exploration of potential mechanisms. Thorax. 2016;71(9):820–9.
Krüger S, et al. Pro-atrial natriuretic peptide and pro-vasopressin for predicting short-term and long-term survival in community-acquired pneumonia: results from the German Competence Network CAPNETZ. Thorax. 2010;65(3):208–14.
Ludwig E, et al. The remaining challenges of pneumococcal disease in adults. Eur Respir Rev. 2012;21(123):57–65.
Waterer GW, Somes GW, Wunderink RG. Monotherapy may be suboptimal for severe bacteremic pneumococcal pneumonia. Arch Intern Med. 2001;161(15):1837–42.
Houck PM, et al. Empiric antibiotic therapy and mortality among medicare pneumonia inpatients in 10 western states : 1993, 1995, and 1997. Chest. 2001;119(5):1420–6.
Blot, S.I., et al., Effects of delayed oxygenation assessment on time to antibiotic delivery and mortality in patients with severe community-acquired pneumonia*. Critical Care Medicine, 2007. 35(11).
Niederman, M.S., et al., Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med, 2001. 163(7): p. 1730–54.
Bartlett JG, et al. Practice guidelines for the management of community-acquired pneumonia in adults. Infectious Diseases Society of America. Clin Infect Dis. 2000;31(2):347–82.
Lim WS, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(Suppl 3):iii1-55.
Mandell LA, et al. Canadian guidelines for the initial management of community-acquired pneumonia: an evidence-based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Canadian Community-Acquired Pneumonia Working Group. Clin Infect Dis. 2000;31(2):383–421.
Metlay JP, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–67.
Garnacho-Montero J, et al. Determinants of outcome in patients with bacteraemic pneumococcal pneumonia: Importance of early adequate treatment. Scand J Infect Dis. 2010;42(3):185–92.
Garnacho-Montero J, et al. Timing of adequate antibiotic therapy is a greater determinant of outcome than are TNF and IL-10 polymorphisms in patients with sepsis. Crit Care. 2006;10(4):R111.
Zasowski EJ, et al. A Systematic Review of the Effect of Delayed Appropriate Antibiotic Treatment on the Outcomes of Patients With Severe Bacterial Infections. Chest. 2020;158(3):929–38.
Nauclér P, et al. Impact of time to antibiotic therapy on clinical outcome in patients with bacterial infections in the emergency department: implications for antimicrobial stewardship. Clin Microbiol Infect. 2021;27(2):175–81.
Mortensen EM, et al. Effects of guideline-concordant antimicrobial therapy on mortality among patients with community-acquired pneumonia. Am J Med. 2004;117(10):726–31.
Bodi M, et al. Antibiotic prescription for community-acquired pneumonia in the intensive care unit: impact of adherence to Infectious Diseases Society of America guidelines on survival. Clin Infect Dis. 2005;41(12):1709–16.
Malone DC, Shaban HM. Adherence to ATS guidelines for hospitalized patients with community-acquired pneumonia. Ann Pharmacother. 2001;35(10):1180–5.
Menendez R, et al. Influence of deviation from guidelines on the outcome of community-acquired pneumonia. Chest. 2002;122(2):612–7.
Lee C-C, et al. Timing of appropriate empirical antimicrobial administration and outcome of adults with community-onset bacteremia. Crit Care. 2017;21(1):119.
Ferrer, R., et al., Empiric Antibiotic Treatment Reduces Mortality in Severe Sepsis and Septic Shock From the First Hour: Results From a Guideline-Based Performance Improvement Program*. Critical Care Medicine, 2014. 42(8).
Kobayashi M, et al. Use of 15-Valent Pneumococcal Conjugate Vaccine and 20-Valent Pneumococcal Conjugate Vaccine Among U.S. Adults: Updated Recommendations of the Advisory Committee on Immunization Practices - United States, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(4):109–17.
McCullers JA. Insights into the interaction between influenza virus and pneumococcus. Clin Microbiol Rev. 2006;19(3):571–82.
O’brien KL, et al. Severe pneumococcal pneumonia in previously healthy children: the role of preceding influenza infection. Clin Infect Dis. 2000;30(5):784–9.
Naqvi SB, Collins AJ. Infectious Complications in Chronic Kidney Disease. Adv Chronic Kidney Dis. 2006;13(3):199–204.
Weisfelt M, et al. Pneumococcal meningitis in adults: new approaches to management and prevention. Lancet Neurol. 2006;5(4):332–42.
Koelman DLH, Brouwer MC, van de Beek D. Resurgence of pneumococcal meningitis in Europe and Northern America. Clin Microbiol Infect. 2020;26(2):199–204.
Organization, W.H., Global vaccine action plan 2011–2020. 2013.
Schuck-Paim C, et al. Effect of pneumococcal conjugate vaccine introduction on childhood pneumonia mortality in Brazil: a retrospective observational study. Lancet Glob Health. 2019;7(2):e249–56.
Andrews R, Moberley SA. The controversy over the efficacy of pneumococcal vaccine. CMAJ. 2009;180(1):18–9.
Shapiro ED, et al. The protective efficacy of polyvalent pneumococcal polysaccharide vaccine. N Engl J Med. 1991;325(21):1453–60.
Broome CV, Facklam RR, Fraser DW. Pneumococcal disease after pneumococcal vaccination: an alternative method to estimate the efficacy of pneumococcal vaccine. N Engl J Med. 1980;303(10):549–52.
Gable CB, et al. The Cost Effectiveness of Pneumococcal Vaccination Strategies. Pharmacoeconomics. 1997;12(2):161–74.
Ament A, Fedson DS, Christie P. Pneumococcal Vaccination and Pneumonia: Even a Low Level of Clinical Effectiveness Is Highly Cost-Effective. Clin Infect Dis. 2001;33(12):2078–9.
Jackson LA, et al. Effectiveness of pneumococcal polysaccharide vaccine in older adults. N Engl J Med. 2003;348(18):1747–55.
Hsiao A, et al. Incidence and Estimated Vaccine Effectiveness Against Hospitalizations for All-Cause Pneumonia Among Older US Adults Who Were Vaccinated and Not Vaccinated With 13-Valent Pneumococcal Conjugate Vaccine. JAMA Netw Open. 2022;5(3):e221111.
Moberley S, et al. Vaccines for preventing pneumococcal infection in adults. Cochrane Database Syst Rev. 2013;2013(1):Cd000422.
van Werkhoven CH, et al. Pneumococcal conjugate vaccine herd effects on non-invasive pneumococcal pneumonia in elderly. Vaccine. 2016;34(28):3275–82.
Kim JH, et al. Direct effectiveness of pneumococcal polysaccharide vaccine against invasive pneumococcal disease and non-bacteremic pneumococcal pneumonia in elderly population in the era of pneumococcal conjugate vaccine: A case-control study. Vaccine. 2019;37(21):2797–804.
Plotkin S, Jackson LA, Janoff EN. Pneumococcal Vaccination of Elderly Adults: New Paradigms for Protection. Clin Infect Dis. 2008;47(10):1328–38.
Tsai Y-H, et al. The 23-valent pneumococcal polysaccharide vaccine is effective in elderly adults over 75 years old—Taiwan’s PPV vaccination program. Vaccine. 2015;33(25):2897–902.
Thorrington D, et al. Elucidating the impact of the pneumococcal conjugate vaccine programme on pneumonia, sepsis and otitis media hospital admissions in England using a composite control. BMC Med. 2018;16(1):13.
He W, Goodkind D, Kowal PR, An aging world,. 2016. DC: United States Census Bureau Washington; 2015.
Ortman, J.M.,. Velkoff, V.A,. Hogan H, An aging nation: the older population in the United States. 2014.
Nichol KL, et al. The health and economic benefits associated with pneumococcal vaccination of elderly persons with chronic lung disease. Arch Intern Med. 1999;159(20):2437–42.
Grijalva CG, et al. Decline in pneumonia admissions after routine childhood immunisation with pneumococcal conjugate vaccine in the USA: a time-series analysis. Lancet. 2007;369(9568):1179–86.
de Oliveira LH, et al. Declines in Pneumonia Mortality Following the Introduction of Pneumococcal Conjugate Vaccines in Latin American and Caribbean Countries. Clin Infect Dis. 2021;73(2):306–13.
Wisløff T, et al. Cost effectiveness of adding 7-valent pneumococcal conjugate (PCV-7) vaccine to the Norwegian childhood vaccination program. Vaccine. 2006;24(29):5690–9.
Berman-Rosa, M., et al., Efficacy and effectiveness of the PCV-10 and PCV-13 vaccines against invasive pneumococcal disease. Pediatrics, 2020. 145(4).
Murphy, S.L., Kochanek, Kenneth D., Xu, Jiaquan, Arias, Elizabeth;, Mortality in the United States, 2020. National Center for Health Statistics (U.S.). Division of Vital Statistics., 2020. NCHS data brief ; no. 427.
Funding
National Institutes of Health, R01AI114800
National Institutes of Health, R01AI1156898
National Institutes of Health, R21AI148368
Author information
Authors and Affiliations
Contributions
K.K. and C.O. devised the main conceptual ideas and outline of the review. K.K. and K.Z. wrote the manuscript in consultation with C.O. and D.B.. All authors reviewed the manuscript and provided critical feedback. K.K. designed the figures.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kruckow, K.L., Zhao, K., Bowdish, D.M. et al. Acute organ injury and long-term sequelae of severe pneumococcal infections. Pneumonia 15, 5 (2023). https://doi.org/10.1186/s41479-023-00110-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41479-023-00110-y