Abstract
Objective
Developments in 3-dimensional (3D) printing technology has made it possible to produce high quality, affordable 3D printed models for use in medicine. As a result, there is a growing assessment of this approach being published in the medical literature. The objective of this study was to outline the clinical applications of individualized 3D printing in gynecology through a scoping review.
Data sources
Four medical databases (Medline, Embase, Cochrane CENTRAL, Scopus) and grey literature were searched for publications meeting eligibility criteria up to 31 May 2021.
Study eligibility criteria
Publications were included if they were published in English, had a gynecologic context, and involved production of patient specific 3D printed product(s).
Study appraisal and synthesis methods
Studies were manually screened and assessed for eligibility by two independent reviewers and data were extracted using pre-established criteria using Covidence software.
Results
Overall, 32 studies (15 abstracts,17 full text articles) were included in the scoping review. Most studies were either case reports (12/32,38%) or case series (15/32,47%). Gynecologic sub-specialties in which the 3D printed models were intended for use included: gynecologic oncology (21/32,66%), benign gynecology (6/32,19%), pediatrics (2/32,6%), urogynecology (2/32,6%) and reproductive endocrinology and infertility (1/32,3%). Twenty studies (63%) printed 5 or less models, 6/32 studies (19%) printed greater than 5 (up to 50 models). Types of 3D models printed included: anatomical models (11/32,34%), medical devices, (2/32,6%) and template/guide/cylindrical applicators for brachytherapy (19/32,59%).
Conclusions
Our scoping review has outlined novel clinical applications for individualized 3D printed models in gynecology. To date, they have mainly been used for production of patient specific 3D printed brachytherapy guides/applicators in patients with gynecologic cancer. However, individualized 3D printing shows great promise for utility in surgical planning, surgical education, and production of patient specific devices, across gynecologic subspecialties. Evidence supporting the clinical value of individualized 3D printing in gynecology is limited by studies with small sample size and non-standardized reporting, which should be the focus of future studies.
Similar content being viewed by others
Introduction
Recent advancements in three-dimensional (3D) printing technology have facilitated the production of 3D printed models of exemplary quality. Continued reductions in operating costs and time to generate 3D printed models has increased feasibility and gained considerable interest from the medical field. 3D printed models can be scaled to size, and display fine details, closely resembling human anatomy. As a result, there is an increasing body of literature reporting on the clinical applications of 3D printing in medicine.
In high-fidelity 3D printing protocols, segmentation software is used to convert high quality 2-dimensional (2D) Magnetic Resonance (MR), Computed Tomography (CT) or ultrasound (US) images to 3D digital models, which can then be printed [1]. Hence, 3D printed models have the ability to be patient specific, with clinical applications in personalized medicine. In gynecology, 3D printed models can depict patient-specific female pelvic anatomy and gynecologic pathology, which may benefit physicians, trainees, and patients in their understanding of complex disease and management options.
With a growing body of literature in the area of 3D printing, there has been a need to summarize the data on 3D printing and develop clinical recommendations for its use. Systematic reviews have outlined the applications of 3D printing in surgery, identifying advantages including, better visualization of anatomy for pre-operative planning, improved operative outcomes, and decreased surgical time [2, 3]. As well, there have been studies which have reviewed the uses of 3D devices within specific surgical specialties such as orthopedics, spinal surgery, neurosurgery, plastics, and urology [4,5,6,7,8]. However, challenges in summarizing the data has been reported [9] such that the overall efficacy and effectiveness of 3D printed models across medical specialties remains unknown due to the breadth of uses, lack of comparable hypotheses, and non standardized reporting of outcomes across the literature [9].
Objectives
A broad range of clinically meaningful applications for 3D printing in gynecology have been identified in the literature. The primary objective of this study is to systematically report the clinical applications of individualized 3D printing in gynecology. Additional objectives will be to summarize the production process for printing patient specific 3D printed models and determine the feasibility of personalized 3D printing in gynecology. We have chosen to use a scoping review to summarize our data, considering the challenges with performing systematic reviews on the topic of 3D printing in medicine [9] and mainly related to the heterogeneity of relevant studies.
Methods
Eligibility criteria, information sources, search strategy
A systematic review of the published literature was conducted to evaluate the uses of 3D printing in gynecology. Inclusion criteria consisted of publications up to and including 31 May 2021, of all study designs, which were published in English, had a gynecologic context and involved production of patient specific 3D printed models. Publications involving 3D imaging alone, without patient-specific 3D model production; where 3D printing was used for bioprinting, scaffolding, tissue engineering; or where 3D printing was used in a purely obstetrical context (i.e for fetal imaging, investigating fetal pathology), were excluded.
Four medical databases (Medline, Embase, CENTRAL, Scopus) and grey literature were searched using search terms which included “3D printing,” “gynecology” and relevant anatomic structures (vagina, cervix, uterus, fallopian tubes, ovaries, pelvic floor, ureters, urethra) or derivatives of these terms (Supplementary Material).
Study selection
Studies were manually screened and assessed for eligibility by two independent reviewers, (CC, TF) initially by title and abstract review and subsequently by full text review.
Data extraction
All data from studies selected for inclusion was extracted using a pre-established data extraction form. Disagreements between reviewers regarding study screening, eligibility, and data extraction were settled through discussion and consensus between the reviewers. Screening and data extraction was performed using the online platform Covidence. The study followed PRISMA protocol for scoping reviews [10].
Assessment of risk of Bias
NA
Data synthesis
The primary outcome was clinical applications of individualized 3D printing in gynecology. Additional outcomes assessed were 1) the production process used for producing 3D printed models (software, 3D printer, printing materials), 2) measures of feasibility (3D printing costs, production time). A descriptive approach for data synthesis was used.
Results
Study selection
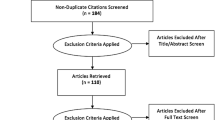
Our search yielded 4102 studies, of which 990 duplicates were removed, leaving 3112 studies to be screened. Title and abstract screening was performed by the reviewers leaving 120 studies for assessment of full text for eligibility. Eighty-eight studies were excluded for the following reasons: models were not patient specific (52), articles were duplicates (17), not the correct patient population (8), models were not printed (7), not in English (2), non-human models (1), and/or could not be accessed (1). In total 32 studies were included for review. PRIMSA flowchart can be seen in Fig. 1.
Study characteristics
Of the 32 studies reviewed, 13 (41%) were case series, 12 (38%) were case reports, 4 (13%) were cohort studies, 2 (6%) were controlled trials (1 randomized and 1 non randomized) and 1 (3%) was a retrospective study. Nineteen studies (59%) were full text articles and the remaining 13 (41%) were conference abstracts. Studies were carried out in 13 different countries, with the most common places being China (9), The United States (6) and Canda (4). Studies were performed from 2014 to most recent. Most studies (21, 66%) printed 5 or less models. Seven studies (22%) printed greater than 5, (up to 50 models) and 4 (13%) studies did not specify the number of models produced. Additional study characteristics can be seen in Tables 1 and 2.
Risk of bias
NA
Synthesis of results
Primary outcome
Clinical applications and impact of personalized 3D printed models
3D printed models were intended for use by physicians (25/32, 78%), both physicians and patients (4/32, 13%), both physicians and trainees (1/32, 3%) or patients (2/32, 6%). Models were used in studies for each of the gynecologic subspecialties including, gynecologic oncology (23/32, 72%), benign gynecology (5/32, 16%), urogynecology (2/32, 6%), pediatric gynecology (1/32, 3%), and reproductive endocrinology and infertility (1/32, 3%). Patient pathologies studied included gynecologic cancer (23/32, 72%), uterine fibroids (3/32, 9%), Mullerian anomalies (2/32, 6%), endometriosis (1/32, 3%), placenta percreta (1/32, 3%), stress urinary incontinence (1/32, 3%), and infertility (1/32, 3%). In 20 (63%) studies, the patient specific 3D printed models being produced were brachytherapy templates/cylindrical applicators; in 10 (31%) studies they were anatomical models; and in 2 (6%) studies they were other medical devices. Specific 3D printed models produced in each study can be seen in Table 1.
Secondary outcomes
3D printed model production and feasibility
Data sources used for production of the 3D printed models included: MRI (14/32, 44%), CT (7/32, 22%), both MRI and CT (5, 16%), physical exam (2/32, 6%), trial and error (2/32, 6%) or did not specify (2/32, 6%). Data software, 3D printers and 3D printing materials used varied across studies. The most commonly used 1) data software were Computer Aided Design (CAD) Software (4/32, 13%) and Solidworks (5/32, 16%); 2) 3D printers were Stratasys Fortus (3/32, 9%) and PolyJet J750 (3/32, 9%); and 3D printing material was polylactic acid (5/32, 16%). A large number of studies did not specify data software (12/32, 38%), 3D printer (13/32, 41%), or 3D printing materials (11/32, 34%) used. One study produced a 3D printed mold, from which multiple models could be produced.
3D printing costs were only provided by 2 (6%) studies and production time by 7 (22%) studies. Costs listed per model were $10.94 and $35 USD. Production time varied from 86 minutes to 5 days.
Discussion
With a growing body of literature in the area of 3D printing and continuous advancements in its technology, there has been a need to summarize the data on 3D printing and its clinical applications in medicine. We performed a scoping review to systematically report on the clinical applications of individualized 3D printing in gynecology. Although a review on the role of 3D printing in gynecology has previously been published [13], this study was limited in its reporting of applications for reproductive surgery only. Furthermore, its search was limited to a single platform (Pubmed), yeidling only 11 studies, and lacked information on the feasibility and impact of 3D printing on patient outcomes in gynecology. Here, we present on themes regarding clinical applications of patient specific 3D printing in gynecology, as summarized below.
Medical devices
Brachytherapy is an integral component of the management of both primary and recurrent gynecologic cancers. It facilitates the delivery of a high dose of localizaed radiation to a small volume tumor, while minimizing radiation dose to surrounding normal tissue [42]. To optimize treatment, selection of the most appropriate brachytherapy technique, intracavitary versus interstitial, and applicator, should be individualized based on the depth of invasion, distribution of disease, and patient specific anatomy [43]. A variety of applicator designs and sizes have been developed to limit patient discomfort while enhancing radiation dose distribution [42, 43]. However, still it remains a challenge to find an optimally fitting brachytherapy applicator for each patient’s individual anatomy and pathology [43].
Our scoping review has highlighted that patient specific 3D printed brachytherapy devices have been the most commonly studied individualized 3D printed model in gynecology in the literature to date [19,20,21,22,23, 25, 27, 29, 30, 33,34,35,36,37, 39,40,41, 44]. The 3D printed models produced and studied were mainly personalized vaginal brachytherapy cylinder applicators and or interstitial brachytherapy needle templates in a population of patients with gynecologic malignanies including primary vaginal cancer, locally advanced or recurrent cervical or endometrial cancer [19, 20, 22, 23, 25, 29, 30, 33,34,35,36,37, 39,40,41, 44]. In addition, some studies created 3D printed devices that could be personalized and used in combination with standardized applicators or templates [21, 27].
Some of the larger cohort studies provided clinically relevant results supporting the utility of individualized 3D printed devices for use in brachytherapy treatment of gynecological malignancies. Specifically, Logar et al. (2019) and Yuan et al. (2019) report increased radiation doses to the target volume and decreased dose to organs at risk, in patients with gynecologic malignancies previously treated with external beam radiation, when 3D printed individualized 1) vaginal applicators and 2) guidance templates, respectively, were used for brachytherapy treatment, in comparison to standardized devices [22, 39]. Similarly, 3D printed individualized brachytherapy trans-vaginal template/applicator +/− transperineal template facilitated high dose parameters, a high response rate (84.4% 1 month after completion), with no severe complications, in of a group of patients with central recurrent gynecologic malignancy in the study by Jiang et al. (2020) [44]. Further, Qu et al. (2021) showed that 3D-printed non-coplanar template (3D-PNCT)-assisted computed tomography (CT)-guided iodine-125 seed ablative brachytherapy could reduce the misalignment error and improve accuracy of needle puncture for non-central pelvic lesions [30].
These studies each used uniquely designed patient specific 3D printed brachytherapy applicators/templates for specific gynecologic oncology patient populations, and altogether suggest significant benefit to their use. Studies which can reproduce these results, and provide long term data on outcomes, while also investigating feasibility may facilitate wider spread use of these devices in a clinical setting in the future.
While the literature regarding the use of patient specific 3D printed personalized devices has been well explored in the context of brachytherapy applicators, there may be further utility of 3D printed personlized medical devices for other purposes. Barsky et al. (2018) showed that a patient specific silicone pessary produced from a 3D printed mold was effective in management of stress urinary incontinence and showed no short term complications [14]. Authors from another study, which was however excluded from this review due to it’s obstetrical context, similarly used 3D printing to produce a patient specific cervical cerclage pessary [45]. Unique utility was additionally shown by Pavan et al. where an individualized 3D printed vaginal mold was used by a patient with Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome following McIndoe modified vaginoplasty, as a permanent dilator post-operatively promoting return to sexual function [26].
This scoping review has outlined excellent examples of patient specific medical devices in gynecology, including brachytherapy applicator/templates, pessaries, and a vaginal dilator. Other studies have presented approaches and assessed the feasability of using 3D printing to introduce multiple shapes and sizes of various gynecologic devices such that variations in patient anatomy can be better accomodated for. Examples include connector tubing for dilatation and evacuation [46], intrauterine balloons for management of post partum hemorrhage [47], vaginal speculums [48], and drug eluting intravaginal rings [49,50,51,52,53,54]. When applicable, create patient specific devices using 3D printing can have an even greater potential for best fit, which can improve their effectiveness and patient experience. Hence efforts should be made to continue to create, produce, and study personalized devices in gynecology further. Some challenges to the widespread production and use of patient specific devices are related to cost and time burden of production, and the requirement of approval from health regulatory bodies. But, larger studies showing effectiveness and safety may help to overcome some of these limitations.
Surgical planning
Studies have also suggested a role for individualized 3D printed models for surgical planning. As initial proof of this concept, Ajao et al. and Mackey et al. produced high fidelity individualized 3D printed models which were shown to accurately represent gynecologic pathology (i.e endometriotic nodules or fibroids) in relation to the surrounding tissues, and closely correlated with patient anatomy at the time of surgery [11, 24].
Additional studies have outlined the the utility of patient-specific 3D printed models for surgical planning and intraoperative assistance further [12, 13, 16, 17, 31, 32] In preparation for benign gynecologic procedures, Flaxman et al. (2020) found that that the use of patient-specific 3D-printed models altered the surgeons’ perception of surgical difficulty, perceived risk for surgical complications, and planned hemostatic techniques, and increased their confidence in their pre-operative plan [17] and Chen et al. (2017) showed that the models decreased operative time and blood loss [16]. Baek et al. (2016) and Sayed Aluwee et al. (2017) reported that gynecologic oncologists had an increased comprehension of patient anatomy and pathology (eg. tumor size, shape, borders) [12, 32], and increased confidence in route of excision [12], with use of individualized 3D printed models, in preparation for oncologic surgeries. Finally, Barbosa et al. (2019) reported that patient specific 3D printed models provided novel information and assisted in planning of infertility procedures, including hyperoscopic myomectomy, septoplasty and embryo transfer, and assessment of ovarian reserve in preparation for IVF [13].
Overall, these studies highlight that in preparation for complex gynecologic procedures, across gynecologic subspecialties, personalized 3D printed models may provide additional infomation to the surgeon regarding patient specific anatomy and pathology, greatly assisting in the development of their surgical plan. While theoretically, with better preparation for the surgical procedure, it seems that there is the potential for the models to help to reduce complications and improve outcomes, none of the studies in this review were able to provide evidence to support this. Hence, studies are needed to further investigate surgical outcomes related to the use of patient specific 3D printed models for surgical planning to provide clearer evidence to the benefit of their use.
Two studies have also shown benefit of 3D printed patient specific models for brachytherapy planning [15, 38]. In these studies, 3D printed patient specific models were effective and non invasive for pre-planning brachytherapy in patients with cervical cancer [15, 38]. Physicians using the models, reported high fidelity and usefulness, and their overall evaluation of the cervical cancer model was 8.0 ± 0.8 points [38].
Education
Personalized 3D printed models have also been investigated as an educational tool. In one study, patient specific 3D models of Mullerian anomalies were found to increase gynecologists’ understanding of Mullerian anomalies and their confidence in surgical correction [18]. There is also evidence that they may help to promote patient education [12, 32, 38]. Patients report greater understanding of their disease and radiotherapy treatment or surgical intervention with the assistance of the 3D printed models [12, 32, 38].
The literature regarding the utility of patient specific 3D printed models for educational purposes in this scoping review appears limited. However, during our review of the literature, we did note that there is more significant data regarding the use of non-patient specific 3D printed models in education in gynecology [55,56,57]. Unfortunately, these were excluded from our scoping review due to the non-patient specific nature of the 3D printed models. This has idenitified a need for a furture study to summarize the literature regarding 3D printing overall, inclusive of both patient specfic and non-patient specific models, for the purposes of trainee education in gynecology.
Methodological considerations
Our study has identified a need for larger, higher quality studies and more consistent reporting on the topic of individualized 3D printing in gynecology. The majority of the studies in this scoping review were case reports or small case series which were proof of concept pilot studies. These studies have provided strong evidence that we now have the technology to produce patient specific 3D printed models in gynecology, and that there are many great uses possible. However, unfortunately the workflow process for production of the personalized 3D printed models including software, 3D printer, and materials used, as well as measures of feasibility, such as cost, and time for production were widely under-reported. As a result, reproducibility of these studies is limited. Further, the true feasibility of personalized 3D printed models remains unknown, as measures of feasibility were mainly unreported. Further, when they were reported, for example, cost per model of $10.94 and $35 USD, is misleading, as this does not account for the costs of the printer itself, and payment of the team who are needed to assist in preparing images for 3D printing. Further production time again was mainly unreported or else highly variable and non specific.
Finally, while the studies in this scoping review suggest clinical benefit to the use of patient specific 3D printed models, the data to support this was scant. Again, there was a focus on the ability to produce patient specific 3D printed models, but minimal data providing evidence to their impact on patient outcomes. In order for personalized 3D printing to be used in a widespread fashion in gynecology and supported by our heathcare system, we need studies which provide cost-to-benefit analysis and which provide evidence of their ability to improve patient outcomes. Hence, we are putting out a call for larger, experimental studies with clear and consistent reporting of feasibility measures on the topic of personalized 3D printing in gynecology, which will provide us with the data we need to promote their ongoing utility in this specialty.
Conclusion
Overall, this study has highlighted that there are a number of studies on the topic of personalized 3D printing in gynecology currently available. Through our scoping review we have summarized the literature to date on the topic of personalized 3D printing in gynecology and outlined many novel and potentially practice changing uses across gynecologic subspecialties. Some of these uses have included personalized applicators/templates for brachtherapy in the management of gynecologic malignancies, and other customized medical devices, as well as patient specific models for surgical planning and patient and trainee education.
Availability of data and materials
Not available.
References
Flaxman TE, Cooke CM, Miguel OX, et al. A review and guide to creating patient specific 3D printed anatomical models from MRI for benign gynecologic surgery. 3D Print Med. 2021;7:17. https://doi.org/10.1186/s41205-021-00107-7.
Tack P, Victor J, Gemmel P, et al. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15(1):115. https://doi.org/10.1186/s12938-016-0236-4.
Martelli N, Serrano C, van den Brink H, et al. Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery. 2016;159(6):1485–500. https://doi.org/10.1016/j.surg.2015.12.017.
Jiang M, Chen G, Coles-Black J, et al. Three-dimensional printing in orthopaedic preoperative planning improves intraoperative metrics: a systematic review. ANZ J Surg. 2020;90(3):243–50. https://doi.org/10.1111/ans.15549.
Wilcox B, Mobbs RJ, Wu AM, et al. Systematic review of 3D printing in spinal surgery: the current state of play. J Spine Surg. 2017;3(3):433–43. https://doi.org/10.21037/jss.2017.09.01.
Randazzo M, Pisapia JM, Singh N, et al. 3D printing in neurosurgery: a systematic review. Surg Neurol Int. 2016;7(Suppl 33):S801–S09. https://doi.org/10.4103/2152-7806.194059.
Bauermeister AJ, Zuriarrain A, Newman MI. Three-dimensional printing in plastic and reconstructive surgery: a systematic review. Ann Plast Surg. 2016;77(5):569–76. https://doi.org/10.1097/SAP.0000000000000671.
Cacciamani GE, Okhunov Z, Meneses AD, et al. Impact of three-dimensional printing in urology: state of the art and future perspectives. A systematic review by ESUT-YAUWP group. Eur Urol. 2019;76(2):209–21. https://doi.org/10.1016/j.eururo.2019.04.044.
Diment LE, Thompson MS, Bergmann JHM. Clinical efficacy and effectiveness of 3D printing: a systematic review. BMJ Open. 2017;7(12):e016891. https://doi.org/10.1136/bmjopen-2017-91.
PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Ajao MO, Clark NV, Kelil T, et al. Case report: three-dimensional printed model for deep infiltrating endometriosis. J Minim Invasive Gynecol. 2017;24(7):1239–42. https://doi.org/10.1016/j.jmig.2017.06.006 Epub 17 Jun 19.
Baek M-H, Kim D-Y, Kim N, et al. Incorporating a 3-dimensional printer into the management of early-stage cervical cancer. J Surg Oncol. 2016;114(2):150–2. https://doi.org/10.1002/jso.24292.
Barbosa MZ, Zylbersztejn DS, de Mattos LA, et al. Three-dimensionally-printed models in reproductive surgery: systematic review and clinical applications. Minerva Ginecol. 2019;71(3):235–44. https://doi.org/10.23736/S0026-4784.19.04319-3.
Barsky M, Kelley R, Bhora FY, et al. Customized pessary fabrication using three-dimensional printing technology. Obstet Gynecol. 2018;131(3):493–7. https://doi.org/10.1097/AOG.0000000000002461.
Chang A. 3D printing technology is a feasible and efficient tool for pre-planning for image guided brachytherapy of cervix cancers. Brachytherapy. 2018;17(4 Supplement 1):S111.
Chen J, He H, Song T, et al. Utilizing 3D printing model of placenta percreta to guide obstetric operation. Obstet Gynecol. 2017;129(1):42S.
Flaxman T, Cooke CM, Sheikh A, et al. Pre-surgical planning using patient-specific 3D printed anatomical models for women with uterine fibroids. J Minim Invasive Gynecol. 2020;27(7):S71–2. https://doi.org/10.1016/j.jmig.2020.08.596.
Hadden R, Grover S, Chuen J, et al. Utility of 3D printed models of Mullerian anomalies as a teaching tool. 3D Print Med Conference. 2018;4(Supplement 1). https://doi.org/10.1186/s41205-018-0036-5.
Kudla M, Batchelar D, Crook J, et al. Custom applicator design and manufacture automation for interstitial gynecological brachytherapy. Brachytherapy. 2019;18(3):S14. https://doi.org/10.1016/j.brachy.2019.04.035.
Laan RC, Nout RA, Dankelman J, et al. MRI-driven design of customised 3D printed gynaecological brachytherapy applicators with curved needle channels. 3D Print Med. 2019;5(1):8. https://doi.org/10.1186/s41205-019-0047-x.
Lindegaard JC, Madsen ML, Traberg A, et al. Individualised 3D printed vaginal template for MRI guided brachytherapy in locally advanced cervical cancer. Radiother Oncol. 2016;118(1):173–5. https://doi.org/10.1016/j.radonc.2015.12.012.
Logar HBZ, Hudej R, Segedin B. Development and assessment of 3D-printed individual applicators in gynecological MRI-guided brachytherapy. J Contemp Brachytherapy. 2019;11(2):128–36. https://doi.org/10.5114/jcb.2019.84741.
Logar H, Hudej R, Kobav M. 3d-printed multi-channel vaginal applicator for brachytherapy in gynecological cancer. International J Gynecol Cancer. 2020;30(4):A102–A03. https://doi.org/10.1136/ijgc-2020-ESGO.178.
Mackey A, Ng JI, Core J, et al. Three-dimensional-printed uterine model for surgical planning of a cesarean delivery complicated by multiple Myomas. Obstet Gynecol. 2019;133(4):720–4. https://doi.org/10.1097/AOG.0000000000003107.
Mohammadi R, Siavashpour Z, Aghdam SRH, et al. Manufacturing and evaluation of multi-channel cylinder applicator with 3D printing technology. J Contemp Brachytherapy. 2021;13(1):80–90. https://doi.org/10.5114/jcb.2021.103590.
Pavan LI, Bourguignon GA, Ubertazzi EP. Vaginoplasty: modified McIndoe using xenograft and a tailored 3D-printer mold. Int Urogynecol J Pelvic Floor Dysfunct. 2021;04:04. https://doi.org/10.1007/s00192-021-04689-y.
Petric P, Fokdal LU, Traberg Hansen A, et al. 3D-printed tandem-needle-template for image guided adaptive brachytherapy in cervical cancer. Radiother Oncol. 2019;133(1):S87. https://doi.org/10.1016/S0167-8140%2819%2930595-X.
Qu A, Sun H, Wang J, et al. 3D Printing Individual Applicator Used for Interstitial Brachytherapy in Recurrent Cervical Cancer. Brachytherapy. 2017;16(3 Supplement):S68-9. https://doi.org/10.1016/j.brachy.2017.04.119.
Qu A, Wang JJ, Jiang YL, et al. Comparison of planning between 3D-printing non-coplanar template and 3D-printing coplanar template assisted radioactive seed implantation as re-irradiation for Pelvic Wall recurrent gynecologic malignant tumors. Int J Radiation Oncol Biol Physics. 2019;105(1):E711. https://doi.org/10.1016/j.ijrobp.2019.06.875.
Qu A, Jiang P, Wei S, et al. Accuracy and dosimetric parameters comparison of 3D-printed non-coplanar template-assisted computed tomography-guided iodine-125 seed ablative brachytherapy in pelvic lateral recurrence of gynecological carcinomas. J Contemp Brachytherapy. 2021;13(1):39–45. https://doi.org/10.5114/JCB.2021.103585.
Reddy H, Maghsoudlou P, Pepin K, et al. Use of 3D model in laparoscopic myomectomy. J Minim Invasive Gynecol. 2019;26(7):S19. https://doi.org/10.1016/j.jmig.2019.09.507.
Sayed Aluwee SAZB, Zhou X, Kato H, et al. Evaluation of pre-surgical models for uterine surgery by use of three-dimensional printing and mold casting. Radiol Phys Technol. 2017;10(3):279–85. https://doi.org/10.1007/s12194-017-0397-2.
Sekii S, Tsujino K, Kosaka K, et al. Inversely designed, 3D-printed personalized template-guided interstitial brachytherapy for vaginal tumors. J Contemp Brachyther. 2018;10(5):470–7. https://doi.org/10.5114/jcb.2018.78832.
Semeniuk O, Cherpak A, Robar J. Design and evaluation of 3D printable patient-specific applicators for gynecologic HDR brachytherapy. Med Phys. 2021;20:20. https://doi.org/10.1002/mp.14888.
Sethi R, Cunha JAN, Mellis K, et al. 3d printed custom applicator for high-dose-rate intracavitary vaginal cuff brachytherapy. Brachytherapy. 2014;13:S93.
Sethi R, Cunha A, Mellis K, et al. Clinical applications of custom-made vaginal cylinders constructed using three-dimensional printing technology. J Contemp Brachytherapy. 2016;8(3):208–14. https://doi.org/10.5114/jcb.2016.60679.
Wadi-Ramahi S, Jastaniyah N, Constantinescu C, et al. 3D printed patient-specific mould for HDR gyn treatment. Med Phys. 2018;45(6):e594–e95. https://doi.org/10.1002/mp.12938.
Wang F, Luo H, Cheng H, et al. Is 3D printinggided threedimensional brachytherapy suitable for cervical cancer: from one single research institute? Eur J Gynaecol Oncol. 2020;41(4):591–7. https://doi.org/10.31083/J.EJGO.2020.04.4932.
Yuan X, Zhang Y, Miao J, et al. Dosimetric analysis of 3D-printed minimally invasive-guided template in the combined intracavitary/interstitial brachytherapy treatment of locally advanced cervical cancer. Int J Gynecologic Cancer. 2019;29(4):A284.
Zhao J, Liang Y, Liu Z, et al. Dosimetry verification of 3D-printing template assisted 125I Seedinterstitial brachytherapy for retroperitoneal lymph node metastasis in Gynecologicaloncology. Brachytherapy. 2019;18(3):S103. https://doi.org/10.1016/j.brachy.2019.04.225.
Zhao Z, Tang X, Mao Z, et al. The design of an individualized cylindrical vaginal applicator with oblique guide holes using 3D modeling and printing technologies. J Contemp Brachytherapy. 2019;11(5):479–87. https://doi.org/10.5114/jcb.2019.88441.
Jonathan S. Berek NFH, illustrations and design by Tim Hengst GBDB. Berek & Hacker's gynecologic oncology. 5th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2010.
Glaser SM, Mohindra P, Mahantshetty U, et al. Complications of intracavitary brachytherapy for gynecologic cancers and their management: a comprehensive review. Brachytherapy. 2021;20(5):984–94.
Jiang P, Qu A, Wei S, et al. The preliminary results of 3-dimensional printed individual template assisted 192Ir high-dose rate interstitial brachytherapy for central recurrent gynecologic Cancer. Technol Cancer Res Treat. 2020;19:1533033820971607. https://doi.org/10.1177/1533033820971607.
Tudela F, Kelley R, Ascher-Walsh C, et al. Low cost 3D printing for the creation of cervical cerclage pessary used to prevent preterm birth: a preliminary study. Obstet Gynecol. 2016;127(1):154S. https://doi.org/10.1097/01.AOG.0000483614.84976.50.
Stitely ML, Paterson H. Using three-dimensional printing to fabricate a tubing connector for dilation and evacuation. Obstet Gynecol. 2016;127(2):317–9. https://doi.org/10.1097/AOG.0000000000001237.
Kondoh E, Chigusa Y, Ueda A, et al. Novel intrauterine balloon tamponade systems for postpartum hemorrhage. Acta Obstet Gynecol Scand. 2019;98(12):1612–7. https://doi.org/10.1111/aogs.13692.
Wolford JE, Crawford E, Tewari SE, et al. Pilot study of 3d printed vaginal speculums (3dps) for screen-and-treat cervical neoplasia program in Mwanza, Tanzania. Int J Gynecol Cancer. 2018;28(2):86. https://doi.org/10.1097/01.IGC.0000546279.09648.02.
Welsh N, Wilson M, Malcolm K, et al. 3D printing of microbicide vaginal rings: a proof-of-concept study. AIDS Res Hum Retrovir. 2016;32(1):114. https://doi.org/10.1089/aid.2016.5000.abstracts.
Tappa K, Jammalamadaka U, Ballard DH, et al. Medication eluting devices for the field of OBGYN (MEDOBGYN): 3D printed biodegradable hormone eluting constructs, a proof of concept study. PLoS One. 2017;12(8):e0182929. https://doi.org/10.1371/journal.pone.0182929.
Walker L, Chen Y, Traore YL, et al. Mathematical prediction of hydrophilic chemotherapeutic elution kinetics from a reservoir polyurethane intravaginal ring fabricated by fused deposition modeling 3D printing. J Pharm Pharm Sci. 2017;20(2):122s.
Benhabbour SR, Janusziewicz R, Mecham S, et al. Innovative 3D printed intravaginal rings: reengineering multipurpose intravaginal rings for prevention of HIV and unintended pregnancy. AIDS Res Hum Retrovir. 2018;34(1):72. https://doi.org/10.1089/aid.2018.5000.abstracts.
Fu J, Yu X, Jin Y. 3D printing of vaginal rings with personalized shapes for controlled release of progesterone. Int J Pharm. 2018;539(1–2):75–82. https://doi.org/10.1016/j.ijpharm.2018.01.036.
Tiboni M, Campana R, Frangipani E, et al. 3D printed clotrimazole intravaginal ring for the treatment of recurrent vaginal candidiasis. Int J Pharm. 2021;596:120290. https://doi.org/10.1016/j.ijpharm.2021.120290.
Crain CL, Winfrey OK, Jackson WL, et al. Teaching pediatric straddle injury repair with use of a 3D printed model. J Pediatr Adolesc Gynecol. 2021;34(6):862–4. https://doi.org/10.1016/j.jpag.2021.05.005.
Towner MN, Lozada-Capriles Y, LaLonde A, et al. Creation and piloting of a model for simulating a minimally invasive myomectomy. Cureus. 2019;11(3):e4223. https://doi.org/10.7759/cureus.4223.
Bartellas M, Ryan S, Doucet G, et al. Three-dimensional printing of a hemorrhagic cervical cancer model for postgraduate gynecological training. Cureus. 2017;9(1):e950. https://doi.org/10.7759/cureus.950.
Funding
This work has been supported by the Physicians’ Services Incorporated Foundation Canada (Grant Number: R20–23).
Author information
Authors and Affiliations
Contributions
C.C. and T.F. did data extraction. C.C. wrote main manuscript text. L.S. conducted search strategy and provided methodological support. O.M. provided content expertise. S.S. provided study conceptualization and content expertise. All authors reviewed final manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search Strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cooke, C.M., Flaxman, T.E., Sikora, L. et al. Individualized medicine using 3D printing technology in gynecology: a scoping review. 3D Print Med 9, 6 (2023). https://doi.org/10.1186/s41205-023-00169-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41205-023-00169-9