Abstract
Background
Open defecation facilitates the transmission of pathogens that cause diarrheal diseases, which is the second leading contributor to the global burden of disease. It also exposed hundreds of millions of girls and women around the world to increased sexual exploitation. Open defecation is more practice in sub-Saharan African (SSA) countries and is considered an indicator of low socioeconomic status. However, there is little evidence on the pooled prevalence and factors contributing to open defecation practice among households in SSA.
Objectives
This study aimed to assess the pooled prevalence, wealth-related inequalities, and other determinants of open defecation practice among households in sub-Saharan Africa.
Methods
Demographic and Health Survey data sets of 33 SSA countries with a total sample of 452,281 households were used for this study. Data were weighted, cleaned, and analyzed using STATA 14 software. Meta analyses were used to determine the pooled prevalence of open defecation practice among households in SSA. Multilevel analysis was employed to identify factors contributing to open defecation practice among households in SSA. Moreover, concentration index and graph were used to assess wealth-related inequalities of open defecation practice. The associations between dependent and independent variables were presented using adjusted odds ratios and 95% confidence intervals with a p value of < 0.05.
Results
The pooled prevalence of open defecation practice among households in sub-Saharan African countries was 22.55% (95%CI: 17.49%, 27.61%) with I2 = 99.9% and ranges from 0.81% in Comoros to 72.75% in Niger. Individual level factors, such as age, educational attainment, media exposure, wealth status, and access to drinking water, as well community level factors, such as residence, country income status, and region in SSA, had a significant association with open defecation practice. The concentration index value [C = − 0.55; 95% CI: − 0.54, − 0.56] showed that open defecation practice was significantly disproportionately concentrated on the poor households (pro-poor distribution).
Conclusions
Open defecation practice remains a public health problem in sub-Saharan Africa. Individual level factors, such as age, educational attainment, media exposure, household wealth status, and access to drinking water had an association with open defecation practice. Moreover, community level factors such as residence, country income status and region in SSA have a significant effect on open defecation. There is a significantly disproportional pro-poor distribution of open defecation practice in SSA. Each country should prioritize eliminating open defecation practices that focused poorest communities, rural societies, and limited water access areas. Media exposure and education should be strengthened. Moreover, public health interventions should target to narrow the poor-rich gap in the open defecation practice among households including provisions of subsidies to the poor. Policymakers and program planners better use this evidence as preliminary evidence to plan and decide accordingly.
Similar content being viewed by others
Background
The disposal of human faces in the fields, bushes, forests, open bodies of water, beaches, and other open spaces is called open defecation [1]. According to World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) Joint monitoring program (JMP) 2021 reports, 494 million people practice open defecation [2]. Most of (92%) these people lived in rural areas and nearly half of them lived in sub-Saharan Africa [2]. There was a nearly 50% decrement (from 23 to 12%) in open defecation practice in Central and Southern Asia from 20,015 to 2020, whereas in sub-Saharan African countries, it decreased only from 22 to 18% [3].
Diarrheal disease is the second major cause of death in children under the age of five, causing 1.7 million morbidities and 760,000 deaths every year globally [4]. In Africa, it is also one of the main causes of death in under-five children [5]. Poor sanitation is a serious public health issue that has been related to several undesirable health outcomes, including diarrheal diseases and trachoma [6]. The practice of open defecation (OD) aids in the transmission of microorganisms that cause diarrheal diseases [7], with children being the most vulnerable [8]. A study showed that the prevalence of diarrhea was four times higher among OD practice communities as compared to OD-free areas [9]. Open defecation also the risks of exposing hundreds of millions of girls and women around the world to increased sexual exploitation and lack of privacy when they are menstruating [10].
Studies showed that the majority of OD practices were taken place in rural areas of low-income countries [11]. Other factors such as financial status of the household [12, 13], household size [13], occupation [13], and region [14] had an association with open defecation.
Interventions to improve human excreta disposal facilities have been demonstrated to be successful in preventing diarrheal diseases at their most important source by preventing human fecal contamination of water and soil [5, 15]. According to the 2030 Sustainable Development Agenda, no child should die or get sick as a result of drinking contaminated drinking water, and/or being exposed to other people's excreta [16].
However, with these interventions, the practice of OD in sub-Saharan Africa (SSA) is not significantly decreased [2, 17, 18] as a result, children's death due to diarrheal disease is common [19]. However, there is little evidence on the pooled prevalence and factors contributing to OD practice among households in SSA. Therefore, this study amid to assess the pooled prevalence, wealth-related inequalities, and other determinants of OD practice among households in SSA. Understanding these different patterns of inequality is an important first step in devising appropriate strategies to reduce them [20]. It is also critical to understand what factors influence the pace of improving sanitation and reducing diarrhea morbidity and mortality caused by the lack of sanitation.
Methods
Study setting, and period
This study was conducted among 33 SSA countries. The sub-Saharan is the area in the continent of Africa that lies south of the Sahara and consists of four vast and distinct regions, i.e., Eastern Africa, Central Africa, Western Africa, and Southern Africa. Together, they constitute an area of 9.4 million square miles and a total population of 1.3 billion inhabitants [21]. Recent standard DHS data set of SSA countries within 10 years (2010–2020) were our data source. To get a representative sample of recent standard DHS data from each region of SSA, 10 years of DHS data (starting from 2010) were taken. The surveys are nationally representative of each country and population-based with large sample sizes [22].
A total of thirty-three SSA countries were represented for this study in the four regions. In Eastern Africa, eleven countries (Burundi, Comoros, Ethiopia, Kenya, Malawi, Mozambique, Rwanda, Tanzania, Uganda, Zambia, Zimbabwe), in Southern Africa three countries (Lesotho, Namibia, South Africa), in Central Africa six countries (Angola, Cameroon, Chad, the Democratic Republic of the Congo, Republic of the Congo, Gabon), and in Western Africa thirteen countries (Benin, Burkina Faso, Ivory Coast, Gambia, Ghana, Guinea, Liberia, Mali, Niger, Nigeria, Senegal, Sierra Leone, Togo) were included for this study.
Population
Of the total of 47 countries located in SSA, only 41 countries had Demographic and Health Survey reports. From these, five countries, namely, Central Africa Republic (DHS report 1994/95), Eswatini (DHS report 2006/07), Sao Tome Principe (DHS report 2008/09), Madagascar (DHS report 2008/09), and Sudan (DHS report 1989–90) have a survey report before the 2010 survey year and excluded from further analysis. Moreover, three countries (Botswana, Mauritania, and Eritrea) were excluded due to the DHS data set not being publicly available. Finally, a total of 33 sub-Saharan African countries were included in this study.
All households which were found across 33 SSA countries during the survey period were our source population. Whereas households assessed for sanitation facilities during each survey across 33 SSA countries were our study population. Finally, the analysis contained a total weighted sample of 452,281 households.
Sampling method
The most recent standard census frame was used in all of the surveys conducted in the selected countries. Typically, DHS samples are stratified by administrative geographic region and by urban/rural areas within each region.
DHS sample designs are usually two-stage probability samples drawn from an existing sample frame. Stratification was achieved by separating every geographical region in the countries into urban and rural areas. In the first stage of sampling, Enumeration Areas (EAs) were selected with probability proportional to size within each stratum. In selected EAs, following the listing of the households, a fixed number of households is selected by equal probability systematic sampling The detailed sampling procedure was available in each DHS reports from the Measure DHS [22].
The household records (HR files) data sets were used. Weighted values were used before using the DHS data set to restore the representativeness of the sample data. Since the overall probability of selection of each household is not constant. DHS guideline set four sampling weighting methods and from that, we used the household sampling weight (hv005). Sample weights were generated by dividing (hv005) by 1,000,000 before use to approximate the number of cases [23]. However, there was no change in the value of the total sample size after weighting which was 452,281 (Table 1).
Study variables
The outcome variables of the study were open defecation which includes households with a lack of sanitation facility, defecating on bush or field [24]. The independent variables considered for this study were categorized as individual-level variables, such as age, sex, marital status, and educational attainment of household head, household family size, media exposure status of the households, and household wealth index. Whereas community level variables, such as place of residence, region in sub-Saharan Africa, survey year, and country income level (Table 2).
Data management and analysis
This study was performed based on the DHSs data obtained from the official DHS measure after permission was obtained. The set of household data (HR) data was used to extract the outcome and the independent variables. The data clearance, descriptive, and summary statistics were conducted using STATA version 14 software. Before we conduct any statistical analysis, the data were weighted for the sampling probabilities using the weighting factor to restore the representativeness of the survey and to get reliable statistical estimates.
The pooled estimate of open defecation practice among households in SSA and sub-regions was estimated using a metan STATA command. It was determined using the proportion of OD of each SSA country and the standard error which was calculated from the proportion and sample size in each country. Then further subgroup analyses were done to minimize the heterogeneity between studies using region in SSA, level of income of the country, and the DHS survey year.
Mixed effect analyses and model building
Since the DHS data have a hierarchical structure, where households are nested within a cluster/EAs, which violates the assumption of independence of observations and equal variance across clusters, mixed effect models which include both fixed and random effects were used to assess the clustering effect of open defecation usage among 33 sub-Saharan African countries.
The fixed effects were used to estimate the association between the likelihood of OD and explanatory variables at both individual and community levels. In the multivariable analysis, the associations between dependent and independent variables were presented using adjusted odds ratios and 95% confidence intervals with a p value of < 0.05.
Random-effects were used to estimate a measure of variation and estimated using the Interclass Correlation Coefficient (ICC), Median Odds Ratio (MOR), and Proportional Change in Variance (PCV).
The ICC reveals the variation of OD between clusters is calculated as; \(\mathrm{ICC}=\frac{\mathrm{VC}}{\mathrm{VC}+3.29}*100\%\), where VC = cluster level variance.
The MOR is defined as the median value of the odds ratio between the area at the lowest risk and at the highest risk when randomly picking out two clusters.
MOR = exp.[√(2 × VC) × 0.6745], or \({{ \mathrm{MOR}=e}^{0.95}}^{\sqrt{\mathrm{VC}}}\) where VC is the cluster level variance.
The PCV shows the variation in OD among households explained by both individual and community level factors. \(\mathrm{PCV}=\frac{V\mathrm{null}-\mathrm{VC}}{V \mathrm{null}}*100\%\) where Vnull = variance of the initial model, and VC = cluster level variance of the next model [27,28,29].
In general, in mixed-effect analysis, four models were fitted. The first was the null model containing only the outcome variables which were used to check the variability of OD in the cluster. The second and the third multilevel models contain household-level variables and community-level variables, respectively, whereas in the fourth model both household and community level variables simultaneously were fitted with the OD. Model comparison was done using the likelihood ratio and deviance test and the model with the highest likelihood and the lowest deviance was selected as the best-fitted model [27,28,29].
Concentration index and graph analyses
The concentration index and graph approach are used to examine socioeconomic inequalities in health outcomes [30, 31]. The concentration curve is used to identify whether socioeconomic inequality in some health variables exists and whether it is more pronounced at one point. It displays the share of health outcomes accounted for cumulative proportions of individuals in the population ranked by wealth status from the poorest to the richest [31, 32]. This study's health outcome variable was the cumulative proportion of open defecation practice, whereas the wealth status of the households was ranked the poorest to the richest (poorest, poorer, middle, richer, and richest).
The concentration curve would be a 450 line indicating the absence of inequity. Whereas, the concentration curve lying above and below the equality line (450) indicated that OD practice is disproportionately concentrated between poor and rich, respectively [33]. The greater the degree of inequity, the more the concentration curve diverged from the diagonal line [31]. Twice the area between the concentration curve and the diagonal line is the concentration index [32, 34]. It ranges from − 1 to + 1 and the sign indicates the direction of the relationship between the health variable (OD practice) and the distribution of living standards (wealth status) [31, 35].
Result
Sociodemographic characteristics of the study population
A total weighted 452,281 households in 33 SSA countries were included in this study. From these, nearly three fourth 328,270 (72.58%) of the household heads were males. Nearly three-fifths (61.48%) of the study participants were living in rural areas and of them about one-third (31.87%) practice OD. Nearly one-third (32.85%) of the head of household had no formal education and from them, two-fifths (38.17%) practiced OD. From the total 150,716 (35.19%) households, 34.54% were practice OD (Table 3).
The pooled prevalence of open defecation among households in sub-Saharan Africa
The overall pooled estimate of open defecation among households in sub-Saharan African countries was 22.55% (95%CI: 17.49%, 27.61%) with I2 = 99.9% and ranges from 0.81% (95%CI: 0.55, 1.07) in Comoros to 72.75% (95%CI: 71.90, 73.59) in Niger (Fig. 1).
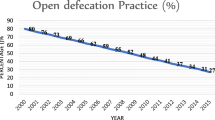
Since the I2 value was large, which shows the true variabilities (the variability not by chance) of OD among households in 33 SSA countries, then to treat this heterogeneity effect further subgroup analyses were performed based on the region in SSA, level of income of the country and the DHS survey year. Based on subgroup analysis using regions in SSA, the pooled prevalence of OD ranges from 12.02% (95%CI: 8.12%, 15.93%) in Eastern Africa across 11 countries to 31.10% (95%CI: 18.71%, 43.49%) among 13 West African countries. Moreover, the pooled prevalence of OD across countries' income levels was determined. Among 21 low-income level countries, the pooled prevalence of OD was 25.13% (95%CI: 17.73%, 32.53%), whereas it was 20.23% (95%CI: 6.50%, 33.97%) across 4 upper middle-income countries. In addition, the pooled prevalence in 15 countries whose DHS survey was conducted before and in 2015 was 31.03% (95%CI: 20.11%, 41.95%), whereas it was 15.48% (95%CI: 10.85%, 20.12%) in 18 countries whose DHS survey after 2015 (Table 4).
Multi-level analysis of factors associated with open defecation among households in sub-Saharan Africa
In random effect analysis, the ICC in the null model showed that about 36% of the variations of OD practices among study households were attributed to the difference at the cluster level. The MOR value in the null model also revealed that the median odds of using OD between the highest open defecate clusters and the lowest open defecate clusters was 3.64.
Furthermore, the PCV valve in the final model (0.054) indicates the variation in the OD usage among study households was explained by both the individual and community level factors simultaneously. Model comparison/fitness was done using loglikelihood and deviance test, then the last model (Model III) has the highest log-likelihood and the lowest deviance and was taken as the best-fitted model (Table 5).
In fixed-effect analysis, as the age of household head increase to 26–40 and ≥ 60, the odds of OD usage decrease by 27% [AOR = 0.73; 95%CI; 0.71, 0.75] and 34% [AOR = 0.65; 95%CI; 0.63, 0.67], respectively. The odds of using OD decreases by 43% and 57%, as the head of household educational status increases to primary and above primary educational status [AOR = 0.67;95%CI;0.66, 0.69] and [AOR = 0.43;95%CI; 0.42,0.44], respectively.
Households who have media exposure were 30% less likely to use OD as compared to none exposed [AOR = 0.70;95%CI; 0.69, 0.71]. Peoples who live in rural households were 2.75 times more likely to use OD as compared to urban [AOR = 2.75; 95%CI; 2.68, 2.83]. Having middle and high wealth status of the households were 0.43% and 0.14% less likely to have OD as compared to poor households [AOR = 0.43;95%CI; 0.42,0.44] and [AOR = 0.14;95%CI; 0.13, 0.14], respectively. Households who have unimproved drinking water were 1.46 times more likely to use OD than having improved drinking water [AOR = 1.46; 95%CI; 1.44,1.49].
Living in the West Africa region were nearly three times more likely to use OD, but living in Eastern Africa region were 52% less likely to practice it as compared to living in Central Africa regions, [AOR = 2.758;95%CI; 2.64, 2.80] and [AOR = 0.48;95%CI; 0.46, 0.49], respectively (Table 5).
Wealth related inequality of open defecation
In this study, the wag staff normalized concentration index (C) and curve were done to assess the wealth-related inequality of OD practice among households in SSA. The result showed that OD was significantly disproportionately concentrated on the poor households (pro-poor distribution) with [C = − 0.55; 95% CI: − 0.54, − 0.56], which means that when households income status becomes lowest the burden of practicing OD is increasing. The graph in Fig. 2 also showed that the distribution line of OD is above the line of equality. This shows that OD among households in SSA was disproportionately concentrated on the poor household (pro-poor distribution) (Fig. 2).
Discussion
This study was conducted to assess the pooled prevalence and determinants of open defecation among households in SSA. Based on this the pooled prevalence of OD practice among households of 33 SSA countries was 22.55% (95%CI: 17.49%, 27.61%). This is in line with a report by the Joint Monitoring Program (JMP) of WHO and UNICEF 2021 report in sub-Saharan Africa (18%) [2]. However, this study is lower than studies in India (39.91% and 43%) [36, 37] and, higher than a JMP 2021 report worldwide (6%), and Central and Southern Asia (12%) [2] of households practicing OD. This might be due to the difference in government commitments and involvement of different community initiative programs, which have a better approach toward the reduction of OD practice and the achievement of the desired sanitation program [12, 38]. Having household money constraints to build the sanitation facilities is also another reason to practice it [37]. On the other hand, having a toilet facility at home may not be a guarantee to use toilet facilities [13]. The community accustomed to it as the old habit are also another reason for more practicing OD [37].
In this study as the age of household head increases, the chance of OD practice becomes decreases. This is supported by studies in rural North India and Tanzania, OD practice decreases sharply among the oldest household members [39, 40]. The study in Indonesia is also showed that OD practice increasing among adults [41]. This might be due to that, as the age increases people on average are unable to move more freely outside their homes. On the other side, disability or incontinence mostly occurs in the advanced age group, which makes OD difficult or impractical [39].
In this study OD practice decrease as the educational status of the household head increase. This is supported by a study in a systematic review and meta-analysis in Ethiopia [42], a study in Tanzania [43], Nigeria [44], and Ghana [13]. This might be because educated household heads have a relatively better understanding of the relevance of having sanitation facilities and the effects of OD practice. Moreover, a higher level of education status increases the probabilities of income earning capacity of households, which is the main constrain to constructing a toilet facility [37, 45].
Households that have limited access to drinking water were more likely to use OD. This is supported by a study in Dangilla Ethiopia, which showed that having limited water access has an association with OD practice [9]. This is could be explained by the fact that households having water shortages could not keep their hygiene and might not have water for toilet usage.
In our finding, households who have media exposure were less likely to use OD. It is supported by a study in India [46], in Nigeria [47] which showed that using mass media, social media, and community-based media was important for the prevention of OD practice. Exposure to mass media increases awareness about the impacts of open defecation and enables a better internalize the benefits of using a toilet [44, 46].
In this study, having middle and high wealth status of the household, as well as households from lower-middle and upper middle-income level countries, were less likely to have OD as compared to poor households and households from lower-income level. This is in line with a study in Ethiopia [4], Nigeria [44], and Gahanna [13]. The majority of OD practices have been taking place in low-income countries [11]. However, in contrast to other studies, the prevalence of OD in upper middle-income countries was higher than in the lower middle-income countries in this study. This might be due to a small number of countries eventually a small sample sizes included in upper middle-income countries as compared to lower middle-income.
The concentration index and graph in this study also revealed that OD was significantly disproportionately concentrated in poor households. This is in line with a study in Tanzania, where a pro-poor distribution of OD practice [40]. Studies showed that there are economic inequalities of OD practices between the poorest and richest households [14]. Absolute sanitation inequalities are greatest in countries such as Pakistan with the largest spread between the richest and the poorest [20]. Countries that practiced OD most widely are those with high levels of poverty [13, 20]. A study showed that per capita aid disbursement for sanitation had a strong relationship to OD reduction in low-income countries [11].
In this study, rural households were more likely to use OD as compared to urban. This is in line with WHO reports [14], a study done in Nigeria [44], India [48], and Nepal [49]. This might be due to an unequal distribution of power and limited access to infrastructure, information, and income which leads to poor practices of OD and limited sanitation in rural residences [44].
The main strength of this study was the use of the weighted nationally representative data with a large sample which makes it representative at the national. Therefore, it can be generalized to all households during the study period in SSA countries. Moreover, the use of pooled estimation and a multilevel model took into account the nested nature of the DHS data and the variability within the countries to get a reliable estimate and standard errors. Another strength of this study was estimating the pooled estimate of OD practice in sub- Saharan Africa and sub-regions will give invaluable information for region-specific intervention. However, it is not free of limitations. The heterogeneity of the pooled estimate of OD was not managed using further subgroup analysis. Moreover, since we use the secondary data recall biases and social desirability biases might be expected.
Conclusions
Open defecation practice remains a public health problem in sub-Saharan Africa. Individual level factors, such as being aged, having higher educational attainment, having media exposure, and having middle and higher household wealth status had a preventive effect for OD practice. However, having limited access to drinking water had a positive association with it. Moreover, community level factors, such as living in rural residences, and living in West African countries had a positive association with OD practice whereas living in East Africa and living in lower-income and lower middle income have a preventive effect for OD. There is a significantly disproportional pro-poor distribution of OD practice in SSA which means that its distribution favors the poor households. Each country should prioritize eliminating OD that focused poorest communities, rural societies, and limited water access regions. Media exposure and education should be strengthened. Moreover, public health interventions should target to narrow the poor-rich gap in the OD practice among households. Policymakers and program planners better use this evidence as preliminary evidence to plan and decide accordingly.
Availability of data and materials
Data is available online from the “measures DHS program” and taken after writing a concept note and getting permission to use it. Anyone can access this data set by registering through this website https://dhsprogram.com/data/new-user-registration.cfm. You can access the data set through the following my data set account https://dhsprogram.com/data/dataset_admin/login_main.cfm?CFID=10818526&CFTOKEN=c131014a480fe56-4E0C6B7F-F551-E6B2-5081744BEE982E82. The following under quotation sentences are the direct instructions, and additional information from DHS programs to use the data set. “Before you can download data sets, you must register as a DHS data user. Data set access is only granted for legitimate research purposes. Learn more about data restrictions, why we require registration, how to request access or view a list of available datasets”.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- DHS:
-
Demographic and Health Survey
- HR:
-
Household record
- JMP:
-
Joint Monitoring Program
- OD:
-
Open defecation
- SDG:
-
Sustainable development goal
- WHO:
-
World Health Organization
- UNICEF:
-
United Nations Children’s Fund
References
Organization, W.H. and UNICEF. Progress on sanitation and drinking-water. 2013: World Health Organization.
Organization, W.H. Progress on household drinking water, sanitation and hygiene 2000–2020: five years into the SDGs. 2021.
Abebe TA, Tucho GT. Open defecation-free slippage and its associated factors in Ethiopia: a systematic review. Syst Rev. 2020;9(1):252.
Gebru T, Taha M, Kassahun W. Risk factors of diarrhoeal disease in under-five children among health extension model and non-model families in Sheko district rural community, Southwest Ethiopia: a comparative cross-sectional study. BMC Public Health. 2014;14(1):1–6.
Liu L, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61.
Spears, D., A. Ghosh, and O. Cumming, Open defecation and childhood stunting in India: an ecological analysis of new data from 112 districts. PloS one, 2013. 8(9): p. e73784.
Galan DI, Kim SS, Graham JP. Exploring changes in open defecation prevalence in sub-Saharan Africa based on national level indices. BMC Public Health. 2013;13(1):1–2.
Debela TH, et al. Fecal contamination of soil and water in sub-Saharan Africa cities: the case of Addis Ababa, Ethiopia. Ecohydrol Hydrobiol. 2018;18(2):225–30.
Ayalew AM, et al. Assessment of diarrhea and its associated factors in under-five children among open defecation and open defecation-free rural settings of Dangla District, Northwest Ethiopia. J Environ Public Health. 2018. https://doi.org/10.1155/2018/4271915.
Nations, U. United Nations Department of Economic and Social Affairs, Transformational benefits’ of ending outdoor defecation: Why toilets matter available on,https://www.un.org/development/desa/en/news/sustainable/world-toilet-day2019.html. 2018.
Galan DI, Kim S-S, Graham JP. Exploring changes in open defecation prevalence in sub-Saharan Africa based on national level indices. BMC Public Health. 2013;13(1):1–12.
Abebe TA, Tucho GT. Open defecation-free slippage and its associated factors in Ethiopia: a systematic review. Syst Rev. 2020;9(1):1–15.
Osumanu IK, Kosoe EA, Ategeeng F. Determinants of open defecation in the Wa municipality of Ghana: empirical findings highlighting sociocultural and economic dynamics among households. J Environ Public Health. 2019. https://doi.org/10.1155/2019/3075840.
Organization WH, UNICEF. Progress on drinking water, sanitation and hygiene update and SDG baselines 2017. 2017, WHO, Geneva.
Clasen TF, et al. Interventions to improve disposal of human excreta for preventing diarrhea. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.CD007180.pub2.
Organization, W.H. and UNICEF, Progress on Drinking Water, Sanitation and Hygiene Update and SDG Baselines 2017. 2017, WHO, Geneva.
Leshargie CT, et al. Household latrine utilization and its association with educational status of household heads in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2018;18(1):1–12.
WHO U. Safely managed drinking water-thematic report on drinking water. Geneva: World Health Organisation (WHO) and the United Nations Children’s Fund (UNICEF), 2017.
UNICEF. Sanitation issue. Addis Ababa: Ethiopian Newsletter, 2004.
Programme WUJWSSM. Progress on sanitation and drinking water: 2015 update and MDG assessment. 2015: World Health Organization.
Worldometr, Subregions in Africa by population (2021). 2021.
Croft et al. Guide to DHS Statistics. . 2018: Rockville, Maryland, USA: ICF.
Croft T, Marshall A, Allen C. Guide to DHS Statistics: DHS-7 (version 2). 2020.
Croft T, Aileen M, Marshall A, Allen C. (2018). Guide to DHS statistics.
Worku MG, et al. Prevalence and associated factors of adolescent pregnancy (15–19 years) in East Africa: a multilevel analysis. BMC Pregnancy Childbirth. 2021;21(1):1–8.
Bank W. World Bank List of Economies (June 2019). 2019.
Liyew AM, Teshale AB. Individual and community level factors associated with anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health survey, 2016; a multilevel analysis. BMC Public Health. 2020;20:1–11.
Merlo J, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Commun Health. 2005;59(6):443–9.
Merlo J, et al. A brief conceptual tutorial on multilevel analysis in social epidemiology: interpreting neighborhood differences and the effect of neighborhood characteristics on individual health. J Epidemiol Commun Health. 2005;59(12):1022–9.
Kakwani N, Wagstaff A, Van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econ. 1997;77(1):87–103.
Debie A, et al. Complete vaccination service utilization inequalities among children aged 12–23 months in Ethiopia: a multivariate decomposition analyses. Int J Equity Health. 2020;19:1–16.
Wagstaff A, Paci P, Van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33(5):545–57.
Heckley G, Gerdtham U-G, Kjellsson G. A general method for decomposing the causes of socioeconomic inequality in health. J Health Econ. 2016;48:89–106.
Wagstaff A, Watanabe N. Socioeconomic inequalities in child malnutrition in the developing world. 1999: The World Bank.
O'Donnell O, et al. Analyzing health equity using household survey data: a guide to techniques and their implementation. 2007: The World Bank.
Gupta A, et al. Changes in open defecation in rural north India: 2014–2018. 2019.
Patwa J, Pandit N. Open defecation-free India by 2019: How villages are progressing? Indian J Commun Med. 2018;43(3):246.
Kar K, Chambers R. Handbook on community-led total sanitation. 2008.
Coffey D, et al. Revealed preference for open defecation. Econ Pol Wkly. 2014;49(38):43.
Maliti E. Evolution of open defecation prevalence in Tanzania 2002–2015: evidence from national demographic and health surveys. Dev Pract. 2021;31(1):112–24.
Indriyani Y, Wibowo A, Indawati R. The behaviour of open defecation by age groups. Indian J Public Health Res Dev. 2019. https://doi.org/10.37506/v10/i12/2019/ijphrd/192178.
Leshargie CT, et al. systematic review and meta-analysis. BMC Public Health. 2018;18(1):1–12.
Mumbi TL, Cholo W. An assessment of open defecation among residents of Thika East Sub-County, Kiambu County, Kenya. Int J Med Res. 2017;2(3):09–20.
Abubakar IR. Exploring the determinants of open defecation in Nigeria using demographic and health survey data. Sci Total Environ. 2018;637:1455–65.
Paavola J. Livelihoods, vulnerability and adaptation to climate change in Morogoro, Tanzania. Environ Sci Policy. 2008;11(7):642–54.
Chatterjee A, Agarwal S. Can women empowerment help to reduce open defecation in india: evidence from NFHS 4. 2019.
Ngwu UI. The practice of open defecation in rural communities in Nigeria: a call for social and behavior change communication intervention. Int J Commun Res. 2017;7(3):201–6.
O’Reilly K, Dhanju R, Goel A. Exploring “the remote” and “the rural”: open defecation and latrine use in Uttarakhand, India. World Dev. 2017;93:193–205.
Bhatt N, et al. What motivates open defecation? A qualitative study from a rural setting in Nepal. PLoS ONE. 2019;14(7): e0219246.
Acknowledgements
We would like to thank the “measure DHS program” for providing the data set. I would like to thank Mr. Zewudu Andualem (MSc. Environmental health) for his support and advice on the journey of this manuscript preparation.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
The conception of the work, design of the work, acquisition of data, analysis, and interpretation of data behavior by DGB, MHA, MG, and NTT. Data curation, drafting the article, revising it critically for intellectual content, validation and final approval of the version to be published was done by DGB, MHA, MG, NTT, ME, and FMA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study doesn’t involve the collection of information from subjects. It is a further secondary data analysis. Consent to participate is not applicable. Since the study is a secondary data analysis based on DHS data. The “measures DHS program” waived all the consent and ethical approval letters.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. There are no financial, non-financial, and commercial organizations competing of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Melaku Hunie Asratie, Fantu Mamo Aragaw, Nuhamin Tesfa Tsega, Mastewal Endalew and Moges Gashaw are co-authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Belay, D.G., Asratie, M.H., Aragaw, F.M. et al. Open defecation practice and its determinants among households in sub-Saharan Africa: pooled prevalence and multilevel analysis of 33 sub-Saharan Africa countries demographic and health survey. Trop Med Health 50, 28 (2022). https://doi.org/10.1186/s41182-022-00416-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-022-00416-5