Abstract
Background
Maternal anemia is a worldwide public health problem especially in developing countries including Ethiopia. The anemia burden among lactating mothers was higher in Africa particularly in Ethiopia, and scant attention was paid. To date, there is limited evidence on community level determinants of anemia among lactating mothers in Ethiopia. This study, therefore, aimed to assess the prevalence and factors associated with anemia among lactating mothers in Ethiopia.
Methods
Secondary data analysis was employed using the 2016 Ethiopian Demographic and Health Survey. A total weighted sample of 4658 lactating women was included. A multilevel logistic regression model was used to identify individual and community level determinants of anemia during lactation. Finally, the adjusted odds ratio with a 95% confidence interval was reported.
Results
The overall prevalence of anemia was 28.3% (95% CI; 26.7, 30.0) with the higher regional prevalence in Somali (68.3%) and Afar (47.2%) regions. Current modern contraceptive use [AOR = 0.71; 95% CI: 0.58, 0.87], Poorer [AOR = 0.77; 95% CI: 0.61, 0.98], middle [AOR = 0.74; 95% CI: 0.56, 0.97], rich [AOR = 0.64; 95% CI: 0.46, 0.85], and richest [AOR = 0.66; 95% CI: 0.43, 0.98] wealth index, being working within the 12 months preceding the survey [AOR = 0.77; 95% CI: 0.64, 0.92], and taking iron during pregnancy [AOR = 0.82; 95% CI: 0.68, 0.98] were associated with lower odds of anemia. Whereas, being female household head [AOR = 1.22; 95% CI: 1.01, 1.49], having two births [AOR = 1.27; 95% CI: 1.04, 1.55] and three to four births [AOR = 1.53; 95% CI: 1.14, 2.06] within 5 years, and higher community illiteracy level [AOR = 1.06; 95% CI: 1.06, 1.70] were associated with the increased odds of anemia during lactation.
Conclusion
In this study the prevalence of anemia among lactating mothers was high. It was affected by both individual and community level factors. Therefore, focusing on family planning services especially on modern contraceptive methods, iron supplementation during pregnancy, child spacing, and improving community literacy could decrease anemia during lactation.
Similar content being viewed by others
Background
Anemia refers to low hemoglobin in blood with a cutoff point < 110 g/L for pregnant women and < 120 g/L for non-pregnant women [1]. It is a condition which is characterized by a decreased number of red blood cells or hemoglobin level that results in insufficient oxygen-carrying capacity of blood to meet the cellular metabolic demand of the body. It is a worldwide public health problem affecting both developing and developed countries and all population groups [2]. The World Health Organization (WHO) defines anemia as a major public health problem, moderate public health problem, and mild public health problem when prevalence is over 40%, between 20 and 40%, and between 5 and 20% respectively [3].
Globally, 38% of pregnant women and 29% of non-pregnant women are anemic. Pregnant women in low-income and middle-income countries had high rates of anemia, in which the highest prevalence rates are reported in Central and West Africa (56%), South Asia (52%), and East Africa (36%) [4]. Iron deficiency is the major contributor to anemia globally and it is a major nutritional problem that accounted for 50% of the cases of anemia. However, folic acid, vitamin B12, and vitamin A deficiency can also cause nutritional deficiency anemia. In addition, acute and chronic inflammations, parasitic infections, and acquired or inherited disorders that affect the synthesis of hemoglobin and production or survival of red blood cells can be causes for anemia [2, 3].
Anemia in lactating mother is common especially if the mother were anemic during their pregnancy [5]. Lactating mothers are vulnerable to anemia morbidity due to their susceptibility to iron depletion during pregnancy and lactation as well as due to bad consequences of blood loss during their childbirth [6, 7]. Prevalence of anemia in lactating mother is different across different regions of the world; in Vietnam 66%, in India 63%, in Myanmar 60.3%, in Kenya 43.8%, and in china which is 32.7% [8,9,10,11,12]. In Ethiopia, the burden of anemia in lactating mothers ranges from 10.9 to 28.7% [13,14,15].
Anemia in lactating mother has various adverse effects like decreased immunity which in turn results in; delayed wound healing, and increased susceptibility to infections such as mastitis, ductitis, and urinary tract infection and diminished quality or volume of the breast milk. It has also associated with reduction of global household income, cognitive impairment, impaired quality of life, and emotional instability as well as postpartum depression [16,17,18,19]. These devastating impacts make anemia in lactating mothers to be one of the global health priority areas at the global level, especially in resource-limited areas [20].
Evidences revealed that different factors such as; maternal age, educational status of the mother, parity, wealth status, sex of household head, maternal body mass index (BMI), antenatal care (ANC) visit, cesarean delivery, history of a terminated pregnancy, smoking, health insurance, maternal occupation, religion, marital status, source of drinking water, type of toilet facility, place of delivery, iron supplementation during pregnancy, current modern contraceptive use, duration of breastfeeding, number of births within the past 5 years, birth interval, region, and place of residence are associated with anemia among lactating mothers [11, 15, 21,22,23,24,25].
Reducing anemia in women of reproductive age is considered an essential part of improving the health of a woman, and WHO has set a global target of achieving a 50% reduction of anemia among women of reproductive age by 2025 [26]. To achieve this target tackling anemia during lactation have its great importance. So far there are limited studies conducted in Africa particularly in Ethiopia and community level factors that might affect anemia during lactation were largely overlooked. Therefore, this study was aimed to assess the prevalence and the individual and community level factors associated with anemia during lactation. Since this is based on nationally representative data, it will give an insight for health professionals and policymakers in understanding the burden of anemia in lactating mothers and its determinants for setting possible interventions at both individual and community levels.
Methods
Study setting
The study was conducted in Ethiopia (3o -14o N and 33o - 48°E) which is located at the horn of Africa. The country covers 1.1 million Sq. km and has a great geographical diversity, which ranges 4550 m above sea level down to the Afar depression to 110 m below sea level. There are nine regional states and two city administrations subdivided into 68 zones, 817 districts, and 16,253 kebeles (lowest administrative units of the country) in the administrative structure of the country [27].
Data source and sampling procedure
For this study, we used the 2016 Ethiopian Demographic and Health Survey (EDHS) data which was conducted from January 18, 2016, to June 27, 2016. It is a nationally representative data containing key health indicators such as; child and maternal health, and anemia among reproductive-age women. Besides, the sociodemographic and socioeconomic characteristics of the respondents were also collected and found in the survey.
A stratified two-stage cluster sampling procedure was employed to select study participants. In the first stage, 645 enumeration areas (EAs) (202 urban and 443 rural) were selected from a list of 84,915 EAs created for the 2007 Ethiopia Population and Housing Census. Then, in the second stage, 28 households per each cluster were selected. A total of 16,583 eligible women were interviewed. The hemoglobin level was measured for those eligible reproductive-aged women and adjusted for altitude using the adjustment formula (adjust = − 0.032*alt + 0.022*alt2 and adjHb = Hb - adjust (for adjust > 0) [27, 28]. In the current study, a total weighted sample of 4658 lactating mothers was included. To reach such sample size several exclusion criteria were employed (Fig. 1). Further information regarding the data collection procedure, questionnaire, in general about how the survey was conducted, is found in the EDHS 2016 report [27].
Variables of the study
Dependent variable
The current study was based on the altitude adjusted hemoglobin level which was already provided in the EDHS data. The outcome variable is anemia in lactating mother, which is operationalized as a categorical variable by predefined cut-off points for mild, moderate, and severe anemia recommended by the WHO for women above the age of 15 years. For this analysis, we recategorized anemia level as anemic and non-anemic from prior classifications in levels (no, mild, moderate, severe) because of very small numbers of cases in the categories of severe and mild anemia. Therefore, women with hemoglobin level < 120 g/L were considered as anemic and coded as “1” whereas those nonanemic were coded as “0” for our analysis.
Independent variables
For this study both individual and community level variables were considered. The mothers’ age, educational level of the mother, parity, wealth status, sex of household head, BMI, ANC visit, cesarean delivery, history of a terminated pregnancy, smoking, health insurance, maternal occupation, religion, marital status, perception of distance from the health facility, source of drinking water, type of toilet facility, place of delivery, iron supplementation during pregnancy, current modern contraceptive use, duration of breastfeeding, births within the past 5 years and birth interval were considered as individual level variables. Whereas community poverty, community media exposure, community illiteracy level, region, and place of residence were considered as community level variables. Some individual level variables were recategorized to make them suitable for analysis. The aggregate community level explanatory variables were constructed by aggregating individual level characteristics at the community (cluster) level. They were dichotomized as high or low based on the distribution of the proportion values computed for each community, after checking their distribution. Since all aggregated variable was not normally distributed, the median value was used as a cut-off point for categorization. Community poverty level was categorized as high if the proportion of women from the two lowest wealth quintiles in a given community was 50–100% and low if the proportion was 0–49%. Community media exposure was categorized as low if the proportion of women exposed to media in the community was 0–28.60% and categorized as high if the proportion above 28.60%. Community illiteracy level was categorized as high if the proportion of illiterate women per cluster was 83.3–100% and low if it was less than 83.30%. These independent variables (both individual and community level variables) were constructed/adapted from the searching of different literatures.
Model building
Four models were fitted. The first was the null model (Model I) containing no exposure variables which was used to check the variability of anemia in the community and provide evidence to assess random effect using the intraclass correlation coefficient (ICC). The second (Model II) and the third (Model III) multilevel models contain individual level variables and community level variables respectively. In the fourth model (Model IV) both individual and community level variables were fitted simultaneously with the outcome variable. Model comparison was done using deviance and the model with the lowest deviance was selected as the best-fitted model.
Parameter estimation method
The fixed effects (a measure of association) were used to estimate the association between the likelihood of anemia and explanatory variables at both community and individual levels and were expressed as odds ratios with 95% confidence interval. Regarding the measures of variation (random-effects), median odds ratio (MOR), ICC, and Proportional Change in Variance (PCV) were estimated.
The MOR aims to translate the area level variance in the widely used odds ratio scale, which has a consistent and intuitive interpretation. The MOR is defined as the median value of the odds ratio between the area at the highest risk and the area at the lowest risk when randomly picking out two areas or clusters. The MOR can be conceptualized as the increased risk (in median) that would have if moving to another area with a higher risk.
It is computed by; MOR = exp.[√(2 × Va) × 0.6745], where; VA is the area level variance, and 0.6745 is the 75th centile of the cumulative distribution function of the normal distribution with mean zero and variance one [29, 30]. Whereas the PCV reveal the variation in anemia among lactating mother across communities which is explained by both individual and community level factors. The PCV is calculated as; PCV = [(VA-VB)/VA]*100 [30, 31], where; VA = variance of the initial model, and VB = variance of the model with more terms. Moreover, the ICC which reveals the variation of anemia between clusters is calculated as; ICC = [VA/(VB + 3.29)], where; VA = area/cluster level variance, and VB = individual level variance [30].
Results
Sociodemographic characteristics of study participants
In this study, we used weighted samples of 4658 breastfeeding/lactating women. The median age of the study participants was 28 (IQR = 24–33) years. About half (49.52%) of study subjects had no formal education and the majority (39.17%) of respondents were followers of orthodox religion. Regarding household status, 22.64 and 22.63% of study subjects were from the poorest and poorer households. The majority (74.70%) of lactating mothers had normal nutritional status (BMI = 18.5–24.99) and 95.21% of respondents were not covered by health insurance. Most (72.29%) of respondents had no media exposure and 59.29% perceived distance from the health facility as a big problem. Looking to source of drinking water and type of toilet facility, 42.97 and 91.21% of study subjects used unimproved water sources for drinking and unimproved toilet facility respectively. Regarding respondent’s residence and region, 89.26 and 96.65% of respondents were from rural residence and agrarian regions respectively (Table 1).
Prevalence of anemia among lactating mothers in Ethiopia, 2016
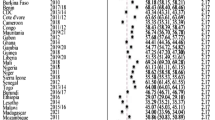
The prevalence of anemia in this study was 28.3% (95% CI; 26.7, 30.0). Regarding the regional prevalence of anemia during lactation, the highest prevalence was observed in the Somali region (68.3%) followed by the Afar region (47.2%).
Random effect and model comparison
Table 2 revealed the random effect or community variation and model comparison/fitness. As indicated from the table, the ICC in the null model was 0.21, which means about 21% of the variations of anemia in lactating mothers were attributable to the difference at cluster level or community level factors. The higher MOR value (2.46) in the null model also revealed that anemia among lactating mothers was different between clusters or EAs. Furthermore, the higher PCV value (0.44) in the final model indicates that about 44% of the variation of anemia among lactating mothers was attributable to both the individual level and community level factors. Regarding model comparison/fitness, we used deviance and the model with the lowest deviance value (Model IV) was the best-fitted model.
Determinants of anemia among lactating mothers
In the bivariable multilevel logistic regression analysis all factors, except maternal age, smoking, marital status, birth interval, health insurance coverage, and religion, were associated with anemia in lactating mother (p < 0.20). In the multivariable analysis household wealth status, maternal working status within the 12 months preceding the survey, sex of household head, current modern contraceptive use, iron supplementation during their last pregnancy, number of births within 5 years and community illiteracy level was significantly associated with anemia in lactating women (p < 0.05).
Mothers from poorer, middle, rich and richest households had 23% [Adjusted odds ratio (AOR) = 0.77; 95% CI: 0.61, 0.98], 26% [AOR = 0.74; 95% CI: 0.56, 0.97], 36% [AOR = 0.64; 95% CI: 0.46, 0.85], and 34% [AOR = 0.66; 95% CI: 0.43, 0.98] lower odds of having anemia as compared to mothers from poorest households. Looking at the sex of the household head, being mothers from households with female household head had 1.22 [AOR = 1.22; 95% CI: 1.01, 1.49] times higher odds of having anemia. The odds of anemia were 23% [AOR = 0.77; 95% CI: 0.64, 0.92] lower among lactating mothers who had been working within the 12 months preceding the survey as compared to their counterparts. The odd of having anemia was 18% [AOR = 0.82; 95% CI: 0.68, 0.98] lower in mothers who took iron during their last pregnancy as compared to their counterpart. Lactating mothers who use modern contraceptive methods currently have 29% [AOR = 0.71; 95% CI: 0.58, 0.87] lower odds of having anemia. Regarding the number of births within 5 years, lactating mothers who had two and three to four births had 1.27 [AOR = 1.27; 95% CI: 1.04, 1.55] and 1.53 [AOR = 1.53; 95% CI: 1.14, 2.06] times higher odds of anemia as compared to mothers who had one birth within 5 years. Moreover, lactating mothers from communities with higher illiteracy had 1.34 [AOR = 1.06; 95% CI: 1.06, 1.70] times higher odds of anemia as compared to their counterparts (Table 3).
Discussion
Anemia in lactating mother is a neglected public health problem which has its impact for both the mother and the newborn [12]. Thus, we investigated the prevalence and determinants of anemia among lactating women in Ethiopia.
In this study, the prevalence of anemia among lactating mothers was 28.3% and this was in line with a study done in India [32] and Ethiopia [14]. The prevalence of anemia in lactating mothers found in this study was lower than studies conducted in China, India, Vietnam, and Myanmar [9,10,11,12]. This might be because mothers near to and after giving birth are granted sufficient maternity leave according to the social and cultural norms in Ethiopia, which also allows them to get adequate rest. Also, in Ethiopia, lactating mothers are allowed to eat a range of foods like animal products, even during the fasting period. It may also be because Teff Injera (which has a higher iron content) is the staple Ethiopian food eaten by the majority of the country’s population [33].
However, the current finding is higher than a previous study in Ethiopia using EDHS 2011 data [15]. This might be attributed to increased coffee, tea, and red wine consumption (both alcoholic and non-alcoholic) from time to time, which decreases iron absorption and induces anemia [34, 35]. This high prevalence of anemia in lactating mothers can result various adverse consequences both for the mother and the child mostly due to its impact in the immune system; such as maternal death, clogged milk ducts, mastitis, thrush, and diminished quality or volume of the milk [19].
Consistent with a study in Ethiopia based on EDHS 2011 [15], we found that lactating mothers who had been working within the 12 months preceding the survey had lower odds of having anemia. This might be because mothers who were working can have a good income and buy the necessary and variety of foods including iron-containing foods [36]. The other plausible explanation is that mothers who worked would have a great deal of trust and decision-making ability to have sufficient feeding practice.
Similarly, mothers who were from poorer, middle, rich, and richest households had lower odds of having anemia as compared to those from poorest households. This finding is supported by studies in Nepal [24], Myanmar [11], Rwanda [23], and Ethiopia [15]. This might be because mothers from rich households had a great opportunity to have a balanced diet in terms of meal frequency and variety of food [37].
This study also indicated that mothers who had supplemented with iron during their last pregnancy had lower odds of having anemia as compared to their counterparts. This is supported by a study in Bahir Dar-Ethiopia [38], which showed that iron supplementation during pregnancy is negatively associated with having anemia both for pregnant and lactating women. The possible explanation could be, iron is the most important nutrient which is used for the formation of red blood cells and when it was taken during pregnancy it can have a probability of preventing anemia during the locational period as well.
Consistent with a study done in Nepal [24] and Ethiopia [21], which indicated being male household head lower the chances of the mothers to be anemic, in our study households who had female head had higher odds of anemia as compared with those households whose head was male. This may be due to the fact that awareness towards anemia and treatment-seeking behaviors for any health problems might be lower in female-headed households [21]. This study also revealed that lactating mothers who were taking modern contraceptives had a lower risk of having anemia. This is congruent with studies done in low and middle-income countries [22], sub-Saharan Africa [39], Rwanda [23], and Ethiopia [15]. This is because taking contraceptives could potentially minimize the monthly (menstrual) bleeding [40, 41]. Moreover, by reducing a woman’s likelihood of becoming pregnant, oral contraceptives may also reduce the risk of anemia from antepartum or postpartum hemorrhage.
The number of births a woman had with 5 years is another factor associated with anemia among lactating mothers which revealed that mothers who had two and three to four children within 5 years had higher odds of having anemia. This finding is supported by a study in Ethiopia [42] which showed having too frequent birth is among a significant predictor of anemia. This is since too many births in a short period (within 5 years) might not give enough time to replenish or substitute lost nutrient stores before another reproductive cycle starts and result in iron deficiency anemia [43]. Besides, mothers with frequent birth might have both antepartum and postpartum hemorrhage with consecutive births, which in turn result in chronic and repeated anemia.
Moreover, in our study higher community illiteracy level was another important factor which was associated with higher odds of having anemia in lactating mother. Another study also revealed that maternal health service utilization is associated with literacy level in the community in which mothers from communities with higher illiteracy level had higher odds of utilizing maternal health services [44]. The possible reason for the association of women illiteracy level with anemia in lactating mothers might be lower education level decreases communication within the family particularly with the husband on health-related issues. In addition, illiteracy prevents women from developing the confidence to make decisions regarding their health and seek out quality health services [45, 46]. In remote societies, higher proportions of illiterate females also indicate lower autonomy which in turn results in restriction from accessing important maternal health care services during pregnancy, childbirth, and the postpartum period which finally end up with comorbidities like anemia.
This study had both limitations and strengths. Among limitations, some important variables which are known to cause anemia such as helminthic infection and protozoan infections like malaria were not assessed. In addition, due to the cross-sectional nature of the data, it is difficult to show a cause and effect relationship between independent and dependent variables. The main strength of this study was the use of nationally representative data with a large sample size, based on laboratory-confirmed anemia, which makes the findings of the study more representative to all lactating mothers in Ethiopia. The other strength is since it is based on the national survey it has the potential to give an insight for policy-makers and program planners to design intervention strategies at the individual and community level.
Conclusion
In this study the prevalence of anemia among lactating mothers was high. Both individual and community level factors were associated with anemia among lactating mothers. Mothers from rich households, those who had been working in the 12 months preceding the survey, current modern contraceptive users, those mothers who had been taking iron during the last pregnancy, having more than one number of births within 5 years had lower odds of having anemia. While being mothers from households with female household heads and being from communities with higher proportions of illiterate women increases the odds of having anemia. Therefore, focusing on family planning services especially on modern contraceptive methods, iron supplementation during every pregnancy, child spacing, and improving community literacy could decrease anemia during lactation.
Availability of data and materials
All relevant data are available within the manuscript.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- BMI:
-
Body Mass Index
- EAs:
-
Enumeration Areas
- EDHS:
-
Ethiopia Demographic and Health Survey
- MOR:
-
Median Odds Ratio
- PCV:
-
Proportional Change in Variance
- SNNPR:
-
Southern Nation Nationality and People Region
- ICC:
-
Intraclass Correlation Coefficient
- WHO:
-
World Health Organization
References
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity: World Health Organization; 2011..
Organization WH. Assessing the iron status of populations: report of a joint World Health Organization/Centers for Disease Control and Prevention technical consultation on the assessment of iron status at the population level. Geneva: World Health Organization; 2007.
World Health Organization. Worldwide prevalence of anaemia 1993–2005: WHO global database on anaemia..
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1(1):e16–25.
Bodnar LM, Scanlon KS, Freedman DS, Siega-Riz AM, Cogswell ME. High prevalence of postpartum anemia among low-income women in the United States. Am J Obstet Gynecol. 2001;185(2):438–43.
Whitney ERS. In: Adams P, editor. Understanding Nutrition. 11th ed. USA: Thomson Learning Academic Resource Center; 2008.
Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr. 2000;72(1):257S–64S.
Ettyang GA, van Marken Lichtenbelt WD, Oloo A, Saris WH. Serum retinol, iron status and body composition of lactating women in Nandi, Kenya. Ann Nutr Metab. 2003;47(6):276–83.
Siddiqui MZ, Goli S, Reja T, Doshi R, Chakravorty S, Tiwari C, et al. Prevalence of anemia and its determinants among pregnant, lactating, and nonpregnant nonlactating women in India. SAGE Open. 2017;7(3):2158244017725555.
Trinh LTT, Dibley M. Anaemia in pregnant, postpartum and non pregnant women in Lak district, Daklak province of Vietnam. Asia Pacific J Clin Nutr. 2007;16(2):310–5.
Zhao A, Zhang Y, Li B, Wang P, Li J, Xue Y, et al. Prevalence of anemia and its risk factors among lactating mothers in Myanmar. Am J Trop Med Hygiene. 2014;90(5):963–7.
Zhao A, Zhang J, Wu W, Wang P, Zhang Y. Postpartum anemia is a neglected public health issue in China: a cross-sectional study. Asia Pac J Clin Nutr. 2019;28(4):793.
Roba KT, O’Connor TP, Belachew T, O’Brien NM. Serum zinc, iron and urinary iodine levels and their relationship to other indices of malnutrition among lactating mothers in two agro-ecological zones of rural Ethiopia. J Nutr Health Sci. 2016;3(2):202.
Alemayehu M. Factors associated with Anemia among lactating mothers in subsistence farming households from selected districts of Jimma zone, South Western Ethiopia: a community based cross-sectional study. J Nutr Food Sci. 2017;7(595):2.
Lakew Y, Biadgilign S, Haile D. Anaemia prevalence and associated factors among lactating mothers in Ethiopia: evidence from the 2005 and 2011 demographic and health surveys. BMJ Open. 2015;5(4):e006001.
Gibbs RS. Clinical risk factors for puerperal infection. Obstet Gynecol. 1980;55(5 Suppl):178S–84S.
Henly SJ, Anderson CM, Avery MD, Hills-Bonuyk SG, Potter S, Duckett LJ. Anemia and insufficient milk in first-time mothers. Birth. 1995 Jun;22(2):87–92.
Beard JL, Hendricks MK, Perez EM, Murray-Kolb LE, Berg A, Vernon-Feagans L, Irlam J, Isaacs W, Sive A, Tomlinson M. Maternal iron deficiency anemia affects postpartum emotions and cognition. J Nutr. 2005 Feb 1;135(2):267–72.
Harding S. Breast-feeding & an anemic mother; 2017.
Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123(5):615–24.
Ali JH. Gender differences in household headship and level of awareness on anaemia among Ethiopian women: Evidences from a nationwide cross-sectional survey. Ethiopian J Health Dev. 2018;32(2)..
Bellizzi S, Ali MM. Effect of oral contraception on anemia in 12 low-and middle-income countries. Contraception. 2018;97(3):236–42.
Habyarimana F, Zewotir T, Ramroop S. Spatial Distribution and Analysis of Risk Factors Associated with Anemia Among Women of Reproductive Age: Case of 2014 Rwanda demographic and health survey data. Open Public Health J. 2018;11(1).
Nisar R, Anwar S, Nisar S. Food security as determinant of anemia at household level in Nepal. J Food Sec. 2013;1(2):27–9.
Gebremedhin S, Enquselassie F. Correlates of anemia among women of reproductive age in Ethiopia: evidence from Ethiopian DHS 2005. Ethiop J Health Dev. 2011;25(1):22–30.
Targets WGN. 2025: anaemia policy brief. Geneva: World Health Organization; 2014.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Rockville: CSA and ICF; 2016.
Croft TN, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S. Guide to DHS statistics. ICF: Rockville; 2018.
Goldstein H, Browne W, Rasbash J. Partitioning variation in multilevel models. Underst Stat. 2002;1(4):223–31.
Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59(6):443–9.
Merlo J, Yang M, Chaix B, Lynch J, Råstam L. A brief conceptual tutorial on multilevel analysis in social epidemiology: investigating contextual phenomena in different groups of people. J Epidemiol Community Health. 2005;59(9):729–36.
Bhagwan D, Kumar A, Rao CR, Kamath A. Prevalence of anaemia among postnatal mothers in coastal Karnataka. J Clin Diagn Res. 2016;10(1):LC17.
Baye K. Teff: nutrient composition and health benefits. Intl Food Policy Res Inst; 2014.
Kumera G, Haile K, Abebe N, Marie T, Eshete T. Anemia and its association with coffee consumption and hookworm infection among pregnant women attending antenatal care at Debre Markos Referral Hospital, Northwest Ethiopia. PloS one. 2018;13(11):e0206880.
Obse N, Mossie A, Gobena T. Magnitude of anemia and associated risk factors among pregnant women attending antenatal care in Shalla Woreda, west Arsi zone, Oromia region, Ethiopia. Ethiop J Health Sci. 2013;23(2):165–73.
Taruvinga A, Muchenje V, Mushunje A. Determinants of rural household dietary diversity: the case of Amatole and Nyandeni districts, South Africa. Int J Dev Sustainability. 2013;2(4):2233–47.
Doan D. Does income growth improve diet diversity in China? 2014.
Feleke BE, Feleke TE. Pregnant mothers are more anemic than lactating mothers, a comparative cross-sectional study, Bahir Dar, Ethiopia. BMC Hematol. 2018;18(1):2.
Gebremedhin S, Asefa A. Association between type of contraceptive use and haemoglobin status among women of reproductive age in 24 sub-Saharan Africa countries. BMJ Sex Reprod Health. 2019;45(1):54–60.
Glasier AF, Smith KB, Van der Spuy ZM, Ho PC, Cheng L, Dada K, Wellings K, Baird DT. Amenorrhea associated with contraception—an international study on acceptability. Contraception. 2003;67(1):1–8.
Miller L, Hughes JP. Continuous combination oral contraceptive pills to eliminate withdrawal bleeding: a randomized trial. Obstet Gynecol. 2003;101(4):653–61.
Alemu T, Umeta M. Reproductive and obstetric factors are key predictors of maternal anemia during pregnancy in Ethiopia: evidence from demographic and health survey (2011). Anemia. 2015;2015:649815.
Merchant K, Martorell R. Frequent reproductive cycling: does it lead to nutritional depletion of mothers? Progress Food Nutr Sci. 1988;12(4):339–69.
Singh PK, Kumar C, Rai RK, Singh L. Factors associated with maternal healthcare services utilization in nine high focus states in India: a multilevel analysis based on 14 385 communities in 292 districts. Health Policy Plan. 2014;29(5):542–59.
Lam Y, Broaddus ET, Surkan PJ. Literacy and healthcare-seeking among women with low educational attainment: analysis of cross-sectional data from the 2011 Nepal demographic and health survey. Int J Equity Health. 2013;12(1):95.
Woldemicael G, Tenkorang EY. Women’s autonomy and maternal health-seeking behavior in Ethiopia. Matern Child Health J. 2010;14(6):988–98.
Acknowledgments
The authors would like to thank measure DHS for their permission to access the EDHS datasets.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
AML and ABT involved in the design and conception of the study, data analysis, interpretation and write up of the manuscript. Both the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was approved by an Institutional Review Committee of the Institute of Public Health, College of Medicine and Health Sciences, University of Gondar. The approval letter for the use of the EDHS data set was also gained from the Measure DHS program. No personal identifiers were in the data set and this data set was not disclosed to any third person.
Consent for publication
Not applicable.
Competing interests
Both authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liyew, A.M., Teshale, A.B. Individual and community level factors associated with anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health survey, 2016; a multilevel analysis. BMC Public Health 20, 775 (2020). https://doi.org/10.1186/s12889-020-08934-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-020-08934-9