Abstract
Background
Because of the high under-five mortality rate, the government in Zambia has adopted the World Health Organization (WHO) policy on child delivery which insists on professional maternal care. However, there are scholars who criticize this policy by arguing that although built on good intentions, the policy to ban traditional birth attendants (TBAs) is out of touch with local reality in Zambia. There is lack of evidence to legitimize either of the two positions, nor how the outcome differs between women with HIV and those without HIV. Thus, the aim of this paper is to investigate the effect of using professional maternal care or TBA care by mothers (during antenatal, delivery, and postnatal) on under-five mortality of their children. We also compare these outcomes between HIV-positive and HIV-negative women.
Methods
By relying on data from the 2013–2014 Zambia Demographic Health Survey (ZDHS), we carried out propensity score matching (PSM) to investigate the effect of utilization of professional care or TBA during antenatal, childbirth, and postnatal on under-five mortality. This method allows us to estimate the average treatment effect on the treated (ATT).
Results
Our results show that the use of professional care as opposed to TBAs in all three stages of maternal care increases the probability of children surviving beyond 5 years old. Specifically for women with HIV, professional care usage during antenatal, at birth, and during postnatal periods increases probability of survival by 0.07 percentage points (p.p), 0.71 p.p, and 0.87 p.p respectively. Similarly, for HIV-negative women, professional care usage during antenatal, at birth, and during postnatal periods increases probability of survival by 0.71 p.p, 0.52 p.p, and 0.37 p.p respectively. However, although there is a positive impact when mothers choose professional care over TBAs, the differences at all three points of maternal care are small.
Conclusion
Given our findings, showing small differences in under-five child’s mortality between utilizers of professional care and utilizers of TBAs, it may be questioned whether the government’s intention of completely excluding TBAs (who despite being outlawed are still being used) without replacement by good quality professional care is the right decision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Following the western-influenced evidence-based biomedical approach and the World Health Organization (WHO) policy on child delivery which insists on skilled delivery, most countries in Sub-Saharan Africa (SSA) have moved to exclude traditional birth attendants (TBAs) in preference for institutional care [1]. Nowhere else is this more evident than in Zambia where TBAs were officially excluded from the line of care in 2010 [2,3,4].
Proponents of institutional care argue that opportunistic infections such as malaria, tuberculosis, and delicate complications that mothers face during antenatal, child birth, and postnatal periods require the attention of trained personnel, especially for women with HIV. This is in order to ensure better management of postpartum hemorrhage, pre-eclampsia, and neonatal sepsis including prevention of mother to child transmission (PMTCT) [4, 5]. Scholars from this school of thought argue that the low utilization of skilled attendants in Zambia has led to unacceptably high maternal, neonatal, infant, and under-five mortality [6,7,8,9]. This is worsened by high HIV rates among women of reproductive age (15–49 years old) which currently stands at 16.1% in Zambia [6]. Evidence from Zambia indicates that children born from women with HIV are more likely to die before reaching the age of 5 than those born from HIV-negative mothers [7, 10, 11]. As an antidote to this predicament, proponents of institutional care have been calling for mandatory skilled attendance during antenatal, childbirth, and postnatal periods especially for women with HIV [12]. This is in order to ensure consistent uptake of antiretroviral treatment and any necessary surgical procedures to reduce the child’s chances of dying before reaching age five.
There are however other scholars who criticize the Zambian government’s policy on TBAs by suggesting that although built on good intentions, the policy to exclude TBAs is out of touch with reality in Zambia and contributes to high maternal, neonatal, infant, and under-five mortality rates in the country [2, 3, 13, 14]. Excluding TBAs who in most cases are the only feasible source of maternity care in preference for ideally better trained but unavailable professionals is counterproductive [2]. These scholars intimate that the Zambian health system is too weak to sustain the government’s policy of strict institutional care. For example, Lukonga and Michelo [12] posit that Zambia has poorly equipped and overcrowded health institutions which lack sufficient numbers of technically skilled personnel. This makes professional care ideal but not practical. A combination of all these shortcomings compromises the care for pregnant women, and subsequently the survival of their children beyond the age of 5 [11]. This is why despite the government directive to exclude TBAs in preference for professional care, many women in Zambia have continued to utilize TBAs [2, 15].
Further, despite the forgoing two conflicting positions, there is a lack of evidence to legitimize either of the two positions [12, 16]. It is not yet known whether in the Zambian case, utilization of skilled professionals as opposed to TBAs during antenatal, childbirth, and postnatal periods significantly reduces under-five mortality [13]. It is also not yet known if on the basis of type of care, the resulting under-five mortality outcomes are similar for women with HIV and those who are HIV negative. There are no studies that specifically focus on comparing the differences in outcomes on the basis of utilizing skilled care or TBAs during the continuum of maternal care for women with HIV and those without HIV [5, 13, 17].
The expectation however is that in both HIV-negative women and women with HIV, skilled care along the continuum of maternal care would reduce the chances of under-five mortality [18]. It is expected that the impact will be higher for women with HIV [18]. This is because skilled care allows women with HIV (who are more vulnerable) to access life-saving antiretroviral treatment, cesarean birth, and continuation of antiretroviral treatment which promote PMTCT and ultimately reduce under-five mortality [19]. However, the extent to which this is evident in Zambia is still unclear [20]. It is vital to provide evidence on the causal nature of this relationship and clearly demonstrate how in the context of Zambia, utilization of skilled attendants affects under-five mortality for women with HIV and how this differs for HIV-negative women. This delineation will serve as a first step towards the formulation of context-specific and effective policy to reduce under-five mortality in Zambia [16]. Thus, the aim of this paper is to investigate and compare the effect of utilization of professional maternal care (or TBA care) during antenatal, delivery, and postnatal periods on under-five mortality in women with HIV and in HIV-negative women.
Methods
Data
We used the 2013–2014 Zambia Demographic Health Survey (ZDHS). The ZDHS included data demographic and health indicators for women who were aged between 15 and 49 years during the survey. Regarding HIV test results, the HIV data were obtained by collecting blood samples during interviews from consenting participants which were later tested for HIV. The HIV data were however not publicly available. The data were only availed to us after obtaining ethical clearance from the Zambia ethics board, the Ministry of Health of Zambia, and the ZDHS team. This was followed by signing a confidentiality form to treat the data with strict confidentiality. We then linked the HIV data to the rest of the ZDHS data based on unique IDs as instructed and recommended by the ZDHS team.
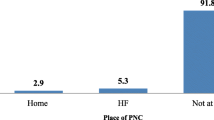
From the main ZDHS dataset on all women (aged 15 to 49), we selected a sub-sample of women who had stated that they had given birth at least once in the last 5 years preceding the survey and who consented to having an HIV test. If the respondents did not consent to testing using their sample, their HIV statuses were left unstated in the data and treated as missing [6]. The final sample and the associated data are shown in Table 1. These data enabled us to investigate the effect of utilizing professional maternal care (or TBAs) during antenatal, childbirth, and postnatal periods on under-five mortality of children for both women with HIV and those without HIV.
Estimation
Propensity score matching (PMS) was applied to investigate the effect of utilizing professional care or TBA during antenatal, childbirth, and postnatal periods on under-five mortality. This method allows us to calculate the average treatment effect on the treated (ATT). We do this at three different stages (antenatal, childbirth, and postnatal) for both women with HIV and HIV-negative women giving us six different PSM investigations.
More specifically, we investigated (a) the effect of utilizing either professional care or TBAs during antenatal among women with HIV (and those without HIV) on under-five mortality, (b) the effect of utilizing either professional care or TBAs during childbirth among women with HIV (and those without HIV) on under-five mortality, and (c) the effect of utilizing either professional care or TBAs during postnatal among women with HIV (and those without HIV) on under-five mortality.
The propensity score was estimated using a probit regression with the following confounders: age at the most recent birth of the woman, total number of children, mother’s level of education, mother’s employment status, household wealth, whether the woman resides in an urban or rural area, religion, ethnicity, distance to nearest health facility, and access to health insurance. The selection of variables was guided by theory and consensus in extant empirical literature regarding what factors are likely to influence women to access professional care [21, 22].
We generated the propensity scores by using STATA. This means we used PSM to enable us to statistically create a control group (women with HIV/HIV-negative women who utilize TBAs) by matching the observed characteristics of the treated participants (women with HIV/HIV-negative women who utilize skilled attendants) to the control group. This is done on the basis of similar values of the propensity score [23]. Heckman et al. [24] defined PSM as the probability of selection into the treated group, which in this case means the probability of utilizing professional care. It is also important to note that the “unbiased inference” which arises from propensity score matching is based on the assumption that the potential outcomes are independent of treatment assignment conditional on observable characteristics [25]. Another important condition is that there must exist a “common-support” region in the propensity score distributions comprising of participants from both the treatment and control groups [25].
To estimate the ATT, we used the nearest neighbor matching technique. The nearest neighbor matching method works by matching individuals in the control to the treated group and then discards individuals who are not selected as matches [23]. By using this technique, the individual from the comparison group is selected which then acts as a matching partner for the closest treated partner in terms of the propensity score [26, 27]. We make use of the 1:1 nearest neighbor matching technique which works by selecting for each individual in the treated group, the closest individual (in terms of propensity score) from the control group. The disadvantage of 1:1 nearest neighbor matching technique is that it discards a large number of observations which may reduce statistical power [28]. This is however not a concern for our study since we have enough observations in our sample to identify statistically significant effects.
The reliability of the estimated effect of either utilizing professional care or TBAs on under-five mortality when using PSM depends on selection of observables [25]. We thus checked to ensure that the common support assumption was satisfied. This was done by inspecting the propensity score distribution [29]. For the balancing test, several iterations of estimation of the propensity score were carried out in which variables were recoded to have satisfied the balancing property [30].
For robustness, we compare our ATT results obtained from the nearest neighbor matching method with two other matching techniques (see Appendix) to ensure that our findings are consistent, namely Kernel matching and stratification matching [26]. The Kernel matching uses weighted average of the individuals in the control group to construct a counterfactual [25] whereas stratification matching works by partitioning the common support into different strata and after which impact is computed in each of those two strata [26].
Hidden bias and sensitivity test
The weakness with PSM is that it does not correct for bias due to unobserved characteristics. In order to overcome this bias, conducting sensitivity analysis of hidden bias is recommended. This is achieved by establishing the level of unobserved heterogeneity that would change the statistical significance of the treatment effects (ATT) [25]. Therefore, we adopt the technique proposed by Altonji et al. [31] to estimate how sensitive the estimates are to selection on unobservables. This technique links selection on observed factors to selection on unobserved factors. For this, we estimate a bivariate probit model and impose constraints on the correlation between unobserved factors that influence, on the one hand, the probability of being in the treatment group and, on the other, the outcome.
Results
By relying on PSM, we investigated the effect of utilizing professional care (or TBA care) by mothers during antenatal, delivery, and postnatal periods on under-five mortality of children. This was done for mothers with HIV and those without HIV. As recommended [26], the three steps of propensity score matching estimation were followed. Firstly, we ran probit models for the three stages of maternal care (antenatal, birth, and postnatal) in order to estimate the propensity score. After this, the estimated propensity scores were used to match a group of individuals who utilized professional care but were comparable to those that utilized TBAs in terms of propensity scores generated in the first step. The final step was to compare the under-five child’s mortality outcomes of professional care and TBA-utilizers between women with HIV and HIV-negative women at the three different stages of maternal care, a process which enables us to estimate the ATT effects.
By checking the ATT result column in Table 2, we can see the effect of the mothers’ choice of care (between professional and TBA care) on the survival of their children beyond 5 years.
In general, the results in Table 2 show that utilizing professional care (as opposed to TBAs) in all three stages of maternal care for both women with HIV and those without HIV slightly increases the probability of their children surviving beyond 5 years old.
For the specific stages in women with HIV, uptake of professional antenatal care (as opposed to TBAs) by women with HIV increased the probability of the child surviving beyond age five by 0.07 percentage points (p.p) representing a survival rate of 97.1% for professional care utilizers and 97.0% for TBA utilizers. Similarly, the uptake of professional care during childbirth (as opposed to TBAs) by women with HIV increased the probability of the child surviving beyond age five by 0.71 p.p, representing a survival rate of 97.2% for professional care users and 96.5% for TBA users. At postnatal, the probability increases by 0.87 p.p. representing a survival rate of 97.7% for professional care utilizers and 96.8% for TBA-utilizers.
Similarly, for HIV-negative women, uptake of professional care (as opposed to TBAs) during antenatal, at birth, and postnatal period slightly increased the probability of the child surviving beyond age 5. For example, the probability of a child surviving beyond age increased by 0.71 p.p as a result of using professional care. This represents a survival rate of 97.8% for professional care utilizers and 97.1% for TBA utilizers. At birth, the uptake of professional care for HIV-negative women increased the probability of the child surviving beyond age 5 by 0.52 p.p representing a survival rate of 97.5% for professional care utilizers and 97.0% for TBA utilizers. During postnatal, it increased by 0.37p.p representing a survival rate of 97.6% for professional care utilizers and 97.2% for TBA utilizers.
Robustness checks for the ATT were done by the use of two alternative matching techniques, namely, Kernel matching and stratification matching (see Appendices 1 and 2). Both of the matching techniques produced similar ATT results in direction and magnitude for all the three stages. We further carried out the Altonji test to see if there was any bias resulting from the effect of unobservables. The Altonji sensitivity test indicates that our results are robust to selection on unobservables (see Appendix 3).
Discussion
The aim of this paper was to investigate the effect of utilization of professional maternal care or TBA care during antenatal, delivery, and postnatal period on under-five mortality for women with HIV and those who are HIV negative.
Our findings highlight the fact that, in general, children born from mothers who utilize professional care (as opposed to TBAs) have a slightly higher probability of surviving beyond the age of 5 regardless of the HIV status of the mother. However, despite these positive results in support of professional care, the differences, although statistically significant, are small in magnitude. From the forgoing, we make the following two conclusions: (a) for both HIV-negative women and those living with HIV, professional care at all the three stages of care leads to slightly higher probability of their children surviving beyond age 5; (b) although professional care appears to produce comparatively higher survival rates, the difference between those who utilize professional care and those who utilize TBAs is relatively small.
The slightly lower probability of under-five mortality resulting from professional care stands out as the most important finding of this paper, especially considering the fact that in the recent past, there has been an increased focus on the need to promote professional care during antenatal, at birth, and postnatal period, from the Zambian government and the WHO [15, 32]. Other studies have emphasized the importance of professional care as a means of reducing under-five mortality [5, 19]. In this regard, professional care is credited for helping to mitigate pregnancy-related complications, particularly pre-eclampsia, and also specifically for mothers with HIV, it helps in the promotion of PMTCT [33]. These studies have also demonstrated that professional care at all three stages is a practical platform through which any potential complications arising during birth can be effectively handled. This is especially important for women with HIV where ART and periodic monitoring by professionals can help in the promotion of PMTCT. This is why, according to Lincetto et al. [33], the WHO [32] and subsequently the government of Zambia disapproves of TBAs in preference for professional caregivers with the anticipation that professional caregivers could significantly reduce the probability of dying before age five [33].
However, our findings indicate that in both women with HIV and those without HIV, professional maternal care led to a slightly higher probability of surviving beyond age 5.
The WHO’s notion of change that anchored on the assumption that professional care automatically and significantly leads to high reduction in under-five mortality has been challenged [34]. Some scholars have observed that the increased utilization of professional antenatal care has not significantly reduced under-five mortality in Zambia regardless of HIV status. This could, as other scholars have shown, be the result of poor standards of care under professional care in Zambia epitomized by inadequate medical supplies, equipment, and staff [11, 34]. We have shown that in the case of Zambia, there is a small difference in under-five mortality between professional care utilizers and TBA-utilizers for both HIV negative and women living with HIV. That notwithstanding, it seems legitimate to assume that when these results are combined with maternal mortality outcomes (which we did not investigate in this study), the effects of professional care utilization may even be greater. It was also evident that the effect of professional care does not differ much between HIV-negative women and those living with HIV.
Given these findings, important questions worth asking are (a) how good is the quality of professional care in Zambia? (b) and, similarly, how good is the care under TBAs?
Although professional care produces slightly better outcomes than TBAs, there is a lack of adequate health personnel in Zambia [4, 8, 35]. This observation is in line with what other studies from Zambia [1, 4, 36] have continued to highlight, which is that most professional maternal care stations in Zambia are crippled with a shortage of qualified medical personnel and medical equipment, shortage of life-saving antiretroviral drugs, overcrowding, and poor infrastructure especially in rural parts of Zambia [1, 2, 10, 36]. Further, whereas it appears logical to recommend improvement in the availability and quality of care in Zambia, such recommendations are frequently not achievable due to the high costs involved in implementing them. The government in Zambia has been reluctant and to some extent financially incapable of implementing these ideal, yet costly recommendations [10]. Given the small differences between professional care and TBAs in terms of probability of under-five mortality in our results, it seems legitimate to explore ways through which TBAs can be better involved to complement the weak health system in Zambia. Elsewhere within Sub-Saharan Africa, it has been demonstrated that training and incorporating TBAs in the line of care increases the availability of care and may improve maternal outcomes [37]. Similarly, another study in neighboring Malawi has shown that banning TBAs does not lead to a reduction in maternal mortality [38]. Thus, the decision to exclude TBAs in the line of care in Zambia without good quality professional care being available to replace it seems counterproductive especially considering that they are still being relied upon (albeit illegally) amidst an inefficient health system. In a country like Zambia, which is experiencing a critical shortage of professional health workers, relying on already established traditional and indigenous solutions such as TBAs may be necessary and useful. TBAs may also be trained, regulated, and given suitable functions within the line of maternal care. This might help complement professional attendants (who are in most cases inadequate or unavailable).
Limitations
A dominant limitation in this paper, like in many other studies that rely on household surveys, is the problem of recall bias. The quality of the survey normally depends on the respondent’s ability to accurately recall events, which in some cases is very difficult to assure, and to deal with. We believe the probability of recalling such events is similar in the treatment group (i.e., utilizing professional care) and the control group (i.e., utilizing TBAs) and therefore PSM partly accounts for possible bias. Secondly, some women who did not consent to have their HIV status determined were excluded from the sample which might have affected the representativeness of the sample and hence external validity of the findings. Further, the HIV-positive population could have been underrepresented in the sample due to the fact that people who already know their HIV-positive status could have been less willing to participate in the study, which represents the so-called selection bias. Similarly, we also note that given the fact that TBAs are outlawed in Zambia, respondents are more inclined not to report usage of TBAs. These two biases are however difficult to address in the absence of quasi-experimental variation in the data [39]. That notwithstanding, our findings provide useful insights in understanding the impact of professional care on under-five mortality. Therefore, more studies must be undertaken in this area of research, preferably by addressing the stated above limitations, in order to substantiate the internal validity and the generalizability of our findings.
Conclusion
In this paper, we have demonstrated that in general, children born to mothers who utilize professional care have a slightly higher probability of surviving beyond the age of 5, regardless of the HIV status of the mother. However, although there is a positive impact when mothers choose professional care over TBAs, the difference at all the three points of maternal care is small (although it is possible that when this is combined with maternal mortality outcomes, the effects of professional care utilization may even be greater).
Given our findings, showing small differences in under-five child’s mortality between utilizers of professional care and utilizers of TBAs, it may be questioned whether the government’s intention of completely excluding TBAs (who despite being outlawed are still being used) without replacement by good quality professional care is the right decision. The idea of completely excluding TBAs in the line of care in Zambia may be counterproductive in a health system that lacks personnel and equipment and is highly inaccessible to the majority of the rural population. The current policy in Zambia might benefit from further investigation of professionalization of TBA’s.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- ART:
-
Antiretroviral treatment
- HIV:
-
Human immunodeficiency virus
- PMTCT:
-
Prevention of mother to child transmission
- SSA:
-
Sub-Saharan Africa
- TBA:
-
Traditional birth attendants
- WHO:
-
World Health Organization
References
Sialubanje C, Massar K, Hamer DH, Ruiter RA. Reasons for home delivery and use of traditional birth attendants in rural Zambia: a qualitative study. BMC J Preg Childb. 2015;15(26)
Stekelenburg J, Kyanamina S, Mukelabai M, Wolffers I, van Roosmalen J. Waiting too long: low use of maternal health services in Kalabo, Zambia. Tropical Med Int Health. 2004;9:390–8.
Sialubanje C, Massar K, Hamer DH, Ruiter RA. Reasons for home delivery and use of traditional birth attendants in rural Zambia: a qualitative study. BMC Preg Childb. 2015;15(216)
Cheelo C, Nzala S, Zulu JM. Banning traditional birth attendants from conducting deliveries: experiences and effects of the ban in a rural district of Kazungula in Zambia. BMC Preg Childb. 2016;16(323)
Chi BH, Bolton-Moore MC, Holmes CB. Prevention of mother-to-child HIV transmission within the continuum of maternal, newborn, and child health services. Curr Opin HIV AIDS. 2013;8(5):498–503.
ZDHS. Zambia demographic and health survey. Lusaka: ZDS/CSO; 2014.
Vallely L, Ahmed Y, Murray SF. Postpartum maternal morbidity requiring hospital admission in Lusaka, Zambia—a descriptive study. BMC Preg Childb. 2005;5(1)
Banda PC. Status of maternal mortality in Zambia: use of routine data. Afr Popul Stud. 2015;29(2)
Catling C, Medley N, Foureur M, Ryan C, Leap NTAH. Group versus conventional antenatal care for pregnant women. Cochrane. 2015;2
Gartland MG, Chintu NT, Li MS, Lembalemba MK, Mulenga SN, Bweupe M, Musonda P, Stringer EM. Field effectiveness of combination antiretroviral prophylaxis for the prevention of mother-to-child HIV transmission in rural Zambia. AIDS. 2013;27(8)
Gill CJ. Effect of training traditional birth attendants on neonatal mortality (Lufwanyama Neonatal Survival Project): randomised controlled study. BMJ Glob Health J. 2011;342(346).
Lukonga E, Michelo C. Factors associated with neonatal mortality in the general population: evidence from the 2007 Zambia Demographic and Health Survey (ZDHS); a cross sectional study. Pan Afr Med J. 2064:2015.
Kendall T, Dane I, Cooper D, Dilmitis S, Kaida A. Eliminating preventable HIV-related maternal mortality in sub-Saharan Africa: what do we need to know? J Acq Immune Deficiency Syndrome. 2014;1(64):250–8.
Green-top-Guideline-No-39. Management of HIV in pregnancy. London: Royal College of Obstetricians and Gynaecologists; 2010.
Bolu O, Anand A, Swartzendruber A, Hladik W, Marum L, Sheikh A. Utility of antenatal HIV surveillance data to evaluate prevention of mother-to-child HIV transmission programs in resource-limited settings. Am J Obstetr Gynecol. 2007;197:17–25.
Kendall T, Langer A. Critical maternal health knowledge gaps in low- and middle-income countries for the post-2015 era. Reprod Health. 2015;12(55):1–4.
Kuhn L, Aldrovandi GM, Sinkala M, Kankasa C, Mwiya M, Thea DM. Potential impact of new World Health Organization criteria for antiretroviral treatment for prevention of mother-to-child HIV transmission. AIDS. 2010;24(9):1374–7.
WHO. Child health and development. Geneva: WHO; 2015.
Avert. Prevention of mother-to-child transmission (Pmtct) of HIV. London: Avert; 2016.
Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Preg Childb. 2014;14(161)
Andersen R. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10.
Ansari Z, Carson N, Ackland M, Vaughan L, Serraglio A. A public health model of the social determinants of health. J Prev Med. 2003;48(4):242–51.
Rosenbaum P. Observational studies. New York: Springer; 2002.
Heckman JJ, Ichimura H, Todd P. Matching as an Econometric Evaluation Estimator. Rev Econ Stud. 1998;65(2):261–94
Caliendo M, Bonn I, Kopeinig S. Some practical guidance on how to implement propensity score matching. Köln: University of Cologne; 2008.
S. R. Khanker, G. B. Koowal and H. A. Samad, Handbook on impact evaluation: quantitative methods, world bank, 2010.
DiPrete T, Gangl M. Assessing bias in the estimation of causal effects: Rosenbaum bounds on matching estimators and instrumental variables estimation with imperfect instruments. Sociol Methodol. 2004;34(1):271–310.
Huber M, Lechner M, Steinmayr A. RADIUSMATCH: Stata module to perform distance-weighted radius matching with bias adjustment. Boston: ideas; 2012.
Rosenbaum P, Rubin D. The central role of the propensity score in observational. Biometrika. 1983;70(1):41–5.
Garrido MM, Kelley AS, Paris J, Roza K, Meier DE, Morrison RS. Methods for constructing and assessing propensity scores. Health Serv Res. 2014;49(5):1701–20.
Altonji JG, Elder TE, Taber CR. Selection on Observed and Unobserved Variables: Assessing the Effectiveness of Catholic Schools. J Polit Econ. 2005;113(1)
WHO. World health statistics 2013. Geneva: WHO; 2013.
Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Antenatal care. Geneva: WHO; 2010.
Kyei NNA, Chansa C, Gabrysch S. Quality of antenatal care in Zambia: a national assessment. BMC Preg Childb. 2012;12(151).
Graham W, Varghese B. Quality, quality, quality: gaps in the continuum of care. Lancet. 2012;379:5–6.
van den Broek N, Graham W. Quality of care for maternal and newborn health: the neglected agenda. BJOG Int J Obstet Gynaecol. 2009;116(1):18–21.
Chileshe M. ARV treatment in ZAMBIA: current issues. Lusaka: Institute of Economic and Social Research, University of Zambia; 2014.
Wilson A, Gallos ID, Plana N, Lissaue D, Khan KS, Zamora J, MacArthur C. Effectiveness of strategies incorporating training and support of traditional birth attendants on perinatal and maternal mortality: meta-analysis. Br Med J. 2011;343(7102)
Godlonton S, Okeke EN. Does a ban on informal health providers save lives? Evidence from Malawi. J Dev Econ. 2016;1(118):112–32.
Acknowledgements
We would like to acknowledge the DHS team for their assistance in the collection and provision of the data.
Funding
The study was self-funded.
Availability of data and materials
The data generated and/or analyzed during the current study are available upon request to the DHS team.
Author information
Authors and Affiliations
Contributions
All authors collaborated and contributed in the formulation of objectives of the study and oversaw the development of the study concept and design, data collection, and analysis, including the drafting of the manuscript. All authors at every stage contributed to drafting, correcting, and perfecting the manuscript. CM was tasked with consolidating all the contributions to the manuscript and taking care of all correspondence. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained ethical clearance from the National Health Research Authority of Zambia. Other than that, ZDHS also provided clearance and permission for the use of HIV data.
Consent for publication
Consent to publish the results was granted by the National Research Authority of Zambia and the Demographic Health Survey team.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Appendix 1
Appendix 2
Appendix 3
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Muzyamba, C., Groot, W., Pavlova, M. et al. Professional care delivery or traditional birth attendants? The impact of the type of care utilized by mothers on under-five mortality of their children. Trop Med Health 46, 8 (2018). https://doi.org/10.1186/s41182-018-0090-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-018-0090-0