Abstract
Maternal and neonatal mortality and morbidity, particularly in developing countries, are high even in the twenty-first century, which is a cause for concern. Therefore, this paper examines the Continuum of Mother and Neonatal Health Care (MNH), i.e., at least four ante-natal care visits (ANC 4 +), skilled birth attendance at delivery (SBA), post-natal care (PNC), and its determinants in 10 developing countries in Asia. It uses Demographic and Household Survey data (2014–2021) and finds that only 46% of women received all the MNH services, and 8% did not receive any services. In Afghanistan, only 2.8% of women availed complete care of MNH services, followed by Timor-Leste (26.1%), Bangladesh (31.5%), Pakistan (35.1%), and Nepal (38.8%). Empirical analysis shows that women with higher education, those living in urban areas, from wealthy families, and female-headed households have higher odds of availing all MNH. Media exposure, ease of access to MNH services, and the women who have attended the first ANC at less than four months of pregnancy have higher odds of availing all three MNH services. Therefore, the MNH policy should target women in rural areas who have a lower level of education and come from low-income families to improve the mother and neonatal health situation in South and Southeast Asia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Reducing the burden of maternal and neonatal mortality and morbidity to achieve Sustainable Development Goal (SDG) 3 has become a major focus for public health and has been given top priority within the global political agenda (United Nations, 2016). Recent estimates by the World Health Organization (WHO, 2023) highlight that approximately 287,000 women died during pregnancy and childbirth in 2020, with almost 94% of all maternal deaths occurring in low- and middle-income countries. Messner et al., (2020), based on an assessment of 178 countries, classified 15 sub-Saharan African and South Asian countries as having a “very high” or “high” alert for maternal and neonatal mortality. These two regions accounted for 253,000 (about 88%) of maternal deaths in 2020 (WHO, 2023). South Asia contributed to one-fifth of global maternal deaths and is experiencing a dismal state of maternal mortality rate (MMR)Footnote 1 as the region is still struggling to achieve the SDG 3 target (WHO, 2023).
India had the second-highest estimated number of fatalities, accounting for 8% of global maternal deaths in 2020, with a 103 maternal mortality ratio per 100,000 live births (WHO, 2023). Although South and Southeast Asian countries share many similarities in aspects such as geographical proximity, socio-cultural factors, and health systems, the region’s maternal mortality ratio shows significant variation across countries. For example, Afghanistan had an MMR of 620 per 100,000 live births and was ranked among the top 10 countries with the highest MMR; Cambodia had an MMR of 218 per 100,000 live births; while, Maldives had an MMR of 57 per 100,000 live births (WHO, 2023). The high number of maternal deaths in the South and Southeast Asia region reflects inequalities in access to quality health services, highlighting gaps between different socio-economic groups (WHO, 2023). For instance, women in less developed countries tend to marry at a younger age than those in developed countries, increasing the risk of teenage pregnancy and leading to a lifetime risk of death or morbidity.
The major complications that cause nearly 75% of maternal deaths and up to two-thirds of neonatal deaths develop at three different maternal stages, i.e., complications during pregnancy; severe bleeding during childbirth, eclampsia; and infection after childbirth, and can be prevented by offering effective health measures right from pregnancy to the first week of childbirth (WHO, 2023). Considering the fact that nearly 800 women died each day in 2020 due to preventable reasons associated with pregnancy and childbirth, i.e., skill care before, during, and after childbirth, the maternal mortality and morbidity burden is unacceptably high (WHO, 2023). Thus, there is a need for a straightforward, cost-effective, and integrated approach “Continuum of Care” (CoC) to meet the maternal and neonatal health (MNH)Footnote 2 challenges, which include services during pregnancy and labour; skilled birth attendant (SBA)Footnote 3; and after-birth care for both mother and newborn. The continuum of care was a recurring theme in the World Health Report (2005), and in 2007, the World Health Assembly also emphasized the importance of CoC in maternal and neonatal health (MNH) services. According to The Lancet Neonatal Survival Series (2005), “The continuum-of-care approach promotes care for mothers and children from pregnancy to delivery, the immediate post-natal period, and childhood, recognizing that safe childbirth is critical to the health of both the woman and the newborn child—and that a healthy start in life is an essential step toward a sound childhood and a productive life.”
Earlier MNH services tended to address maternal and neonatal health issues separately. The CoC approach aims to avoid dichotomies between mothers and children, places of service delivery, or single health issues (Singh et al., 2016; Tinker et al., 2005). As Kerber et al. (2007) have defined, the health of the mother and the newborn are linked in the MNH–CoC framework and should be integrated, including during adolescence, pregnancy, childbirth, the post-natal period, and childhood. In this approach, all women should have access to reproductive health choices and care during pregnancy, delivery, and childbirth, and all babies should be able to grow into children who survive and thrive (Gill et al., 2007; Högberg, 2005; Kerber et al., 2007; Lawn et al., 2006; OECD, 2005).
Considering the scenario outlined above, this study applies the integrated approach of CoC, following women through their reproductive journey. With the onset of pregnancy, a mother should receive effective ante-natal care (ANC),Footnote 4 which is defined as care a woman receives from health professionals during pregnancy. During delivery, they should receive skilled birth attendance (SBA), defined as the presence of qualified healthcare professionals with technical competence to manage childbirth complications and provide immediate post-natal care. Finally, during the postpartum period, they should have continued post-natal care (PNC) for themselves and their newborns, defined as the care provided by healthcare professionals during the first 6–8 weeks after delivery, which is a fragile time for the mother and the newborn. The main objective is to quantify the integrated access to maternal and neonatal health care services in South and Southeast Asian countries to evaluate the dropouts that occur. A pregnant woman may drop out for several reasons, such as lack of access to the next facility due to poverty, decision-making power, preference, or other demographic and cultural covariates. Our multi-country analysis examines major components of the CoC, including at least four ante-natal visits, skilled birth assistance during delivery, and PNC within six weeks for the mother and the newborn. Including this, the next aim of this paper is to investigate the socio-economic and demographic differences between women who complete the continuum of care, as well as explore what variables predict completion.
Background of the region
South and Southeast Asia provide an important context for research on the accessibility of maternal and child health services. The sub-region is characterized by a high maternal mortality ratio, absence of affordable quality public health services, gender norms and restrictions on women’s mobility, and socio-demographic factors that continue to hinder the effective delivery of maternal and child health services (Tey & Lei, 2013; Asim et al., 2020; Raina et al., 2023). The sub-region is by far the worst affected by high fertility rates, child marriage, and teenage pregnancy (WHO, 2023; UNICEF, 2023). One in four young women in South Asia were first married or in a union before 18 years of age following maternal morbidities (UNICEF, 2023). For the country under study, a profile is provided in Table 1, which shows the wide variation in Maternal Mortality Ratio (ranging from 78 per 100,000 in the Philippines to 620 per 100,000 in Afghanistan), Infant Mortality Rate (ranging from 6 per 1000 in Maldives to 63 per 1000 in Pakistan), and Neonatal Mortality Rate (ranging from 4 per 1000 in Maldives to 39 per 1000 in Pakistan).
Data
This study used data from 10 Demographic Health Surveys (DHS) conducted between 2014 and 2021 in South and Southeast Asian countries: Afghanistan (2015), Bangladesh (2017–18), India (2019–21), Indonesia (2017), Cambodia (2014), Maldives (2016–17), Nepal (2016), Philippines (2017), Pakistan (2017–18), and Timor-Leste (2016). The analysis utilized the most recent data available for these countries. Funded by the U.S. Agency for International Development (USAID), DHS is a nationwide cross-sectional survey that provides nationally representative large-scale datasets across low- and middle-income countries. The survey used a two-stage stratified sampling design to collect data on major demographic indicators like fertility, mortality, reproductive health, and child health, including female empowerment indicators like decision-making and domestic violence. The details of survey design, data collection procedures, and implementation are described in the final reports of the respective surveys.
The individual files of women are used to identify disparities in the utilization of maternal and child health services. The questionnaire collects information on care provided to women during ante-natal visits, delivery, and postpartum. Comparable estimates are derived from the datasets of 10 different countries as the survey used the same sampling design and tool. The study focuses on women between 15 and 49 years of age who gave birth during the five years preceding the surveys, to avoid recall bias. In addition, the sample consisted of only women with complete observations on the variables of interest in this study. After dropping the missing observations, we obtained a sample of 246,025 women from all 10 countries. Permission to use the dataset was sought from Measure DHS.Footnote 5 Using combined datasets to analyze country effects could have been a more efficient approach. Pooling datasets increases the sample sizes of subgroups to reduce variances and generates more accurate confidence intervals for outcomes (Bangdiwala et al., 2016). However, there are concerns about the accuracy of findings when pooled datasets are used for a small number of countries (Bryan & Jenkins, 2016). Likely drawbacks are that combining different datasets increases the variability and could produce spurious results (Bangdiwala et al., 2016); however, the current datasets used in studies from 10 countries are homogenous as the sampling methods and instruments were similar and implemented by the same organization.
The study utilized pooled data to identify factors influencing the utilization of health care services for mothers and newborns at the regional level. Further, country-specific analysis was also performed, and the results are provided in the Supplementary file: Appendix 1-Table 1A, Appendix 2-Table 2A to 2J, and Appendix 3-Table 3A to 3J.
Outcome variable
The outcome variable of interest is a complete continuum of health care for mothers and newborns. This composite indicator was constructed by using indicators based on integrated health service delivery received at three stages: during pregnancy, during delivery, and after delivery, either at the health facility or at home. The indicators are defined as follows:
Health Services received during pregnancy: At least four visits (ANC 4 +) to the health care facility done by the respondent during pregnancy for health check-ups.
Health Services received during delivery: Childbirth assisted by a skilled birth professional, e.g., doctors, nurses, midwives.
Health Services received after delivery: Post-natal check-up for mother and newborn within six weeks after delivery.
A continuum of care was binary and considered discontinued if a woman had not availed of any of these services at any stage of pregnancy and childbirth. Firstly, visiting a healthcare facility for ANC check-ups was defined as a continuum of care during pregnancy (coded as 1 “who visited healthcare facility at least four times during pregnancy,” vs. 0 “who didn’t receive 4 + ANC services”). Secondly, receiving service during delivery (i.e., SBA) along with ANC 4 + service was defined continuum of care during delivery (coded as 1 “if a woman delivered the baby in the presence of skilled birth attended and received ANC4 + care,” vs. 0 “who received only ANC 4 + care”). Lastly, completion of ANC 4 + , SBA, along with post-natal care, defined as completed continuum care, (coded as 1 “individual who received post-natal care for herself and her baby along with SBA during pregnancy and ANC4 + during delivery,” vs. 0 “who received ANC 4 + & SBA”) (Haile et al., 2020; Mohan et al., 2017; Kikuchi et al., 2018; Hamed et al., 2018).
Independent variables
Based on the literature review carried out above and following the seminal work of Haile et al., 2020; Chalise et al., 2019; Lund et al., 2014; Yaya et al., 2016 regarding adequate usage of maternal health care, the study incorporated 14 socio-economic and demographic variables. These are: mother’s age at birth (bifurcated into < 20 years and > = 20 years groups); mother’s educational status (recoded as no education, primary, secondary, and higher); mother’s current occupation; coded into five groups (not working, white collar jobs, agricultural work, service, and manual work, don’t know or missing information); dwelling setting (coded as rural and urban); birth order of child (categorized as first, second, third, and fourth or higher); and wealth quintiles determined by creating asset indices based on household and characteristics of the house (such as drinking facility, building materials, toilet, and electricity). These variables are analyzed using principal component analysis, which produces components that are linear combinations of the variables. Urban and rural households are analyzed separately, and the resulting indices are scaled so that a given score on each index indicates the same level of wealth. Subsequently, households are divided into five quintiles based on their wealth score, with the lowest quintile representing the poorest 20% and the highest quintile representing the richest 20%. Women are then classified into these quintiles based on the wealth status of their household (Rutstein, 2008; Rutstein & Johnson, 2004). Mother’s exposure to media was computed by combining three types of media exposure, i.e., newspaper, radio, and television, and categorized as no exposure (not exposed to any of three), partially exposed (exposed to any two), and full exposure (exposed to all three). The desirability of the last pregnancy was recoded into three groups: wanted then, wanted later, and unwanted.
The sex of the child and household head (male vs. female) are also included in the analysis along with one accessibility variable, i.e., whether the distance to the health facility is a problem, and the response recorded into two categories” “big problem” and “not a big problem.” Service-related indicators, i.e., the timing of first ANC visit, defined as a visit in the first four months of pregnancy (coded as “yes” or “no”) were also considered. Our research also included other factors, such as getting permission to visit a health facility and getting money for medical support (coded as a “big problem” or “not a big problem”).
Methodology
Patient and public involvement statement
This study did not involve patients, as we used the publicly available Demographic and Health Surveys (DHS) datasets. Procedures and questionnaires for standard DHS surveys have been reviewed and approved by ICF Institutional Review Board (IRB). Additionally, country-specific DHS survey protocols are reviewed by the ICF IRB and typically by an IRB in the host country. ICF IRB ensures that the survey complies with the U.S. Department of Health and Human Services regulations for the protection of human subjects (45 CFR 46), while the host country IRB ensures that the survey complies with the laws and norms of the nation.
Model
We used univariate, bivariate, and three sequential logistic regression models to identify CoC predictors. Model I was fitted to all study participants to identify the factors that influenced ANC4 + visits. Among those women who received four or more ANC visits, some received SBA during delivery, and the second model was outfitted among those women who continued from ANC to SBA. Lastly, the third model was outfitted among women who had continued service until delivery and received care during the postpartum period, i.e., completed CoC. The models are described in Eq. (1)
where subscript \(k and j\) denote the woman and cluster, respectively; \({p}_{kj}\) is the probability that the j-th woman from community k completed CoC; \(\alpha\) is the constant corresponding to the study variable; \({X}_{kj}\) is the selected socio-economic and demographic characteristics of woman j for community k; \(\beta\) is a vector of constants giving the log odds resultant from a one-unit change in the variable \({X}_{kj}\) ; and \({\mu }_{kj}\) is the error term.
Further, the age of women at childbirth and the order of birth were classified into two groups to examine the contribution of various factors to the differences present in CoC. Mother’s age at birth was classified as less than 20 years and greater than 20 years to examine the effect of adolescent pregnancy on availing the MNH services; similarly, birth order was coded as categorical dummy first, second and third and higher. Multivariate decomposition analysis, also known as the Oaxaca–Blinder decomposition technique derived by Blinder (1973) and Oaxaca (1973), was used. An extended version designed for nonlinear regression is used for decomposition (Fairlie, 2005; Powers & Pullum, 2006; Power and Yun, 2009).
This approach provides an opportunity to clarify the extent to which group disparities in observed characteristics (covariates) contribute to differences in outcomes, as well as how much can be attributed to discrimination or differential effects of these observed characteristics. The results are broken down into three parts: endowment (explained), which denotes the portion of the difference explained by group variations in observable explanatory variables; coefficient, which represents the difference caused by varying effects of these variables on outcome across comparison groups and cannot be explained by their levels alone; and interaction, accounting for simultaneous effects from differences in endowments and coefficients. This decomposition analysis relies on information regarding completed CoC prevalence for selected covariates according to maternal age at birth, along with coefficients derived from multivariate binary logistic regression models predicting completed CoC for different maternal age categories separately. STATA 15.0 was utilized for all analyses, incorporating appropriate sampling weights during estimation.
Result
Descriptive presentation of the continuum of care
In the exhaustive analysis process, the first step is demonstrating COC in the South and Southeast Asia region across their background characteristics. Table 2 describes the socio-economic and demographic profile of the respondents selected in the study. Further, continuing with the bivariate analysis, Table 2 also depicts the prevalence of the continuum of care at each stage by selected covariates. In total (246,025), women age group 15–49 years were included in the analysis. Most women live in rural dwelling settings and belong to male-headed households. Fewer than half of women belong to the poorest and poorer wealth quintiles. More than one-fourth of them could not read and write, and more than one-fourth were unemployed. The finding highlights that almost two-thirds of women had been exposed to any one or two sources of media platforms.
Regarding the obstetric history of women, more than one-third of sampled women with birth order two, and about half of the last-born children were male. The finding also suggests that about 8% of respondents delivered a child at the age of 19 years or less. Regarding access to health care services, most women (71%) considered that distance to health facilities and availability of money for treatment are not big problems. Only 18% of women reported that getting permission to go to the health facility is a problem in seeking medical care. Findings revealed that most women went for their first ante-natal care visit within the first 16 weeks of the gestational period (68%). We also analyzed the country-specific prevalence of CoC at each stage by socio-economic and demographic characteristics of women for their most recent birth and found the result confirming the findings from the pooled data (presented in Supplementary file: Appendix 1-Table 1A).
Table 3 shows the utilization of a combination of MNH services received by the mother and the newborn. The finding highlights that almost half of the women had received all three services (46%), whereas 8% had not availed of any of these services. More than half of the women had availed of ANC 4 + services during pregnancy. Among all delivery and postpartum services, more than three-fourths (85%) of deliveries were assisted by an SBA, and more than two-thirds of sampled women received PNC care for themselves and the newborn. Less than one-fourth of women (15%) had received only one service, whereas almost one-third of women had availed at least two services. Considering the combinations of services, more than two-thirds had received SBA following with PNC, while the percentage of women who had availed ANC 4 + and PNC is exceptionally low (2%). Regarding the country-specific distribution, Afghanistan has the lowest prevalence of women who received MNH services (3%), followed by Timor-Leste and Bangladesh. More than two-thirds of Indonesian women received all three services, and less than 1% of Maldivian women had not received any service. In four of the ten countries there was a higher prevalence of complete CoC compared to the average in the South and Southeast Asian countries (Indonesia: 70%, Cambodia: 60%, Maldives: 60%, and the Philippines: 70%). In the remaining six countries, fewer than half of women received all three MNH services: Afghanistan (3%), Timor-Leste (26%), Bangladesh (32%), Pakistan (35%), Nepal (39%), and India (48%).
Figure 1 illustrates the continuum of care route map for selected maternal health services. The figure also highlights the occurrence of a large number of dropouts from one MNH to the next. The findings show that more than half of the sampled women received ANC 4 + service (58.8%); however, more than half of women (54.3%) had at least four ANC visits and delivery with SBA. About a one-tenth (7.6%) dropout was registered at this stage of the pathway. Further, in the last stage of CoC, fewer than half (45.6%) of women received all services: ANC 4 + , SBA, and PNC for mothers and newborns, with a loss of 16.2%. The most significant dropouts in the Continuum of Care were observed at the beginning of pregnancy, specifically in the receipt of ANC during pregnancy, resulting in a loss of nearly more than one-third of women (41%). The proportion of women who dropped out during delivery was the smallest across the continuum.
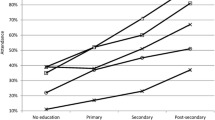
Table 4 represents the prevalence of CoC during pregnancy, delivery, and completed CoC among the pooled sampled women of all 10 countries according to the selected socio-economic and demographic covariates. The data show that mothers who live in urban areas had a greater proportion of CoC in all three care pathways, but the urban–rural gap in receiving MNH services is heterogeneous at different stages of CoC. The highest rural–urban coverage gap was recorded for receiving the CoC services during pregnancy (i.e., ANC 4 +) at around 9 percentage points. A monotonic increasing and significant association between the education of women and CoC for MNH services has been noted; illiterate women had received the lowest CoC starting from pregnancy and delivery to the postpartum period, which increased as the mother’s level of education increased. A similar positive relationship is also evident between household wealth and the CoC for MNH services. Women with white-collar jobs (clerical, managerial, professional, technical) had the highest CoC during pregnancy and delivery. Media exposure increases the percentage of CoC received during pregnancy, delivery, and completion. More than 90% of women who received CoC during childbirth were exposed to at least one source of the media platform.
Further, with the increase in maternal age, the percentage receiving CoC goes up; adolescent mothers (maternal age < 20 years) received CoC during pregnancy, delivery, and in the postpartum period lower than those who were 20 years and above. The woman’s current fertility status directly drives the use of MNH services. Table 4 shows that women with first-order birth had the highest percentage of CoC received, which gradually decreased as the birth order increased. Women with fifth and higher-order births registered the lowest reach of CoC services for all three touchpoints. Women with planned pregnancies had a higher rate of CoC compared with those who didn’t plan their fertility. The sex of the child and household head failed to explain the inequality in completing the CoC services. It is worth mentioning that women who visited for their first ante-natal check-up within the first 16 weeks of their pregnancy had higher CoC than those who didn’t receive ante-natal care within the first 16 weeks of pregnancy. Further noted that, at any given level, the coverage of MNH services is directly driven by the level of access and affordability of these services. Women who reported distance to the health facility, getting money for treatment, and getting permission to visit health facility as “not a big problem” had higher CoC (about 85% or more) than women who cited these as a problem. χ2 test was utilized to examine associations among the covariates and the study variables. The CoC by country is provided in the Supplementary file: Appendix 2-Table 2A to 2J, which confirms the finding of the pooled data.
Multivariate results of the continuum of care
Factors influence the continuum of complete MNH care using binary logistic regression
The impact of movement from one socio-demographic strata to another on the continuous utilization of MNH services has been estimated using binary logistic regression. A correlation matrix of estimates for variables used in the regression was created to check for the possible existence of multicollinearity. Each correlation value was found to be significantly less than 0.8, meeting the criterion and providing no evidence of multicollinearity. The regression result in terms of odds ratio with a 95% confidence interval is reported in Table 5. The odds ratios for women receiving ANC 4 + care compared with those who received none are shown in Column I; Column II is about the achievement of ANC 4 + and SBA compared with those who received only ANC 4 + , which are defined as continued care at delivery and the last column (III) illustrates the results of model III on complete CoC (ANC4 and SBA and PNC).
Our findings suggest that all selected covariates were significantly related to four or more ANC visits. This highlighted a strong association between ANC + 4 with education and wealth. Compared to illiterate women, those with higher education had significantly higher odds of receiving continuous care MNH services from pregnancy to postpartum. The odds of receiving CoC during delivery and completing CoC increased considerably with an increase in educational attainment. In addition to this, higher wealth quintiles lead to higher coverage of MNH services in a continuum fashion. Compared to women in the poorer wealth quintile, women in the richest wealth quintile were three times more likely to receive CoC during delivery; however, the odds of receiving complete CoC is 19% higher among the richest women compared to the poorer women. Women’s occupation seems to have a significant impact on the use of maternal health services.
Further, the odds of receiving ANC 4 + and ANC 4 + & SBA were higher (37% & 17%) if a woman resides in urban rather than rural areas. In contrast, the odds of receiving complete care were lower among urban dwellers than rural dwellers. Women in female-headed households had 1.06 times higher odds of receiving ANC 4 + care compared to women who belonged to male-headed households. In contrast, the odds of receiving ANC 4 + & SBA were 10% lower among the women who belonged to female-headed households compared to those who belonged to male-headed households. Exposure to mass media increased the odds of continuous use of MNH services starting from pregnancy to post-natal care. Notably, the odds of using ANC 4 + service were 9 times higher among the women who received their first ANC visit in the 16 weeks of the gestational period.
Overall, women of higher birth order had significantly lower odds of receiving a continuum of care during pregnancy, delivery, and postpartum compared with primiparous women. Women who gave birth in their 20s or later had significantly higher odds of receiving some or all the elements of the continuum of care compared to younger mothers. Finally, accessibility to health care services increased the odds of using MNH services. Women who recorded distance to a health facility as not a major issue had higher odds of receiving ANC 4 + , ANC 4 + , & SBA (65, 44, and 13%, respectively), and all three combined compared with those who quoted distance as a major issue. Similarly, women quoting no issue in getting money and permission to avail health services had higher odds of receiving MNH services compared with those who mentioned these as a problem.
This study also performed a sequential logistic regression for 10 countries to assess the inhibiting factors for women to continue using MNH services, and the result is summarized in Table 6. The detailed result for each country separately with odds ratio and 95% confidence interval is presented in the Supplementary file: Appendix 3-Table 3A to 3J. For continued care during pregnancy, the timing of the first ANC visit (within 4 months) emerges as the most significant driver, followed by media exposure, the mother’s education, and the family’s wealth. Nine out of 10 countries show that the odds of using ANC 4 + service were higher among the women who received their first ANC visit in the 16 weeks of the gestational period compared to those who didn’t visit a health facility in the first 16 weeks for ante-natal care. All 8 countries show that women from wealthier families had a higher chance of availing of MNH service during pregnancy.
Out of the 10 countries, 7 show that first-order children were more likely to receive ANC care than the fourth and higher-order children. For continued care during delivery, wealth status also emerges as the most significant driver in most countries, followed by the dwelling setting and the mother’s education. In over 7 countries, women in urban dwellings had higher odds of receiving ANC 4 + and SBA services than women living in rural areas. The education of mothers is positive and significant for using MNH services during delivery, and compared with illiterate women, women with secondary and higher education had higher odds of being cared for by skilled birth attendees during delivery in 8 and 7 countries, respectively. Similarly, wealth and media exposure were significant drivers for complete CoC. Wealthier women and women with full media exposure had higher odds of completing the MNH services compared with the poorest women with no media exposure in 4 and 6 countries, respectively.
Decomposition analysis using the Blinder–Oaxaca model
Tables 7 and 8 address the variation in the CoC in MNH services due to the woman’s age at childbirth and order of birth; bifurcate this difference into three components, i.e., endowment or explained part measure the gap attributable to the difference in women’s categories (“ < 20 years vs. > = 20 years” for age & “First vs. Second and higher” for birth order); and the remaining two parts (coefficient and interaction) measure the effects of these characteristics and their interaction with other characteristics.
Women’s age at childbirth (< 20 years vs. > = 20 years)
It is evident from Table 7 that adolescent mothers had a lower percentage of CoC of MNH services received than women who gave birth in the age group 20–49 years. Of the total difference in receiving ANC 4 + care over the group, almost 121% was accounted for by endowment effects, which explains the change in the composition of women. The remaining 21% unexplained difference was driven by the coefficient effects of the selected explanatory variable and the interaction term, but the result of the interaction effect was insignificant at 5% level of significance, indicating that differences in endowments and coefficients simultaneously between the two groups do not affect the difference in the outcome. However, the share of the explained effect was about 75% for receiving the care during pregnancy and delivery. In the case of complete CoC, only the coefficient was significant to the gap attributed between adolescent and mature mothers. Country-specific results show that 5 out of 10 countries offered significant and negative differences except for Nepal, which offered significant and higher odds among adolescent mothers for measuring the reach of ANC4 + service. For complete CoC, 5 countries showed significant and negative differences.
Birth order (first vs. second and higher)
The decomposition result for birth order is given in Table 8. It is evident from the result that first-order births had a higher percentage of CoC of MNH services received than second and higher-order births. 74%, 37%, and 67% of total differences in receiving ANC4 + , ANC4 + , and SBA and complete CoC services were accounted for by endowment or explained as part of the model. Talking about the country-specific results, the differences for receiving only ANC4 + service and ANC4 + with SBA are significant and in the same direction for all selected countries, whereas only 4 countries offered significant differences for completing all three services. In 7 out of 10 countries, the contribution of endowment parts is higher than the unexplained parts in measuring the reach of ANC4 + services, whereas for CoC during delivery, the contribution of the coefficient is higher than the endowment.
Discussion
This study applied a conservative approach to focus on the continuous use of MNH services. As the CoC framework promotes integrated MNH services, measuring the heterogeneity in utilizing healthcare facilities along the pathway of CoC in developing countries, including South and Southeast Asia, is crucial (Kothavale and Meher, 2021). Each element relates to a continuum of care framework that deals with maternal and child health services; thus, measurement of the current state of the continuum of care in South Asia, where maternal and child mortality is highest, is crucial (WHO, 2023).
Current research shows that only a small subset of South Asian women availed a complete continuum of care. The low completion rate of CoC in the region highlights a higher risk of maternal and neonatal mortality and morbidity. However, the reach of complete CoC is higher compared with the previous studies reported in Tanzania, Cambodia, Pakistan, Ethiopia, Nepal, and other sub-Saharan African and South Asian countries (Haile et al., 2020; Mohan et al., 2017; Kikuchi et al., 2018; Iqbal et al., 2017, Chalise et al., 2019). Despite its proven benefits and investment in the policies to alleviate maternal, neonatal, and child mortality rates, the suboptimal South Asian uptake of a complete continuum of care is a challenge. A low level of completion implies that most women, along with their newborns, could miss proven benefits at various contact points of the continuum, after conception, during birth, and in the postpartum period.
After examining the dropouts at the above-defined touch points on the care pathway, one can conclude that providing an enabling environment to pregnant women, such as family support, awareness, proximity to MNH facilities, community-based MNH extension to have at least four ante-natal visits is crucial for the completion of the continuum of care. A huge drop registered at the first stage of the CoC—all sampled women who received ANC4 + service. Many studies advocate the importance of receiving ANC 4 + care in safeguarding maternal and neonatal mortality (Stanton et al., 2007; Ensor et al., 2014; Adiwanou et al., 2013). ANC 4 + has a crucial link to other services, viz., SBA and PNC. The connection between ANC and other MNH services is well-established in academic literature (Adiwanou et al., 2013;Gottfredsdottir et al., 2016; Jacobs et al., 2017). In most pregnancies, ANC allows health personnel and pregnant women to discuss pregnancy-related issues like the health of the baby and mother, diet, complications, remedies, etc. Multiple interactions between health workers and mothers could explain the link between four or more ANC visits and skilled birth attendants during delivery, as this helps ensure efficient care (Guliani et al., 2012; Magoma et al., 2013).
Given the critical role of ANC4 + visits in the continuum of the care pathway, South and Southeast Asian countries need to encourage appropriate policies and ensure strict implementation to make such care easier to access and more affordable. In the growing phase of technologies, one can think of smart connectivity solutions, using mobile phones to send messages and calendar alarms, and spreading informative messages about the importance of ANC to help increase CoC’s reach. Previous research in Zanzibar proved that using a mobile phone to send reminders and messages about ANC visits and its benefits was positively related to a woman having at least four ANC visits (Lund et al., 2014).
In accordance with previous studies (James et al., 2022; Barman et al., 2020; Weitzman, 2017; Wang et al., 2015, Yaya et al., 2016), findings of the multivariate analysis highlighted that the richest, most educated, and working women had higher odds of availing MNH facilities. Older mothers had lower odds of receiving CoC at each touchpoint compared to adolescent mothers. One reason for this could be that a higher age can help a mother understand the benefit of safe motherhood and increase the chances of receiving high-quality and comprehensive maternal health care (Iqbal et al., 2017; Hamed et al., 2018). However, the odds of availing of complete or partial CoC decreased as the birth order increased. Women with higher birth order may have trouble accessing services because of childcare or may have relied on experiences from other pregnancies. Our study documented a significant and positive association between the accessibility variables and utilization of MNH services, confirming the findings of Bobo et al. (2017) and Master et al. (2013).
Conclusion and policy recommendations
Motivated by the fact that maternal and neonatal mortality and morbidity are prevalent in developing countries even today, this study uses the nationally representative Demographic and Household Survey (DHS) Data (2014–2021) from 10 South and Southeast Asian countries (Afghanistan, Bangladesh, India, Indonesia, Cambodia, Maldives, Nepal, Philippines, Pakistan, and Timor-Leste 2016) to analyze the Continuum of Mother and Child Health Care and its determinants. The results show that only 46% received all the maternal and neonatal health (MNH) care services, and 8% did not receive any services. Afghanistan had the lowest prevalence of receiving MNH services; only 3% of total women availed complete care of MNH services, followed by Timor-Leste and Bangladesh. Over two-thirds of Indonesian women received all three services, and less than 1% of Maldivian women had not received any service.
The regression result shows that compared with women living in rural areas, those residing in urban areas have a higher probability of availing of MNH services; hence, the policy to improve mother and child health should focus on rural women. Though the proportion of women-headed households is very small, women in female-headed households have higher odds of availing of CoC. This indicates that improving women’s decision-making power could go a long way in improving the MNH in developing countries. Women with higher education and those from more affluent families also tend to avail of CoC. Similarly, media exposure and ease of access also positively affect the households’ probability of availing of CoC. If the pregnancy is planned and the women have attended the first ANC at less than four months of pregnancy, they tend to avail MNH services.
This MNH policy in developing countries should target women living in rural areas and male-headed households to ensure CoC services coverage and attain SDG 3. Focus on gender sensitization is crucial to help men understand the importance of maternal and neonatal care. This can be achieved by encouraging couples to visit health centers together during pregnancy. Engaging men in MNH services is crucial. This can be done through targeted interventions to increase male involvement in decision-making regarding family planning and healthcare utilization. Challenges encountered by women residing in rural areas, such as limited transportation services, inadequate road infrastructure, the presence of trained health staff, and access to education and economic opportunities, require attention to enhance the utilization of MNH services. Further, the MNH policy should also focus on illiterate women from low-income families. A potential intervention could involve implementing reminders through mobile phones and utilizing IVR calls or text messages from the health department. This approach aims to remind pregnant women of their scheduled ante-natal care visits to help minimize the likelihood of missed appointments. Additionally, it creates an opportunity for comprehensive couple’s counselling at different touchpoints during and after pregnancy. Besides, media exposure and improving access and affordability of the MNH services would also improve coverage and reduce maternal and neonatal deaths in developing countries.
In summary, the findings of this study highlight a worrying lack of continuity in Maternal, Neonatal, and Child Health (MNCH) services in South and Southeast Asia. Factors such as education level, wealth index, and health insurance coverage were strongly associated with completing the continuum of care for MNCH services. One significant obstacle to achieving Continuum of Care for maternal and child health is the low utilization of Ante-natal Care services at the initial stage of the continuum. Addressing this issue is essential for improving the overall CoC completion rate. Despite continuous efforts by the government to ensure comprehensive ANC, there are still areas where adequate ANC levels remain insufficiently attained. The identified gaps across all CoC levels underscore an urgent need to prioritize a CoC approach in India’s MNCH system. A strategic plan should be developed to seamlessly connect all components of MNCH while minimizing dropouts and standardizing provision so that every woman and child can access these vital services.
Our analysis has some limitations. First, it was not possible to include quality aspects of MNH services offered in the health facilities. Second, the reasons for discontinuing CoC services, which include factors related to both beneficiaries and providers, are also lacking in the study. Furthermore, in a cross-sectional survey, responses are retrospective in nature, which may introduce bias due to recall, although this error was minimized by analyzing the information on the recent birth.
Notes
According to World Health Organization, “the maternal mortality ratio (MMR) is the number of maternal deaths during a given period per 100,000 live births during the same period. It shows the risk of maternal death in relation to the number of live births and effectively depicts the risk of death in a single pregnancy or a single live birth. The maternal mortality ratio can be computed by dividing documented maternal deaths by the total recorded live births in the same period and multiplying by 100,000” https://www.who.int/data/gho/indicator-metadata-registry/imr-details/26.
According to WHO, “Maternal health and neonatal/new born health is defined as the health of women during pregnancy, childbirth, and the postnatal period and the health for the first month of newborn babies.” https://www.who.int/europe/health-topics/maternal-health#tab=tab_1.
According to World Health Organization, SBA is defined as “an accredited health professional such as a midwife, doctor, or nurse who has been educated and trained to proficiency in the skills needed to manage normal (uncomplicated) pregnancies, childbirth, and the immediate postnatal period, and in the identification, management and referral of complications in women and newborns.” https://www.who.int/data/nutrition/nlis/info/births-attended-by-skilled-health-personnel.
According to WHO, “antenatal care (ANC) is defined as the percentage of women aged 15–49 with a live birth in a given time period that received antenatal care four or more times.” https://www.who.int/data/gho/indicator-metadata-registry/imr-details/80.
The dataset is publicly available on the Measure DHS website and can be accessed on request from https://dhsprogram.com/data/available-datasets.cfm.
References
Adjiwanou, V., & LeGrand, T. (2013). Does ante-natal care matter in the use of skilled birth attendance in rural Africa: A multi-country analysis. Social Science & Medicine, 86, 26–34.
Asim, M., Saleem, S., Ahmad, Z. H., Naeem, I., Abrejo, F., Fatmi, Z., & Siddiqi, S. (2020). Barriers to accessing maternal and newborn care: A qualitative study in district Thatta, Pakistan. https://doi.org/10.21203/rs.3.rs-124358/v1
Bangdiwala, S. I., Bhargava, A., O’Connor, D. P., Robinson, T. N., Michie, S., Murray, D. M., Stevens, J., Belle, S. H., Templin, T. N., & Pratt, C. A. (2016). Statistical methodologies to pool across multiple intervention studies. Translational Behavioral Medicine, 6(2), 228–35. https://doi.org/10.1007/s13142-016-0386-8
Barman, B., Saha, J., & Chouhan, P. (2020). Impact of education on the utilization of maternal health care services: An investigation from National Family Health Survey (2015–16) in India. Children and Youth Services Review, 108, 104642.
Blinder, A. S. (1973). Wage discrimination: Reduced form and structural estimates. Journal of Human Resources, 8, 436–455.
Bobo, F. T., Yesuf, E. A., & Woldie, M. (2017). Inequities in utilization of reproductive and maternal health services in Ethiopia. International Journal for Equity in Health, 16(1), 1–8.
Bryan, M. L., & Jenkins, S. P. (2016). Multilevel modelling of country effects: A cautionary tale. European Sociological Review, 32(1), 3–22.
Chalise, B., Chalise, M., Bista, B., Pandey, A. R., & Thapa, S. (2019). Correlates of continuum of maternal health services among Nepalese women: Evidence from Nepal Multiple Indicator Cluster Survey. PLoS ONE, 14(4), e0215613.
Ensor, T., Quigley, P., Green, C., Razak Badru, A., Kaluba, D., & Siziya, S. (2014). Knowledgeable ante-natal care as a pathway to skilled delivery: Modelling the interactions between use of services and knowledge in Zambia. Health Policy and Planning, 29(5), 580–588.
Fairlie, R. W. (2005). An extension of the Blinder-Oaxaca decomposition technique to logit and probit models. Journal of Economic and Social Measurement, 30(4), 305–316.
Gill, K., Pande, R., & Malhotra, A. (2007). Women deliver for development. The Lancet, 370(9595), 1347–1357.
Gottfredsdottir, H., Steingrímsdóttir, Þ, Björnsdóttir, A., Guðmundsdóttir, E. Ý, & Kristjánsdóttir, H. (2016). Content of ante-natal care: Does it prepare women for birth? Midwifery, 39, 71–77.
Guliani, H., Sepehri, A., & Serieux, J. (2012). What impact does contact with the prenatal care system have on women’s use of facility delivery? Evidence from low-income countries. Social Science & Medicine, 74(12), 1882–1890.
Haile, D., Kondale, M., Andarge, E., Tunje, A., Fikadu, T., & Boti, N. (2020). Level of completion along continuum of care for maternal and newborn health services and factors associated with it among women in Arba Minch Zuria woreda, Gamo zone, Southern Ethiopia: A community based cross-sectional study. PLoS ONE, 15(6), e0221670.
Hamed, A., Mohamed, E., & Sabry, M. (2018). Egyptian status of continuum of care for maternal, newborn, and child health: Sohag Governorate as an example. International Journal of Medical Science and Public Health, 7(6), 1.
Högberg, U. (2005). The World Health Report 2005:“Make every mother and child count”—including Africans. Scandinavian Journal of Public Health, 33(6), 409–411.
Iqbal, S., Maqsood, S., Zakar, R., Zakar, M. Z., & Fischer, F. (2017). Continuum of care in maternal, newborn and child health in Pakistan: Analysis of trends and determinants from 2006 to 2012. BMC Health Services Research, 17(1), 1–15.
Jacobs, C., Moshabela, M., Maswenyeho, S., Lambo, N., & Michelo, C. (2017). Predictors of ante-natal care, skilled birth attendance, and post-natal care utilization among the remote and poorest rural communities of Zambia: A multilevel analysis. Frontiers in Public Health, 5, 11.
James, K. S., Mishra, U. S., & Pallikadavath, S. (2022). Sequential impact of components of maternal and child health care services on the continuum of care in India. Journal of Biosocial Science, 54(3), 450–472.
Kerber, K. J., de Graft-Johnson, J. E., Bhutta, Z. A., Okong, P., Starrs, A., & Lawn, J. E. (2007). Continuum of care for maternal, newborn, and child health: From slogan to service delivery. The Lancet, 370(9595), 1358–1369.
Kikuchi, K., Yasuoka, J., Nanishi, K., Ahmed, A., Nohara, Y., Nishikitani, M., & Nakashima, N. (2018). Post-natal care could be the key to improving the continuum of care in maternal and child health in Ratanakiri, Cambodia. PloS One, 13(6), e0198829.
Kothavale, A., & Meher, T. (2021). Level of completion along continuum of care for maternal, newborn and child health services and factors associated with it among women in India: A population-based cross-sectional study. BMC Pregnancy and Childbirth, 21(1), 1–12.
Lawn, J. E., Tinker, A., Munjanja, S. P., & Cousens, S. (2006). Where is maternal and child health now? The Lancet, 368(9546), 1474–1477.
Lund, S., Nielsen, B. B., Hemed, M., Boas, I. M., Said, A., Said, K., & Rasch, V. (2014). Mobile phones improve ante-natal care attendance in Zanzibar: a cluster randomized controlled trial. BMC Pregnancy and Childbirth, 14(1), 1–10.
Magoma, M., Requejo, J., Campbell, O., Cousens, S., Merialdi, M., & Filippi, V. (2013). The effectiveness of birth plans in increasing use of skilled care at delivery and post-natal care in rural Tanzania: A cluster randomised trial. Tropical Medicine & International Health, 18(4), 435–443.
Masters, S. H., Burstein, R., Amofah, G., Abaogye, P., Kumar, S., & Hanlon, M. (2013). Travel time to maternity care and its effect on utilization in rural Ghana: A multilevel analysis. Social Science & Medicine, 93, 147–154.
Messner, J., Haken, N., Maglo, M., Cockey, S., Holzer, R., Fiertz, N., Taft, P., Wilson, W., Grathwohl, F., & Iuliano, K. (2020). Fragile States Index Annual Report 2020, https://fragilestatesindex.org/. The Fund for Peace, 1101 14th Street NW, Suite 1020, Washington, D.C. 20005, USA.
Mohan, D., LeFevre, A. E., George, A., Mpembeni, R., Bazant, E., Rusibamayila, N., & Baqui, A. H. (2017). Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy and Planning, 32(6), 791–799.
Oaxaca, R. (1973). Male-female wage differentials in urban labor markets. International Economic Review, 14, 693–709.
OECD. (2005). The Paris declaration on aid effectiveness. Organisation for Economic Cooperation and Development.
Powers, A. D., & Pullum, T. W. (2006). Multivariate decomposition for nonlinear models. The Stata Journal, 11(4), 556–576.
Powers, A. D., & Yun, M. S. (2009). Multivariate decomposition for hazard rate models. Sociological Methodology, 39(1), 233–263.
Raina, N., Khanna, R., Gupta, S., Jayathilaka, C. A., Mehta, R., & Behera, S. (2023). Progress in achieving SDG targets for mortality reduction among mothers, newborns, and children in the WHO South-East Asia Region. The Lancet Regional Health-Southeast Asia.
Rutstein, S. O., & Johnson, K. (2004). The DHS wealth index. ORC Macro.
Rutstein, S. O. (2008). The DHS wealth index: Approaches for urban and rural areas. Macro International.
Singh, K., Story, W. T., & Moran, A. C. (2016). Assessing the continuum of care pathway for maternal health in South Asia and sub-Saharan Africa. Maternal and Child Health Journal, 20(2), 281–289.
Stanton, C., Blanc, A. K., Croft, T., & Choi, Y. (2007). Skilled care at birth in the developing world: Progress to date and strategies for expanding coverage. Journal of Biosocial Science, 39(1), 109–120.
Tey, N. P., & Lai, S. L. (2013). Correlates of and barriers to the utilization of health services for delivery in South Asia and Sub-Saharan Africa. The Scientific World Journal.
Tinker, A., ten Hoope-Bender, P., Azfar, S., Bustreo, F., & Bell, R. (2005). A continuum of care to save newborn lives. The Lancet, 365(9462), 822–825.
United Nations. (2016). The Sustainable Development Goals (SDG) Report 2016, Department of Economic and Social Affairs (DESA). United Nations Publications, 300 East 42nd Street, New York, NY, 10017, United States of America.
United Nations Children’s Fund. (2023). A profile of child marriage in South Asia. UNICEF.
World Health Organization (2023). Trends in maternal mortality 2000 to 2020: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division.
World Health Statistics (2023). Monitoring health for the SDGs, Sustainable Development Goals. Geneva: World Health Organization; 2023. Licence: CC BY-NC-SA 3.0 IGO
Wang, W., & Hong, R. (2015). Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy and Childbirth, 15(1), 1–9.
Weitzman, A. (2017). The effects of women’s education on maternal health: Evidence from Peru. Social Science & Medicine, 180, 1–9.
Yaya, S., Bishwajit, G., & Shah, V. (2016). Wealth, education and urban–rural inequality and maternal healthcare service usage in Malawi. BMJ Global Health, 1(2), e000085.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rahut, D.B., Singh, A. & Sonobe, T. Continuum of maternal and new-natal health care: empirical evidence from 10 developing countries in South and South East Asia. J Pop Research 41, 11 (2024). https://doi.org/10.1007/s12546-024-09327-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s12546-024-09327-0