Abstract
Background
The aim of this study was to evaluate the associations between phase angle (PhA), sarcopenia, and the length of stay (LOS) in the coronary intensive care unit (ICU) in patients with non-ST acute coronary syndrome (NSTE-ACS).
Methods
This was a prospective observational study that evaluated 80 patients with NSTE-ACS over the age of 18 years, admitted to the ICU from January to June 2014. Upon admission, the patients’ demographic information was recorded. Handgrip strength and bioelectrical impedance analysis (BIA) were performed, and blood samples were taken within the first 72 h of admission. All of the patients were followed during their ICU stays.
Results
We evaluated 80 patients, five were excluded due to impossibility of assessing handgrip strength, and seven patients were not subjected to BIA. Thus, 68 patients with a mean age of 63.3 ± 13.1 years were included in the analysis. Among these patients, 60.1% were male, 27.9% of the patients had sarcopenia, 8.8% had LOSs ≥8 days, and median phase angle was 6.5 (6.1–7.3)°. Multiple logistic regression adjusted for age and gender revealed that PhA was not associated with the presence of sarcopenia. Additionally, PhA (OR 0.337; CI 95% 0.118–0.961; p = 0.04) but not sarcopenia (OR 0.517; CI 95% 0.055–4.879; p = 0.56) was associated with an increased LOS.
Conclusions
PhA is associated with LOS in patients with NSTE-ACS. Additionally, there was no association between PhA and sarcopenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Currently, cardiovascular diseases are the major cause of death worldwide [1, 2]. Acute coronary syndrome is the most common cause of cardiovascular morbidity and mortality [1, 2]. Acute coronary syndrome is a term that refers to a spectrum of conditions that are compatible with acute myocardial ischemia and/or infarction. Acute coronary syndrome is classified as ST elevation myocardial infarction or non-ST elevation acute coronary syndrome (NSTE-ACS). NSTE-ACS can be further divided into non-ST elevation myocardial infarction and unstable angina [1]. More than 625000 patients present with NSTE-ACS each year in the United States, and the in-hospital mortality is approximately 5–13% within 6 months [1, 2]. The 4-year mortality rate for NSTE-ACS is twofolds greater than that of ST-elevation myocardial infarction. This difference might be attributable to the fact that NSTE-ACS patients are older and have more comorbidities [3].
With the aging process, several alterations in organs and systems can lead to decreased strength and functionality [4]. Age-related decline in skeletal muscle mass and strength is defined as sarcopenia. The prevalence of sarcopenia is approximately 1 to 33% across different populations, and the direct costs of this condition in the United States exceed $18.5 billion annually [5]. Sarcopenia increases the risk for adverse outcomes, such as physical disability, poor quality of life, and death [4, 5]. Sarcopenia is associated with poor outcomes in patients who undergo major surgery and transplantation, patients with cancer, hospitalized patients, and elderly residents of nursing homes [6]. However, the role of sarcopenia in acute coronary syndrome outcomes has not yet been studied.
Currently, the diagnosis of sarcopenia is based on low whole-body or appendicular fat-free masses in combination with poor physical functioning [7]. There are several techniques for assessing skeletal muscle mass, including dual energy X-ray absorptiometry, magnetic resonance imaging, and bioelectrical impedance analysis (BIA). In addition to body composition assessment, one of the most clinically established impedance parameters is the phase angle (PhA) [7]. The PhA is estimated as the direct ratio between the resistance and reactance and has been used as a prognostic tool in several clinical situations, such as malnutrition and cancer [7, 8]. Basile et al. showed that the PhA in elderly patients is inversely related to muscle mass and strength and can be used to identify elderly patients who are at risk for sarcopenia [7].
The relationships between PhA, sarcopenia, and outcomes in hospitalized patients with NSTE-ACS have not yet been evaluated. The diagnosis of sarcopenia and lower values of PhA could identify patients that need a close monitoring and a more aggressive treatment. Thus, the aim of this study was to evaluate the associations between phase angle, sarcopenia, and the length of stay (LOS) in the ICU among patients with NSTE-ACS.
Methods
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human patients were approved by the Ethics Committee of the Botucatu Medical School (protocol number: 4213–2012). Written informed consent was obtained from all patients. The Fisher and Belle formula was used to estimate the sample size based on the following variables: a prevalence of sarcopenia in the general population of 1 to 33%, the 95% confidence interval, and a 10% sample error [5]. The result was a sample size of 62 patients.
In total, 80 patients with non-ST acute coronary syndrome over the age of 18 years who were admitted to the coronary intensive care unit from January to June of 2014 were prospectively evaluated. The exclusion criteria were pregnancy, valve disease, congenital cardiomyopathy, and corticosteroid use.
Upon admission, the patients’ demographic information, including age, gender, and diagnosis were recorded. Handgrip strength and BIA were assessed, and blood samples were collected for serum biochemistry within the first 72 h of admission. All of the patients were followed during their ICU stays, and the LOSs were recorded.
Sarcopenia was defined as a decreased skeletal muscle mass index (♀ < 6.76 and ♂ < 10.76 kg/m2) associated with a reduced handgrip strength (♀ < 20 and ♂ < 30 kg). The skeletal muscle mass index was calculated according to the following formula using the BIA data: SMI (kg/m2) = {[(height2/resistance*0.401) + (gender*3825) + (age*−0.071)] + 5102}/height2, where the height was in centimeter, the resistance was in ohms, gender was coded as men = 1, and woman = 0, and age was in years [4].
Non-ST acute coronary syndrome was defined as the presence of ischemic chest pain (retrosternal area with radiation to either or both of the arms, neck or jaw) with at least one of the following features: occurring at rest or with minimal exertion lasting ≥ 10 min, new onset or increased exertional dyspnea, the absence of ST elevation on an electrocardiogram, and with or without troponin increase [1].
LOS stay was categorized as less than 8 days or ≥ 8 days [1]. The definition of diabetes mellitus was based on clinical features, and a fasting glucose level of at least 126 mg/dL on two separate occasions or ongoing disease treatment. Systemic hypertension was defined by a systolic blood pressure greater than 140 mmHg and/or a diastolic blood pressure greater than 90 mmHg or ongoing disease treatment. Renal disease was defined as creatinine clearance < 60 ml/min/1.73 m2 on ICU admission calculated by Cockcroft-Gault formula.
Handgrip strength
Handgrip strength was measured as previously described [9]. Briefly, a standard adjustable handle (TEC-60; Technical Products; Clifton, NJ, USA) was used. All of the measurements were performed with the non-dominant hand, with the elbow supported on the bed, and with a trained examiner administering all of the tests. The subjects performed a maximum of three attempts for each measurement, and the best performance of these tests was recorded. During the testing, the participant was strongly encouraged to exert the maximum possible force. One minute rests were given between each attempt to minimize fatigue effects.
Laboratory data analysis
The total serum levels of creatine phosphokinase (CK), creatine phosphokinase-MB (CK-MB), sodium, potassium, creatinine, and urea were measured using the dry chemistry method (Ortho-Clinical Diagnostics VITROS 950®, Johnson & Johnson). The CK and CM-MB levels were measured every 6 h after ICU admission, and the highest levels were recorded. Troponin I was measured using the immunoenzymatic method. Hemograms were acquired with a Coulter STKS hematological autoanalyzer. The serum concentrations of 25(OH) vitamin D were assessed by high-performance liquid chromatography (HPLC; Immundiagnostik AG, Bensheim, Germany) according to a previously described method [10]. The assay sensitivity was 2.5 μg/L, and the coefficient of variation was < 7% [10].
Bioelectrical impedance analysis
BIA was measured using tetrapolar and single-frequency equipment (Biodynamic-450, 800 μA; 50 kHz) and applied to the skin using adhesive electrodes with the subject lying in the supine position. All measurements were performed in the morning by the same researcher. The phase angle derived from the BIA was determined as previously described, and its values were calculated as follows: phase angle = (arc tangent reactance/resistance * (180°/π)) [11]. The skeletal muscle mass index calculation has been described previously.
Statistical analysis
The data are expressed as the means ± SDs or medians (including the lower and upper quartiles). The statistical comparisons between groups for continuous variables were performed using Student’s t tests for parameters that were normally distributed. For data that were not normally distributed, the comparisons between groups (length of ICU stay < 8 days or ≥ 8 days; sarcopenia yes or no) were made using the Mann-Whitney test. Fisher’s tests or χ 2 tests were used for all categorical data. We also performed multiple logistic regression analyses that were adjusted for age and gender to evaluate the associations of phase angle, sarcopenia, skeletal muscle mass index, and handgrip strength with the length of ICU stay (≥8 days). The data analyses were performed using SigmaPlot software for Windows v12.0 (Systat Software Inc., San Jose, CA, USA). The significance level was 5%.
Results
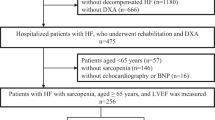
In total, 80 patients were evaluated, but five were excluded because they could not complete the handgrip strength test, and seven were excluded because they were not submitted to BIA testing within 72 h. Thus, 68 patients with a mean age of 63.3 ± 13.1 years were included in the analysis. Among these patients, 60.1% were male, 27.9% of the patients had sarcopenia, and the median PhA was 6.5 (6.1–7.3)°. The median LOS was 4 (3–5) days, and 8.8% of the patients had LOSs ≥ 8 days. No patients died during their ICU stays. The greatest proportion of patients had high-risk unstable angina (47.1%) followed by non-ST myocardial infarction (38.2%) and intermediate risk unstable angina (14.7%).
The demographic, clinical and laboratorial data according to LOS are listed in Table 1. The patients with lengths of ICU stays ≥ 8 days exhibited higher urea and lower CK and phase angle values. In Table 2, the patients’ characteristics are listed according to the presence of sarcopenia. The patients with sarcopenia were older, and the majority was male. Additionally, the patients with sarcopenia exhibited lower handgrip strength and phase angle values. There was no difference in vitamin D serum levels in the patients with and without sarcopenia. Importantly, the patients of both groups received adequate treatment.
As shown in Table 3, the phase angle was not associated with the presence of sarcopenia even after adjusting for age and gender (OR: 0.812; CI 95%: 0.538–1.225; p = 0.32). The multiple logistic regression analysis that was adjusted for age and gender (Table 4) revealed that the phase angle (OR: 0.337; CI 95%: 0.118–0.961; p = 0.04) but not sarcopenia (OR: 0.517; CI 95%: 0.055–4.879; p = 0.56) was associated with a higher LOS. The skeletal muscle mass index and handgrip strength were also not associated with LOS. For each one-degree increase in PhA, the likelihood of a longer LOS decreased by almost threefolds.
Discussion
The aim of this study was to evaluate the associations between PhA, sarcopenia, and LOS in patients with NSTE-ACS. The diagnosis of sarcopenia and lower values of PhA could identify patients that need a close monitoring and a more aggressive treatment. However, only PhA was associated with LOS in these patients. Additionally, there was no association between PhA and sarcopenia.
Due to the importance of acute coronary syndrome, the identification of modifiable risk factors that could help to improve outcomes is urgent. Sarcopenia is associated with adverse clinical outcomes in several diseases; however, the association between sarcopenia and acute coronary syndrome had not yet been evaluated [6, 12, 13].
It is also important to consider that the characteristics of sarcopenia are included in frailty diagnoses [4]. Thus, most frail older people also exhibit sarcopenia [4]. There are several mechanisms involved in the onset and progression of sarcopenia, such protein synthesis, neuromuscular integrity, muscle fat content and hormonal changes including changes in vitamin D status [4, 14]. In the present study, the prevalence of sarcopenia among the patients with NSTE-ACS was the same as that described for the general population. Additionally, as we expected, the patients with sarcopenia were older and exhibited lower handgrip strengths than the patients without this condition. Although our objective was not to evaluate the association between sarcopenia and vitamin D status, it is interesting that the vitamin D serum levels were not lower in the patients with sarcopenia. Vitamin D deficiency has been associated with muscle strength reductions and increased numbers of falls in older people [15]. Visser et al. reported that older adults with vitamin D serum levels below than 25 nmol/L exhibit decreased skeletal muscle mass and strength [16]. In this study, the acute phase response due to NSTE-ACS could have influenced the vitamin D serum levels. Additionally, different cutoffs values for identifying vitamin D deficiencies might also explain these differences.
Regarding the length of hospital stay, Gariballa and Alessa reported that the length of hospital stay was longer in patients with sarcopenia among a cohort of 432 hospitalized older patients [17]. Additionally, Cawthon et al. reported that in adults aged 70 to 80 years, low muscle density and grip strength were associated with greater risks of hospitalization [18]. It is also interesting that increases in the length of hospital stay worsen sarcopenia, which creates a vicious cycle of disease severity and increases in the length of hospital stay and re-hospitalization rate [19]. However, in our study, the presence of sarcopenia did not influence the LOS.
The association between sarcopenia and PhA has also been evaluated. In a recent study, the relationships of PhA with muscle mass and strength were investigated in 207 elderly participants who were admitted for multidimensional geriatric evaluation [7]. The authors found that PhA was inversely related to muscle mass and strength in elderly subjects [7]. Wilhelm-Leen et al. also revealed that lower PhAs were associated with frailty and mortality in 4667 older adults [20]. However, there was no association between PhA and sarcopenia in our study. The reason that this relationship was not observed in our study remains to be elucidated.
In addition to the calculation of the PhA, BIA is typically used to estimate body composition and skeletal muscle mass. BIA is a non-invasive method that measures the opposition of the body to alternating currents consisting of both resistance and reactance [21]. The reactance arises from the cell membranes, and the resistance arises from the extra- and intracellular fluids [21]. BIA divides the body into two compartments, i.e., fat-free mass and fat mass. The fat-free mass includes visceral proteins, bone mineral content, and intra- and extracellular water. Thus, there are a large number of BIA equations in the literature for predicting fat-free mass [8]. The formula that we used to estimate skeletal muscle mass is that of the European Consensus of Sarcopenia in Older Adults [4]. Other techniques for assessing skeletal muscle can be used including dual energy X-ray absorptiometry and magnetic resonance imaging; however, BIA is a portable, easy-to-use and inexpensive method [21].
The PhA is estimated as the ratio between resistance and reactance. The relationship between these factors reflects different electrical properties of tissues that are affected in different manners by disease, hydration and nutritional status [21]. Additionally, due to its close correlations with nutritional and functional statuses, PhA has been used to predict outcomes in different clinical situations. Authors have found that low PhA values predict worse outcomes in patients with renal insufficiency, liver cirrhosis, and surgical patients [22–24]. However, PhA had not previously been evaluated in patients with NSTE-ACS. In our study, the patients with higher PhA values were associated with lower LOSs even after adjusting for age and gender. For each one-degree increase in PhA, the likelihood of a longer LOS decreased by almost threefolds. Therefore, PhA could be incorporated into clinical practice as a tool for predicting the LOSs of patients with NSTE-ACS.
It is important to consider some limitations of our study. Our study included a small sample size and patients from a unique medical center. We also used single-frequency BIA to determine the reactance and resistance and to evaluate the skeletal muscle mass index. Despite these limitations, this is the first study to evaluate the relationship between PhA and sarcopenia in patients with NSTE-ACS.
Conclusions
In conclusion, PhA, but not sarcopenia, is associated with the lengths of ICU stay in patients with NSTE-ACS. Additionally, there was no association between PhA and sarcopenia.
Abbreviations
- BIA:
-
Bioelectrical impedance analysis
- CK:
-
Creatine phosphokinase
- CK-MB:
-
Creatine phosphokinase-MB
- ICU:
-
Intensive care unit
- LOS:
-
Length of stay
- NSTE-ACS:
-
Non-ST acute coronary syndrome
- PhA:
-
Phase angle
- SMI:
-
Skeletal muscle mass index
References
Amsterdam EA, Wenger NK, Brindis RG, Casey Jr DE, Ganiats TG, Holmes Jr DR, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e344–426.
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. 2016;37:267–315.
Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, et al. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–93.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on Sarcopenia in older people. Age Ageing. 2010;39:412–23.
Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43:748–59.
Beaudart C, Rizzoli R, Bruyère O, Reginster JY, Biver E. Sarcopenia: burden and challenges for public health. Arch Public Health. 2014;72:45.
Basile C, Della-Morte D, Cacciatore F, Gargiulo G, Galizia G, Roselli M, et al. Phase angle as bioelectrical marker to identify elderly patients at risk of sarcopenia. Exp Gerontol. 2014;58:43–6.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, et al. Bioelectrical impedance analysis--part I: review of principles and methods. Clin Nutr. 2004;23:1226–43.
Gumieiro DN, Rafacho BP, Gradella LM, Azevedo PS, Gaspardo D, Zornoff LA, et al. Handgrip strength predicts pressure ulcers in patients with hip fractures. Nutrition. 2012;28:874–8.
Gumieiro DN, Murino Rafacho BP, Buzati Pereira BL, Cavallari KA, Tanni SE, Azevedo PS, et al. Vitamin D serum levels are associated with handgrip strength but not with muscle mass or length of hospital stay after hip fracture. Nutrition. 2015;31:931–4.
Kyle UG, Soundar EP, Genton L, Pichard C. Can phase angle determined by bioelectrical impedance analysis assess nutritional risk? A comparison between healthy and hospitalized subjects. Clin Nutr. 2012;31:875–81.
Sheetz KH, Waits SA, Terjimanian MN, Sullivan J, Campbell DA, Wang SC, et al. Cost of major surgery in the sarcopenic patient. J Am Coll Surg. 2013;217:813–8.
Tan BH, Birdsell LA, Martin L, Baracos VE, Fearon KC. Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res. 2009;15:6973–9.
Lang T, Streeper T, Cawthon P, Baldwin K, Taaffe DR, Harris TB. Sarcopenia: etiology, clinical consequences, intervention, and assessment. Osteoporos Int. 2010;21:543–59.
Snijder MB, van Schoor NM, Pluijm SM, van Dam RM, Visser M, Lips P. Vitamin D status in relation to one-year risk of recurrent falling in older men and women. J Clin Endocrinol Metab. 2006;91:2980–5.
Visser M, Deeg DJ, Lips P. Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab. 2003;88:5766–72.
Gariballa S, Alessa A. Sarcopenia: prevalence and prognostic significance in hospitalized patients. Clin Nutr. 2013;32:772–6.
Cawthon PM, Fox KM, Gandra SR, Delmonico MJ, Chiou CF, Anthony MS, et al. Do muscle mass, muscle density, strength, and physical function similarly influence risk of hospitalization in older adults? J Am Geriatr Soc. 2009;57:1411–9.
Vandewoude MF, Alish CJ, Sauer AC, Hegazi RA. Malnutrition-sarcopenia syndrome: is this the future of nutrition screening and assessment for older adults? J Aging Res. 2012;2012:651570.
Wilhelm-Leen ER, Hall YN, Horwitz RI, Chertow GM. Phase angle, frailty and mortality in older adults. J Gen Intern Med. 2014;29:147–54.
Norman K, Stobäus N, Pirlich M, Bosy-Westphal A. Bioelectrical phase angle and impedance vector analysis--clinical relevance and applicability of impedance parameters. Clin Nutr. 2012;31:854–61.
Barbosa-Silva MC, Barros AJ. Bioelectric impedance and individual characteristics as prognostic factors for post-operative complications. Clin Nutr. 2005;24:830–8.
de Souza Dorna M, Santos LA, Gondo FF, Augusti L, Franzoni LC, Sassaki LY, et al. Phase angle is associated with advanced fibrosis in patients chronically infected with hepatitis C virus. Life Sci. 2016. [in press].
de Araujo Antunes A, Vannini FD, de Arruda Silveira LV, Barretti P, Martin LC, Caramori JC. Associations between bioelectrical impedance parameters and cardiovascular events in chronic dialysis patients. Int Urol Nephrol. 2013;45:1397–403.
Acknowledgements
This study was supported by the São Paulo Research Foundation (FAPESP 2013/05478-6).
Authors’ contributions
BFP, MAH are responsible for data collection and writing of the manuscript; BLBP, RACS, AFG, KAC, NAC, PSA, and MSD are responsible for data collection; SET statistical analysis; LAMZ, SARP, and MFM are responsible for study design, data interpretation, correction of the manuscript. All authors read and approved the final manuscript.
Competing interests
The editor-in-chief of Nutrire, Marcos Minicucci, is one of the authors of this article. He did not get involved in the peer review process of this manuscript. The other authors declare that there are no conflicts of interest.
Ethics approval and consent to participate
This study was approved by the local ethics committee (protocol number 4213–2012), and informed consent to participate in this study was obtained of all participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Polegato, B.F., Herrera, M.A., Pereira, B.L.B. et al. Phase angle is associated with the length of ICU stay in patients with non-ST elevation acute coronary syndrome. Nutrire 42, 2 (2017). https://doi.org/10.1186/s41110-016-0026-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41110-016-0026-6