Abstract
Background
Peritoneal dialysis (PD)-associated peritonitis caused by Sphingomonas paucimobilis (S. paucimobilis) is very rare, and most of the characteristics of such cases are still unknown.
Case presentation
An 80-year-old Japanese woman on PD was diagnosed with PD-associated peritonitis and received ceftazidime and cefazolin. The number of cells in the peritoneal dialysate decreased quickly. However, because S. paucimobilis was detected, the antibiotic was changed to meropenem according to the susceptibility test results. She was treated with meropenem for two weeks and discharged. After 21 days, she was hospitalized for relapsing peritonitis. S. paucimobilis was detected again, and improvement after the administration of meropenem was poor, eventually resulting in catheter removal.
Conclusions
S. paucimobilis may be resistant to empirical antibiotics; furthermore, catheter removal may still be required, even with sensitive-antibiotic treatment.
Similar content being viewed by others
Background
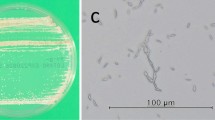
Sphingomonas paucimobilis (S. paucimobilis) is a non-fermentative Gram-negative bacillus that is widely distributed in nature and is also present in the hospital environment [1, 2]. S. paucimobilis rarely infects humans, but when it does, it is suspected to cause meningitis, urinary tract infection, endophthalmitis, splenic abscess, arthritis, osteomyelitis, empyema, pneumonia, and catheter-related infection [2,3,4]. It has been reported that contaminated solutions, such as distilled water, haemodialysis fluid and sterile drug solutions, cause bacteraemia and sepsis [2]. The pathogenicity of S. paucimobilis is considered to be low because the prognosis is generally good despite inappropriate treatment [3]. S. paucimobilis infection is most likely to occur in patients complicated with underlying diseases, such as malignant carcinoma, immunodeficiency, or diabetes [3, 4]. The incidence of peritoneal dialysis (PD)-associated peritonitis has decreased due to technological progress [5], but it remains an important complication and a major cause of PD withdrawal [6]. In this report, we present the case of a woman with PD-associated peritonitis caused by S. paucimobilis who had to undergo catheter removal and PD withdrawal. Given that studies on S. paucimobilis-related peritonitis are rarely reported, this is considered a valuable case.
Case presentation
An 80-year-old Japanese woman developed end-stage renal disease due to nephrosclerosis 2 years previously and started maintenance haemodialysis. Six months later, PD, instead of haemodialysis, was initiated due to remarkably low left heart function. She underwent three-cuff Swan neck catheter implantation. She used an automated connecting device with ultraviolet light undergoing PD. She visited our hospital after experiencing discomfort; she was admitted because of cloudy dialysate and mild abdominal pain starting on the previous day. The dialysis effluent white cell count was 4875/μL, with a predominance of neutrophils (86%), and she was diagnosed with PD-associated peritonitis. On admission, her body temperature was 36.4 ℃, blood pressure was 133/71 mmHg, heart rate was 70/min, height was 155 cm, and weight was 49.9 kg. Only mild abdominal tenderness was noted without muscular defence or rebound tenderness. Diarrhoea was not present. No apparent signs of infection at the exit or in the tunnel were observed. Laboratory findings on admission are summarized in Table 1. Her haemoglobin was 12.2 g/dL, white blood cell (WBC) count was 5600/μL, C-reactive protein was 3.20 mg/dL (normal < 0.3 mg/dL), and albumin was 2.6 g/dL. Blood culture was negative. When 1 g of ceftazidime and 1 g of cefazolin were administered intraperitoneally daily, the dialysis effluent white cell count decreased rapidly. On the fourth day, Gram-negative rods were detected in the peritoneal fluid culture, so only ceftazidime was administered. The causative organism was subsequently identified as S. paucimobilis. Given that this organism was resistant to ceftazidime and sensitive to meropenem (Table 2), antibiotic treatment was changed to 0.5 g of intravenous meropenem per day on the seventh day. This dosage was administered for 2 weeks. After the antibiotic was changed to meropenem, the dialysis effluent white cell count was continuously greater than 100/μL, but the neutrophil count in the dialysis effluent was decreased. The neutrophil percentage was 3% on the 18th day. Therefore, we considered meropenem to be effective. The patient was discharged on the 21st day (Fig. 1).
However, three weeks later, the dialysate became cloudy again. The dialysis effluent white cell count was 2604/μL, with a predominance of neutrophils (97%). She was admitted a second time for relapsing peritonitis. On the second admission, her body temperature was 36.7 ℃, blood pressure was 129/73 mmHg, and heart rate was 65/min. As before, mild tenderness was noted throughout the abdomen, without muscle defence or rebound tenderness. No clear signs of infection at the exit tunnel were observed. The haemoglobin level was 10.4 g/dL, WBC count was 5800/μL, C-reactive protein was 2.27 mg/dL, and albumin was 2.5 g/dL (Table 1). From the first day of the second hospitalization, 0.5 g of intravenous meropenem was administered daily. S. paucimobilis was detected again in the peritoneal fluid culture during the second admission, and sensitivity testing indicated that it was sensitive to meropenem (Table 2). On the sixth day of the second hospitalization, the dialysis effluent white cell count was 1376/μL. Due to poor improvement, 15 mg of tobramycin was additionally administered intraperitoneally daily. On the ninth day of the second hospitalization, the dialysis effluent white cell count decreased to 337/μL, but we hypothesized that peritonitis was not controlled, because S. paucimobilis was detected again in the peritoneal fluid culture on the 6th day. Furthermore, we were worried that the patient was exhausted. On the next day, the PD catheter was removed (Fig. 1). The culture results of the internal cuff, middle cuff, external cuff, catheter between the internal cuff and middle cuff, catheter between the middle cuff and external cuff, and catheter tip were negative. She transitioned to haemodialysis, continued to receive meropenem for 15 days after surgery and was discharged.
Discussion and conclusions
S. paucimobilis is an unusual pathogen for PD-associated peritonitis. We report a case of peritonitis due to S. paucimobilis that required catheter removal.
Lin et al. reported 42 cases of S. paucimobilis bacteraemia [3]. In that study, primary S. paucimobilis bacteraemia was found in 35.7% of patients. Catheter-related bloodstream infections were identified in 33.3% of patients, skin and soft tissue infections were identified in 9.5% of patients, pneumonia was identified in 9.5% of patients, urinary tract infections were identified in 4.8% of patients, biliary tract infections were identified in 4.8% of patients, and meningitis was identified in 2.4% of patients. Although three patients experienced septic shock, all 42 patients survived the S. paucimobilis bacteraemia episodes. The authors concluded that S. paucimobilis exhibited low clinical virulence. S. paucimobilis infections other than PD-related peritonitis may not be difficult to treat.
Fourteen cases of PD-associated peritonitis due to S. paucimobilis have been reported. The clinical characteristics of this case and the cases reported thus far are summarized in Table 3 [7,8,9,10,11,12,13,14,15,16,17,18,19]. The ages of patients ranged from 3.5 to 80 years, and there was no difference in the male-to-female ratio at 7:8. The reports included 2 diabetic patients, 10 nondiabetic patients, and 3 patients with unknown status, and no particular diabetic complications were noted. There were two cases in which the only symptom was cloudy dialysate; however, most cases were accompanied by abdominal symptoms.
Catheters were removed in 8 of 15 cases. The difference between patients who do versus do not require catheter removal is unclear. However, the unpredictable antibiotic sensitivity pattern of S. paucimobilis has been implicated in therapeutic failure [12]. Depending on the antibiotic sensitivity pattern of S. paucimobilis, the appropriate treatment can be delayed, which may lead to a refractory infection. Imipenem or meropenem alone and an aminoglycoside plus a third-generation cephalosporin have been suggested as suitable antibiotics for the treatment of infections caused by this organism [15, 20]. However, Bayram et al. reported that 20.0% of bacteria in reported cases were resistant to cefotaxime, and 13.6% were resistant to amikacin [21]. In the present summary, S. paucimobilis was sensitive to ceftazidime in a few cases. Regarding empirical treatment of PD-associated peritonitis, selection of third-generation cephalosporins or aminoglycosides is recommended for Gram-negative bacteria [6]. However, it should be noted that S. paucimobilis may be resistant to these antibiotics. In the case reported by Lee et al., the bacterium was initially sensitive to ceftazidime, and peritonitis improved, but when it recurred, the bacterium showed resistance to ceftazidime, resulting in catheter removal [16]. Therefore, antibiotic resistance was observed during monotherapy with ceftazidime. Even if S. paucimobilis is sensitive to third-generation cephalosporins, the addition of an aminoglycoside to a third-generation cephalosporin may be beneficial. The organism responsible for infection of the patient in the present case was resistant to ceftazidime and sensitive to meropenem. Antibiotic resistance during monotherapy with meropenem was not noted. However, because this bacterium was detected during meropenem administration, the combined use of another antibiotic (e.g. tobramycin) should have been considered when relapse occurred.
In this review, 5 of 8 patients with catheter removal, including the present patient, relapsed after improvement and required catheter removal. Biofilm formation is one of the causes of relapse. Although the culture results of the areas between the cuffs and catheter tip were negative, we suggest that it is possible that a biofilm was formed on the PD catheter in this patient. Nodaira et al. reported that all catheters removed because of PD-associated peritonitis showed biofilms on electron microscopy (EM) scanning; however, patients with catheters removed for other reasons, such as gastrointestinal neoplasm or perforation, did not demonstrate biofilms [22]. EM scanning might have detected a biofilm in the present case. The administration of meropenem was delayed for this patient. Generally, a delay in starting initial antimicrobial therapy can allow pathogens to proliferate, rendering patients less responsive to treatment. Moreover, biofilms that form due to delayed treatment initiation might increase the risk of catheter removal by contributing to the re-development of peritonitis after initiation of treatment [23]. If S. paucimobilis is detected and initiation of appropriate treatment is delayed, careful observation is important even after treatment with effective antibiotics because of the risk of relapse.
In this case, the patient was treated with meropenem for only 2 weeks during the first admission because the dialysis effluent white cell count decreased rapidly after cefazolin and ceftazidime were administered, and ceftazidime was administered for one week. The International Society for Peritoneal Dialysis Guidelines (ISPD GL) recommend treating Gram-negative bacilli peritonitis with effective antibiotics for three weeks [6]. Recent studies have reported success in patients who were treated with two antibiotics for three weeks [17, 19]. More than half of the previous reports described failure to eradicate this bacterium, suggesting that two effective antibiotics are needed for three weeks (Table 3).
In summary, we treated a patient with PD-associated peritonitis due to S. paucimobilis and summarized and described the cases reported thus far. PD-associated peritonitis due to S. paucimobilis is extremely rare, but it is important because catheter removal is often required.
Availability of data and materials
All data and materials were included in the manuscript.
Abbreviations
- PD:
-
Peritoneal dialysis
- S. paucimobilis :
-
Sphingomonas paucimobilis
- WBC:
-
White blood cell
- ISPD GL:
-
International Society for Peritoneal Dialysis Guidelines
- UV:
-
Ultraviolet
- EM:
-
Electron microscopy
References
Pascale R, Russo E, Esposito I, Leone S, Esposito S. Sphingomonas paucimobilis osteomyelitis in an immunocompetent patient: a rare case report and literature review. New Microbiol. 2013;36:423–6.
Ryan MP, Adley CC. Sphingomonas paucimobilis: a persistent gram-negative nosocomial infectious organism. J Hosp Infect. 2010;75:153–7.
Lin JN, Lai CH, Chen YH, Lin HL, Huang CK, Chen WF, Wang JL, Chung HC, Liang SH, Lin HH. Sphingomonas paucimobilis bacteremia in humans: 16 case reports and a literature review. J Microbiol Immunol Infect. 2010;43:35–42.
Toh HS, Tay HT, Kuar WK, Weng TC, Tang HJ, Tan CK. Risk factors associated with Sphingomonas paucimobilis infection. J Microbiol Immunol Infect. 2011;44:289–95.
Mehrotra R, Devuyst O, Davies SJ, Johnson DW. The Current State Of Peritoneal Dialysis. J Am Soc Nephrol. 2016;27:3238–52.
Li PK, Szeto CC, Piraino B, de Arteaga J, Fan S, Figueiredo AE, Fish DN, Goffin E, Kim YL, Salzer W, Struijk DG, Teitelbaum I, Johnson DW. ISPD peritonitis recommendations: 2016 update on prevention and treatment. Perit Dial Int. 2016;36:481–508.
Glupczynski Y, Hansen W, Dratwa M, Tielemans C, Wens R, Collart F, Yourassowsky E. Pseudomonas paucimobilis peritonitis in patients treated by peritoneal dialysis. J Clin Microbiol. 1984;20:1225–6.
Swann RA, Foulkes SJ, Holmes B, Young JB, Mitchell RG, Reeders ST. Agrobacterium yellow group and Pseudomonas paucimobilis causing peritonitis in patients receiving continuous ambulatory peritoneal dialysis. J Clin Pathol. 1985;38:1293–9.
Baddour LM, Kraus AP Jr, Smalley DL. Peritonitis due to Pseudomonas paucimobilis during ambulatory peritoneal dialysis. South Med J. 1985;78:366.
Nguyen V, Swartz RD, Reynolds J, Wilson D, Port FK. Successful treatment of Pseudomonas peritonitis during continuous ambulatory peritoneal dialysis. Am J Nephrol. 1987;7:38–43.
De Paoli VE, Rossi MR, Farinelli A. Pseudomonas-like species IIK-1 peritonitis in peritoneal dialysis. Nephron. 1988;48:337.
Phillips G, Fleming LW, Stewart WK. Pseudomonas paucimobilis peritonitis in a patient on CAPD successfully treated with ciprofloxacin and netilmicin. Eur J Clin Microbiol Infect Dis. 1990;9:630–1.
Yoon JS, Hwang EA, Chang MH, Park WY, Jin KB, Han SY, Park SB, Kim HC, Ryoo NH. Peritonitis by Chryseobacterium indologenes and Sphingomonas paucimobilis in a patient undergoing continuous ambulatory peritoneal dialysis (CAPD). Korean J Nephrol. 2007;26:801–5.
Dervisoglu E, Meric M, Kalender B, Sengul E. Sphingomonas paucimobilis peritonitis: a case report and literature review. Perit Dial Int. 2008;28:547–50.
Tambawala AQ, Hamid S, Khan I, Ali A. CAPD associated peritonitis in a child: a rare case of peritonitis caused by Sphingomonas paucimobilis. J Pak Med Assoc. 2011;61:178–80.
Lee JU, Kim JK, Yun SH, Park MS, Lee NE, Sun IO, Lee KY. A case of peritoneal dialysis-associated peritonitis caused by Sphingomonas paucimobilis. Kidney Res Clin Pract. 2013;32:78–80.
Mohan D, Railey M. Sphingomonas paucimobilis peritonitis: a case report and review of the literature. Saudi J Kidney Dis Transpl. 2015;26:567–71.
Owen J, Washco V, Reisin E. Successful return to peritoneal dialysis after a case of relapsing Sphingomonas paucimobilis peritonitis. Clin Nephrol. 2016;86:287–9.
Yılmaz F, Bora F, Ersoy F. Peritoneal dialysis related peritonitis by Sphingomonas Paucimobilis. Ther Apher Dial. 2018;22:205–6.
Hsueh PR, Teng LJ, Yang PC, Chen YC, Pan HJ, Ho SW, Luh KT. Nosocomial infections caused by Sphingomonas paucimobilis: clinical features and microbiological characteristics. Clin Infect Dis. 1998;26:676–81.
Bayram N, Devrim I, Apa H, Gülfidan G, Türkyılmaz HN, Günay I. Sphingomonas paucimobilis infections in children: 24 case reports. Mediterr J Hematol Infect Dis. 2013;5:e2013040.
Nodaira Y, Ikeda N, Kobayashi K, Watanabe Y, Inoue T, Gen S, Kanno Y, Nakamoto H, Suzuki H. Risk factors and cause of removal of peritoneal dialysis catheter in patients on continuous ambulatory peritoneal dialysis. Adv Perit Dial. 2008;24:65–8.
Oki R, Tsuji S, Hamasaki Y, Komaru Y, Miyamoto Y, Matsuura R, Yamada D, Doi K, Kume H, Nangaku M. Time until treatment initiation is associated with catheter survival in peritoneal dialysis-related peritonitis. Sci Rep. 2021;22:1.
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Contributions
CK, KM, YK, TH and AO participated in discussions of the patient’s case. CK drafted and is responsible for the final version of the manuscript. All authors read and approved the manuscript and agree with its submission to this journal. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This report was written in compliance with the Declaration of Helsinki. For this type of case report, ethics approval is not required.
Consent for publication
Written informed consent was obtained from the patient’s family for the publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kinoshita, C., Matsuda, K., Kawai, Y. et al. A case of Sphingomonas paucimobilis causing peritoneal dialysis-associated peritonitis and review of the literature. Ren Replace Ther 7, 64 (2021). https://doi.org/10.1186/s41100-021-00375-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-021-00375-3