Abstract
Background
Colorectal cancer (CRC) has been ranked as the second most deadly cancer and the third most diagnosed cancer cases for the year 2020. Specifically for Romania, the number of CRC-related deaths in 2019 was estimated at 6307 people, with a standardized mortality rate of 33.8 per 100,000 inhabitants. Although the tumor protein 53 (TP53) gene is intensively studied, there are few data on TP53 mutations in Romanian CRC. Furthermore, since genetic alterations may show geographical differences, our study aimed to analyze the clinical status and TP53 somatic variation in Romanian CRC patients.
Subjects and methods
DNA from 40 randomly selected cases of CRC was extracted from formalin-fixed paraffin-embedded tissues and sequenced using direct Sanger sequencing techniques, and variants were annotated according to the recommendations of the Human Genome Variation Society. Novel variants were analyzed using MutationTaster2021 to predict their effects.
Results
The mean age was 63.6 years (range 33–85 years) with a male to female ratio of 2.3. More than 45% (18/40) had an advanced cancer stage (≥ stage III). Mutations were found in 21/40 cases (52.5%), with one case having two mutations, giving a total of twenty-two mutations in the TP53 coding DNA. These mutations include 3 (13.6%) insertion-deletion mutations, two of which are novel frameshift mutations: c.165delT (in exon 4) and c.928_935dup (in exon 9), both of which are predicted to lead to nonsense-mediated mRNA decay and are classified as deleterious. The remaining 19 (86.36%) were substitution mutations: 1 nonsense and 18 (81.8%) missense mutations, with G > A (n = 7/19; 36.8%) and C > T (n = 6/19; 31.5%) transitions being the most common. The G > T transversion was found in 21.05% (4/19) of the substitution mutations.
Conclusion
We have described two novel frameshift mutations in TP53. The discovery of novel mutations following the efforts of The Cancer Genome Atlas and other large-scale cancer genome sequencing projects may be further evidence of the heterogeneous nature of mutations in cancer and may indicate that the identification of carcinogenic mutations is not yet saturated. Further sequencing is therefore needed, especially in less studied populations. Importantly, consideration of their geographical environment will shed light on population-specific carcinogenesis.
Similar content being viewed by others
Introduction
In the 2020 GLOBOCAN report on cancer statistics, the colorectal cancer (CRC) was ranked as the second most deadly cancer after lung cancer and the third most diagnosed cancer after breast and lung cancer [1]. The incidence of CRC varies widely according to geographical location and socioeconomic status [2, 3]. Incidence rates are approximately four times higher in developed countries than in developing countries [1]. On the other hand, a little variation in mortality rates is observed across different countries because of increased fatality in developing countries [1]. The highest incidence rates for CRC are recorded in European regions, Australia/ New Zealand, and North America. The same trend exists for rectal cancer incidence rates, but the highest rates are found in East Asia [1].
Specifically for Romania, a Southeastern European country, the number of CRC related deaths in 2019 was estimated at 6307 people, with a standardized mortality rate of 33.8 per 100,000 inhabitants [4]. The number of cases is gradually increasing and, due to the lack of screening programs, most cases are still diagnosed at an advanced stage.
Cancer genetics is a key to both prevention and treatment of this deadly disease, but cancer genetics can exhibit geographical differences that may be due to differences in germline variants secondary to founder mutation (s) and/or somatic mutations that are more influenced by environmental carcinogenesis.
The tumor protein 53 (TP53) gene is a key gene in most of human cancers and has been called the “guardian of the genome” due to its role in responding to DNA damage to prevent the spread of damaged DNA [5, 6]. This gene is a tumor suppressor gene, with approximately twelve TP53 isoform proteins currently described [7, 8]. Its proteins act as transcription factors and play many roles in maintaining cell life and integrity, including regulation of cell metabolism, cell cycle, apoptosis, senescence, and DNA damage repair among others [6, 9, 10].
TP53 is among the mostly studied genes [10], and as more studies dig deeper to learn more about it, more knowledge is being discovered, including novel mutations, single nucleotide polymorphisms (SNPs) and their implication in the development, progression and treatment of various diseases [11,12,13,14,15].
Mutations and/or allelic variants in the TP53 gene have been proven to influence carcinogenesis, disease progression and/or response to treatment in several cancers including CRC [12, 13, 16]. The commonest TP53 mutations in different cancers are missense mutations, accounting for approximately 40%, followed by frameshift deletions in 20% and frameshift insertions in 10% [17].
In CRC, the frequency of TP53 mutations ranges from 33 to 60% [16, 18] but there is insufficiency of available data regarding the TP53 mutations in Romanian patients with CRC. Additionally, while dietary and environmental factors have been linked with CRC in humans and animals [19,20,21], recent studies have documented a shift from the typical traditional Romanian diet to other dietary patterns, including a high meat/ high fat and Western patterns [22]. Furthermore, Romanian patients with CRC had a dietary habit linked with a Western style diet [23], and Gavrilaș et al. [23] reported that consumption of processed meat was associated with a sixfold risk (odd ratio of 6, p < 0.001) of developing colon cancer in Romanians.
Given the increasing CRC incidence in Romanians, and the recent change in their diet, our study aimed to analyze the TP53 mutations in Romanian CRC patients. Moreover, novel somatic mutations in understudied populations would expand our knowledge about TP53 mutations and CRC carcinogenesis which may be influenced by the dietary pattern of the population and other environmental factors. Therefore, in this paper, we also describe two novel TP53 frameshift (FS) mutations.
Materials and methods
Patients
Forty patients with histologically confirmed CRC were included in this study. Cases were retrospectively collected among patients who benefited surgical resection for a CRC during 2016/2017. The randomly selected cases were histologically confirmed in the Department of Pathology of Clinical Emergency Hospital of Targu-Mures, Romania. All cases included in this study were naïve for preoperative oncologic therapy and all were microsatellite stable.
DNA extraction
DNA was extracted from formalin-fixed paraffin-embedded (FFPE) tissue blocks using QIAamp® DNA FFPE Tissue Kit (Qiagen GmbH, Qiagen strasse1, 40,724 Hilden, Germany) according to manufacturer’s guidelines. The extracted DNA was quantified using nanodrop® 1000 (ThermoFisher Scientific, Wilmington, CO, USA) spectrophotometer and for all cases 260/280 ratio was between 1.7 and 1.9.
DNA amplification and sequencing
DNA from exons number 2 to 11 of TP53 [24] was amplified using HotStarTaq (Qiagen) and sequenced in the forward and reverse directions by the Sanger sequencing method using the BigDye Terminator Cycle Sequencing Reaction Kit, ver.3.1 and ABI 3130xL Genetic Analyzer (ThermoFisher Scientific) as described by Natsume et al. [25].
Mutation detection, annotation and in silico analysis
DNA sequence data were aligned to TP53 genomic sequence NC_000017.11 (GRCh38.14) on chr17:7668421–7687490 [26] using both UniproUGENE V.35 [27] and GENETYX® software package ver.14.1.0 (Genetyx Corporation, Tokyo, Japan). Known variants were annotated using dbSNP (build 156) database and following the Human Genome Variation Society (HGVS)’ recommendations. The novel variants were analyzed using MutationTaster2021 [28] in silico tool to predict the consequence of DNA variation. Every detected mutation was confirmed in two independent Sanger sequencing experiments. We only reported new mutations and mutations that are reported to be pathogenic or likely pathogenic or those with MAF < 0.0001 in major databases (ALFA, ClinVar, dbSNP, VariSome, 1000 genome project and TOPMed) (Supplementary Table S1). We did not determine if mutations were purely somatic or germline.
Ethical approval
This study was approved by the Ethics Committee of the University of Medicine and Pharmacy of Targu-Mures, Romania (agreement no 124/28.07.2016) and by the Ethics Committee of Hamamatsu University School of Medicine (EC HUSM number: 20 − 011).
Results
Forty patients with a mean age of 63.6 years [range, 33–85 years] and a male/female ratio of 2.3 were included in the database. More than 45% (18/40) had advanced cancer (≥ stage III). Most cases (31/40) were diagnosed in the distal colon (Table 1). Twenty-one out of 40 cases (52.5%) had a mutation in TP53, and there was only one case with 2 different mutations, making a total of 22 mutations. Of the 22 mutations counted, 18 (81.81%) were in the DNA binding domain, 19 (86.36%) were substitution mutations and 3 (13.6%) were insertion-deletion mutations, two of which are novel mutations to our knowledge.
Two novel frameshift mutations in TP53
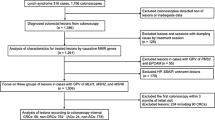
In this study we found two novel frameshift mutations, each occurring once: c.165delT which is located in exon 4 and c.928_935dup which is located in exon 9. Their details are shown in Table 2 and their electropherograms are shown in Fig. 1. The wild-type amino acid sequence of the TP53 protein is 341 in length (with the stop codon at position number 342), the deletion mutation c.165delT introduced a premature stop codon at position number 122, so the mutated amino acid sequence was predicted to result in a truncated protein of only 121 amino acids (the stop amino acid at position 122). The novel frameshift duplication mutation c.928_935dup is predicted to be 47 bp shorter than the normal protein. The 2 novel frameshift mutations are predicted to be deleterious by MutationTaster2021 because the mutated amino acid sequences could lead to nonsense-mediated mRNA decay (NMD) and the corresponding protein features would be affected.
Electropherograms for novel frameshift mutations in Romanian patients with CRC. A: c.165delT mutation, the top graph corresponds to case RC21 with mixed electropherogram (see the right side of highlighted area marked by an arrow) secondary to deletion of T. The middle electropherogram shows the same case after cloning of the corresponding PCR product and this cloning allowed to confirm the deletion of T (at the gap space highlighted by a vertical dark column). The lower graph corresponds to a wild type case (a control case without mutation). B: c.928_935dup mutation, the top electropherogram corresponds to case RC33 with a sequence of 8 bases that is duplicated; marked by a horizontal black line with a star on top and it was obtained after cloning of its PCR product in plasmid. The lower electropherogram corresponds to a wild type case (a control case without mutation)
Other TP53 mutations in our study population of Romanian CRC patients
In addition to the novel mutations described above, we found 17 different types of mutations: 1 deletion mutation in one case and 16 substitution mutations, of which the p.R248Q occurred in 3 cases and p.R273C in 2 cases (Table 3). Because of these recurrent mutations, the total number of substitution mutations was 19, of which only one was a nonsense mutation (p.R342*) occurring once in exon 10. The remaining substitutions were missense mutations. Exons 5 and 6 each had 3 different mutations, and 3 mutations occurred in exon 8 (all at the residue p.R273). Exon 7 was the most frequently mutated with 9 mutations, 4 of them at amino acid position R248 (p.R248Q or p.R248W) and another 5 different mutations at different amino acid residues. Further analysis of the 19 substitution mutations showed that G > A (n = 7/19; 36.8%) and C > T (n = 6/19; 31.5%) transitions were the most frequent. The G > T transversion was found in 21.05% (4/19) of the substitution mutations.
Discussion
TP53 mutations were found in 21 out of 40 cases (52.5%). The reported mutation rates in CRC vary from study to study and they range from 33 to 60% [16, 18]. The difference in mutation rates may be explained by the different methods used to analyze mutation status. Mainly, some studies have analyzed exons 5 to 8 or 5 to 9, while others have analyzed exons 2 to 11, but with other possible range of analysis [17, 31].
Previous studies in CRCs from Romanian patients were reported by Murarasu et al. [32], who described 18 different single nucleotide variants (SNVs) in the coding region of TP53 and 2 SNVs in the intronic region. Only 2 SNVs (NM_000546.6: c.455 C > T and NM_000546.6: c.817 C > T) were identical in both studies. No other reports were found in the literature regarding the spectrum of TP53 mutations in Romanian patients with CRC. Although our study sample was small, the percentage of transition mutations G > A (36.8%) and C > T (31.5%) was close to that reported in the Catalogue Of Somatic Mutations In Cancer (COSMIC): G > A with 41.49% and C > T with 31.73% for large intestine cancer [30,33].
The novel frameshift mutation c.165delT is a mutation with deletion of T. Mutations with deletion of T are described in the COSMIC v97 Mutational Signatures v3.3 under the insertion-deletion (ID) mutational signature ID18 [34]. The ID18 mutation signature is mainly found in CRC and normal colorectal epithelial cells [33,34,35,36]. The proposed etiology for this signature is exposure to colibactin, a genotoxic compound produced by E.coli bacteria bearing pks pathogenicity island [34, 36].
Furthermore, in one of our patients we found a frameshift mutation c.267delC which has been previously reported in ClinVar [37], Medical Genomics Japan Variant Database (MGeND) [38] and in the COSMIC [39] as a germline [37] and as a somatic mutation in various cancers [39]. This is a homopolymer deletion mutation, with four additional equivalent representations and has been predicted to be pathogenic [40, 41]. This frameshift deletion mutation will result in a truncated amino acid sequence of the same length as the novel frameshift deletion mutation (c.165delT) described above. For both of them, the last 33 amino acids sequence were predicted to be identical and their mutated amino acid sequences were predicted to lead to an NMD. From this perspective of some similarity between the two frameshift mutations, we can expect that the novel frameshift mutation c.165delT would also be a potentially disease-causing mutation.
The nonsense mutation c.1024 C > T (p.R342*) leads to a protein truncation of 52 amino acids and is predicted to cause NMD and loss of many protein features. This mutation is reported and interpreted as pathogenic in ClinVar (ID: 182,970) for several conditions (Li- Fraumeni syndrome, ovarian neoplasms, gallbladder cancer, hereditary cancer predisposition syndrome and colonic diverticular disease) [42]. It has been found in both somatic and germline conditions. However, it is not reported in 1000G, ExAC and gnomAD. On the other hand, it is reported in the top 100 cancer driver mutations and accounts for 0.33% of all cancer patients [43].
As stated above, all of our cases with nonsense and frameshift mutations are predicted to lead to NMD. In vivo, NMD has been described as a complex surveillance process [44] with cellular variability in its efficiency [45, 46], and there is a possibility that mRNA with a premature stop codon may still not be degraded via NMD, leading to the expression of a truncated protein [47, 48].
However, it should be noted that since NMD has been predicted by in-silico tools for mutations detected in cancer tissues, therefore we can expect that the tumor tissues may still express the TP53 protein from wild-type transcripts. TP53 protein levels and TP53-mediated transactivation are negatively regulated by mouse double minute 2 (MDM2) [48,49,50,51]. Moreover, previous studies have shown that mutant p53 induces the stabilization of MDM2 [52, 53] and MDM2 amplification has been reported in CRC including in some cases of mutant TP53 CRC [54]. Therefore, we might expect that the level of wild-type TP53 protein would be strongly affected by the corresponding level of MDM2 expression in the same tumor.
Most of the missense SNVs in the TP53 gene are located in hotspot mutation positions. Eighteen out of twenty-two (81.8%) are missense mutations and are all located in the DNA binding domain of the TP53 protein (spanning from position 102–292 amino acids), which is a common occurrence in cancer cells [55]. When considering the top most frequently mutated residues in the TP53 protein, we found that 14/18 (77.7%) of the missense mutations in our study are recorded in the top 50 most frequently mutated residues and 9/18 (50%) are in the top 10 hotspot mutation positions [55]. These hotspot positions are: R248, R273, R249 and G245 with 4, 3, 1 and 1 cases respectively. Murarasu et al. [32] found that mutations in 4 hotspots (R175, G245, R273 and R282) accounted for 48.3% in their study of Romanian CRC cases. Finally, note that all, except three (V203, S215 and G244) of the missense mutations residue in this study are recoded among the top 100 cancer driver mutations of human cancers [43].
The mechanisms by which mutations in the TP53 gene may contribute to cancer pathogenesis and progression have evolved and will continue to evolve over time. For example, Wills et al. [56] found that mutant p53 exerts a dominant-negative effect compared to wild-type by suppressing both the DNA binding ability, the potential to induce cell cycle arrest and the growth suppressive utility of wild-type TP53. Stabilization and accumulation of MDM2 induced by different mutant TP53 cancer cells [52, 53] and amplification of MDM2 in mutant TP53 CRC have been reported. We can hypothesize that there may be a combined effect of the degradation of wild-type TP53 protein by MDM2 and the dominant negative effect of mutant TP53 in favor of cancer development and/or progression. This hypothesis needs to be evaluated using in vitro and in vivo strategies.
Limitations of the study
Our study has some limitations that further research may be able to address. We only analysed tissue samples from patients, without testing family members. Hence, we could not confirm if the mutations were germline or purely somatic. The functional analysis of the protein from cases with novel mutations that we describe in this paper was done using an in silico tool. Therefore, the in vivo or in vitro nature of the TP53 protein should be investigated, as there may be some differences between what is predicted by the computer tools and what might occur under natural conditions in terms of the type and expression level of the TP53 transcripts and protein. Our data are too small to give any insight that the mutations in CRC in Romania may reflect known or unknown specific environmental or dietary exposures, but the accumulation of the mutation spectrum would highlight the risk and the reason for the increase of CRC in Romania in the future. Recently, we observed the difference in TP53 mutation spectrum between Eastern Europe and East Asia [25], and it would be interesting to see the status of TP53 mutation in CRC in East Asia for comparison.
Conclusion
In this study, we found that most of TP53 missense mutations are concentrated in the DNA binding domain, as it has been previously reported. However, we identified two novel frameshift mutations, both of which are predicted to be deleterious/ disease causing mutations and will require further studies to confirm their functional consequences in vivo. Our findings highlight the heterogeneous nature of the mutational status within cancers. The continued discovery of new mutations after the efforts of The Cancer Genome Atlas and other large-scale cancer genome study projects may indicate that the collection of carcinogenic mutations that vary from individual to individual is not yet saturated. Further sequencing is therefore needed, especially in geographical populations that have not yet been studied. We can expect that more new mutations or variants will continue to be discovered, especially in understudied populations, and that consideration of their geographical environment will shed light on population-specific carcinogenesis.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ALFA:
-
Allele frequency aggregator
- COSMIC:
-
Catalogue of somatic mutations in cancer
- CRC:
-
Colorectal cancer
- dbSNP:
-
Database of single nucleotide polymorphism.
- DNA:
-
Deoxyribonucleic acid
- FFPE:
-
Formalin-fixed paraffin-embedded
- FS:
-
Frameshift
- gnomAD:
-
Genome Aggregation Database
- GRCh:
-
Genome Research Consortium human build
- MDM2:
-
Mouse double minute 2 or MDM2 proto-oncogene
- MGeND:
-
Medical Genomics Japan Variant Database
- NMD:
-
Nonsense-mediated mRNA decay
- RNA:
-
Ribo Nucleic Acid
- SNP:
-
Single Nucleotide Polymorphism
- SNV:
-
Single Nucleotide Variant
- TOPMed:
-
Trans-omics for precision medicine
- TP53 :
-
Tumor Protein 53
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Fidler MM, Soerjomataram I, Bray F. A global view on cancer incidence and national levels of the human development index. Int J Cancer. 2016;139:2436–46.
Fidler MM, Bray F, Vaccarella S, Soerjomataram I. Assessing global transitions in human development and colorectal cancer incidence. Int J Cancer. 2017;140:2709–15.
Eurostat. Cancer statistics - specific cancers. Statistics Explained. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Cancer_statistics_-_specific_cancers#Colorectal_cancer. Accessed 19 May 2023.
Brady CA, Jiang D, Mello SS, Johnson TM, Jarvis LA, Kozak MM, et al. Distinct p53 transcriptional programs dictate acute DNA-damage responses and tumor suppression. Cell. 2011;145:571–83.
Kastenhuber ER, Lowe SW. Putting p53 in context. Cell. 2017;170:1062–78.
Khoury MP, Bourdon J-C. The isoforms of the p53 protein. Cold Spring Harb Perspect Biol. 2010;2:a000927.
Anbarasan T, Bourdon J-C. The emerging landscape of p53 isoforms in physiology, cancer and degenerative diseases. Int J Mol Sci. 2019;20:6257.
Levine AJ. p53: 800 million years of evolution and 40 years of discovery. Nat Rev Cancer. 2020;20:471–80.
Levine AJ, Oren M. The first 30 years of p53: growing ever more complex. Nat Rev Cancer. 2009;9:749–58.
Pham T-H, Park H-M, Kim J, Hong JT, Yoon D-Y. STAT3 and p53: dual target for cancer therapy. Biomedicines. 2020;8:637.
Basu S, Barnoud T, Kung C-P, Reiss M, Murphy ME. The african-specific S47 polymorphism of p53 alters chemosensitivity. Cell Cycle. 2016;15:2557–60.
Zhang G, Xu Q, Liu J, Lv Z, Lu Y, Yang H, et al. Five P53 SNPs involved in low rectal cancer risk and prognosis in a chinese population. J Cancer. 2019;10:1772–80.
Suzuki K, Matsubara H. Recent advances in p53 research and cancer treatment. J Biomed Biotechnol. 2011;2011:978312.
Powers J, Pinto EM, Barnoud T, Leung JC, Martynyuk T, Kossenkov AV, et al. A rare TP53 mutation predominant in Ashkenazi Jews confers risk of multiple cancers. Cancer Res. 2020;80:3732–44.
Kandioler D, Mittlböck M, Kappel S, Puhalla H, Herbst F, Langner C, et al. TP53 mutational status and prediction of benefit from adjuvant 5-fluorouracil in stage III colon cancer patients. EBioMedicine. 2015;2:825–30.
Donehower LA, Soussi T, Korkut A, Liu Y, Schultz A, Cardenas M, et al. Integrated analysis of TP53 gene and pathway alterations in the Cancer Genome Atlas. Cell Rep. 2019;28:1370–84.
Murarasu D, Puiu L, Mihalcea C-E, Pitica IMA, Mambet C, Radu EL, et al. Characterization of TP53 polymorphisms in romanian colorectal cancer patients. Rom Biotechnol Lett. 2018;23:14124–34.
Kamiya H, Oikawa S. Life Style and Cancer – The Open Symposium of the Japanese Environmental Mutagen Society (JEMS) in 2015. Genes Environ. 2016;38:8.
Le Marchand L. The role of heterocyclic aromatic amines in colorectal cancer: the evidence from epidemiologic studies. Genes Environ. 2021;43:20.
Hakura A, Koyama N, Seki Y, Sonoda J, Asakura S, o-Aminoazotoluene. 7,12-dimethylbenz[a]anthracene, and N-ethyl-N-nitrosourea, which are mutagenic but not carcinogenic in the colon, rapidly induce colonic tumors in mice with dextran sulfate sodium-induced colitis. Genes Environ. 2022;44:11.
Roman G, Rusu A, Graur M, Creteanu G, Morosanu M, Radulian G, et al. Dietary patterns and their association with obesity: a cross-sectional study. Acta Endocrinol (Buchar). 2019;15:86–95.
Gavrilaş LI, Ionescu C, Bălăcescu O, Revnic C, Ciobârcă D, Filip L, et al. Foods and food groups associated with colorectal cancer: a case-control study. Farmacia. 2018;66:846–52.
Gurzu S, Jung I, Sugimura H, Staden RIS, Yamada H, Natsume H, et al. Maspin subcellular expression in wild-type and mutant TP53 gastric cancers. World J Gastrointest Oncol. 2020;12:741–55.
Natsume H, Szczepaniak K, Yamada H, Iwashita Y, Gędek M, Šuto J, et al. Non-CpG sites preference in G:C > A:T transition of TP53 in gastric cancer of Eastern Europe (Poland, Romania and Hungary) compared to east asian countries (China and Japan). Genes Environ. 2023;45:1.
National Library of Medicine. National Center for Biotechnology Information. Homo sapiens chromosome 17, GRCh38.p14 Primary Assembly. NCBI Reference Sequence: NC_000017.11. https://www.ncbi.nlm.nih.gov/nuccore/NC_000017.11?from=7668421&to=7687490&report=fasta&strand=true. Accessed 15 Apr 2022.
Okonechnikov K, Golosova O, Fursov M, UGENE team. Unipro UGENE: a unified bioinformatics toolkit. Bioinformatics. 2012;28:1166–7.
Steinhaus R, Proft S, Schuelke M, Cooper DN, Schwarz JM, Seelow D. MutationTaster2021. Nucleic Acids Res. 2021;49:W446–51.
Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM, et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 2001;29:308–11.
Tate JG, Bamford S, Jubb HC, Sondka Z, Beare DM, Bindal N, et al. COSMIC: the catalogue of somatic mutations in Cancer. Nucleic Acids Res. 2019;47:D941–7.
Rehman S, Sameer AS, Zahoor L, Abdullah S, Shah ZA, Afroze D, et al. Distinct pattern of mutations of conserved regions of TP53 in colorectal cancer patients in the Kashmir population: an emerging high-risk area. Ecancermedicalscience. 2009;3:129.
Murarasu D, Puiu L, Pitica IMA, Mambet C, Mihalcea CE, Marincas AM, et al. TP53 somatic mutations and LOH profile in colorectal cancer in Romania. Rom Biotechnol Lett. 2018;23:13530–40.
COSMIC. Catalogue Of Somatic Mutations In Cancer. Gene TP53. https://cancer.sanger.ac.uk/cosmic/gene/analysis?coords=bp:AA&sn=large_intestine&wgs=off&samps=1001&preset-sn=large_intestine&id=348585&ln=TP53&start=1&end=394. Accessed 19 May 2023.
Catalogue of Somatic Mutations In Cancer. Mutational Signatures (v3.3-June 2022) ID18.GRCh37.COSMIC v97. https://cancer.sanger.ac.uk/signatures/id/id18/. Accessed 19 May 2023.
Lee-Six H, Olafsson S, Ellis P, Osborne RJ, Sanders MA, Moore L, et al. The landscape of somatic mutation in normal colorectal epithelial cells. Nature. 2019;574:532–7.
Pleguezuelos-Manzano C, Puschhof J, Rosendahl Huber A, van Hoeck A, Wood HM, Nomburg J, et al. Mutational signature in colorectal cancer caused by genotoxic pks + E. coli. Nature. 2020;580:269–73.
National Center for Biotechnology Information. ClinVar; [VCV000156515.2]. https://www.ncbi.nlm.nih.gov/clinvar/variation/156515/. Accessed 19 May 2023.
Medical Genomics Japan Variant Database (MGeND). chr17:7579420:G > Detail (hg19), TP53. (). https://mgend.med.kyoto-u.ac.jp/variant/info/DELETION%7Chg19%7Cchr17:7579420-7579420%7CgG%3E?query=rs587783062. Accessed 15 Apr 2022.
COSMIC. Catalogue of Somatic Mutations in Cancer. Mutation COSV52685476. https://cancer.sanger.ac.uk/cosmic/mutation/overview?id=100539319. Accessed 19 May 2023.
VariSome. chr17-7676102-G- (TP53:p.S90Pfs*33). https://varsome.com/variant/hg38/chr17-7676102-G-?. Accessed 19 May 2023.
Kopanos C, Tsiolkas V, Kouris A, Chapple CE, Aguilera MA, Meyer R et al. VarSome: the human genomic variant search engine. Wren J, editor. Bioinformatics. 2019;35:1978–80.
National Center for Biotechnology Information. ClinVar; [VCV000182970.35]. https://www.ncbi.nlm.nih.gov/clinvar/variation/182970/. Accessed 19 May 2023.
Wang Q. Building personalized cancer therapeutics through multi-omics assays and bacteriophage-eukaryotic cell interactions. Int J Mol Sci. 2021;22:9712.
Bongiorno R, Colombo MP, Lecis D. Deciphering the nonsense-mediated mRNA decay pathway to identify cancer cell vulnerabilities for effective cancer therapy. J Exp Clin Cancer Res. 2021;40:376.
Sato H, Singer RH. Cellular variability of nonsense-mediated mRNA decay. Nat Commun. 2021;12:7203.
Lindeboom RG, Supek F, Lehner B. The rules and impact of nonsense-mediated mRNA decay in human cancers. Nat Genet. 2016;48:1112–8.
Anczuków O, Ware MD, Buisson M, Zetoune AB, Stoppa-Lyonnet D, Sinilnikova OM, et al. Does the nonsense-mediated mRNA decay mechanism prevent the synthesis of truncated BRCA1, CHK2, and p53 proteins? Hum Mutat. 2008;29:65–73.
Supek F, Lehner B, Lindeboom RG. To NMD or not to NMD: nonsense-mediated mRNA decay in cancer and other genetic diseases. Trends Genet. 2021;37:657–68.
Haupt Y, Maya R, Kazaz A, Oren M. Mdm2 promotes the rapid degradation of p53. Nature. 1997;387:296–9.
Kubbutat MH, Jones SN, Vousden KH. Regulation of p53 stability by Mdm2. Nature. 1997;387:299–303.
Momand J, Zambetti GP, Olson DC, George D, Levine AJ. The mdm-2 oncogene product forms a complex with the p53 protein and inhibits p53-mediated transactivation. Cell. 1992;69:1237–45.
Peng Y, Chen L, Li C, Lu W, Agrawal S, Chen J. Stabilization of the MDM2 oncoprotein by mutant p53. J Biol Chem. 2001;276:6874–8.
Yang L, Song T, Cheng Q, Chen L, Chen J. Mutant p53 sequestration of the MDM2 acidic domain inhibits E3 ligase activity. Mol Cell Biol. 2019;39:e00375–18.
Forslund A, Zeng Z, Qin L-X, Rosenberg S, Ndubuisi M, Pincas H, et al. MDM2 gene amplification is correlated to tumor progression but not to the presence of SNP309 or TP53 mutational status in primary colorectal cancers. Mol Cancer Res. 2008;6:205–11.
Baugh EH, Ke H, Levine AJ, Bonneau RA, Chan CS. Why are there hotspot mutations in the TP53 gene in human cancers? Cell Death Differ. 2018;25:154–60.
Willis A, Jung EJ, Wakefield T, Chen X. Mutant p53 exerts a dominant negative effect by preventing wild-type p53 from binding to the promoter of its target genes. Oncogene. 2004;23:2330–8.
Acknowledgements
We are thankful to Ms Shiho Omori for excellent help for preparation of histologic tissue sections. We acknowledge all staff of Advanced Research Facilities & Service of the Preeminent Medical Photonics Education & Research Center, Hamamatsu University School of Medicine. Felix MANIRAKIZA is grateful to Otsuka Toshimi Scholarship Foundation for scholarship support during the time of this research project.
Funding
This study was partially funded by the CNCS – UEFISCDI, Romania, project number PN-III-P4-PCE2021-1113. We would also like to acknowledge financial support from the Japan Society for the Promotion of Science (22H04979), Smoking Research Foundation, and SECOM Science and Technology Foundation.
Author information
Authors and Affiliations
Contributions
HS, HY, YI, SG: Conceptualization, methodology, formal analysis, project administration and supervision. FM: Methodology, data acquisition & analysis and writing original draft. KI, RI and AN: Methodology, data acquisition and analysis. ZK and EO: collection of cases, DNA isolation, follow-up of patients. All authors read, reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of the University of Medicine and Pharmacy of Targu-Mures, Romania (agreement no 124/28.07.2016) and the Ethics Committee of Hamamatsu University School of Medicine (EC HUSM number: 20 − 011). All research related activities were done according to Romanian and Japanese national guidelines and regulations and in accordance to Declaration of Helsinki. According to the Romanian rules, as the cases were retrospectively collected, no signed informed consent from patients was necessary.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Manirakiza, F., Yamada, H., Iwashita, Y. et al. TP53 mutations in Romanian patients with colorectal cancer. Genes and Environ 45, 20 (2023). https://doi.org/10.1186/s41021-023-00277-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41021-023-00277-2