Abstract
Objectives
To investigate the association between radiotherapy (RT) and cardiac biomarkers in women with left-sided breast cancer.
Methods
This prospective observational study recruited patients with stage I-III left-sided breast cancer without coronary heart disease who required adjuvant RT. High-sensitivity troponin I(hsTnI), N-terminal pro-brain natriuretic peptide(NT-proBNP), and high-sensitivity C-reactive protein(hsCRP) levels were measured pre-RT, immediately after RT, and 3 months post-RT. Cardiac-sparing RT techniques were utilized (Field-in-Field IMRT/VMAT ± voluntary deep inspiration breath-hold). Statistical analyses were performed using non-parametric tests and multivariable quantile regression (QR).
Results
One hundred five patients completed the study, with 63 evaluable at three months post-RT. Pre- and post-RT biomarkers showed no significant differences. Median pre-RT and post-RT values were: hsTnI (0.012ng/mL; 0.012ng/mL), hsCRP (3.1 mg/L; 2.8 mg/L), and NT-proBNP (59pg/mL; 45pg/mL). Three months post-RT, hsTnI, hsCRP and NT-proBNP levels also showed no significant differences. Multivariable QR revealed no association between heart Dmean [median(IQR): 2.87 Gy (2.05–3.94)] and post-RT biomarkers. Age and BMI were associated with hsCRP and NT-proBNP, respectively.
Conclusions
hsTnI, NT-proBNP, and hsCRP are not correlated with contemporary low cardiac exposure in left-sided breast cancer patients treated with contemporary RT techniques.
Similar content being viewed by others
Background
Cardiovascular diseases (CVD) in cancer patients are driven by treatment-related risk, which spans therapeutic classes and shares damage mechanisms leading to combined toxicity [1,2,3]. Cardio-oncology guidelines endorse surveillance with blood-based biomarkers (troponins and natriuretic peptides) and cardiac imaging [4]. Troponins are cardiac-specific, but not disease-specific, and natriuretic peptides are associated with heart failure (HF) [5]. Oxidative stress and inflammation induce C-reactive protein secretion, which is associated with poor outcomes in decompensated HF [5]. Association between radiotherapy (RT) and these biomarkers is inconclusive, therefore specific recommendations for radiation-induced cardiac damage are absent [4].
Our primary objectives were to evaluate: (a) the effect of RT on biomarkers reflective of myocardial injury/inflammation [high-sensitivity cardiac troponin I (hsTnI), N-terminal pro brain natriuretic peptide (NT-proBNP) and oxidative stress [high-sensitivity C-reactive protein (hsCRP)], and; (b) the association between mean heart dose (Dmean) and biomarkers.
Methods
Study population
This prospective, single-institution, IRB-approved (Protocol ID: Res/SCM/52/2022/40; IRB Approval ID: IRB-BHR/75/2022) observational study was conducted between June 2022 and July 2023. Women with left-sided breast cancer were eligible. Inclusion criteria were: (a) greater than 18 years with pathological stage I-III disease after either breast conservation surgery or mastectomy; (b) without coronary heart disease (CHD) or CHD risk equivalent; (c) requiring adjuvant RT (42.5 Gy/16Fx, 5 days/week) to whole breast or chest wall with/without elective regional nodal irradiation (sequential lumpectomy boost permitted; 10 Gy in 4Fx), and; (d) normal 2D transthoracic echocardiography prior to starting RT. Chemotherapy (neoadjuvant/adjuvant)(with trastuzumab for Her2-expressing tumors) was permitted. Adjuvant RT was delivered 3–4 weeks after completion of the preceding surgery or chemotherapy.
Study procedures
After obtaining informed consent, demographic, clinical, CVD risk factors, and treatment details were collected. Blood samples were collected pre-RT, immediately after RT completion (median: 0 days, Range: 0–18 days), and three months after RT completion (median: 92 days, IQR: 90–99 days). Since only 30% of patients return for a 3-month review post-RT (internal audit), 3-month biomarker measurement was optional. After accruing 52 patients, the data monitoring committee excluded hsTnI from the panel of tests, as 40 patients had values below the detection limit (0.012 ng/ml) at pre- and post-RT time points.
All patients were assessed for treatment in deep inspiration breath hold (DIBH)(RPM system, Varian Medical Systems, USA) and received RT via Field-in-Field Intensity-Modulated Radiotherapy Technique (FiF IMRT) or Volumetric Modulated Arc Therapy on a 6MV LINAC with daily kV-MV verification (Clinac 2100c, Varian Medical Systems, USA) [6]. Contouring for primary, nodal regions and organs-at-risk was performed as per RTOG 0413 protocol, RTOG consensus recommendations, and RTOG 1005 protocol (NCT01349322), respectively [7, 8]. Mean heart dose (Dmean) was recorded for the whole heart contour using a calculation grid size of 2.5 mm with AAA v15.6 algorithm (Varian Medical Systems, USA).
Biomarker measurements
All assays were performed on the Vitros 5600 platform (QuidelOrtho, USA). The hsCRP assay had a detection limit of 0.26 mg/L, coefficient of variation (CV) of < 8.3% at the 99th percentile with a reference limit of < 5.0 mg/L. The NT-proBNP assay had a measurement range of 11.1–35,000 pg/mL, CV of 11% at the 99th percentile with a reference limit of 125 pg/mL and 450 pg/mL for patients less than or greater than 75 years, respectively. The hsTnI assay had a measurement range of 0.012–80.0 ng/ml, CV of < 8.0% at the 99th percentile with a reference limit of 0.034 ng/mL. Whenever an elevated biomarker was detected, a cardiologist obtained a cardiac history and performed a cardiac examination.
Statistical analysis
The sample size for a relative effect size of 30% with 80% power and alpha = 0.05 with a two-tailed, paired-sample design assuming a normal distribution was 94. Another 15% were added for dropout, resulting in a sample size of 108. Baseline characteristics were reported as median with interquartile range (IQR)(continuous variables) or frequencies and percentages (categorical variables). All biomarkers had non-normal distribution; therefore, the Wilcoxon matched-pairs signed-rank test was used to compare pre- and post-RT levels with tied pairs handled by Pratt’s method [9]. The Friedman test was used to compare biomarkers at pre-, post-RT, and 3-months post-RT. Paired comparisons between time points utilized Dunn’s post-test [10]. Spearman rank correlation was used to assess correlation between biomarkers.
Multivariable quantile regression (QR) was used to test association of biomarkers with predictors without considering interactions [11]. Compared to ordinary least-squares (OLS) regression, QR demonstrates robust performance in non-normal distributions and in the presence of outliers. The Markov chain marginal bootstrap determined the standard error [12]. QR results were compared to OLS regression after log-transformation of biomarkers (Supplemental Materials).
This report complies with the ‘Strengthening the Reporting of Observational Studies in Epidemiology cohort’ guidelines (Supplemental Materials). Statistical analyses were performed using Prism v10 (DotMatics, USA) and R v4.2.3 (R Foundation for Statistical Computing, Austria). Statistical significance was set at p < 0.05 (two-sided).
Results
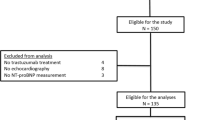
One hundred five patients completed the study and were analyzed for pre-/post-RT comparison, while 63 patients completed the 3-months post-RT evaluation (Fig. 1). Because the data monitoring committee recommended stopping hsTnI testing, 86 patients were analyzable for pre-/post-RT comparison, and 38 were analyzable at all three time points. The patients’ baseline characteristics are presented in Table 1. There was no correlation between markers (Supplemental materials). None of the patients developed a Major Adverse Cardiac Event (MACE) with a median follow-up of 15.0 months (IQR: 12.9–17.3) after the completion of RT. In addition, all patients with elevated biomarkers were asymptomatic on specialist examination, required no additional investigations and completed treatment without interruptions (Supplemental Materials).
Biomarker comparison: Pre- vs. Post-RT (Fig. 2)
The median (IQR) values of hsTnI, hsCRP, and NT-proBNP pre-RT were 0.012 ng/mL (0.012–0.012), 3.1 mg/L (1.5-6.0) and 59 pg/mL (26–116), respectively. The post-RT biomarkers were 0.012 ng/mL (0.012–0.012), 2.8 mg/L (1.6–6.8), and 45 pg/mL (24–101), respectively. The pre-/post-RT comparisons were not significantly different.
Biomarker comparison: Pre-, Post- and 3 months after RT (Fig. 3)
The median (IQR) values of hsTnI, hsCRP, and NT-proBNP pre-RT were 0.012 ng/mL (0.012–0.012), 3.1 mg/L (1.4–6.1) and 56 pg/mL (29–125), respectively. The post-RT levels were 0.012 ng/mL (0.012–0.012), 2.4 mg/L (1.5–6.8), and 50 pg/mL (28–143), respectively. 3-months post-RT, the levels were 0.012 ng/mL (0.012–0.012), 2.7 mg/L (1.1-6.0), and 60 pg/mL (31–151), respectively. Comparisons between pre-, post-, and 3-months post-RT values were not significantly different.
Multivariable median quantile regression: pre- and Post-RT (Table 2)
Multivariable median quantile regression demonstrated no influence of heart Dmean on any post-RT biomarker. No treatment-related factors (anthracycline or anti-Her2 exposure) influenced pre- or post-RT biomarkers. BMI and age were related to hsCRP and NT-proBNP at pre- and post-RT measurements, respectively. hsTnI analysis was not clinically meaningful as the variables had an estimate of < 0.0001 (Supplemental Materials), because the measurements were below the detection threshold. Finally, the results of QR were comparable to OLS regression (Supplemental materials).
Discussion
Identifying measurable markers associated with cardiac radiation exposure may permit MACE risk stratification of patients during follow-up and provide an objective measure to stratify risks with emerging RT techniques. Despite two decades of research, a reliable association has not been established (Table 3) [13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Therefore, this prospective study of predefined, serial time-point biomarker measurements was deliberately designed in a homogeneous low-risk population of patients with left-sided breast cancer who received standardized modern RT to reduce variability, thereby isolating and enhancing the probability of detecting any RT effect. The biomarkers were chosen based on their role in monitoring cardiotoxic therapies and availability in community practice, in contrast to candidate research markers, which require specialized/centralized testing laboratories [25, 26].
Early investigations reported elevation in troponins and natriuretic peptides with RT but were limited by retrospective design or indirect estimates of irradiated heart volume [13, 14]. Subsequent analyses were limited by modest sample sizes and statistical power, precluding conclusive association between RT and biomarkers [15, 17,18,19, 26]. In contrast, this study was adequately powered to detect a 30% change in biomarkers and used rigorous QR and OLS regression strategies with consistent results.
The achieved median heart Dmean (2.87 Gy) demonstrates that exposure can be minimized in the real world, and the threshold for measurable cardiac damage using these biomarkers is clearly above this dose. This is supported by the fact that the majority of reported heart Dmean of individual studies was around 3 Gy (Table 3), without clear association with absolute cardiac biomarker change. Contemporaneous cardiac damage detection will require ultrasensitive biomarkers or long-term studies of cardiac outcomes to establish the magnitude of effect (NCT04361240; NCT04790266; NCT03297346). However, it must be emphasized that the reducing cardiac exposure is adequately achieved with FiF IMRT, which was developed two decades ago and remains the benchmark for comparing newer, more complicated RT techniques [27].
The sample size was designed to be adequate to detect changes in biomarkers, but we acknowledge that it is modest for detecting subtler temporal trends. We intend to follow this cohort biennially for 15 years to record MACE, and perform a post-hoc analysis in the future, if statistically appropriate. We also did not measure these biomarkers pre-chemotherapy because we intended to establish association with RT [4]. Since heart Dmean is the most validated dosimetric parameter for cardiac outcomes, we chose not to investigate association with other sub-structures or parameters thereof, to avoid creating a multiple testing problem [28]. Enrolling right-sided breast cancer patients as controls was considered. But since their risk of developing RT-induced CVD is extremely low, repeated blood investigations were deemed unwarranted by our IRB. Our study population was intentionally composed of patients with low cardiac risk, to isolate the effect of radiotherapy on cardiac markers. It is plausible that patients at higher cardiac risk could demonstrate a more pronounced change in cardiac markers in response to radiotherapy, and could be an avenue for future research.
In conclusion, the lack of correlation between these biomarkers and cardiac radiation exposure will aid in narrowing the scope of future research. These results and prior reports clearly argue against their routine use to detect radiotherapy-induced cardiac injury with modern RT techniques.
Availability of data and materials
This study was performed at Rajiv Gandhi Cancer Institute & Research Centre and is stored in the institutions data repository. The authors do not own these data and hence are not permitted to share them in the original form (only in aggregate form). Reasonable requests for access to data will be considered on an individual basis, by contacting the corresponding author.
References
Lenihan DJ, Cardinale DM. Late cardiac effects of cancer treatment. J Clin Oncol. 2012;30:3657–64.
Zaha VG, Hayek SS, Alexander KM, et al. Future perspectives of cardiovascular biomarker utilization in cancer survivors: a scientific statement from the American Heart Association. Circulation. 2021;144:e551-563.
Lyon AR, López-Fernández T, Couch LS, et al. 2022 ESC guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J. 2022;43:4229–361.
Pudil R, Christian M, Čelutkienė J, et al. Role of serum biomarkers in cancer patients receiving cardiotoxic cancer therapies: a position statement from the Cardio-Oncology Study Group of the Heart Failure Association and the Cardio-Oncology Council of the European Society of Cardiology. Eur J Heart Fail. 2020;22:1966–83.
Xiao H, Xiaojie W, Li S, et al. Advances in biomarkers for detecting early cancer treatment-related cardiac dysfunction. Front Cardiovasc Med. 2021;8:753313.
Ahmad I, Chufal KS, Bhatt CP, et al. Plan quality assessment of modern radiotherapy delivery techniques in left-sided breast cancer: an analysis stratified by target delineation guidelines. BJR Open. 2020;2:20200007.
Jain AK, Vallow LA, Gale AA, et al. Does three-dimensional external beam partial breast irradiation spare lung tissue compared with standard whole breast irradiation? Int J Radiat Oncol Biol Phys. 2009;75:82–8.
Ahmad I, Chufal KS, Miller AA, et al. Risk-adapted target delineation for breast cancer: controversies and considerations. Pract Radiat Oncol. 2023;13:e115-120.
Pratt JW, Gibbons JD. Concepts of nonparametric theory. New York, NY: Springer New York; 1981.
Dunn OJ. Multiple comparisons using rank sums. Technometrics. 1964;6:241–52.
Koenker R. Quantile regression. In: Balakrishnan N, Colton T, Everitt B, et al. editors. Wiley StatsRef: statistics reference online. 1st ed. Wiley; 2014. https://doi.org/10.1002/9781118445112.stat07557.
He X, Hu F. Markov chain marginal bootstrap. J Am Stat Assoc. 2002;97:783–95.
Hughes-Davies L, Sacks D, Rescigno J, et al. Serum cardiac troponin T levels during treatment of early-stage breast cancer. J Clin Oncol. 1995;13:2582–4.
Wondergem J, Erwin GS, Frölich M, et al. Circulating atrial natriuretic peptide plasma levels as a marker for cardiac damage after radiotherapy. Radiother Oncol. 2001;58:295–301.
Erven K, Anca F, Slagmolen P, et al. Subclinical cardiotoxicity detected by strain rate imaging up to 14 months after breast radiation therapy. Int J Radiat Oncol Biol Phys. 2012;85:1172–8.
D’Errico MP, Grimaldi L, Petruzzelli MF, et al. N-Terminal Pro-B–Type natriuretic peptide plasma levels as a potential biomarker for cardiac damage after radiotherapy in patients with left-sided breast cancer. Int J Radiat Oncol Biol Phys. 2012;82:e239-246.
Skyttä T, Touhinen S, Boman E, et al. Troponin T-release associates with cardiac radiation doses during adjuvant left-sided breast cancer radiotherapy. Radiat Oncol. 2015;10:141–141.
D’Errico MP, Petruzzelli MF, Gianicolo EAL, et al. Kinetics of B-type natriuretic peptide plasma levels in patients with left-sided breast cancer treated with radiation therapy: results after one-year follow-up. Int J Radiat Oncol Biol Phys. 2015;91:804–9.
Palumbo I, Barbara P, Fravolini ML, et al. Brain natriuretic peptide as a cardiac marker of transient radiotherapy-related damage in left-sided breast cancer patients: a prospective study. Breast. 2015;25:45–50.
Skyttä T, Tuohinen S, Luukkaala T, et al. Adjuvant radiotherapy-induced cardiac changes among patients with early breast cancer: a three-year follow-up study. Acta Oncol. 2019;58:1250–8.
Demissei BG, Freedman G, Feigenberg SJ, et al. Early changes in cardiovascular biomarkers with contemporary thoracic radiation therapy for breast cancer, lung cancer, and lymphoma. Int J Radiat Oncol Biol Phys. 2019;103:851–60.
Yu AF, Ho AY, Braunstein LZ, et al. Assessment of early radiation-induced changes in left ventricular function by myocardial strain imaging after breast radiation therapy. J Am Soc Echocardiogr. 2019;32:521–8.
Chalubinska-Fendler J, Graczyk L, Piotrowski G, et al. Lipopolysaccharide-binding protein is an early biomarker of cardiac function after radiation therapy for breast cancer. Int J Radiat Oncol Biol Phys. 2019;104:1074–83.
De Sanctis V, Alfo M, Vitiello C, et al. Markers of cardiotoxicity in early breast cancer patients treated with a hypofractionated schedule: a prospective study. Clin Breast Cancer. 2020;21:e141-149.
Aula H, Skyttä T, Tuohinen S, et al. ST2 levels increased and were associated with changes in left ventricular systolic function during a three-year follow-up after adjuvant radiotherapy for breast cancer. Breast. 2020;49:183–6.
Speers C, Murthy VL, Walker EM, et al. Cardiac Magnetic resonance imaging and blood biomarkers for evaluation of radiation-induced cardiotoxicity in patients with breast cancer: results of a phase 2 clinical trial. Int J Radiat Oncol Biol Phys. 2022;112:417–25.
Chufal KS, Ahmad I, Miller AA, et al. A practical and practicable framework for implementing cardiac-sparing radiotherapy techniques in breast cancer. Cancer Res Stat Treat. 2023;6:492–5.
Davey Smith G. Data dredging, bias, or confounding. BMJ. 2002;325:1437–8.
Acknowledgements
We are grateful to Dr Sudhir Rawal, Dr Anurag Mehta, Mr Rajesh Thacker & Mr DS Negi for their encouragement and support.
Prior presentations
The findings of this research were presented in abstract form at: (a) 10th Annual Young Radiation Oncologists Conference, held between 19th to 21st January 2024 at Jodhpur, India, and; (b) 21st Annual Conference of Women's Cancer Initiative - Tata Memorial Hospital, held between 1st to 2nd March 2024 at Mumbai, India.
Funding
The study was funded by Rajiv Gandhi Cancer Institute & Research Centre.
Author information
Authors and Affiliations
Contributions
All authors contributed equally in the design, conception and writing of this manuscript.
Corresponding author
Ethics declarations
Ethics and approval and consent to participate
The authors confirm that they have obtained informed consent from all participants after obtaining Rajiv Gandhi Cancer Institute & Research Centre’s IRB and Ethics Committee approval (IRB Approval ID: IRB-BHR/75/2022).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chufal, K., Ahmad, I., Prakash, A. et al. Cardiac markers in left-sided breast cancer patients receiving adjuvant radiotherapy: a prospective study. Cardio-Oncology 10, 21 (2024). https://doi.org/10.1186/s40959-024-00225-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40959-024-00225-1