Abstract
Background
Precise, submillimeter visualization of retinal microstructures is useful for treatment monitoring of retinoblastoma. Herein, we report the use of hand-held optical coherence tomography (HH-OCT) to document a nearly-invisible retinoblastoma and monitor tumor response to transpupillary thermotherapy (TTT).
Case presentation
A 3-week-old boy was diagnosed with unilateral familial retinoblastoma in the left eye, classified as group B, and treated with intravenous chemoreduction. At 13-month follow-up, the tumor in the left eye was regressed, and evaluation of the right eye revealed a microscopic, nearly invisible tumor measuring 372 µm in thickness and 1.51 mm in basal dimension. The tumor was confirmed on HH-OCT and the diagnosis was changed to bilateral familial retinoblastoma. The new tumor was subsequently treated with TTT and after 1 month, the tumor regressed to an optically dense scar 166 µm in thickness by HH-OCT. Five months after TTT, the scar was clinically flat and measured 73 µm.
Conclusions
HH-OCT has assumed a significant role in the monitoring of retinoblastoma in children. In this case, imaging with HH-OCT allowed precise localization of the tumor and submillimeter monitoring of treatment response following TTT.
Similar content being viewed by others
Background
Optical coherence tomography (OCT) is an imaging technology that utilizes the predictable properties of light refraction to produce precise cross sectional images of the human fundus [1]. Following the popularization of OCT since 1991, OCT technologies including spectral domain OCT (SD-OCT) have allowed for non-invasive, higher-resolution evaluation of retinal and choroidal microstructures. Subsequent technological advancements have given rise to hand-held OCT (HH-OCT), a portable SD-OCT unit, that can be used intra-operatively to image the eyes of children and non-cooperative patients [2]. HH-OCT has proven particularly useful in detection and monitoring of small or “invisible” parafoveal retinoblastomas as well as estimating visual acuity potential in preverbal children [3,4,5].
Herein, we report a 3-week-old boy with familial retinoblastoma who was detected to have a minimally elevated submillimeter tumor, confirmed on HH-OCT. Following treatment, documentation of tumor regression by HH-OCT was important in confirming complete tumor response.
Case presentation
A 3-week-old white male, with a family history of maternal retinoblastoma, presented for clinical evaluation after fetal ultrasound revealed a tumor in the left eye (OS). On examination, visual acuity was fix and follow in each eye and leukocoria OS was noted. Funduscopic evaluation right eye (OD) showed no tumor, whereas fundus evaluation OS (Fig. 1a) revealed a macular retinoblastoma measuring 10.0 mm in basal dimension and 5.0 mm in thickness, classified as group B familial retinoblastoma. The patient received six cycles of intravenous chemoreduction (CRD) using vincristine, etoposide, and carboplatin. Following CRD, the right eye remained normal and the left eye (Fig. 1b) showed type III regression, with partial calcification and regressed tumor measuring 6.0 mm in basal dimension and 2.1 mm in thickness.
Retinoblastoma regression in the left eye after 6 cycles of intravenous chemoreduction. The left eye demonstrated a macular retinoblastoma (a) measuring 10.0 mm in largest basal dimension and 5.0 mm in thickness. After 6 cycles of chemoreduction, the tumor (b) showed regression to 6.0 mm in basal dimension and 2.1 mm in thickness
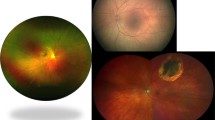
At a 13-month follow-up, a new, minimally elevated parafoveal retinoblastoma measuring 1.51 mm in diameter located 6.0 mm temporal to the foveola OD (Fig. 2a) was detected by indirect ophthalmoscopy. The left eye remained stable with a partially calcified scar. By HH-OCT, the foveola OD was intact and the tiny parafoveal retinoblastoma measured 372 µm in thickness and was without subretinal fluid (Fig. 2b). Ultrasonography confirmed the tiny retinoblastoma OD of 1.5 mm thickness and the regressed calcified retinal scar OS of 2.1 mm thickness.
Retinoblastoma regression documented on hand-held optical coherence tomography (HH-OCT) in the right eye. The initially unaffected right eye (a) demonstrated a small retinoblastoma temporal to the fovea of 1.51 mm in basal dimension and 372 µm in thickness (b). One month following transpupillary thermotherapy (TTT), the tumor (c) showed regression, confirmed as a (d) hyperreflective scar on OCT of 166 µm thickness. At 5 months after TTT, the flat scar (e) measured 73 µm thickness on HH-OCT (f)
The diagnosis was changed to bilateral familial retinoblastoma, and the newly-diagnosed retinoblastoma OD was treated with transpupillary thermotherapy (TTT) using 300 mW power for 4 min with grey-white uptake. One month later, retinoblastoma regression was noted (Fig. 2c) and HH-OCT (Fig. 2d) revealed thickness reduction to 166 µm. Five months after TTT, the scar was clinically flat (Fig. 2e), measuring 73 µm on HH-OCT (Fig. 2f). There were no further tumors.
Discussion
Imaging technologies play a significant role in the detection, diagnosis, and selection of therapeutic options for retinoblastoma. Previously, cross-sectional imaging of retinoblastoma was only possible with ultrasonography, computed tomography, or magnetic resonance imaging. These techniques were only able to detect medium to large retinoblastoma and provide information on tumor configuration, location, size, and extrascleral extension. However, high resolution HH-OCT has recently become available for detection of small retinoblastomas as depicted in Table 1 [3,4,5,6,7,8], and recently even those that are sub-millimeter or nearly clinically invisible, as in this case.
HH-OCT is a portable SD-OCT unit, particularly useful for imaging young children and uncooperative patients. In 2004, Shields et al. [9] reported that time domain OCT was more sensitive than clinical examination in detection and monitoring of a variety of macular pathology in children such as cystoid macular edema and subretinal fluid. Further studies have revealed that HH-OCT is important for monitoring tumor regression [10], detecting subclinical recurrence [6], identifying invisible retinoblastoma [4, 5], and elucidating foveal microanatomy in children following retinoblastoma treatment [11].
Conclusions
Imaging with HH-OCT was helpful in this case as it confirmed tumor presence and allowed for precise, submillimeter monitoring of tumor thickness and regression, with preservation of foveal microanatomy. We encourage all clinicians who manage retinoblastoma to consider the use of HH-OCT for best monitoring of even the tiniest tumors.
Abbreviations
- OD:
-
Right eye
- OS:
-
Left eye
- OCT:
-
Optical coherence tomography
- SD-OCT:
-
Spectral-domain optical coherence tomography
- HH-OCT:
-
Hand-held optical coherence tomography
- CRD:
-
Chemoreduction
- TTT:
-
Transpupillary thermotherapy
References
Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254:1178–81.
Mallipatna A, Vinekar A, Jayadev C, et al. The use of handheld spectral domain optical coherence tomography in pediatric ophthalmology practice: our experience of 975 infants and children. Indian J Ophthalmol. 2015;63:586–93.
Cao C, Markovitz M, Ferenczy S, Shields CL. Hand-held spectral-domain optical coherence tomography of small macular retinoblastoma in infants before and after chemotherapy. J Pediatr Ophthalmol Strabismus. 2014;51:230–4.
Saktanasate J, Vongkulsiri S, Khoo CT. Invisible retinoblastoma. JAMA Ophthalmol. 2015;133:e151123.
Berry JL, David Cobrinik D, Kim JW. Detection and intraretinal localization of an ‘invisible’ retinoblastoma using optical coherence tomography. Ocul Oncol Pathol. 2016;2:148–52.
Park K, Sioufi K, Shields CL. Clinically invisible retinoblastoma recurrence in an infant. Retin Cases Brief Rep. 2017. https://doi.org/10.1097/ICB.0000000000000555 (Epub ahead of print).
Soliman SE, VandenHoven C, MacKeen LD, et al. Optical coherence tomography guided decisions in retinoblastoma management. Ophthalmology. 2017;124:859–72.
Yarovaya V, Sioufi K, Shields CL. Parafoveolar retinoblastoma regression with foveal preservation following intra-arterial chemotherapy documented on hand-held optical coherence tomography in a newborn. Int J Retina Vitreous. 2017;3:43.
Shields CL, Mashayekhi A, Luo CK, et al. Optical coherence tomography in children: analysis of 44 eyes with intraocular tumors and simulating conditions. J Pediatr Ophthalmol Strabismus. 2004;41:338–44.
Shields CL, Manalac J, Das C, et al. Review of spectral domain enhanced depth imaging optical coherence tomography (EDI-OCT) of tumors of the retina and retinal pigment epithelium in children and adults. Indian J Ophthalmol. 2015;63:128–32.
Batrasd A, Pushker N, Venkatesh P, et al. Long-term visual outcomes in intraocular retinoblastoma with eye preservation. Clin Transl Oncol. 2016;18:1034–8.
Authors’ contributions
MM, TS, and CS participated in the design of the study. MM and TS collected data and drafted the manuscript. CS helped draft and finalize the manuscript. All authors read and approved the final manuscript.
Acknowledgements
None.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in this published report.
Consent for publication
Consent for publication has been obtained from the parent or legal guardian of the study patient.
Ethics approval and consent to participate
The present study has been performed in accordance with the Declaration of Helsinki.
Funding
Support provided by the Eye Tumor Research Foundation, Philadelphia, PA (MM, TS, CS). The founders had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review or approval of the manuscript. Carol L. Shields, M.D. has had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
McGarrey, M., Surakiatchanukul, T. & Shields, C.L. Submillimeter retinoblastoma monitoring following transpupillary thermotherapy using hand-held optical coherence tomography. Int J Retin Vitr 4, 9 (2018). https://doi.org/10.1186/s40942-018-0112-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40942-018-0112-4