Abstract
Background
Orthodontic and surgical technical advances in recent years have resulted in treatment opportunities for a whole range of craniofacial skeletal disorders either in the adolescent or adult patient. In the growing child, these can include myofunctional orthodontic appliance therapy or distraction osteogenesis procedures, while in the adult, the mainstay approach revolves around orthognathic surgery.
The literature agrees that for a change in craniofacial morphology to remain stable, the muscles acting upon the facial skeleton must be capable of adaptation in their structure and, therefore, their function. Failure of the muscles to adapt to the change in their length or orientation will place undesirable forces on the muscle attachments leading to potential instability of the skeleton. Adaptation can occur through various processes including those within the neuromuscular feedback mechanism, through changes within muscle structure or through altered muscle physiology, and through changes at the muscle/bone interface.
It is now accepted that because there is no single method of assessing masticatory function, several measures should be taken, and whenever possible, simultaneously.
Methods
This investigation was designed to apply several, newly developed and more sophisticated methods of measuring muscle structure and function to a situation where adaptation of muscle is pivotal to the success of a therapeutic approach. Patients attending the combined orthodontic/orthognathic surgery clinic at the Clitrofa – Centro Médico, Dentário e Cirúrgico, in Trofa, Portugal, were screened. Ten patients scheduled for a bimaxillary osteotomy involving a combination of maxillary Le Fort I impaction procedure coupled with a sagittal split advancement of the mandible were selected to form the study group.
The patients have MRI of the masseter muscle to evaluate the masseter muscle volume and fibre orientation changes. This exam was taken before surgery (T0), 6 to 12 months after surgery (T1), and 3 years after surgery (T2), by two independent observers, according to the protocol jointly developed between the Eastman Dental Institute – University of London and the MRI Centre - Department of Radiology at John Radcliffe Hospital – University of Oxford.
Results
Significant differences (p < 0.05) have been identified between Time 0 (pre-op) and Time 1 (6–12 months post-op) regarding the masseter area (mm2). The differences against Time 0 (pre-op) seem to disappear at Time 2 (3 years post-op).
Conclusions
MRI therefore seems to be a valid tool for measuring differences in the masseter muscle area and volume associated with high-severity occlusal deformities, although showing not to be as efficient in detecting the same differences in cases of low-severity occlusal deformities.
Similar content being viewed by others
Background
Changes in masticatory musculature structure and function may be either developmental, as seen in anomalies of vertical facial form, or adaptative, as seen during procedures such as orthognathic surgery and functional appliance orthodontic therapy [1, 2].
The principal goals of orthognathic surgery are the improvement of occlusal relationships, facial esthetics, and function of the masticatory system in patients with dentoskeletal deformities [3, 4].
The results of some studies indicate that patients scheduled for orthognathic surgery will tend to have lower mastication forces than controls [5, 6]. The lower forces in patients, however, do not seem to be the result of lower efficiency in the jaw muscles. Instead, the results of this study suggest that patients, prior to treatment, may experience differences in sensory feedback or have lower motivation to generate large forces [7].
Advances in medical imaging have created ever increasing volumes of complex data obtained from the patient. The interpretation of such information has become a specialty in itself and the surgeon at times may be left bewildered as to how best to apply the available information to the practicalities of physical intervention. The surgeon seeks to understand the exact morphology of the abnormality, its relationships to surrounding anatomy, and the best way to access and correct the pathology operatively. Such specific information is not readily available in the radiologist’s report and however experienced the surgeon may be at interpreting images such questions often cannot be easily answered [8].
Three-dimensional (3D) imaging has been developed to narrow the communication gap between radiologist and surgeon. By using 3D imaging, a vast number of complex slice images can be quickly appreciated. The term “three-dimensional”, however, is not a truly accurate description of these images as they are still displayed on a radiological film or flat screen in only two dimensions. The advent of 3D imaging has not only improved data display but also promoted the development of even more useful technologies to assist the surgeon in diagnosis and planning [8].
Masseter muscle architecture
The average length of masseter muscle three-layer fibres is 19–30 mm; those in the posterior region are about 35% shorter than those in more anterior. This difference in length is almost certainly related to the need for differential fibre shortening during function, but it is not accounted for entirely by the relative sizes of the respective fibre lever arms measured from the jaw’s function “center” of rotation, and it suggests that fibre tensions may be greater anteriorly than posteriorly as different opening movements are made during function. The masseter also contains at least five intramuscular aponeuroses, some of which descend from the zygomatic arch and interweave with others ascending from the ramus. Fibres pass obliquely between them. These flat tendon sheets can be visualized by magnetic resonance imaging (MRI) in living subjects, and their orientation varies. The motor unit territories are very small in the masseter, and the fibres from each unit tend to remain in close proximity. Differential activation of muscle fibres occurs in various regions of the masseter, causing various fibre collections in the masseter’s mediolateral layers, or between tendon sheets, to contract differentially according to the task. There is probably considerable mechanical diversity within a given muscle and, since each muscle’s structural elements vary from person to person, also equal mechanical diversity between individuals [9].
It is difficult to predict what actually happens internally when the masseter contracts. Depending upon a subject’s morphological type, the task being attempted, and the highly individual contraction strategy used, various groups of muscle fibres will contract and shorten isovolumetrically. As they do so, they thicken, and their transverse diameters will increase. There will be regional changes in muscle thickness, presumably shaped by the relative balance between mutually-contracting fibre groups, thick, layered tendons near the zygomatic arch, and the extent to which tendon sheets move within the muscle. Localized distortion of tendon sheets is possible, and it is likely that regional tensions will be produced at muscle-tendon interfaces, while the net effect may be qualitatively similar between two individuals [10].
To complicate matters, the effects of these changing physical events are themselves uncertain. Different degrees of local intramuscular compression probably alter regional blood flow within the muscle, but presently, there is no evidence describing specifically how vascular physiology in the masseter or any other human jaw muscle is affected selectively by local changes in its physical environment. Apart from any effect on the vascular bed, the production of differential, excessive internal muscle tension, if it follows the same pattern as it does elsewhere in the musculoskeletal system, can lead to local tissue injury. If so, it most probably will occur within the muscle fibres at a short distance from the muscle-tendon interface rather than at the interface itself. Finally, any excessive loading of tendons per se can result in persistent, local inflammation as is commonly found in other skeletal muscles. Any of these hypothetical events would cause biochemical changes in the masseter. The changes would be local and include the release of algesic chemicals [11].
Magnetic resonance imaging
MRI is a non-invasive imaging technique that is one of the most promising and leading imaging modalities for the diagnosis of diseases and other conditions in the head and neck region [12]. A major advantage of MRI over conventional X-ray imaging is the high soft tissue contrast, which allows much better visualization of specific anatomical structures (e.g. nerves, blood vessels) using magnetic fields without exposing patients to ionizing radiation [12]. Despite the limitations in hard tissue imaging, MRI has advanced rapidly over the past two decades with various technical innovations and advanced imaging protocols, offering a wide range of new diagnostic capabilities in dentistry [12, 13].
MRI scans provide the best definition of facial muscles when segmented from DICOMs [13, 14]. Previous works on facial tissue characterization have demonstrated that different areas of facial soft tissues have different biomechanical properties in terms of longitudinal tissue stiffness (Young’s modulus–E) and transverse behavior (Poisson’s ratio–ν) [13, 14].
The residual limitations of MRI in the oral cavity are susceptibility to motion artifacts, complex anatomic courses of small-sized blood vessels and nerves, and image distortion and artifacts due to magnetic field inhomogeneities caused by metallic dental restorations [13].
A customised software programme has been developed at John Radcliffe Hospital - Oxford University which enables the reconstruction of 3D images allowing measurement of muscle volume and area with a high level of accuracy.
To date, this technology had only been applied to tongue muscles, and when applied to the muscles of mastication, the resolution and results were disappointing.
The goal was to develop the system and software to produce accurate and reproducible data for masticatory muscles which not only provided data for muscle area and volume, but also was of sufficient detail to enable analysis of muscle fibre orientation in particular of masseter muscle.
The masseter muscle displays a penniform structure typically characterized by the presence of alternating muscular/aponeurotic layers. The anatomical sections and the MRI section in the same plane allowed the appearance of the intra-muscular aponeurotic layers on the MRI to be defined [15].
Methods
Research design
The present study is an observational prospective study with quantitative methodology.
Sample
A study group of 10 patients attending the combined orthodontic/orthognathic surgery clinic at the Clitrofa – Centro Médico, Dentário e Cirúrgico, in Trofa, Portugal, were selected for the present study by a convenience non-probability sampling method. All the selected patients present skeletal class III malocclusion characterized by a concave facial profile with lower lip protrusion or upper lip retrusion or a combination of the two. The most consistent characteristics of skeletal class III malocclusion seem to be the dental Angle’s class III canines and molars, the presence of anterior cross-bite, and retroclined mandibular incisors.
During the sequential MRI image period, all patients received ear protectors and were instructed to maintain a relaxed muscle posture and closed jaw position (maximal intercuspal position of the lower jaw).
The patients scheduled for a bimaxillary osteotomy involving a combination of maxillary Le Fort I impaction procedure coupled with a sagittal split advancement of the mandible were selected to form the study group. Vertical moves of 2 mm for minor, 4 mm for intermediate, and 6 mm for major impactions are appropriate for all cases. These three categories also simplify the decision-making process. Before surgery, all patients signed their informed consent form.
The inclusion criteria are as follows: All patients presenting at joint orthodontic/orthognathic clinic purposed to orthognathic surgery and that accept the treatment. Diabetic patients were included but noted.
The exclusion criteria are as follows: Patients who gave a history of myopathies, endocrine disorders, connective tissue disorders, autoimmune diseases, bone disease, bleeding disorders, and regular use of prescribed drugs were excluded from the study.
Osteotomies were performed using piezoelectric surgery that is based on the use of ultrasound. It offers precise bone cuts without damaging any soft tissue, minimizing the invasiveness of surgical procedure, and the opportunity of working in a field which is almost totally blood-free. It reduces the impact on soft tissues (vessels and nerves) which lie adjacent to the areas of treatment.
Maxillomandibular fixation (MMF) was performed with surgical archwire fixation, L-shaped osteosynthesis plates, and self-tapping screws. Postoperative orthodontic treatment lasted an average of 6 months. The final occlusion should provide unhindered closure in centric relation, smooth-sliding lateral and protrusive movements, and an optimal bilateral vertical contact dimension.
Data collection instruments
The anatomical and functional heterogeneities of the masseter muscle may influence the spatial differences in muscle thickness. For the sake of systematization and reduction of variables, it was decided to use only the left masseter muscle.
MRI technique was used to measure masseter muscle volume and fibre orientation changes in the selected patients. This evaluation was taken before surgery (T0), 6 to 12 months after surgery (T1), and 3 years after surgery (T2), by two independent observers, according to the protocol jointly developed between the Eastman Dental Institute – University of London and the MRI Centre - Department of Radiology at John Radcliffe Hospital – University of Oxford. It should be considered that during the different evaluation periods, the patients’ occlusion changed, namely, T0-skeletal class III, T1-skeletal class I, and T2-skeletal class I.
Anatomics™ software
The Anatomics™ Rx software is a 3D DICOM viewer and allows to view CT and MRI scan data in both slice format and fully interactive 3D. Anatomics™ can convert 3D images to the STL format for rapid prototyping, or as a bridge from medical imaging to computer-aided design (CAD). A good quality 3D scan is required to create an accurate biomodel or implant.
To standardize the scanning process, a scanning protocol was developed and applied that describes the preferred imaging parameters and provides the imaging technician with an area to note specifics. The patient must remain completely still during the scan; if the patient moves during the scan, it will need to be repeated. Only the original fine-slice data must be used in the software, reformats will not be accepted. Fine overlapping slices must be used, the thickness of 1 mm (or nearest to) and a spacing of 0.8 mm.
The objective was to extract the muscle from the image (margins identification, extract the muscle considering the 3 planes of space, calculation of area and volume). The software allows the correction of limits at any time which gives the observer the capacity to double-check all the processes.
During this study, the MRI machine used was a Sigma MR/I Twinspeed from GE Medical Systems; after several attempts, the software was further developed to produce slices through the muscle at 1-mm intervals rather than 2 mm; the scanning time was about 7 min.
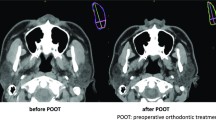
The first masseter muscle 3D image reconstruction was acceptable in terms of definition, area, and volume but with a lack of detail in terms of muscle fibre visualization and orientation (Fig. 1). Increasing the scanning time from 5 to 7 min and changing the muscle slices to 1-mm intervals was possible for the acquisition of more muscle details. As a consequence, the resolution of the muscles was greatly enhanced, and the final masseter muscle 3D image reconstruction permits a good visualization of muscle fibres and their orientation (Fig. 2). This type of reconstruction has also allowed visualization of the muscle’s bony attachments and enabled the measurement of potential changes in orientation in relation to a static landmark unaffected by surgery (e.g. Frankfort plane) or in relation to functional identifiers (e.g. occlusal plane).
Experimental procedure
The experimental design used for this work is depicted in Fig. 3 and involves two different studies: Study A, which investigates the effect of examiner change on the measurement of left masseter muscle area (mm2) and left masseter muscle volume (mm3) of ten different patients by two independent observers; and Study B, which investigates the variation of left masseter muscle area (mm2) and left masseter muscle volume (mm3) in three different times: before surgery (T0), 6 to 12 months after surgery (T1), and 3 years after surgery (T2).
Study A—Effect of examiner (F or C) change on the measurement of left masseter muscle area (mm2) and left masseter muscle volume (mm3) of ten selected patients
Research question: Are there any significant statistical differences between examiners F and C regarding the measurement of mean left masseter area (mm2) and left masseter volume (mm3) of ten patients by MRI?
-
H0: There are no significant statistical differences between examiners F and C regarding the measurement of mean left masseter area (mm2) and left masseter volume (mm3) of ten patients by MRI.
-
H1: There are significant statistical differences between examiners F and C regarding the measurement of mean left masseter area (mm2) and left masseter volume (mm3) of ten patients by MRI.
Study B—Effect of time (Time 0, pre-op versus Time 1, 6–12 months post-op versus Time 2, 3 years post-op) on the left masseter muscle area (mm2) and left masseter muscle volume (mm3) of ten selected patients
Research question(s): Are there any differences between the left masseter muscle area (mm2) and left masseter muscle volume (mm3) of the ten selected patients over time (Time 0, pre-op; Time 1, 6–12 months post-op; and Time 2, 3 years post-op).
-
H0: There are no differences between the left masseter muscle area (mm2) and left masseter muscle volume (mm3) of the ten selected patients over time (Time 0, pre-op; Time 1, 6–12 months post-op; and Time 2, 3 years post-op).
-
H1: There are differences between the left masseter muscle area (mm2) and left masseter muscle volume (mm3) of the ten selected patients over time (Time 0, pre-op; Time 1, 6–12 months post-op; and Time 2, 3 years post-op).
Statistical analysis
IBM® SPSS® version 25 was used to analyze the data obtained in the present work. The data were first tested to ensure they conformed to a normal distribution by using Kolmogorov-Smirnov test. The data were then tested to ensure they complied with variance homogeneity by using the Levene test.
Descriptive statistics measures included the arithmetic mean (x ̅) and standard deviation (SD) if the data were normally distributed and the variance was constant. Where the data were not normally distributed nor the variance was constant, the median and the inter-quartile range (IQR) were noted.
Where the requirements for parametric statistical analysis were met, inferential analysis of examiner comparison in Study A involved the use of paired two-tailed Student’s t-test. In the same conditions, the inferential analysis of times comparison in Study B involved the use of one-way analysis of variance (ANOVA).
Where the requirements for parametric statistical analysis were not met, inferential analysis of examiner comparison in Study A involved the use of the Wilcoxon signed rank (U) test for paired data. In the same conditions, inferential analysis of times comparison in Study B involved the use of the Kruskal-Wallis (H) test.
Where statistically significant differences were found by one-way ANOVA test, the multiple-comparison post hoc Bonferroni test was performed to identify the pairs of categories where the statistically significant differences were located.
The minimum level of significance (α level) accepted throughout the development studies was 0.05 (*), considered to be moderately significant. Levels of 0.01 (**) were considered significant and 0.001 (***) was designated as highly significant. A lack of statistical significance was designated as ns.
Results
In order to make the presentation of results easier to understand, they were subdivided into two items: effect of examiner selection and effect of time. Because one-way ANOVA only gives information about the presence of differences, not specifying where these differences are located, a post hoc Bonferroni test was used to perform pairwise comparison regarding the time points.
Study A—Effect of examiner (F or C) change on the measurement of left masseter muscle area (mm2) and left masseter muscle volume (mm3) of ten selected patients
The following Table 1 presents the mean left masseter areas (mm2) and mean left masseter volumes (mm3) of ten selected patients measured by two independent examiners (F and C).
The statistical comparison between examiners F and C regarding the measurement of mean left masseter area (mm2) and mean left masseter volume (mm3) of ten patients by MRI was performed using a paired Student’s t-test, and the results are presented in the following Table 2.
Study B—Effect of time (Time 0, pre-op versus Time 1, 6–12 months post-op versus Time 2, 3 years post-op) on the left masseter muscle area (mm2) and left masseter muscle volume (mm3) of ten selected patients
The following Table 3 presents the variation of mean left masseter area (mm2) and mean left masseter volume (mm3) of ten selected patients over time (Time 0, pre-op; Time 1, 6–12 months post-op; and Time 2, 3 years post-op).
The statistical comparison between the three time points (Time 0, pre-op; Time 1, 6–12 months post-op; and Time 2, 3 years post-op) regarding the left masseter muscle area (mm2) and left masseter muscle volume (mm3) by MRI of the ten selected patients was performed using a one-way ANOVA test, and the results are presented in the following Table 4.
Post hoc Bonferroni test
Study A: The results show no significant statistical differences between examiner F and examiner C regarding the measurement of the left masseter area (mm2) and left masseter volume (mm3) of the ten selected patients through MRI, when the measurement is made in the same experimental conditions (p > 0.05).
In view of these results, the change of examiner is not a factor that influences the measurement of left masseter area (mm2) and left masseter volume (mm3).
Study B: The results show significant differences in the left masseter muscle area (mm2) over time (p-value = 0.017), although these differences have not been identified regarding the left masseter muscle volume (mm3) (p-value > 0.05).
Because one-way ANOVA only gives information about the presence of differences, not specifying where these differences are located, a post hoc Bonferroni test was used to perform pairwise comparison regarding the time points regarding the left masseter muscle area (mm2) of the ten selected patients, and these results are represented in the following Table 5.
Discussion
Altered muscle function is implicated in the aetiology of vertical facial deformities. The contractile properties of muscle are largely determined by a number of different isoforms of myosin heavy chain (MyHC), and the pattern of MyHC gene expression is one measure of the phenotype and functional potential of a muscle [16].
Two extremes of vertical facial form have been described, long face syndrome and short face syndrome [17]. The long face syndrome (LFS) is characterized by the clinical and radiographic features of increased lower anterior face height, increased maxillary/mandibular plane angle, increased gonial angle, and tendency to anterior open bite. The short face syndrome (SFS) exhibits the reverse of these features. The differences between the two syndromes reflect their divergent growth patterns, where LFS subjects exhibit a downward and posterior growth rotation of the mandible, and SFS subjects exhibit an anterior growth rotation [18]. A significant proportion of the patients presenting with extreme vertical facial discrepancies require surgery to correct their jaw relationship [19, 20].
It has been proposed that the muscles of mastication are important determinants of vertical facial growth [21]. Studies of masseter muscle function have shown significant differences between LFS and SFS subjects with respect to electromyographic (EMG) activity and the magnitude of maximum voluntary bite force; SFS subjects demonstrate higher EMG activity and exert greater bite forces than LFS subjects [22], whether the observed differences in muscle function are primary causal factors or are secondary to the development of vertical facial form [23]. Furthermore, changes in vertical facial form have been induced by either increasing or decreasing the normal activity of the elevator muscles during postnatal growth [21, 24].
The molecular motors of muscle are the myosin heavy chains (MyHC) located in the myofibrillar apparatus of muscle fibres [25]. Muscle fibres are the functional, contractile components of muscle, and the physiological properties of these fibres are largely determined by a number of different MyHC isoforms variously distributed between fibres with different contractile properties [25].
The masseter differs from somatic skeletal muscle in the range of MyHC isoforms expressed in the adult muscle [26]. The myosin heavy chains are encoded by a multigene family, and the major adult isoforms expressed in human skeletal muscle are the slow or ß-cardiac, IIa, and IIx MyHCs that are expressed in the type I, type IIa, and type IIb fibres, respectively [25]. A human homologue to the IIb MyHC isoform described in the rat and other species has yet to be identified [27]. Additionally, the adult human masseter expresses embryonic, perinatal, and α-cardiac MyHCs [28].
The few studies of the distribution of fibre type in the muscles of subjects with extremes of vertical facial form suggest that the contribution of different fibre components to the masseter phenotype overall may vary between normal subjects and those with vertical facial deformity (VFD). Comparisons of the fibre-type distribution and cross-sectional areas in biopsies of the anterior deep masseter have revealed a reduced contribution of type II fibres to the total percentage cross-sectional area in LFS subjects [29]. However, the masseters of SFS subjects have demonstrated either no differences from a control group or an increased type II fibre contribution in the same region of the muscle [29].
The differential increase in anterior and posterior face heights produced at surgery may not only stretch the muscle attachments but also change the orientation of the muscle fibres to the occlusal plane. Adaptation would be necessary with regard to the resting length and also in relation to altered functional activity. It has been noted that such adaptation may occur up to 12 months following surgery [30]. In a study of Hunt and Cunningham [30], surgical alteration of the vertical facial heights was accompanied by an immediate adaptation of the clinical freeway space, presumably mediated through the proprioceptive system. The physiological rest position can be identified by eliminating the sensorimotor feedback from the teeth, so allowing the mandible to adopt a posture dependent upon the resting length of the elevator muscles is partially adapted to the skeletal change immediately following operation, but continued to adapt up to 12 months post-surgery, especially in the vertical excess patients [30].
Any increase in posterior vertical facial dimension is prone to relapse in the long term. At least three possibilities exist as to how this may occur. Firstly, stretching of the pterygo-masseteric sling could lead to increased pressure at the osteotomy site with subsequent bone resorption and loss of vertical dimension. Secondly, in an attempt to maintain an efficient muscular system, both at rest and during function, muscle adaptation could occur through migration of the attachments in preference to increasing the number of sarcomeres. As a consequence, the area of bone devoid of attachment could remodel or resorb thereby reducing the vertical height. Thirdly, a combination of these two hypotheses could exist [30].
The architecture of the masseter muscle has been studied for a long time, but the lack of clinical applications led to descriptions which were often global or contradictory, giving the muscle sometimes two bundles sometimes three. The successive studies of Gaspard [31,32,33], Yoshikawa [34, 35], and Gaudy [36] allowed the definition of the arrangement of the muscular aponeurotic layers making up the human masseter muscle. Unger [37] affirmed the value of magnetic resonance imaging in the oro-facial field for the study of the musculature of the tongue and the walls of the oral cavity, but gave only very general information on the masticatory muscles [38].
Several studies investigated the changes in the size and masticatory force of the masticatory muscles after orthognathic surgery. Katsumata et al. indicated that in mandibular prognathism, the cross-sectional area of the masses decreases after 3 months of mandibular setback but shows a tendency to return to normal after 1 year [39]. In addition, Ueki et al. reported that there are no significant differences in the cross-sectional area of the masseter in mandibular prognathism 1 year after SSRO in comparison with the preoperative area [40]. Trawitzki et al. also reported that when mandibular setback was conducted on patients with a class III dentofacial deformity, the thickness of the masseter muscle increased [41]. The study of Kanga et al. showed that the volume-to-length ratio of the masseter and lateral pterygoid muscles at 1 year after the mandibular setback did not show a significant difference compared with the preoperative value [42].
In a study with 30 skeletal class III patients with dentofacial deformities, 17 were treated by sagittal split ramus osteotomy with rigid osteosynthesis, and 13 were treated by intraoral vertical ramus osteotomy without osteosynthesis; Katsumata et al. reported that masseter muscle crosssectional area was lower in the group who underwent sagittal split ramus osteotomy and intraoral vertical ramus osteotomy. The evaluation was done using three-dimensional CT imaging [39].
Kikuta et al. reported that occlusal force was decreased 3 months after orthognathic surgery, but increased 6 months after the surgery [43]. The results of this study suggest that particular attention should be paid to masseter muscle atrophy in patients with worse open bite after preoperative orthodontic treatment and in those with maxillary undergrowth. However, it is not clear if masticatory ability would be compromised by masseter muscle atrophy immediately after the surgery.
Decreased maximum occlusal force in patients with open bite has been reported, which supports results that increased open bite led to decreased masseter muscle cross-sectional area [44, 45].
Conclusions
A number of studies have reported increased bite force, occlusal contact area, and EMG activity and improved masticatory efficiency after surgery; however, the reason for this improvement is unclear [7]. Previous studies reported that the postoperative improvements in muscular activity were due to better occlusal stability and not to surgically induced biomechanical advantages [46, 47]. The importance of occlusion for the neuromuscular equilibrium and dental supports was investigated in patients undergoing orthognathic surgery. Changes in muscle size; increased occlusal contact area providing greater dental support; sensitivity of teeth, muscles, and the temporomandibular joints; and even the patients’ willingness to exert maximum effort have been suggested as factors in determining the occlusal force after surgery [7].
The continuous changes in masseter muscle size in our study indicate that not only was the skeletal environment altered by surgery, but additional adaptation to new stomatognathic environments also occurred over time with improved occlusion and masticatory activity by orthodontic treatments.
Significant differences (p < 0.05) have been identified between Time 0 (pre-op) and Time 1 (6–12 months post-op) regarding the mean left masseter area (mm2).
It is interesting to notice, however, that the differences against Time 0 (pre-op) seem to disappear at Time 2 (3 years post-op), which may reveal the long-term decrease in the area of mean left masseter area (mm2) or relapse.
An adequate sample makes the investigation more efficient: the data generated is reliable, and the investment of resources is as limited as possible, while at the same time complying with ethical principles. The use of the sampling design directly influences the research results. The sample of 10 patients reveals that this is an uncommon type of surgery, carried out in the vast majority of cases in private health services and requiring the patient’s economic power.
MRI therefore seems to be a valid tool for measuring differences in the masseter muscle area and volume associated with high-severity occlusal deformities (maxillary Le Fort I impaction of 6 mm), although showing not to be as efficient in detecting the same differences in cases of low-severity occlusal deformities (maxillary Le Fort I impaction of 2 mm for minor and 4 mm for intermediate cases).
Future studies comprising larger samples of patients and other different methods of measuring changes in masticatory muscle structure and function are currently being equated to measure the efficacy of orthognathic surgery.
Availability of data and materials
Please contact the author for data requests.
Abbreviations
- 3D:
-
Three-dimensional
- MRI:
-
Magnetic resonance imaging
- MyHC:
-
Myosin heavy chain
- VFD:
-
Vertical facial deformity
- CAD:
-
Computer-aided design
- SD:
-
Standard deviation
- IQR:
-
Inter-quartile range
References
Singh A, Nelson-Moon ZL, Thomas GJ, Hunt NP, Lewis MP (2000) Identification of matrix metalloproteinases and their tissue inhibitors type 1 and 2 in human masseter muscle. Arch Oral Biol 45(6):431–440. https://doi.org/10.1016/s0003-9969(00)00020-0. PMID: 10775672
Pan Y, Chen S, Shen L, Pei Y, Zhang Y, Xu T (2020) Thickness change of masseter muscles and the surrounding soft tissues in female patients during orthodontic treatment: a retrospective study. BMC Oral Health 20(1):181. https://doi.org/10.1186/s12903-020-01168-6. PMID: 32600308; PMCID: PMC7325017
Youssef RE, Throckmorton GS, Ellis E 3rd, Sinn DP (1997) Comparison of habitual masticatory cycles and muscle activity before and after orthognathic surgery. J Oral Maxillofac Surg 55(7):699–707; discussion 707-8. https://doi.org/10.1016/s0278-2391(97)90581-4. PMID: 9216502
Coclici A, Hedeşiu M, Bran S, Băciuţ M, Dinu C, Rotaru H, Roman R (2019) Early and long-term changes in the muscles of the mandible following orthognathic surgery. Clin Oral Investig 23(9):3437–3444. https://doi.org/10.1007/s00784-019-03019-3. Epub 2019 Jul 27. PMID: 31352516
Tate GS, Throckmorton GS, Ellis E 3rd, Sinn DP (1994) Masticatory performance, muscle activity, and occlusal force in preorthognathic surgery patients. J Oral Maxillofac Surg 52(5):476–81; discussion 482. https://doi.org/10.1016/0278-2391(94)90344-1. PMID: 8169710
Tate GS, Throckmorton GS, Ellis E 3rd, Sinn DP, Blackwood DJ (1994) Estimated masticatory forces in patients before orthognathic surgery. J Oral Maxillofac Surg 52(2):130–6; discussion 136-7. https://doi.org/10.1016/0278-2391(94)90393-x. PMID: 8295046
Lee DH, Yu HS (2012) Masseter muscle changes following orthognathic surgery: a long-term three-dimensional computed tomography follow-up. Angle Orthod 82(5):792–8. https://doi.org/10.2319/111911-717.1. Epub 2012 Mar 5. PMID: 22390633; PMCID: PMC8823124
D’Urso PS, Barker TM, Earwaker WJ, Bruce LJ, Atkinson RL, Lanigan MW, Arvier JF, Effeney DJ (1999) Stereolithographic biomodelling in cranio-maxillofacial surgery: a prospective trial. J Craniomaxillofac Surg 27(1):30–37. https://doi.org/10.1016/s1010-5182(99)80007-9. PMID: 10188125
Kubota M, Nakano H, Sanjo I, Satoh K, Sanjo T, Kamegai T, Ishikawa F (1998) Maxillofacial morphology and masseter muscle thickness in adults. Eur J Orthod 20(5):535–542. https://doi.org/10.1093/ejo/20.5.535. PMID: 9825556
Zarb GA, Carlsson GE, Sessle BJ, Mohl ND (1994) Temporomandibular joint and masticatory muscle disorders, 2nd edn. Munksgaard, Copenhagen
Ferrario VF, Sforza C, Serrao G (1999) The influence of crossbite on the coordinated electromyographic activity of human masticatory muscles during mastication. J Oral Rehabil 26(7):575–581. https://doi.org/10.1046/j.1365-2842.1999.00419.x. PMID: 10445477
Ruggiero F, Badiali G, Bevini M, Marchetti C, Ong J, Bolognesi F et al (2022) Parametrizing the genioplasty: a biomechanical virtual study on soft tissue behavior. Int J Comput Assist Radiol Surg 17(1):55–64. https://doi.org/10.1007/s11548-021-02489-9. Epub 2021 Sep 17. PMCID: PMC8739543
Ruggiero F, Borghi A, Bevini M, Badiali G, Lunari O, Dunaway D, Marchetti C (2023) Soft tissue prediction in orthognathic surgery: Improving accuracy by means of anatomical details. PLoS One 18(11):e0294640. https://doi.org/10.1371/journal.pone.0294640. PMID: 38011187; PMCID: PMC10681161
Luboz V, Promayon E, Payan Y (2014) Linear elastic properties of the facial soft tissues using an aspiration device: towards patient specific characterization. Ann Biomed Eng 42(11):2369–2378. https://doi.org/10.1007/s10439-014-1098-1
Brunel G, El-Haddioui A, Bravetti P, Zouaoui A, Gaudy JF (2003) General organization of the human intra-masseteric aponeuroses: changes with ageing. Surg Radiol Anat 25(3–4):270–283. https://doi.org/10.1007/s00276-003-0125-y. Epub 2003 Sep 6. PMID: 13680179
Raberin M (2000) Muscular equilibrium and orthognathic surgery. A preliminary electromyographic study. Orthod Fr 71(1):37–48
Opdebeeck H, Bell WH (1978) The short face syndrome. Am J Orthod 73(5):499–511. https://doi.org/10.1016/0002-9416(78)90240-3. PMID: 277066
Björk A (1969) Prediction of mandibular growth rotation. Am J Orthod 55(6):585–599. https://doi.org/10.1016/0002-9416(69)90036-0. PMID: 5253957
Proffit WR, White RP Jr (1990) Who needs surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg 5(2):81–89. PMID: 2074379
Trawitzki LV, Dantas RO, Mello-Filho FV, Marques W Jr (2010) Masticatory muscle function three years after surgical correction of class III dentofacial deformity. Int J Oral Maxillofac Surg 39(9):853–856. https://doi.org/10.1016/j.ijom.2009.03.006. Epub 2009 Apr 16. PMID: 19375282
Kiliaridis S, Engström C, Thilander B (1985) The relationship between masticatory function and craniofacial morphology. I. A cephalometric longitudinal analysis in the growing rat fed a soft diet. Eur J Orthod 7(4):273–83. https://doi.org/10.1093/ejo/7.4.273. PMID: 3865789
Ferrario VF, Sforza C (1996) Coordinated electromyographic activity of the human masseter and temporalis anterior muscles during mastication. Eur J Oral Sci 104(5–6):511–517. https://doi.org/10.1111/j.1600-0722.1996.tb00134.x. PMID: 9021318
Kiliaridis S, Mejersjö C, Thilander B (1989) Muscle function and craniofacial morphology: a clinical study in patients with myotonic dystrophy. Eur J Orthod 11(2):131–138. https://doi.org/10.1093/oxfordjournals.ejo.a035975. PMID: 2767145
Ingervall B, Bitsanis E (1987) A pilot study of the effect of masticatory muscle training on facial growth in long-face children. Eur J Orthod 9(1):15–23. https://doi.org/10.1093/ejo/9.1.15. PMID: 3470182
Schiaffino S, Reggiani C (1996) Molecular diversity of myofibrillar proteins: gene regulation and functional significance. Physiol Rev 76(2):371–423. https://doi.org/10.1152/physrev.1996.76.2.371. PMID: 8618961
Sciote JJ, Rowlerson AM, Hopper C, Hunt NP (1994) Fibre type classification and myosin isoforms in the human masseter muscle. J Neurol Sci 126(1):15–24. https://doi.org/10.1016/0022-510x(94)90089-2. PMID: 7836942; PMCID: PMC3863992
Smerdu V, Karsch-Mizrachi I, Campione M, Leinwand L, Schiaffino S (1994) Type IIx myosin heavy chain transcripts are expressed in type IIb fibers of human skeletal muscle. Am J Physiol 267(6 Pt 1):C1723–C1728. https://doi.org/10.1152/ajpcell.1994.267.6.C1723. PMID: 7545970
Soussi-Yanicostas N, Barbet JP, Laurent-Winter C, Barton P, Butler-Browne GS (1990) Transition of myosin isozymes during development of human masseter muscle. Persistence of developmental isoforms during postnatal stage. Development 108(2):239–49. https://doi.org/10.1242/dev.108.2.239. PMID: 2140978
Boyd SB, Gonyea WJ, Finn RA, Woodard CE, Bell WH (1984) Histochemical study of the masseter muscle in patients with vertical maxillary excess. J Oral Maxillofac Surg 42(2):75–83. https://doi.org/10.1016/0278-2391(84)90315-x. PMID: 6229616
Hunt NP, Cunningham SJ (1998) The use of kinesiography to assess mandibular rest positions following corrective orthognathic surgery. J Craniomaxillofac Surg 26(3):179–184. https://doi.org/10.1016/s1010-5182(98)80010-3. PMID: 9702638
Gaspard M, Laison F, Lautrou A (1976) Le plan général d’organisation de la musculature masticatrice chez les mammifères [General organization system of the masticatory muscles in mammals]. Actual Odontostomatol (Paris) 113:65–100. French. PMID: 941725
Gaspard M, Laison F, Mailland M (1973) Organisation architecturale et texture du masséter chez les primates et l’homme [Architectural organization and texture of the masseter muscle in primates and man]. J Biol Buccale 1(1):7–20. French. PMID: 4517446
Gaspard M (1987) Structuration fonctionnelle du complexe musculaire temporo-massétérin humain de l’age foetal a l’age adulte [Functional structure of the human temporal-masseter muscle complex in the fetus and the adult]. Orthod Fr 58 Pt 2:549–65. French. PMID: 3334688
Yoshikawa T (1961) The comparative anatomy of the masseter muscle of the mammals. Acta Anat Nippon 36:53–71
Yoshikawa T, Suzuki T (1962) The lamination of the human masseter. The new identification of muscle temporalis superficialis, muscle maxillo-mandibularis and muscle zygomaticomandibularis in the human anatomy. Acta Anat Nippon 37:206–217
Gaudy JF, Hadida A, Brunel G, Tavernier JC (1982) Les muscles masticateurs possédant une insertion capsulo-méniscale au niveau de l’ATM. Inf Dent 39:3517–3519
Unger JM (1985) The oral cavity and tongue: magnetic resonance imaging. Radiology 155(1):151–153. https://doi.org/10.1148/radiology.155.1.3975395. PMID: 3975395
Kobayashi T, Honma K, Shingaki S, Nakajima T (2001) Changes in masticatory function after orthognathic treatment in patients with mandibular prognathism. Br J Oral Maxillofac Surg 39(4):260–265. https://doi.org/10.1054/bjom.2000.0576. PMID: 11437420
Katsumata A, Fujishita M, Ariji Y, Ariji E, Langlais RP (2004) 3D CT evaluation of masseter muscle morphology after setback osteotomy for mandibular prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98(4):461–470
Ueki K, Okabe K, Mukozawa A, Miyazaki M, Marukawa K, Hashiba Y, Nakagawa K, Yamamoto E (2009) Assessment of ramus, condyle, masseter muscle, and occlusal force before and after sagittal split ramus osteotomy in patients with mandibular prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:679–686
Trawitzki LV, Dantas RO, Elias-Júnior J, Mello-Filho FV (2011) Masseter muscle thickness three years after surgical correction of class III dentofacial deformity. Arch Oral Biol 56:799–803
Kang JH, Shin DS, Kim SW, Lim HJ, Kim BC (2022) Volumetric change in the masseter and lateral pterygoid after mandibular setback. J Pers Med 12(5):820. https://doi.org/10.3390/jpm12050820. PMID: 35629242; PMCID: PMC9146455
Kikuta T, Hara I, Seto T, Yoshioka I, Nakashima T, Yasumitsu C (1994) Evaluation of masticatory function after sagittal split ramus osteotomy for patients with mandibular prognathism. Int J Adult Orthod Orthognath Surg 9(1):9–17
Piancino MG, Isola G, Merlo A, Dalessandri D, Debernardi C, Bracco P (2012) Chewing pattern and muscular activation in open bite patients. J Electromyogr Kinesiol 22(2):273–279
Jokaji R, Ooi K, Yahata T, Nakade Y, Kawashiri S (2022) Evaluation of factors related to morphological masseter muscle changes after preoperative orthodontic treatment in female patients with skeletal class III dentofacial deformities. BMC Oral Health 22(1):292. https://doi.org/10.1186/s12903-022-02319-7. PMID: 35843934; PMCID: PMC9288706
Throckmorton GS, Buschang PH, Ellis E (1996) III Improvement of maximum occlusal forces after orthognathic surgery. J Oral Maxillofac Surg 54:1080–1086
Throckmorton GS, Ellis E III (2001) The relationship between surgical changes in dentofacial morphology and changes in maximum bite force. J Oral Maxillofac Surg 59:620–627
Acknowledgements
Not applicable.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
FD, JNS, and CR read and wrote the manuscript. FD and CR were responsible for conducting surgeries. FD and JNS were responsible for the data collection. FD designed and wrote the entire article. CH was responsible for the final revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This project has approval by the Joint Research & Ethics Committee of UCL Hospitals NHS Trust, Reference No.03/E012. This project is covered by the UCL Data Protection Registration Reference No. Z6364106, Section 19, Research: Health Research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duarte, F., Silva, J.N., Ramos, C. et al. Anatomic and functional masseter muscle adaptation following orthognathic surgery—MRI analysis in 3 years of follow-up. Maxillofac Plast Reconstr Surg 46, 26 (2024). https://doi.org/10.1186/s40902-024-00437-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40902-024-00437-6