Abstract
Purpose
Surgical removal of intra-bony calcific benign lesions is technically challenging regarding its accessibility, proximity to vital structures, and deteriorating effect on the remaining bony structures.
Methods
Computer-guided buccal cortical plate separation was performed for ten patients using patient-specific osteotomy locating guides and pre-bent plates. The guide was designed to outline the osteotomy, the buccal cortical plate was separated, the lesion was removed, and finally, the pre-bent plates were used to fix the separated cortex.
Results
Surgical procedures were uneventful for all patients, operation time was 39.5 ± 13.01 min, postoperative pain decreased within the follow-up time intervals, and there was a statistical significant difference between the time intervals (P value < 0.001). Edema and trismus were acceptable. One case showed nerve affection which resolved after 4 weeks.
Conclusion
Computer-guided buccal cortical plate separation for removal of intra-bony calcified benign lesions provides a promising approach, especially for inexperienced surgeons.
Trial registration
ClinicalTrials.gov NCT05329974. Registered on 6 April 2022—retrospectively registered.
Similar content being viewed by others
Introduction
Odontogenic tumors (OTs) have captured the attention of pathologists and surgeons despite their rarity, owing to their devastating impact on the patient’s quality of life [1, 2]. In an ongoing attempt to address the wide diversity of odontogenic tumors, its classification has passed through many stages, starting from the first WHO classification released in 1971 till the fourth and latest classification released in 2017 [3,4,5]. The classification reflects the heterogeneity of the odontogenic tumors with respect to their origin either epithelial and/or mesenchymal tissues. Moreover, OTs differ greatly in their nature and behavior varying from completely benign lesions to locally invasive benign lesions and even malignant lesions [4, 6]
OTs’ inconsistent clinical behavior was reflected in their treatment methods, as some lesions may require no treatment, and others may be treated by conservative enucleation and curettage while others may require a more radical treatment via resection with safety margins [7]. Regardless of the method of treatment, the success of OTs treatment depends primarily on its complete removal to avoid any possible recurrence [8,9,10]. However, this complete removal may be complicated by their size, consistency, nature, and location [11].
The mandibular angle region is the site of predilection for various odontogenic tumors among them benign calcified odontogenic tumors [12,13,14,15,16,17]. Despite their benign nature, the excision of such calcified lesions indicates wide surgical access and extensive bone removal. Intra-oral total or staged excision of the lesion via either the buccal or lingual cortex has been illustrated in the literature [18,19,20,21,22,23,24]. The buccal approach is associated with extensive bone removal in the external oblique ridge which highly compromises mandibular angle strength. While the lingual approach reduces mandibular fracture risk, it endangers the lingual nerve; furthermore, the approach is technically challenging with limited accessibility [25].
In 2005, a new approach was introduced for the removal of deeply impacted third mandibular molars using buccal cortical plate separation (buccal corticotomy). In this approach a rectangular buccal cortical plate window was made over the tooth and separated, then the tooth was removed, and finally, the separated bone was seated and fixed in position [26,27,28].
Over the last two decades, computer-assisted surgery has been widely used in oral and maxillofacial surgery and moved from virtual planning to the construction of different patient-specific hardware. These advances markedly facilitate the surgical procedures and reduce intraoperative time, especially with inexperienced surgeons [29, 30]. In this study, we aim to assess the use of a computer-guided buccal cortical plate separation approach using patient-specific cutting guide for the removal of intra-bony calcified odontogenic lesions affecting the mandibular angle region.
Patients and methods
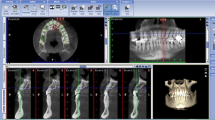
This was a prospective case series conducted on 10 patients with well-defined radiopaque lesions affecting the angle region, recruited consecutively from our out-patient clinic. The study was approved by the research ethics committee (IRB: 18,221) and followed the Declaration of Helsinki on medical research. Patients were selected according to the following clinical criteria: patients with well-defined radiopaque lesion affecting the angle region, its conventional removal may compromise the bone continuity and leads to pathological fracture indicating the need of buccal cortical plate separation technique. Patients with any medical condition contraindicating the surgical procedures were excluded (Fig. 1).
All enrolled patients were subjected to a computer-guided buccal cortical plate separation approach for removal of the calcific intra-bony masses using patient-specific osteotomy locating surgical guide and pre-bent titanium mini-plate either 2.0 for small lesions or 2.3 for large lesions compromising the inferior mandibular border based on the preoperative virtual planning and simulation.
Preoperative preparation and virtual planning
Cone beam computed tomography (CBCT) (SCANORA 3D with Auto-Switch; Soredex, Helsinki, Finland) was requested for all patients. DICOM files were imported to the planning software (Mimics 19.0, Materialise NV, Leuven, Belgium). Intra-bony lesion size and extensions were further 3D analyzed after clinical assessment to assure their correspondence with eligibility criteria and prepare the surgical guide for the mass removal. The virtual planning was performed using the software to formulate the buccal window that totally exposes the intra-bony calcific mass without affection of neighboring vital structure, and the patient-specific osteotomy locating guide was then designed on the bone surface to outline the buccal window (Fig. 2).
Finally, Stereolithography files (STL) of the surgical guide and the mandible were exported to an additive Computer-Aided Manufacturing (CAM) machine (FORMIGA P 110 printer; EOS e-manufacturing solutions, Munich, Germany) and manufactured in white polyamide (PA2200; EOS e-manufacturing solutions, Munich, Germany) using fused deposition modeling (FDM) technology (Fig. 3). The printed mandibular model was used for preoperative adaptation of one conventional either 2.0 or 2.3 titanium mini-plate based on the size of the lesion. The plate was adapted over the mandibular model to rest on sound bone mesial and distal to the created buccal window.
Surgical procedures
Surgical procedures were performed under general anesthesia with nasal intubation. Angel region was exposed through intraoral extended wards’ incision. The osteotomy locating surgical guide was placed on the exposed bony surface and fixed in position with 2 screws, then a reciprocating saw was used to perform the planned osteotomy. The created buccal door was mobilized using spatula chisels and opened to expose the intra-bony calcific mass. The exposed masses were passively removed either without or with sectioning according to the mass size (Fig. 4). The lesion bed was debrided, and the separated buccal cortical plate was repositioned and fixed using the pre-bent plate (Fig. 5). Finally, the wound was sutured.
Postoperative follow-up and outcomes
A pressure band was applied to the cheek areas for 48 h postoperatively. The patients were instructed to apply ice packs over the cheek area for 20 min every hour for 6 h postoperatively and to rinse their mouth with warm saline solution starting on the second day after surgery. The patients were kept on a soft diet for the first 48 h. Postoperative antibiotic, analgesic, and anti-inflammatory drugs were prescribed for 5–7 days. The patients were recalled 2, 5, and 10 days after the surgery for initial clinical assessment.
Intra-operative time was measured from the start of the incision till suturing. Postoperative pain was evaluated 2, 5, and 10 days after the surgery using 0–10 visual analog scale (VAS). Edema and trismus were evaluated 5 and 10 days after the surgery. Edema was assessed using a four-grade scale: grade 0, no edema; grade 1, mild edema (just visible); grade 2; moderate edema (local); and grade 3, severe edema (extended). Trismus was also assessed using four grades scale: grade 0, no trismus; grade 1, mild trismus (the patient could insert two fingers vertically together into the mouth); grade 2; moderate trismus (the patient could insert only one finger); and grade 3, severe trismus (the patient could not open to insert one finger). Inferior alveolar nerve function was assessed at the follow-up time intervals by pricking using a dental probe at multiple points to evaluate the pain perception and by light touch using a cotton wisp to evaluate the tactile sensation. Further clinical assessment was continued at 4 weeks, 6 weeks, and 2 months to monitor the soft tissue healing and detect any plate exposure. Finally, a panoramic radiograph was requested after 2 months of surgery to assess the bone healing and integrity.
Statistical analysis
Statistical analysis was performed using SPSS (Statistical package for the social sciences- IBM® SPSS® Statistics Version 20 for Windows, IBM Corp., Armonk, NY, USA). Qualitative data were represented as percentage and frequency. Quantitative data were represented as mean ± standard deviation. Kruskal–Wallis test was used to compare pain scores between the three-time points, and Bonferroni correction to post hoc multiple comparisons. The results were considered statistically significant if the p value was less than 0.05.
Results
This study was conducted on 10 patients (5 males and 5 females) with well-defined radiopaque lesions affecting the angle region removed using a computer-guided buccal cortical plate separation technique. The mean age of the patients was 27.9 ± 3.7 years. Histological analysis showed that the lesion was complex odontoma in 6 patients (60%), Cementoblastoma in 4 patients (40%) (Table 1). The surgical procedures were uneventful for all patients, and the operation time was 39.5 ± 13.01 min. There was no nerve affection during the follow up time intervals, except only for one case who showed total nerve recovery 4 weeks postoperatively. The pain score decreased with time from 4.7 ± 1.49 at the 2nd day to 2.4 ± 1.07 at the 5th day, and 0.4 ± 0.52 at the 10th day, and there was a statistical significant difference between the 3 time points (P value < 0.001). Post hoc analysis showed no statistical significance difference between 2nd day and 5th day pain (P value 0.091); however, it showed a statistical significant difference between 5th day and 10th day pain (P value 0.026). At the 5th day, edema was moderate in 5 patients (50%) and mild in the other 5 patients (50%), while trismus was severe in one patient (10%), moderate in 2 patients (20%), and mild in 7 patients (70%). At the 10th day, no edema was observed in 4 patients (40%) and 6 patients (60%) showed mild edema, mild trismus was observed in 3 patients (30%), and no trismus in 7 patients (70%) (Fig. 6). Postoperative panoramic radiograph showed complete bone healing and integrity of the osteotomized buccal cortex (Fig. 7).
Discussion
Mandibular molar–angle region represents the most common site for odontogenic calcified benign tumors, that originate from the cellular remnants of the developing wisdom tooth that is usually associated with many molecular and physiological changes [12,13,14,15,16,17]. Different surgical approaches have been utilized for tumor removal at this site. Sagittal split osteotomy via an intra-oral approach avoids large bony defects without compromising the perfect surgical access, yet it may result in injury to the inferior alveolar nerve, possible condylar sag, and unpredicted cortical bone fracture [23, 24]. Intra-oral excision through the buccal or lingual cortex has been utilized as a simpler alternative [25]. However, these approaches are associated with high morbidity due to the excessive bone removal and nerve endangerment.
Buccal cortical plate separation (buccal corticotomy) has been introduced for deeply impacted third mandibular molars removal by Kwon Y-D. et al. [26] in a case report, followed by Tay ABG et al. [27] in another one. This approach is considered as an intermediate link between buccal cortex removal and sagittal split osteotomy. It avoids extensive bone removal, limited visibility, high risk of nerve injury, and mandibular fracture associated with the conventional buccal approach; moreover, it avoids the possible occlusion risk and unfavorable split associated with sagittal split osteotomy. Additionally, it is considered a straightforward and easier procedure compared to sagittal split osteotomy [26,27,28].
A previous case report by Nogueira et al. used free-hand buccal cortical plate separation for the removal of complex odontoma [31]. In this study, we used computer-guided buccal cortical plate separation using patient-specific cutting guide to overcome the pit flows of previous techniques for the removal of odontogenic calcified benign tumors affecting the molar angle region. The computer guidance revolution in dentistry allowed us to gain the advantage of the virtual planning and computer-assisted surgery to determine the extent of the bone window and outline it using the patient-specific cutting guide. Additionally, a printed 3D model was constructed for preoperative plate adaptation to facilitate the surgical procedures [30].
In our study, the patient’s age was mostly in the third decade which was coincident with the literature that most of the benign calcified odontogenic tumors start to appear accidentally during routine radiographic interpretation or after induction of slight swelling and discomfort at this age group [11, 32, 33]. Postoperative histological interpretation revealed complex odontomas in 6 patients. This is also coincident with the literature that demonstrated that odontomas represent the first and most common calcified odontogenic tumor and that posterior odontomas are mostly complex types [11, 34], while in the other 4 cases, the lesion was cementoblastoma, where posterior mandible represents the most common site of this lesion [35,36,37].
The use of a patient-specific surgical guide and pre-bent plate in our study facilitated the safe buccal cortex separation and accurate postoperative readaptation with low effort and minimal time. The wide access and visibility of the lesion facilitated the rapid removal of any undercut with safe excision of the calcified lesion without any induced forces this was reflected positively on the postoperative outcomes that revealed minimum pain, edema, and trismus with maximum inferior alveolar nerve integrity. These findings can be attributed to the wide approach associated with adequate access and maximum visibility of both lesion and vital structures with maximum preservation of the external oblique ridge integrity and mandibular strength [31]. However, the major limitation of this technique is very large lesions associated with thinning of the buccal cortex which contraindicate the buccal cortical plate separation [31].
Conclusion
Surgical removal of intra-bony calcific benign lesions is technically challenging regarding its accessibility, proximity to vital structures, and deteriorating effect on the remaining bony structures. Computer-guided buccal cortical plate separation for intra-bony benign calcified odontogenic tumor removal provides a promising approach with minimal postoperative complications and facilitates surgical procedures, especially for inexperienced surgeons. However, we recommend the conduction of more investigations and comparative studies for further evaluation of its benefits compared to the conventional approach.
Availability of data and materials
All data are available whenever requested.
Abbreviations
- OTs:
-
Odontogenic tumors
- WHO:
-
World Health Organization
- CBCT:
-
Cone beam computed tomography
- STL:
-
Stereolithography files
- CAM:
-
Computer-Aided Manufacturing
- FDM:
-
Fused deposition modeling
- VAS:
-
Visual analog scale
References
Philipsen HP, Reichart PA (2006) Classification of odontogenic tumours. A historical review. J Oral Pathol Med 35(9):525–529. https://doi.org/10.1111/j.1600-0714.2006.00470.x
Mamabolo M, Noffke C, Raubenheimer E (2011) Odontogenic tumours manifesting in the first two decades of life in a rural African population sample: a 26 year retrospective analysis. Dentomaxillofac Radiol 40(6):331–337. https://doi.org/10.1259/dmfr/54585925
Chrysomali E, Leventis M, Titsinides S, Kyriakopoulos V, Sklavounou A (2013) Odontogenic tumors. J Craniofac Surg 24(5):1521–1525. https://doi.org/10.1097/SCS.0b013e3182997aaf
Wright JM, SolukTekkesin M (2017) Odontogenic tumors: where are we in 2017? J Istanb Univ Fac Dent 51(3):S10–S30. https://doi.org/10.17096/jiufd.52886
El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ (2017) Odontogenic and maxilofacial bone tumours. In: WHO classification of Head and Neck Tumour, 4th edn. IARC, Lyon, p 205–260. https://publications.iarc.fr/Book-And-Report-Series/Who-Classification-Of-Tumours/WHO-Classification-Of-Head-And-Neck-Tumours-2017
Hellstein JW (2004) Odontogenesis, odontogenic cysts, and odontogenic tumors. In: Flint PW, Haughey BH, Lund V, et al., editors. Cummings otolaryngology, 6th edn. Saunders, an imprint of Elsevier Inc, Philadelphia, p 1323–1344. https://entokey.com/odontogenesis-odontogenic-cysts-and-odontogenic-tumors/
Covello P, Buchbinder D (2016) Recent trends in the treatment of benign odontogenic tumors. Curr Opin Otolaryngol Head Neck Surg 24(4):343–351. https://doi.org/10.1097/MOO.0000000000000269
Zaitoun H, Kujan O, Sloan P (2007) An unusual recurrent cementoblastoma associated with a developing lower second molar tooth: a case report. J Oral Maxillofac Surg 65(10):2080–2082. https://doi.org/10.1016/j.joms.2006.06.288
Borges DC, Rogério de Faria P, Júnior HM, Pereira LB (2019) Conservative treatment of a periapical cementoblastoma: a case report. J Oral Maxillofac Surg 77(2):272.e1-272.e7. https://doi.org/10.1016/j.joms.2018.10.003
Brannon RB, Fowler CB, Carpenter WM, Corio RL (2002) Cementoblastoma: an innocuous neoplasm? a clinicopathologic study of 44 cases and review of the literature with special emphasis on recurrence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93(3):311–320. https://doi.org/10.1067/moe.2002.121993
Cezairli B, Taşkesen F, Coşkun Ü et al (2017) Surgical treatment of a large complex odontoma. Emre Tosun Meandros Med Dent J 18:148–152
Bereket C, Çakır-Özkan N, Şener İ, Bulut E, Tek M (2015) Complex and compound odontomas: analysis of 69 cases and a rare case of erupted compound odontoma. Niger J Clin Pract 18(6):726–730. https://doi.org/10.4103/1119-3077.154209
Chrcanovic BR, Gomez RS (2017) Cementoblastoma: An updated analysis of 258 cases reported in the literature. J Craniomaxillofac Surg 45(10):1759–1766. https://doi.org/10.1016/j.jcms.2017.08.002
Soluk Tekkesin M, Pehlivan S, Olgac V, Aksakallı N, Alatli C (2012) Clinical and histopathological investigation of odontomas: review of the literature and presentation of 160 cases. J Oral Maxillofac Surg 70(6):1358–1361. https://doi.org/10.1016/j.joms.2011.05.024
Amado Cuesta S, GargalloAlbiol J, BeriniAytés L, Gay Escoda C (2003) Review of 61 cases of odontoma. presentation of an erupted complex odontoma. Med Oral 8(5):366–373
Prakash R, Gill N, Goel S, Verma S (2013) Cementoblastoma. A report of three cases. N Y State Dent J 79(2):41–43
Jeyaraj CP (2014) Clinicopathological study of a case of cementoblastoma and an update on review of literature. J Oral Maxillofac Surg Med Pathol 26:415–442
Kuramochi MM, Vanti LA, Berenguel IA, Pereira WL, Zangrando D (2006) Acesso extra-oral para reconstrução primária em odontoma complexo raro em mandíbula. Rev Port Estomatol Cir Maxilofac 47:35–40
Chrcanovic BR, Jaeger F, Freire-Maia B (2010) Two-stage surgical removal of large complex odontoma. Oral Maxillofac Surg 14(4):247–252. https://doi.org/10.1007/s10006-010-0206-0
Frame JW (1986) Surgical excision of a large complex composite odontome of the mandible. Br J Oral Maxillofac Surg 24(1):47–51. https://doi.org/10.1016/0266-4356(86)90040-9
Or S, Kişnişci R (1987) Complex odontoma of the mandible. Report of a case. Quintessence Int 18(2):159–161
Killey HC, Kay LW (1966) Large complex composite odontomas of the jaws. Int Surg 46(2):103–107
Casap N, Zeltser R, Abu-Tair J, Shteyer A (2006) Removal of a large odontoma by sagittal split osteotomy. J Oral Maxillofac Surg 64(12):1833–1836. https://doi.org/10.1016/j.joms.2005.11.060
Wong GB (1989) Surgical management of a large, complex mandibular odontoma by unilateral sagittal split osteotomy. J Oral Maxillofac Surg 47(2):179–184. https://doi.org/10.1016/s0278-2391(89)80113-2
Blinder D, Peleg M, Taicher S (1993) Surgical considerations in cases of large mandibular odontomas located in the mandibular angle. Int J Oral Maxillofac Surg 22(3):163–165. https://doi.org/10.1016/s0901-5027(05)80243-7
Kwon YD, Ryu DM, Lee B, Kim YG, Oh JH (2006) Separation of the buccal cortical plate for removal of the deeply impacted mandibular molars. Int J Oral Maxillofac Surg 35(2):180–182. https://doi.org/10.1016/j.ijom.2005.07.005
Tay AB (2007) Buccal corticotomy for removal of deeply impacted mandibular molars. Br J Oral Maxillofac Surg 45(1):83–84. https://doi.org/10.1016/j.bjoms.2005.12.009
Scolozzi P (2021) Buccal corticotomy using piezosurgery as a surgical approach for removal of deeply impacted mandibular teeth: an alternative procedure to avoid pitfalls associated with the conventional technique. J Stomatol Oral Maxillofac Surg S2468–7855(21):00088–4. https://doi.org/10.1016/j.jormas.2021.04.012 (Advance online publication)
Ahmed M, Soliman S, Noman SA, Ali S (2020) Computer-guided contouring of craniofacial fibrous dysplasia involving the zygoma using a patient-specific surgical depth guide. Int J Oral Maxillofac Surg 49(12):1605–1610. https://doi.org/10.1016/j.ijom.2020.04.009
Omara M, Ali S, Ahmed M (2021) Accuracy of midface advancement using patient-specific surgical guides and pre-bent plates versus conventional interocclusal wafers and conventional plate fixation in quadrangular Le Forte II osteotomy. A randomised controlled trial. Br J Oral Maxillofac Surg S0266-4356(21):00171–6. https://doi.org/10.1016/j.bjoms.2021.05.002 (Advance online publication)
Nogueira AS, Gonçales ES, Gonçales AG, Thiegui-Neto V, Nogueira CB, Nogueira A, Medeiros R (2013) Surgical treatment of extensive complex odontoma in the mandible by corticotomy a case report. Minerva Stomatol 62(9):335–342
An SY, An CH, Choi KS (2012) Odontoma: a retrospective study of 73 cases. Imaging Sci Dent 42(2):77–81. https://doi.org/10.5624/isd.2012.42.2.77
Levi-Duque F, Ardila CM (2019) Association between odontoma size, age and gender: Multivariate analysis of retrospective data. J Clin Exp Dent 11(8):e701–e706. https://doi.org/10.4317/jced.55733
Avelar RL, Primo BT, Pinheiro-Nogueira CB, Studart-Soares EC, de Oliveira RB, Romulo de Medeiros J, Hernandez PA (2011) Worldwide incidence of odontogenic tumors. J Craniofac Surg 22(6):2118–2123. https://doi.org/10.1097/SCS.0b013e3182323cc7
Pynn BR, Sands TD, Bradley G (2001) Benign cementoblastoma: a case report. J Can Dent Assoc 67(5):260–262
Kramer JR, Pindborg JJ, Shear M (1992) Histological typing of odontogenic tumors, jaw cysts and allied lesions. International histological classification of tumors. World Health Organization, Geneva, pp 23–40
Vindenes H, Nilsen R, Gilhuus-Moe O (1979) Benign cementoblastoma. Int J Oral Surg 8(4):318–324. https://doi.org/10.1016/s0300-9785(79)80055-1
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors (MO, AG, and SA) contributed to the conception and study designing, Acquisition of data, analysis, and interpretation of the collected data. The manuscript was written and revised by all authors (MO, AG, and SA). All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki on medical research and approved by the research ethics committee (IRB:18221). Written informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for the publication of the images.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Omara, M., Gouda, A. & Ali, S. Computer-guided buccal cortical plate separation for removal of calcified benign odontogenic tumors affecting the mandibular angle region. Maxillofac Plast Reconstr Surg 44, 30 (2022). https://doi.org/10.1186/s40902-022-00354-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40902-022-00354-6