Abstract
Background
Solitary Bone Cyst (SBC), also known as a simple bone cyst, hemorrhagic cyst, or traumatic cyst is classified by the WHO among non-odontogenic benign lesions of the jaw. The article explores the use of a static 3D-printed surgical guide to treat mandibular SBC, emphasizing a minimally surgical approach for this lesion.
Case Presentation
A 20-year-old woman was referred for a persistent mandibular SBC lacuna, without specific complaints. Her medical history included a previous bone trepanation for a SBC in the same area, radiologically and surgically confirmed. X-ray assessment showed a well-defined unilocular radiolucency surrounding the root of the first left lower molar (tooth #36), measuring 10 × 10 mm. Pulp sensitivity was normal. CBCT data and STL files of dental cast were obtained preoperatively and registered. A 3D-printed surgical guide was used for minimally invasive trepanation of the buccal cortical. The simulation used a targeted endodontic microsurgery approach in order to determine axis and diameter of the trephine. Surgery was performed under local anesthesia. The guide was tooth supported integrating tubes and a fork for guiding precise trepanation. A 3.5 mm round bone window was created, leaving an empty cavity confirming SBC diagnosis and permitting bone curettage. A blood clot was obtained to promote bone healing. Complete reossification was observed after 6 months. The follow-up at 2 years confirmed a complete bone healing with normal pulp sensitivity.
Discussion
The 3D-printed windowed surgical guide with dental support offers big advantages, including improved visibility and reduced errors. Compared to traditional guides, it eliminates visual hindrance and allows easier and quick access to confined areas as well as an improved irrigation during drilling process. The article also highlights the importance of preoperative planning while acknowledging potential limitations and errors and surgical complications.
Conclusion
The use of the 3D-printed surgical guide could be used in routine for minimally invasive intervention of SBC. This case also demonstrates the potential utility of this approach in various procedures in oral and maxillofacial surgery. The technique provides precise localization, reducing complications and enhances operative efficiency.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Solitary Bone Cyst (SBC), also known as a simple bone cyst, hemorrhagic cyst, or traumatic cyst is classified by the WHO among the benign lesions of the maxillae [1]. The variety of these names to describe a single lesion reflects the poor understanding of its etiopathogenesis. However, trauma seems to be one of the causes attributed to the occurrence of SBCs [2].
SBC is actually a pseudo-cyst. The bone cavity is not lined by an epithelial membrane. The intralesional surgical observation reveals a bony cavity containing a characteristic serous or sero-hematic fluid. The absence of a cystic wall and the intralesional fluid content confirm this diagnosis [3]. Histologically, if the operator sends a curettage product of the bony wall, one may find a very thin layer of nonspecific loose connective tissue [2]. In all cases, for SBCs, the definitive diagnosis relies on the intraoperative clinical view.
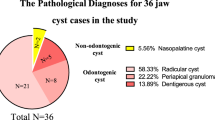
There appears to be no gender predilection, but the prevalence is higher in children and young adults around the 2nd and 3rd decades. It is a bony defect found in the metaphysis of long bones as well as in the jaws. It represents approximately 1% of maxillary cystic lesions. Furthermore, there is a strong predilection for the mandible, with over 90% of lesions found there [4, 5].
80% of SBCs are asymptomatic and discovered incidentally on X-rays. The remaining cases may be revealed by dental sensitivities, bone pain, intra-oral swelling or facial asymmetry [6, 7].
The SBC appears on standard imaging exams (X-rays and CBCT) as a mostly unilocular radiolucency but may sometimes exhibit intralesional septa. It can erode the bony cortices and is bordered by a rim of peripheral osteosclerosis indicating its chronic evolution and benign nature. The buccal and lingual cortices are blown out, and the inferior alveolar nerve canal is indiscernible radiographically inside this lesion [3].
A surgical approach is indicated to achieve a complete bone healing without recurrence. This window can be done using microsurgical instruments mounted on a handpiece, such as a micro-saw or other dedicated bone drills or by using piezo-surgery. Once again, the diagnosis is confirmed intraoperatively upon breaching this bony defect. The goal of surgery is to provide “decompression” of the bony cavity and to perform a proper curettage of the walls to stimulate a bleeding to fill the cavity by a blood clot. This will induce pro-osteogenic action of the adjacent bony walls. However, follow-up is necessary to confirm the complete reossification of the bony defect [5].
Understanding the importance of precise preoperative diagnosis is crucial to optimizing the surgical approach, remaining minimally invasive for bone, teeth vitality, roots and inferior alveolar bundle nerve preservation, reducing operative time, and optimizing bone healing.
In the present report, we introduce a custom-made 3D-printed surgical guide allowing accurate access of SBC via a minimally invasive surgery inspired by a targeted endodontic microsurgery approach [8].
Case presentation
A 20-year-old woman was referred by her dentist concerning a persistent mandibular radiolucency to the Department of Oral Surgery, University Hospital of Strasbourg. She did not have any complaints. His medical history revealed a previous bone trepanation six years ago in the same mandibular area for a SBC. A preliminary diagnosis was previously established through Cone Beam Computed Tomography (CBCT) and Magnetic Resonance Imaging (MRI) assessment [9]. Intraoperatively, the diagnosis was clinically confirmed by the presence of an empty bony cavity, as widely documented in literature [3, 10].
The new CBCT showed a well-defined unilocular radiolucent area below the root apices of the left mandibular first molar, measuring 10 × 10 mm (Fig. 1A, B and C) with a close proximity with mandibular canal located below. The pulp sensitivity was normal for teeth 36 and 37. Based on medical history, imaging assessment, diagnosis of persistent SBC was established. A surgical exploration was proposed to confirm diagnosis and performing a second curettage. As roots were included in the lesion and inferior alveolar canal was close to the bottom of the lesion, a surgical guide was proposed to perform a minimally invasive cortical trepanation and prevent damage to the nearby noble structures.
CBCT DICOM files dataset and stereolithographic (STL) file of dental model scans (Trios; 3Shape, Copenhagen, Denmark) were acquired preoperatively. All dataset were registered in Blue Sky Plan software (Blue Sky Bio LLC, Grayslake, IL, USA). In this case, the simulation was performed with a dental implant compatible with the diameter and length of the trephine (Fig. 2A, B, C AND D). After planning of the position, diameter, depth, axis and size of short dental trephine by the clinician, the company manufactured and shipped the individual patient surgical guide (2INGIS®, Zaventem, Belgium) (Fig. 2E). The surgical guide was printed in try-in resin using a 3D printer NextDent™ 5100 (3D Systems®). A tooth support structure was designed. It consisted of the two parallel solid tubes integrated in the framework of the guide (Fig. 3A), into which the two legs of a fork attached to the head of the contra-angle can slide (Fig. 3B). The penetration of the trephine (Fig. 3C) was controlled by the depth stop on the fork on the guide framework.
Surgical 3D planification. A. Overview of 3D images reconstructions of CBCT and mouth cast registration with simulation of implant placement. B, C, D. CBCT 3D reconstruction images showing simulation of implant placement with its apex going through buccal cortical in interradicular space of tooth #36. E. Computer aided design of custom-made surgical guide
View of custom-made 3D-printed sleeveless surgical guide with guided head of the contra-angle. A. Tooth support resin surgical guide with two parallel solid tubes integrated in the framework of the guide. B. Two legs of a fork attached to the head of the contra-angle. C. Graduated short trephine Ø3.5
Local anaesthesia of buccal alveolar mucosa below the first lower molar was done. Then, the surgical guide was positioned in the mouth ((Fig. 4A and B). A vertical incision was made on the alveolar mucosa (Fig. 4C). A full-thickness flap was raised to access to the bone cortical with the trephine (Fig. 4D). A specific surgical kit was used. It included a contra-angle with guide forks of different lengths (depending on the patient’s capacity to open the mouth and laxity of cheek musculature). The guidance system was supported by a double tube (one on either side of the drilling axis). A ring of uniform thickness was created at the point of impact on the buccal cortical with the graduated short trephine of 3.5 mm diameter (Thomas; FFDM Tivoly, Bourges, France) (Fig. 4E). This “window” was removed and placed in saline solution. An empty cavity was visually and tactilely identified during slight curettage avoiding root. Diagnosis of solitary bone cyst was confirmed. The cavity’s walls were curetted until the cavity was fully filled by a blood clot (Fig. 4F). The bone lid was repositioned into the defect (Fig. 4G), and two resorbable sutures were made to close mucosa. Post-operative medications were mouthwash (chlorhexidine 0.12%) one day after surgery for seven days.
Clinical views of surgical steps procedure. A. Intraoral placement of the surgical Guide. B. Good visibility of the surgical site. C. Vertical incision in the alveolar mucosa. D. Trephine penetration in cortical bone, the head of the contra-angle is guided by the the forks insered in two parallel solid tubes integrated in the framework of the guide. E. A ring bone was removed at the point of impact on the vestibular cortical bone. F. Curettage performed using a long and thin curette to create a blood clot, ensuring bone healing. G. Repositioning of the bone lid
The patient had only taken acetaminophen 1 g in postoperative time surgery. Surgical outcomes were uneventful. Soft tissue healing was complete after two weeks. After 6 months of follow-up a complete reossification of the bony defect was objectived (Fig. 5) and left mandibular molars had normal pulp sensitivities. After 2 years of follow-up, no local recurrence was noted (Fig. 6) but the roots showed slightly signs of external resorption.
Discussion
SBC is a benign intraosseous pseudocyst, most commonly observed in young adults. The mandible is almost exclusively affected. Most SBCs are discovered incidentally. Usually, SBC is radiolucent and unilocular with no or only slight expansion of bone and cortical thinning. Superior margins extend between the roots of teeth and are characteristically scalloped and corticated [11]. MRI demonstrates presence of fluid, fibrous connective tissue and/or gas. It confirms its cystic nature [12]. MRI features of SBC were highly characteristic and might allow them to be differentiated from others jaw diseases [13]. In this case, the combination of clinical and radiological findings confirmed the diagnosis of SBC. Given the benign nature of SBC and absence of epithelial lining, a minimally invasive approach through was warranted using a surgical guide for optimal bone cavity access. The objective of this surgical procedure was to achieve bone reossification while avoiding teeth and mandibular neurovascular bundle and ensuring minimal postoperative complications using a similar approach to guided targeted endodontic microsurgery [8, 14].
The main indications of 3D-printed surgical guide tools in oral and maxillofacial surgery include dental implant surgery, orthognathic surgery, mandibular reconstruction, Temporomandibular Joint reconstruction, maxillofacial prosthodontics and so far patient communication and education [15]. More recently, 3D-printed surgical guide tools were also used in the surgical management of jaws cysts and benign tumors [16, 17]. Two main types of surgical guide were designed: drilling location guides, which allows the surgical site to be precisely located, and osteotomy locating guides or cutting guides, which is used to delineate the osteotomy lines [16, 18,19,20,21]. Despite their benign nature, the excision of jaw cyst or tumoral lesions could require wide surgical access and extensive bone removal [22]. Management of less invasive pathology procedures might not require major reconstruction, however, use of surgical guide allows precise localization of the lesions with minimal bone removal, which is especially important when lesions are close to “noble organs” [23].
In a similar field, bone biopsies with 3D-printed surgical guide may be a helpful tool for enhancing the accuracy of the biopsy. Postl et al. demonstrated that guided procedures were more accurate with 3D-printed surgical guides compared to freehand methods. The mean deviation between biopsy axes was significantly lower in guided procedures than in freehand biopsies (1.4 mm ± 0.9 mm vs. 3.6 mm ± 1.0 mm; p = 0.0005). Similarly, the mean biopsy angle deviation was significantly lower in guided biopsies compared to freehand biopsies (6.8 ± 4.0 degrees vs. 15.4 ± 3.6 degrees; p = 0.0005). However, there was no significant difference in biopsy depth between guided and freehand biopsies [24].
Lotz et al. also described a tooth-supported drilling template technique for guided biopsy of the jawbone. They compared variation of digital planning of the biopsies and the position of the biopsies cylinder on the post-operative CBCT on fourteen patients. They found a mean angular deviation of 4.35 ± 2.5 degrees and a mean depth deviation of 1.40 ± 1.41 mm [17].
No clinical studies have so far been conducted on large patient samples to compare the accuracy or correspondence between the planned position in the software and the actual implant position post-intervention for traditional guided surgery systems versus the current sleeveless system.
Nevertheless, this sleeveless guided surgery system was tested, in order to determine the accuracy of implant insertion with one-piece ceramic implants. In total, 12 patients were enrolled in that study and installed with 20 implants by means of the aforementioned sleeveless static surgical guides. The accuracy of implant placement was checked using a non-invasive method, which permitted comparison of the planning data with the actual position of the fixtures after surgery. All implants were placed without any clinical problem and the mean deviations were 0.52 mm (95%CI: 0.37–0.67 mm) at the implant shoulder and 0.82 mm (95%CI: 0.56–1.08 mm) at the implant apex. Finally, the mean angular deviation was 2.85° (95%CI: 2.18°- 3.51°) with a deviation in height/depth of 0.35 mm (95%CI: 0.01–0.68 mm) [25]. Moreover, Zhao et al. (2023) showed in clinical endodontic microsurgery study that a designed 3D-printed surgical guide improve accuracy by fixing both the position and the angle of apectomy [26]. Ackerman et al. (2019) and Hawkins et al. (2020) also concluded, respectively in cadaver study and in vitro study, that targeted guided endodontic microsurgery was more accurate compared to freehand surgery to determine peri-apical lesion location and remove it, similarly as in our SBC case [8, 14].
The presence of two guides that drive the handpiece, positioned laterally, might potentially contribute to stabilizing trephine placement and reducing errors [25, 27, 28]. The access and visibility of the lesion facilitated the rapid curettage with safe excision of the ring bone without any induced forces this was reflected positively on the postoperative outcomes minimizing pain, swelling and trismus while, preserving the dental roots and the inferior alveolar nerve integrity. This kind of surgical guide can solves the lack of vertical space in mouth’s posterior region and allows the clinicians to work with shorter trephines or drills permitting to perform surgeries in partially dentate patients with limited mouth opening [28,29,30]. It was nevertheless necessary to evaluate the laxity of cheek musculature in pre-operative time.
The use of trephine drill-guided osteotomies can induce excessive frictional heat, leading to thermal damage of soft and hard tissue. The trephine has closely arranged cutting blades at the tip, which generate significant friction. Heat generation with trephines was found to be greater compared to conventional drills [31]. To counteract excessive heat generation, a large diameter and reduced depth penetration have shown lower heat generation during guided osteotomy preparation [32]. Moreover, the specific guide design allows permanent direct external irrigation at the trepanation site [25], with pumping movements limiting osseous necrosis [17].
A therapeutic alternative that could have been considered in our case is dynamic surgical navigation. This approach is comparable to static guided surgery in terms of accuracy, minimally invasive intervention, reduced operating time with minimal space requirement for drilling with a very good surgical open access [33, 34]. However, the necessity of a specific costly device, operator’s learning curve with specific ergonomics (indirect vision, size of the contra-angle) don’t allow dynamic navigation to be used by all surgeons [35, 36]. Similarly, augmented reality could be an other interesting approach to determine the better surgical access with a minimal invasiveness but need to be confirmed with further studies [37, 38].
Presurgical errors can manifest at various step of guide fabrication, including manual or digital impression-taking, cast fabrication, or registration of DICOM dataset with mouth impression STL dataset. Errors may also occur during surgery if the guide is not accurately placed, leading to tilting, or if sideway forces are applied during the ostectomy. Additionally, errors can happen if the drill tilts, particularly in cases where there is a small but specific space between the guide hole and the drill [39]. The fabrication of surgical guides is time-consuming and labor-intensive. Consequently, most dental office lack the capacity to produce in-house surgical guides. While external manufacturers can create case-specific surgical guides, the associated costs could be expensive [39, 40].
However, preoperative planning takes more time, is more difficult or requires a certain degree of knowledge and techniques in computer sciences. Surgical guides surely reduce operative time and reduce operating room costs secondary to shortening procedure times [41].
The use of a surgical guide greatly increases the effectiveness of a procedure. Surgical guides enhance the accuracy and predictability of the surgery, decrease technologic sensitivity and decrease the time required for surgery.
Conclusion
In the procedure described in this report, the custom-made sleeveless static surgical guide played a key role in the success of the surgery because providing a precise location for the SBC. This allowed for a minimal window for accessing to the lesion and avoiding tooth and inferior alveolar bundle. As a result, a complete reossification was obtained with no surgical complications. It represents a surgical tool to determine the location and could be indicated in various cases cysts and tumors of the jaw.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- CBCT:
-
Cone beam computed tomography
- MRI:
-
Magnetic resonance imaging
- SBC:
-
Solitary bone cyst
- STL:
-
Stereolithographic
References
Vered M, Wright JM. Update from the 5th Edition of the World Health Organization Classification of Head and Neck tumors: odontogenic and maxillofacial bone tumours. Head Neck Pathol mars. 2022;16(1):63–75.
Harnet JC, Lombardi T, Klewansky P, Rieger J, Tempe MH, Clavert JM. Solitary bone cyst of the Jaws: a review of the etiopathogenic hypotheses. J Oral Maxillofac Surg Nov. 2008;66(11):2345–8.
Emerich K, Tomczak M, Kozakiewicz M. Radiological evaluation key to diagnosis of idiopathic solitary cyst. J Clin Pediatr Dent 1 janv. 2019;43(4):281–7.
Tamiolakis P, Thermos G, Tosios KI, Sklavounou-Andrikopoulou A. Demographic and clinical characteristics of 5294 Jaw cysts: a retrospective study of 38 years. Head Neck Pathol déc. 2019;13(4):587–96.
Bindra S, Jadaun G, Jois H, Sen P. Traumatic bone cyst of mandible: a case report of rare entity and review of literature. Contemp Clin Dent. 2019;10(1):3.
Madiraju G, Yallamraju S, Rajendran V, SrinivasaRao K. Solitary bone cyst of the mandible: a case report and brief review of literature. Case Rep 30 Juill. 2014;2014(jul30 1):bcr2013200945–2013200945.
Docquier P-L, Schubert T. Kyste osseux solitaire. Radiol Imag MÉDICALE Musculosquelettique -. Neurol - Maxillofac. 2022;41(1):1–10.
Hawkins TK, Wealleans JA, Pratt AM, Ray JJ. Targeted endodontic microsurgery and endodontic microsurgery: a surgical simulation comparison. Int Endod J Mai. 2020;53(5):715–22.
Eriksson L, Hansson LG, Åkesson L, Ståhlberg F. Simple bone cyst: a discrepancy between magnetic resonance imaging and surgical observations. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontology déc. 2001;92(6):694–8.
Rushton MA. Solitary bone cysts in the mandible. Br Dent J Juill. 1946;81(2):37–49.
Gopalakrishnan R. Simple Bone Cyst. In: WHO Classification of Tumours Editorial Board. Head and neck tumours [Internet; beta version ahead of print]. Lyon (France): International Agency for Research on Cancer; 2022 [cited 2024/01/26]. (WHO classification of tumours series, 5th ed.; vol. 9). https://tumourclassification.iarc.who.int/chapters/52.
Konouchi H, Yanagi Y, Hisatomi M, Matsuzaki H, Takenobu T, Unetsubo T, et al. MR imaging diagnostic protocol for unilocular lesions of the jaw. Jpn Dent Sci Rev août. 2012;48(2):81–91.
Yanagi Y, Asaumi J, ichi, Unetsubo T, Ashida M, Takenobu T, Hisatomi M et al. sept. Usefulness of MRI and dynamic contrast-enhanced MRI for differential diagnosis of simple bone cysts from true cysts in the jaw. Oral surg oral Med oral pathol oral Radiol Endodontology. 2010;110(3):364–9.
Ackerman S, Aguilera FC, Buie JM, Glickman GN, Umorin M, Wang Q, et al. Accuracy of 3-dimensional–printed endodontic Surgical Guide: A Human Cadaver Study. J Endod mai. 2019;45(5):615–8.
Louvrier A, Marty P, Barrabé A, Euvrard E, Chatelain B, Weber E, et al. How useful is 3D printing in maxillofacial surgery? J Stomatol Oral Maxillofac Surg Sept. 2017;118(4):206–12.
Gernandt S, Tomasella O, Scolozzi P, Fenelon M. Contribution of 3D printing for the surgical management of jaws cysts and benign tumors: a systematic review of the literature. J Stomatol Oral Maxillofac Surg Sept. 2023;124(4):101433.
Lotz M, Schumacher C, Stadlinger B, Ikenberg K, Rücker M, Valdec S. Accuracy of guided biopsy of the jawbone in a clinical setting: a retrospective analysis. J Cranio-Maxillofac Surg Juill. 2021;49(7):556–61.
Lee H, Choi S, Chae YK, Jung J, Choi SC, Nam OH. Customized surgical guide with a bite block and retraction arm for a deeply impacted odontoma; a technical note. J Stomatol Oral Maxillofac Surg Sept. 2021;122(4):456–7.
Abdelazez AKH, Hany HED, El Din MEG, El Meregy MMM, Abdelhameed AMF, El-Kabany IM, et al. The evaluation of the effect of performing guided lid surgery with enucleation of a cystic lesion; a case report. Int J Surg Case Rep août. 2022;97:107385.
Wilt DC, Kim B, Zaid W. The Use of virtual Surgical-guided Osteoplasty for Maxillofacial Brown tumors. J Craniofac Surg Sept. 2019;30(6):e551–3.
Fujioka-Kobayashi M, Miyasaka N, Miyasaka A, Koyanagi M, Inada R, Miyasaka T, et al. A custom-made Surgical Guide for Accurate Enucleation of Nasopalatine Duct cysts: a technical note and case report. Souza LND, éditeur. Case Rep Dent 1 août. 2023;2023:1–5.
Omara M, Gouda A, Ali S. Computer-guided buccal cortical plate separation for removal of calcified benign odontogenic tumors affecting the mandibular angle region. Maxillofac Plast Reconstr Surg. sept 2022;22(1):30.
Cohen JM, Ziccardi VB. oct. Use of Virtual Surgical Planning as an Adjunct for Enucleation of Multiple Recurrent Odontogenic Keratocysts: Case Report. J Oral Maxillofac Surg. 2018;76(10):2137.e1-2137.e6.
Postl L, Mücke T, Hunger S, Wuersching SN, Holberg S, Bissinger O, et al. Biopsies of osseous jaw lesions using 3D-printed surgical guides: a clinical study. Eur J Med Res déc. 2022;27(1):104.
Schnutenhaus S, von Koenigsmarck V, Blender S, Ambrosius L, Luthardt RG, Rudolph H. Precision of sleeveless 3D drill guides for insertion of one-piece ceramic implants: a prospective clinical trial. Int J Comput Dent. 2018;21(2):97–105.
Zhao D, Xie W, Li T, Wang A, Wu L, Kang W, et al. New-designed 3D printed surgical guide promotes the accuracy of endodontic microsurgery: a study of 14 upper anterior teeth. Sci Rep 19 sept. 2023;13(1):15512.
Fauroux MA, De Boutray M, Malthiéry E, Torres JH. New innovative method relating guided surgery to dental implant placement. J Stomatol Oral Maxillofac Surg juin. 2018;119(3):249–53.
Mouhyi J, Salama MA, Mangano FG, Mangano C, Margiani B, Admakin O. A novel guided surgery system with a sleeveless open frame structure: a retrospective clinical study on 38 partially edentulous patients with 1 year of follow-up. BMC Oral Health déc. 2019;19(1):253.
Torres A, Lerut K, Lambrechts P, Jacobs R. Guided endodontics: Use of a Sleeveless Guide System on an Upper Premolar with Pulp Canal Obliteration and apical periodontitis. J Endod janv. 2021;47(1):133–9.
Bordone A, Ciaschetti M, Perez C, Couvrechel C. Guided endodontics in the management of Intracanal separated instruments: a Case Report. J Contemp Dent Pract 1 août. 2022;23(8):853–6.
Omar S, Jaiswal H, Mishra S, Bhargava D, Kumar P. A comparative study to evaluate the heat generated during osteotomy with conventional Drill, Trephine and Alveolar Expander. Eur Oral Res 29 août. 2022;0(0):0–0.
Kuster M, Mukaddam K, Zitzmann N, Filippi A, Kühl S. Influence of a Novel Drill Design on Heat Generation during Conventional and guided Implant Osteotomy. Int J Oral Maxillofac Implants Mai. 2021;36(3):e31–41.
Block MS, Emery RW, Cullum DR, Sheikh A. Implant Placement is more Accurate using dynamic Navigation. J Oral Maxillofac Surg Juill. 2017;75(7):1377–86.
Wu D, Zhou L, Yang J, Zhang B, Lin Y, Chen J, et al. Accuracy of dynamic navigation compared to static surgical guide for dental implant placement. Int J Implant Dent déc. 2020;6(1):78.
Gargallo-Albiol J, Barootchi S, Salomó-Coll O, Wang H. lay. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann Anat - Anat Anz. sept 2019;225:1–10.
Zhan Y, Wang M, Cheng X, Li Y, Shi X, Liu F. Evaluation of a dynamic navigation system for training students in dental implant placement. J Dent Educ févr. 2021;85(2):120–7.
Remschmidt B, Rieder M, Gsaxner C, Gaessler J, Payer M, Wallner J. Augmented reality-guided apicoectomy based on Maxillofacial CBCT scans. Diagnostics 25 sept. 2023;13(19):3037.
Bosshard FA, Valdec S, Dehghani N, Wiedemeier D, Fürnstahl P, Stadlinger B. Accuracy of augmented reality-assisted vs template-guided apicoectomy - an ex vivo comparative study. Int J Comput Dent 24 févr. 2023;26(1):11–8.
Jo C, Bae D, Choi B, Kim J. Removal of Supernumerary Teeth utilizing a computer-aided Design/Computer-Aided Manufacturing Surgical Guide. J Oral Maxillofac Surg Mai. 2017;75(5):924.
Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, Fortin T. Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials. BMC Oral Health déc. 2017;17(1):150.
Ballard DH, Mills P, Duszak R, Weisman JA, Rybicki FJ, Woodard PK. Medical 3D Printing cost-savings in orthopedic and maxillofacial surgery: cost analysis of operating Room Time Saved with 3D printed anatomic models and Surgical guides. Acad Radiol août. 2020;27(8):1103–13.
Acknowledgements
The authors wish to express their gratitude to Philippe De Moyer and the company 2INGIS® (Zaventem, Belgium) for designing and printing this surgical guide free of charge.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MD made substantial contributions for acquisition of clinical and radiological data. He has been involved in drafting and writing the manuscript. CP made substantial contributions for the conception of the guide. QL made substantial contributions in the analysis and interpretation of the data. FB has been involved in revising the manuscript critically for important intellectual content, translation and gave final approval for the version of the manuscript to be published. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient in written form.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Delarue, M., Perez, C., Lucidarme, Q. et al. Management of a solitary bone cyst using a custom-made surgical guide for a minimally invasive approach: technical note and case report. BMC Oral Health 24, 560 (2024). https://doi.org/10.1186/s12903-024-04308-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04308-4